Abstract
Background
Pulmonary arterial hypertension (PAH) is a severe complication of systemic lupus erythematosus (SLE). This study aims to explore the clinical characteristics and prognosis in SLE-PAH based on consensus clustering and risk prediction model.
Methods
A total of 205 PAH (including 163 SLE-PAH and 42 idiopathic PAH) patients were enrolled retrospectively based on medical records at the First Affiliated Hospital of Zhengzhou University from July 2014 to June 2021. Unsupervised consensus clustering was used to identify SLE-PAH subtypes that best represent the data pattern. The Kaplan–Meier survival was analyzed in different subtypes. Besides, the least absolute shrinkage and selection operator combined with Cox proportional hazards regression model were performed to construct the SLE-PAH risk prediction model.
Results
Clustering analysis defined two subtypes, cluster 1 (n = 134) and cluster 2 (n = 29). Compared with cluster 1, SLE-PAH patients in cluster 2 had less favorable levels of poor cardiac, kidney, and coagulation function markers, with higher SLE disease activity, less frequency of PAH medications, and lower survival rate within 2 years (86.2% vs. 92.8%) (P < 0.05). The risk prediction model was also constructed, including older age at diagnosis (≥ 38 years), anti-dsDNA antibody, neuropsychiatric lupus, and platelet distribution width (PDW).
Conclusions
Consensus clustering identified two distinct SLE-PAH subtypes which were associated with survival outcomes. Four prognostic factors for death were discovered to construct the SLE-PAH risk prediction model.
Similar content being viewed by others
Introduction
Pulmonary arterial hypertension (PAH) is a devastating complication of systemic lupus erythematosus (SLE) [1]. Compared to Western countries, SLE-PAH occurs more frequently in East Asia, carrying high mortality and morbidity [2, 3]. The 5-year overall survival rate varies from 68 to 84% [4, 5]. Although PAH-targeted drugs (PTDs) have been widely prescribed over decades, a fraction of SLE-PAH patients still have poor responses to therapy [6]. This suggests that unique clinical characteristics and immune microenvironment dysregulation in SLE could not be ignored. Apart from cardiopulmonary injury, SLE-PAH patients may also suffer from other organ involvements, implicating the kidney, skin, and central nervous system [7]. These multiple clinical phenotypes could impact their treatment response and prognosis. Hence, recognizing subtypes of SLE-PAH would help to tailor individualized regimens and improve patients’ outcomes [8].
Up to now, a variety of unsupervised clustering methods have been used for subtyping diseases, such as hierarchical clustering, k-means, and latent class analysis [9,10,11]. In 2018, Sun et al. classified SLE-PAH into two subtypes based on k-means, namely the vasculitic subtype and vasculopathic subtype, attempting to interpret the inflammatory and non-inflammatory pathogenesis of SLE-PAH [11]. Nevertheless, any single clustering method cannot avoid result bias, and its rationality and reliability lack unified standard verification [12]. Consensus clustering, an unsupervised integrative clustering methodology, comes into the spotlight. It can aggregate multiple clustering into a more stable clustering via resampling, which has been introduced in many studies [13,14,15]. For instance, by consensus clustering, Zheng et al. identified three clusters of chronic kidney disease patients and found a strong association between clusters and different clinical outcomes [15]. Therefore, re-classifying SLE-PAH by an integrative clustering analysis and exploring its clinical characteristics and outcomes would be clinically informative.
Currently, several risk stratification systems of pulmonary hypertension (PH) have been proposed, such as comprehensive and simplified risk assessment from the 2022 European Society of Cardiology (ESC)/European Respiratory Society (ERS) PH guidelines [16], or PAH risk score calculators released by Registry to Evaluate Early and Long-Term PAH Disease Management (REVEAL) [17, 18]. Conversely, due to pleiotropic clinical phenotypes in SLE-PAH patients, some risk profile tools are not good at discriminating high-risk patients, as well as partial variables that are invasive, time-consuming, and costly [19]. Thus, an accurate, non-invasive, and economical SLE-PAH risk prediction model is also needed.
In general, this study aimed to classify SLE-PAH based on consensus clustering analysis and construct a risk prediction model, for gaining a bettering understanding of SLE-PAH clinical characteristics, treatment, and outcomes. The flow chart of this study was shown in Fig. 1.
The flow chart of this study. SLE, systemic lupus erythematosus; PAH, pulmonary arterial hypertension; TTE, transthoracic echocardiography; RHC, right heart catheterization; K-M, Kaplan–Meier; IPAH, idiopathic PAH, LASSO, the least absolute shrinkage and selection operator; DCA, decision curve analysis
Methods
Patient selection
Patients diagnosed with SLE-PAH and idiopathic PAH (IPAH) in the First Affiliated Hospital of Zhengzhou University between July 2014 and June 2021 were identified in this retrospective study. SLE patients fulfilled the 1997 updated American College of Rheumatology (ACR) criteria or the Systemic Lupus International Collaborating Clinics (SLICC) group 2012 revised SLE classification criteria [20, 21]. PAH was defined as mean pulmonary artery pressure (mPAP) ≥ 20 mmHg at rest, pulmonary arterial wedge pressure ≤ 15 mmHg, and pulmonary vascular resistance (PVR) > 2 Wood units by right heart catheterization (RHC) [16] or a two consecutive pulmonary artery systolic pressure (PASP) values ≥ 40 mmHg within 3 months by transthoracic echocardiography (TTE) [22].
