Abstract
Background
Clonal haematopoiesis of indeterminate potential (CHIP) is a predisposition to haematological malignancy whose relationship with chronic inflammatory diseases, such as cardiovascular diseases, has been highlighted. Here, we aimed to investigate the CHIP emergence rate and its association with inflammatory markers in Behçet’s disease (BD).
Methods
We performed targeted next-generation sequencing to detect the presence of CHIP using peripheral blood cells from 117 BD patients and 5004 healthy controls between March 2009 and September 2021 and analysed the association between CHIP and inflammatory markers.
Results
CHIP was detected in 13.9% of patients in the control group and 11.1% of patients in the BD group, indicating no significant intergroup difference. Among the BD patients of our cohort, five variants (DNMT3A, TET2, ASXL1, STAG2, and IDH2) were detected. DNMT3A mutations were the most common, followed by TET2 mutations. CHIP carriers with BD had a higher serum platelet count, erythrocyte sedimentation rate, and C-reactive protein level; older age; and lower serum albumin level at diagnosis than non-CHIP carriers with BD. However, the significant association between inflammatory markers and CHIP disappeared after the adjustment for various variables, including age. Moreover, CHIP was not an independent risk factor for poor clinical outcomes in patients with BD.
Conclusions
Although BD patients did not have higher CHIP emergence rates than the general population, older age and degree of inflammation in BD were associated with CHIP emergence.
Similar content being viewed by others
Background
Clonal haematopoiesis of indeterminate potential (CHIP), defined as the presence of somatic mutations and clonal expansion in haematopoietic stem cells of the blood or bone marrow, is a common ageing-associated condition that begins in middle age [1]. CHIP, a variant allele frequency (VAF) exceeding 2%, is not a malignancy but rather a predisposition to haematological malignancy and cardiovascular disease [2, 3]. Furthermore, CHIP could contribute to chronic inflammation; for example, loss of ten eleven translocation-2 (TET2) upregulated inflammatory mediators, such as interleukin-6, in mouse colitis and mouse atherosclerosis models [4, 5].
In contrast, inflammation from pre-existing comorbidities, including autoimmune diseases or infections, can cause mutagenesis via DNA damage and promote CHIP [6]. CHIP was reportedly identified in 17% of rheumatoid arthritis patients and 30.4% of patients with anti-neutrophil cytoplasmic antibody (ANCA)–associated vasculitis [7, 8]. In patients with ulcerative colitis (UC), Zhang et al. identified that 12.8% had CHIP variants and interpreted that patients with UC may show a slightly higher tendency toward a CHIP appearance after the sixth decade compared to the general population [9]. Subpopulations of CHIP with DNMT3A mutations were significantly associated with higher serum interferon-gamma levels [9]. In patients with inflammatory bowel disease co-occurring with haematologic disease, Cumbo et al. identified 85% of CHIP variants and suggested a biological link between the proinflammatory environment and haematologic malignancy onset [10].
Behçet’s disease (BD) is a chronic inflammatory immune-mediated disorder that causes recurrent oral and genital ulcers and skin, joint, eye, neurological, and gastrointestinal involvement [11, 12]. Patients with BD have a higher risk of haematological malignancy (pooled relative risk, 2.58; 95% confidence interval [CI], 1.61–3.55) [13, 14]. However, no studies have investigated the relationship between CHIP and BD. Therefore, here, we aimed to characterise the occurrence of CHIP in patients with BD and analyse the associations between CHIP and inflammatory markers in patients with BD and their outcomes.
Methods
Study design and population
For the control group, we collected blood samples from participants during a routine health check-up for screening purposes at the Seoul National University Hospital Healthcare System Gangnam Center between January 2014 and January 2017 (no. 1980–121-1056). For the BD group, we collected blood samples from patients with BD during routine outpatient visits from two tertiary hospitals (Severance Hospital in Seoul, Korea and Seoul National University Hospital in Seoul, South Korea) between March 2009 and September 2021. Systemic BD was diagnosed based on the International Criteria for Behçet’s Disease [15]. Patients with intestinal BD classified as having definite, probable, or suspected intestinal BD were enrolled in this study based on established diagnostic criteria [16]. This study was conducted in accordance with the ethical guidelines of the Declaration of Helsinki. Informed consent was obtained from all individuals, and the study protocol was approved by the Institutional Review Board of Seoul National University (no. 1606–116-772) and Severance Hospital (no. 2012–0039-030).
Targeted gene sequencing and variant annotation
Genomic DNA was extracted from the peripheral blood. Targeted next-generation sequencing was performed using a custom panel consisting of 89 CHIP genes frequently involved in CHIP, DNMT3A, TET2, ASXL1, JAK2, and TP53, with an average target depth of over 1000 × . All non-synonymous variants with a variant allele frequency of 1.5–30% were considered CHIP variants. Common germline variants listed in the gnomAD,10–0 Genomes v3, ESP6500, and ExAC databases and an internal panel of 1000 Koreans were excluded.
Data collection and study outcomes
Demographic and clinical information was collected at outpatient visits, including age, disease duration, sex, body mass index, smoking history, presence of intestinal BD, previous and current medications, and laboratory findings. Medical accelerations for BD, including immunomodulators and biologic agents, surgical requirements for BD, BD-related hospitalisation, and BD-related emergency room visits, were also investigated to determine the patients’ long-term outcomes.
Statistical analysis
Continuous data are expressed as mean and standard deviation (