Patients aged < 16 years or those with a history of recent blood transfusion, recent pregnancy, congenital heart disease, rheumatic heart disease, hypertensive heart disease, myocardial infarction, pulmonary venous occlusion, pulmonary embolism, portal hypertension, chronic obstructive pulmonary disease, pulmonary malignancy, schistosomiasis, left heart diseases, or other connective tissue diseases were excluded.
Collection of clinical data
The date of baseline was defined as the date of SLE-PAH/IPAH diagnosis confirmed by RHC or TTE. Disease duration was defined as the time from symptom onset to SLE-PAH/IPAH diagnosis. Demographic information, clinical features, laboratory findings, and RHC and TTE parameters at the time of diagnosis were collected from hospital records. Anti-dsDNA antibody was detected by indirect immunofluorescence. The severity of SLE was evaluated by the systemic lupus erythematosus disease activity index-2000 (SLEDAI-2 K) [23]. Patients had planned and recorded comprehensive follow-up evaluations every 3 to 12 months. To be included, patients had to have been followed up for at least 1 year. The endpoint was death from any cause. The follow-up time to endpoint was calculated from the date of SLE-PAH/IPAH diagnosis to the date of death from any cause or to the date of last follow-up (up to June 30, 2022).
Statistical analysis
Statistical analysis was performed using SPSS 26.0 software (IBM), R software version 4.2.2 (The R Foundation for Statistical Computing), and Prism 9.3.1 software (GraphPad Software). Continuous variables were described as median (interquartile range [IQR]) and compared using the Mann–Whitney U test or Kruskal–Wallis test. Bonferroni was used to correct the P value for the post hoc test. Categorical variables were expressed as frequency (percentage) and compared using a chi-square test. Consensus clustering analysis was performed using the “ConsensusClusterPlus” R package [24]. The optimal number of clusters was determined by the cumulative distribution function (CDF) curves, consensus clustering score, and consensus plots. Principal component analysis (PCA) was conducted to display the geometrical distance of different subtypes. Kaplan–Meier (K-M) method was applied to describe the survival fractions, the log-rank test was conducted to compare overall survival distributions, and the weighted K-M test was used to compare the short-term survival difference using the R package “ComparisonSurv.”
As for the construction of the risk prediction model, SLE-PAH variables were preliminarily selected based on expert opinion and previous literature. All continuous variables were tested for linear trend, and which do not satisfy linearity would be converted to categorical variables. The cutoff value of these categorical variables was determined by clinical significance, or survival ROC function using the R package “survivalROC.” Subsequently, LASSO regression and univariate Cox analysis were performed to further examine prognostic variables using the R package “glmnet” [25]. Prognostic variables with P < 0.1 were then considered for multivariable modeling, before checking that the proportionality of the hazards assumption was met (Supplementary Table S1). The risk prediction model was built using the R package “rms,” and the bootstrap approach was used to validate the model internally. In addition, the C-index, calibration curves, and decision curve analysis (DCA) curves were also conducted for evaluating the model’s discrimination, calibration, and clinical practicability, respectively. Finally, the cohort was divided into high-risk or low-risk groups based on the cutoff value of the risk score, and survival distributions were estimated by the K-M method. Statistical significance was considered P < 0.05.
Results
SLE-PAH patient characteristics
A total of 163 patients with SLE-PAH were enrolled in this study, including 96.2% (157/163) females, with a median age at diagnosis at 37.0 years (IQR 30.0–49.0), ranging from 16 to 81 years, and the median disease duration was 24 months (IQR 3.0–84.0). All SLE-PAH patients underwent TTE and 46 underwent RHC examination. Besides, there were 100 (61.1%) patients complicated with serositis, 69 (42.6%) with lupus nephritis, and 43 (26.4%) with cardiac disorder. One hundred thirteen (69.3%) patients were in WHO Function Class (WHO FC) III–IV, and the median 6-min walk distance (6MWD) was 436.0 m (IQR 282.0, 534.0). Immunological variables revealed that 160 (98.1%) participants had anti-nuclear antibody (ANA) positivity, followed by 110 (67.9%) anti-Ro52 antibody positivity, 105 (64.8%) anti-nRNP/Sm antibody positivity, and 95 (59.4%) anti-SSA antibody positivity. A median mPAP in RHC was 40.0 mmHg (IQR 28.8, 49.3). Furthermore, 153 (93.9%) patients received glucocorticoids and 99 (60.7%) were treated with immunosuppressants, encompassing 43 (26.4%) mycophenolate mofetil (MMF) and 39 (23.9%) cyclophosphamide (CYC). Besides, 93 (57.1%) patients took PTDs treatment, comprising 55 (33.7%) phosphodiesterase-5 inhibitors (PDE-5Is), 65 (39.9%) endothelin receptor antagonists (ERAs), and 18 (11.1%) prostacyclin (PGI2). Of note, monotherapy of PTDs occupied 68 (41.7%) and combination therapy constituted 25 (15.3%). SLEDAI ≥ 10 accounted for 89 (54.6%) (Tables 1 and 2).
SLE-PAH patient survival
During the observation period, 28/163 (17.1%) patients died at a median of 27.0 months (IQR 7.3, 66.5) from diagnosis. The overall 1-, 3-, and 5-year survival rates in SLE-PAH patients were 93.9%, 87.2%, and 84.8%, correspondingly. Causes of death included 13 (46.4%) patients of heart failure, followed by 8 (28.6%) of respiratory failure, 5 (17.9%) of serious infection, 1 (3.6%) of cerebrovascular disease, and 1 (3.6%) of cirrhosis. For non-survivors, they had older age, shorter duration, higher platelet distribution width (PDW) level, higher ratio of WHO FC III/IV (100% vs. 63%), cardiac disorder (42.9% vs. 23.0%), and thrombocytopenia (42.9% vs. 21.9%) (P < 0.05). In the antinuclear antibody spectrum, the non-survivors’ anti-centromere antibody positivity was higher (21.4% vs. 5.2%), while the anti-dsDNA antibody was lower (28.6% vs. 51.1%) (P < 0.05). As for treatment, the proportion of hydroxychloroquine (HCQ) (57.1% vs. 83%) and MMF (7.1% vs. 30.4%) in the non-survivor group was lower (P < 0.05). Among RHC parameters and 6MWD, non-survivors had higher pulmonary vascular resistance (PVR) and cardiac index (CI) and shorter 6MWD (P < 0.05) (Supplementary Table S2, S3). There was no significant difference in SLEDAI-2 K, TTE parameters, and other regimens.
Identification of subtypes in SLE-PAH
Consensus clustering was used to classify 163 SLE-PAH patients. Among 2–9 clusters, when the value was set to two (k = 2), the consensus score of each cluster was close to 1.0 (Fig. 2A). The consensus matrix from k = 2 to 9 was visualized in heatmaps (Fig. 2B–K). Fluctuation ranges of CDF curves were minimum at consensus index 0.2–0.4 when the cluster was set to two (k = 2) (Fig. 2L). The changes in delta areas were presented in CDF plots when k = 2–9 (Fig. 2M). In sum, 2 subtypes were selected as the optimal clustering, namely cluster 1 (n = 134) and cluster 2 (n = 29). PCA showed 2 subtypes had a distinguished discrimination (Fig. 2N).
Identification of subtypes in SLE-PAH. A Consensus clustering score of clusters 2–9. B Consensus matrix legend of clusters 2–9. C Consensus clustering matrix when k = 2, D k = 3, E k = 4, F k = 5, G k = 6, H k = 7, I k = 8, and J k = 9. K Tracking plot of clustering. L CDF curves of clustering. M CDF delta area curves. N PCA visualizes the distribution of two subtypes. CDF, cumulative distribution function; PCA, principal component analysis
In general, compared with cluster 1, SLE-PAH patients in cluster 2 had less favorable levels of poor cardiac, kidney, and coagulation function markers, with higher SLE disease activity, less frequency of PAH medications, and lower survival rate within 2 years (P < 0.05). These are described as follows:
Lupus nephritis (72.4% vs. 36.6%), serositis (79.3% vs. 57.5%), cardiac disorder (44.8% vs. 22.4%), peripheral thrombosis (13.8% vs. 2.2%), and high SLE disease activity (SLEDAI score ≥ 10) (75.9% vs. 50.0%) were more common in cluster 2 than in cluster 1 (P < 0.05). Among laboratory findings, the levels of creatinine, serum uric acid, D-dimer, and NT-proBNP in cluster 2 raised significantly, while the level of hemoglobin, lymphocyte, eGFR, and C3 declined (P < 0.05). However, there was no significant difference in erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). In the antinuclear antibody spectrum, less frequency of anti-Ro-52 antibody positivity occurred in cluster 2 (51.7% vs. 70.9%, P < 0.05). The ratio of PTDs in cluster 2 was lower (31.0% vs. 62.7%, P < 0.05), especially PDE-5Is (10.3% vs. 38.8%, P < 0.05), yet there was no statistical difference in other therapies. Regarding TTE, RHC parameters, and 6WMD, the cardiac function of cluster 2 was poorer, with lower left ventricular ejection fraction (LVEF) and cardiac index (CI), higher PVR, and shorter 6WMD (P < 0.05) (Tables 1 and 2, and S4). K-M analysis showed that the survival rate of cluster 2 was significantly poorer than cluster 1 within 2 years (86.2% vs. 92.8%, P < 0.05), whereas there was no prominent difference in survival rate over 2 years (Fig. 3).
Comparison between SLE-PAH subtypes and IPAH
Forty-two IPAH patients were included for further comparison to SLE-PAH subtypes. In demography, there was a female predominance in cluster 1 compared with IPAH (97.0% vs. 83.3%, P < 0.05). Among clinical features, cluster 1 and cluster 2 both had a rate of serositis and renal involvement compared to IPAH (P < 0.05). In laboratory findings, hemoglobin and lymphocyte levels in both 2 clusters decreased, and D-dimer levels elevated (P < 0.05). As for detailed differences among the three groups, compared with IPAH, creatinine levels declined in cluster 1, while NT-proBNP, creatinine, and uric acid levels in cluster 2 raised (P < 0.05). Among TTE indicators, IPAH patients had higher PASP and tricuspid regurgitation (TR) than 2 clusters, but cluster 2 had lower LVEF (P < 0.05). In RHC, IPAH had higher mPAP and PVR and lower CI levels than cluster 1 (P < 0.05). In PTDs therapy, the percentage of PTDs (including PDE-5Is and ERAs) used in SLE-PAH subtypes occupied less than in the IPAH group (62.7% and 31.0% vs. 92.9%), especially less frequent in PTD combination therapy (P < 0.05). There was no significant difference in deaths among the three groups (Supplementary Table S5).
Construction and validation of risk prediction model in SLE-PAH
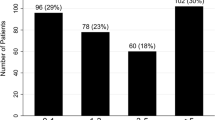
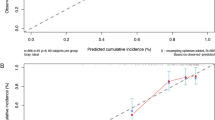
After LASSO-Cox regression analysis (Fig. 4A and B), four prognostic factors were finally identified: older age at diagnosis (≥ 38 years) [HR = 3.17, 95% CI (1.25–8.03)], anti-dsDNA antibody [HR = 0.28, 95% CI (0.11–0.75)], neuropsychiatric lupus [HR = 6.34, 95% CI (1.58–25.49)], and PDW [HR = 2.03, 95% CI (1.25–3.29)] (P < 0.05) (Table 3), of which anti-dsDNA antibody was protective and others were risk for death with SLE-PAH patients. Based on these factors, a nomogram model was constructed and evaluated, where the prognostic index = 0.922 × older age at diagnosis (≥ 38 years) − 0.816 × anti-dsDNA antibodies + 1.268 × neuropsychiatric lupus + 0.841 × PDW (Fig. 4C). The overall C-index of the model was 0.80, and after, the bootstrap correction was 0.77. The 1-, 3-, and 5-year C-index values were 84.4, 79.6, and 81.4, and after, the bootstrap correction were 77.0, 73.6, and 74.8, relatively. Additionally, the DCA curves and 1-, 3-, and 5-year calibration curves were visualized, indicating good clinical effectiveness and calibration (Fig. 4D–G). Furthermore, based on the optimal cutoff value of the risk score (risk score = 0.670), the K-M analysis showed that there was an eminent survival difference between high-risk and low-risk groups (P < 0.05) (Fig. 5).
Construction and validation of risk prediction model of SLE-PAH. A, B Variable selection using the LASSO-Cox regression model. C Nomogram predicting the 1-, 3-, and 5-year survival probability of SLE-PAH patients. D DCA curves. E, F 1-, 3-, and 5-year calibration curves. LASSO, the least absolute shrinkage and selection operator; DCA, decision curve analysis; OS, overall survival
Discussion
As a life-threatening complication of SLE patients, PAH generally causes distinguished clinical worsens and poor outcomes. Thus, it is necessary to explore the clinical phenotype characteristics and prognostic factors in SLE-PAH. In this study, we identified two distinct subtypes of SLE-PAH based on unsupervised consensus clustering methodology for the first time and constructed a risk prediction model of SLE-PAH, with the ultimate goal of improving SLE-PAH assessment, treatment, and prognosis.
In our sample, the 1-, 3-, and 5-year overall survival rates were 93.9%, 87.2%, and 84.8%, respectively, which was higher than the data from a 2017 meta-analysis of 323 SLE-PAH patients (88%, 81%, 68%) and a large, multi-center Chinese cohort reported by the 2019 Chinese SLE Treatment and Research Group (CSTAR) study (92.1%, 84.8%, 72.9%) [4, 5]. The different ethnicity, cohort size, baseline characteristics, and treatment regimens across different regions and countries might be attributed to the heterogeneity in the long-term prognosis of SLE-PAH. In addition, heart failure was the leading cause of death in most SLE-PAH patients [26]. We found that 13 cases had heart failure among 28 non-survivors, which was in line with the early research. This might be because increasing PASP could cause a pronounced right ventricle afterload, eliciting progressive ventricular hypertrophy, right heart failure, and ultimately death [2].
SLE-PAH has complex pathogenesis and strong heterogeneity. Generally, there have been two putative pathological mechanisms of SLE-PAH, autoimmune-mediated inflammatory process and non-inflammatory vascular remodeling. As aforementioned, Sun et al. have divided 108 SLE-PAH patients into two subtypes, namely the vasculitic subtype and the vasculopathic subtype, trying to interpret these two mechanisms [11, 27]. To be specific, patients in the vasculitic subtype had systemic manifestations, high SLE disease activity, better response to drugs, and higher survival rates. In contrast, patients in the vasculopathic subtype were more likely to present purer PAH, that was, high pulmonary arterial pressure, poor cardiac function, poor response to drugs, and lower survival rate, albeit with mild inflammatory response and low disease activity. However, this classification of SLE-PAH has always been controversial.
In our study, we re-identified SLE-PAH subtypes through an integrative unsupervised consensus clustering and also found two distinct subtypes (cluster 1 and cluster 2). Compared with cluster 1, patients in cluster 2 had more organ involvement, higher disease activity, less PTD treatment, and poorer survival rate within 2 years. Furthermore, compared to IPAH, cluster 1 had female predominance and milder kidney and pulmonary damage, whereas cluster 2 had poorer cardiac and renal damage. Both clusters had a lower proportion of PTDs (PDE5-1I or ERA), especially less frequent in PTD combination therapy. In sum, two subtypes were different from the vasculitic and vasculopathic subtypes, suggesting diverse clinical phenotypes in SLE-PAH patients. It seems that inflammation and non-inflammation pathogenesis should not be completely isolated. Cross-interaction of both might lead to SLE-PAH progression. In a clinical view, when managing SLE-PAH patients, especially those who have cluster 2 characteristics, clinicians should focus on a 2-year treatment window and administer PTDs promptly for preventing irreversible pulmonary vascular damage.
Currently, the precise pathogenesis of SLE-PAH has not been fully elucidated. Several studies have explored the risk factors for death of SLE-PAH, such as poor cardiac function and exercise capacity; increased mPAP, PVR, BNP/NT-proBNP, and serum uric acid; and high rate of thrombocytopenia, pulmonary vasculitis, and Raynaud’s phenomenon [28,29,30]. In our study, similarly, we found PVR, the proportion of thrombocytopenia, and WHO FC III/IV were higher in non-survivors. In the risk prediction model, we newly identified four prognostic factors: older age at diagnosis (≥ 38 years), neuropsychiatric lupus, anti-dsDNA antibody, and PDW. As of today, Few studies have reported the relationship between neuropsychiatric lupus and PAH. Celfe et al. identified that neuropsychiatric lupus was more common in the PH group of SLE compared with the non-PH group [31]. Interestingly, in another study about neuropsychiatric SLE patients, Magro-Checa et al. showed that cardiovascular risk factors, especially arterial hypertension, were associated with ischemic changes in brain MRI, mainly lacunar stroke and brain atrophy [32]. Yet, the linkage between PAH and neuropsychiatric involvement in SLE needs to be further explored.
As for autoantibodies, conclusive evidence has not been obtained on whether lupus autoantibodies participated in SLE-PAH pathogenesis. Previous studies have indicated that the anti-RNP antibody in PAH might be implicated in injuring pulmonary vascular endothelial cells, inducing the proliferation of smooth muscle fibers [33, 34]. Antiphospholipid antibodies, especially the anticardiolipin antibody and lupus anticoagulant, were also related to increased risk for PAH occurrence [35, 36]. Anti-dsDNA antibodies are generally a hallmark of SLE diagnosis and classification, yet their role in PAH has not been fully understood. Studies have reported that anti-dsDNA antibodies, together with other autoantibodies, might directly damage vascular epithelial cells or form immune complexes depositing in the vascular wall, eliciting vasoconstriction, platelet aggregation, and thrombosis in SLE-PAH [37]. In the present study, however, we found that anti-dsDNA antibody was protective for death in SLE-PAH patients, which might reveal its complicated effect. As is known, anti-dsDNA antibody has different subclasses, including IgA, IgE, IgG, and IgM. However, not all of them contribute to tissue injuries in SLE. Ubiquitously, IgG and IgA correlate with SLE disease activity, but IgM was protective by inducing the eradication of apoptotic material and via immunomodulatory effects, thus attenuating cardiovascular dysfunction in SLE patients [38]. However, how anti-dsDNA subclasses exert a dual role in SLE-PAH courses is still unclear, and further research is needed to demonstrate.
Intriguingly, our results also confirmed that PDW was an independent risk factor for death in SLE-PAH. As an indicator of platelet activation, elevated PDW level represents a great dispersion in platelet volume and declined homogeneity [39]. As noted above, thrombocytopenia was strongly related to SLE-PAH prognosis. Previous studies have investigated that PDW rose significantly in IPAH and were positively associated with SLE disease activity [39, 40]. He et al. directly found that PDW could be a predictor of the early diagnosis of SLE-PAH [41]. These findings indicated that PDW which symbolizes abnormal platelet activity may play a pivotal role in SLE-PAH. After platelets were activated and destructed, the larger platelets with increased adhesion and aggregation would induce thrombogenesis, ascending PVR and PASP [42, 43]. Meanwhile, platelet activation could also stimulate inflammatory factors and complements releasing in SLE patients, damaging pulmonary vascular endothelial cells, promoting immune complexes depositing in the vessel wall, and eventually triggering the occurrence of pulmonary vascular diseases [44, 45].
There are several limitations to our study. Firstly, the retrospective nature and the selection of cases from a single center might have caused a selection bias. Given patients were selected from a center for SLE-PAH, more severe forms of the disease were recorded. Secondly, in our study, 88/205 individuals had underwent RHC estimation. Despite a previous study has defined a PASP of 40 mmHg measured by TTE as a good cutoff value for PAH diagnosis, RHC is the gold standard for PAH measurement. Finally, the sample size of this study is small, and the risk prediction model lacks external validation, so prospective and multicenter cohort studies are needed for further verification in the future.
Conclusions
In this retrospective cohort study, we found two distinct subtypes in SLE-PAH patients based on consensus clustering analysis. Patients in cluster 2 had more organ involvement, higher SLE disease activity, and poorer survival rate within 2 years. Besides, a risk prediction model for the death of SLE-PAH patients was constructed, including older age at diagnosis (≥ 38 years), anti-dsDNA antibodies, neuropsychiatric lupus, and PDW. The model had great discrimination, calibration, and clinical practicability.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SLE:
-
Systemic lupus erythematosus
- PAH:
-
Pulmonary arterial hypertension
- ILD:
-
Interstitial lung disease
- APS:
-
Antiphospholipid syndrome
- WHO FC:
-
World Health Organization Functional Class
- SLEDAI-2K:
-
Systemic lupus erythematosus disease activity index-2000
- PDW:
-
Platelet distribution width
- NT-proBNP:
-
N-terminal pro-B-type natriuretic peptide
- eGFR:
-
Estimated glomerular filtration rate
- CRP:
-
C-reactive protein
- ESR:
-
Erythrocyte sedimentation rate
- PASP:
-
Pulmonary artery systolic pressure
- TR:
-
Tricuspid regurgitation
- LVEF:
-
Left ventricular ejection fraction
- ANA:
-
Antinuclear antibodies
- dsDNA:
-
Double-stranded DNA
- RNP:
-
Ribonucleoprotein
- TTE:
-
Transthoracic echocardiography
- GC:
-
Glucocorticoids
- IS:
-
Immunosuppressants
- HCQ:
-
Hydroxychloroquine
- MMF:
-
Mycophenolate mofetil
- CYC:
-
Cyclophosphamide
- PTDs:
-
PAH-targeted drugs
- PDE-5I:
-
Phosphodiesterase-5 inhibitor
- ERA:
-
Endothelin receptor antagonist
- PGI2:
-
Prostacyclin
- RHC:
-
Right heart catheterization
- mPAP:
-
Mean pulmonary arterial pressure
- PAWP:
-
Pulmonary arterial wedge pressure
- PVR:
-
Pulmonary vascular resistance
- WU:
-
Wood units
- CI:
-
Cardiac index
- RAP:
-
Right arterial pressure
- SVO2 :
-
Mixed venous oxygen saturation
- 6MWD:
-
6-Min walking distance
References
Fei Y, Shi X, Gan F, Li X, Zhang W, Li M, et al. Death causes and pathogens analysis of systemic lupus erythematosus during the past 26 years. Clin Rheumatol. 2014;33(1):57–63.
Cansu DU, Korkmaz C. Pulmonary hypertension in connective tissue diseases: epidemiology, pathogenesis, and treatment. Clin Rheumatol. 2022;41. https://doi.org/10.1007/s10067-022-06446-y.
Mu L, Hao Y, Fan Y, Huang H, Yang X, Xie A, et al. Mortality and prognostic factors in Chinese patients with systemic lupus erythematosus. Lupus. 2018;27(10):1742–52.
Qian J, Li M, Zhang X, Wang Q, Zhao J, Tian Z, et al. Long-term prognosis of patients with systemic lupus erythematosus-associated pulmonary arterial hypertension: CSTAR-PAH cohort study. Eur Respir J. 2019;53(2):1800081.
Qian J, Wang Y, Huang C, Yang X, Zhao J, Wang Q, et al. Survival and prognostic factors of systemic lupus erythematosus-associated pulmonary arterial hypertension: a PRISMA-compliant systematic review and meta-analysis. Autoimmun Rev. 2016;15(3):250–7.
Parperis K, Velidakis N, Khattab E, Gkougkoudi E, Kadoglou N. Systemic Lupus Erythematosus and Pulmonary Hypertension. Int J Mol Sci. 2023;24(6):5085.
Qu J, Li M, Wang Y, Duan X, Luo H, Zhao C, et al. Predicting the risk of pulmonary arterial hypertension in systemic lupus erythematosus: a Chinese systemic lupus erythematosus treatment and research group cohort study. Arthritis Rheumatol. 2021;73(10):1847–55.
Zhang X, Zhao JL, Ding F, Yang J, Wang J, Zeng XF, et al. Recommendations for the diagnosis and treatment of connective tissue disease associated pulmonary arterial hypertension in China. Zhonghua Nei Ke Za Zhi. 2022;61(11):1206–16.
Murphy SL, Chen YT, Lee YC, Carns M, Aren K, Korman B, et al. Differences in symptom experience among patients with systemic sclerosis: a cluster analytic approach to identifying subgroups. Rheumatology (Oxford). 2023;62(SI):SI64-SI73.
Sugiyama T, Furuta S, Hiraguri M, Ikeda K, Inaba Y, Kagami SI, et al. Latent class analysis of 216 patients with adult-onset Still’s disease. Arthritis Res Ther. 2022;24(1):7.
Sun F, Lei Y, Wu W, Guo L, Wang K, Chen Z, et al. Two distinct clinical phenotypes of pulmonary arterial hypertension secondary to systemic lupus erythematosus. Ann Rheum Dis. 2019;78(1):148–50.
Rodriguez MZ, Comin CH, Casanova D, Bruno OM, Amancio DR, Costa L, et al. Clustering algorithms: a comparative approach. PLoS ONE. 2019;14(1): e0210236.
Soria D, Garibaldi JM, Ambrogi F, Green AR, Powe D, Rakha E, et al. A methodology to identify consensus classes from clustering algorithms applied to immunohistochemical data from breast cancer patients. Comput Biol Med. 2010;40(3):318–30.
Thongprayoon C, Vaitla P, Jadlowiec CC, Leeaphorn N, Mao SA, Mao MA, et al. Use of machine learning consensus clustering to identify distinct subtypes of Black kidney transplant recipients and associated outcomes. JAMA Surg. 2022;157(7): e221286.
Zheng Z, Waikar SS, Schmidt IM, Landis JR, Hsu CY, Shafi T, et al. Subtyping CKD patients by consensus clustering: the Chronic Renal Insufficiency Cohort (CRIC) study. J Am Soc Nephrol. 2021;32(3):639–53.
Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger R, Brida M, et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. 2022;43(38):3618–731.
Benza RL, Kanwar MK, Raina A, Scott JV, Zhao CL, Selej M, et al. Development and validation of an abridged version of the REVEAL 2.0 Risk Score Calculator, REVEAL Lite 2, for use in patients with pulmonary arterial hypertension. Chest. 2021;159(1):337–346.
Benza RL, Gomberg-Maitland M, Miller DP, Frost A, Frantz RP, Foreman AJ, et al. The REVEAL Registry risk score calculator in patients newly diagnosed with pulmonary arterial hypertension. Chest. 2012;141(2):354–62.
Wang Q, Qian J, Li M, Zhang X, Wei W, Zuo X, et al. Risk assessment in systemic lupus erythematosus-associated pulmonary arterial hypertension: CSTAR-PAH cohort study. Ther Adv Chronic Dis. 2022;13:20406223221112530.
Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997;40(9):1725.
Petri M, Orbai AM, Alarcon GS, Gordon C, Merrill JT, Fortin PR, et al. Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum. 2012;64(8):2677–86.
Ruiz-Irastorza G, Garmendia M, Villar I, Egurbide MV, Aguirre C. Pulmonary hypertension in systemic lupus erythematosus: prevalence, predictors and diagnostic strategy. Autoimmun Rev. 2013;12(3):410–5.
Touma Z, Urowitz MB, Gladman DD. Systemic lupus erythematosus disease activity index 2000 responder index-50 website. J Rheumatol. 2013;40(5):733.
Wilkerson MD, Hayes DN. ConsensusClusterPlus: a class discovery tool with confidence assessments and item tracking. Bioinformatics. 2010;26(12):1572–3.
Friedman J, Hastie T, Tibshirani R. Regularization paths for generalized linear models via coordinate descent. J Stat Softw. 2010;33(1):1–22.
Zhang N, Li M, Qian J, Wang Q, Zhao J, Yang Z, et al. Pulmonary arterial hypertension in systemic lupus erythematosus based on a CSTAR-PAH study: baseline characteristics and risk factors. Int J Rheum Dis. 2019;22(5):921–8.
Qian J, Li M, Zhao J, Wang Q, Tian Z, Zeng X. Inflammation in SLE-PAH: good news or not? Ann Rheum Dis. 2019;78(12): e135.
Kim JS, Kim D, Joo YB, Won S, Lee J, Shin J, et al. Factors associated with development and mortality of pulmonary hypertension in systemic lupus erythematosus patients. Lupus. 2018;27(11):1769–77.
Wang J, Wang Y, Li X, Huang Y, Sun X, Wang Q, et al. Serum uric acid is associated with disease severity and may predict clinical outcome in patients of pulmonary arterial hypertension secondary to connective tissue disease in Chinese: a single-center retrospective study. BMC Pulm Med. 2020;20(1):272.
Chow SL, Chandran V, Fazelzad R, Johnson SR. Prognostic factors for survival in systemic lupus erythematosus associated pulmonary hypertension. Lupus. 2012;21(4):353–64.
Cefle A, Inanc M, Sayarlioglu M, Kamali S, Gul A, Ocal L, et al. Pulmonary hypertension in systemic lupus erythematosus: relationship with antiphospholipid antibodies and severe disease outcome. Rheumatol Int. 2011;31(2):183–9.
Magro-Checa C, Kumar S, Ramiro S, Beaart-van DVL, Eikenboom J, Ronen I, et al. Are serum autoantibodies associated with brain changes in systemic lupus erythematosus? MRI data from the Leiden NP-SLE cohort. Lupus. 2019;28(1):94–103.
Huang C, Li M, Liu Y, Wang Q, Guo X, Zhao J, et al. Baseline characteristics and risk factors of pulmonary arterial hypertension in systemic lupus erythematosus patients. Medicine (Baltimore). 2016;95(10): e2761.
Prete M, Fatone MC, Vacca A, Racanelli V, Perosa F. Severe pulmonary hypertension as the initial manifestation of systemic lupus erythematosus: a case report and review of the literature. Clin Exp Rheumatol. 2014;32(2):267–74.
Xia YK, Tu SH, Hu YH, Wang Y, Chen Z, Day HT, et al. Pulmonary hypertension in systemic lupus erythematosus: a systematic review and analysis of 642 cases in Chinese population. Rheumatol Int. 2013;33(5):1211–7.
Prabu A, Patel K, Yee CS, Nightingale P, Situnayake RD, Thickett DR, et al. Prevalence and risk factors for pulmonary arterial hypertension in patients with lupus. Rheumatology (Oxford). 2009;48(12):1506–11.
Tselios K, Gladman DD, Urowitz MB. Systemic lupus erythematosus and pulmonary arterial hypertension: links, risks, and management strategies. Open Access Rheumatol. 2017;9:1–9.
Gronwall C, Akhter E, Oh C, Burlingame RW, Petri M, Silverman GJ. IgM autoantibodies to distinct apoptosis-associated antigens correlate with protection from cardiovascular events and renal disease in patients with SLE. Clin Immunol. 2012;142(3):390–8.
Zheng YG, Yang T, Xiong CM, He JG, Liu ZH, Gu Q, et al. Platelet distribution width and mean platelet volume in idiopathic pulmonary arterial hypertension. Heart Lung Circ. 2015;24(6):566–72.
Chen SY, Du J, Lu XN, Xu JH. Platelet distribution width as a novel indicator of disease activity in systemic lupus erythematosus. J Res Med Sci. 2018;23:48.
He Y, Yu Y, Hu S. Platelet distribution width level in patients with systemic lupus erythematosus-associated pulmonary arterial hypertension and its diagnostic value. Arch Rheumatol. 2020;35(3):394–400.
Sevuk U, Bahadir MV, Altindag R, Baysal E, Yaylak B, Ay N, et al. Value of serial platelet indices measurements for the prediction of pulmonary embolism in patients with deep venous thrombosis. Ther Clin Risk Manag. 2015;11:1243–9.
Vinholt PJ, Hvas AM, Nybo M. An overview of platelet indices and methods for evaluating platelet function in thrombocytopenic patients. Eur J Haematol. 2014;92(5):367–76.
Boilard E, Blanco P, Nigrovic PA. Platelets: active players in the pathogenesis of arthritis and SLE. Nat Rev Rheumatol. 2012;8(9):534–42.
Habets KL, Huizinga TW, Toes RE. Platelets and autoimmunity. Eur J Clin Invest. 2013;43(7):746–57.
Acknowledgements
Thanks to all patients and site staff of the local hospital who participated in this study.
Funding
This work was supported by The Research Project of Medical Science and Technology of Henan Province of China (grant number LHGJ20190260) and The Key R & D Special Project of Henan Province in China (grant number LHGJ20220309 and 212102310754).
Author information
Authors and Affiliations
Contributions
MD, ZY, HS, and YL designed the study, collected the original data and finished the analysis. MD, QW and HY drafted the initial manuscript. ZZ, YZ, CG helped revised the manuscript. YZ, ZZ provided the funding and supervised the study. The final manuscript was read and approved by all authors. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the First Affiliated Hospital of Zhengzhou University (2023-KY-0183–001).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Table S1. Cox proportional hazards assumption test of four prognostic variables. Supplementary Table S2. Comparison of characteristics between survivors and non-survivors in SLE-PAH patients at baseline assessment. Supplementary Table S3. Comparison of RHC parameters between survivors and non-survivors in SLE-PAH patients at baseline assessment. Supplementary Table S4. Comparison between cluster 1 and cluster 2 in SLE-PAH patients at baseline assessment. Supplementary Table S5. Comparison among IPAH, cluster 1 and cluster 2 in SLE-PAH patients at baseline assessment.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dai, M., Zhang, C., Li, C. et al. Clinical characteristics and prognosis in systemic lupus erythematosus-associated pulmonary arterial hypertension based on consensus clustering and risk prediction model. Arthritis Res Ther 25, 155 (2023). https://doi.org/10.1186/s13075-023-03139-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-023-03139-y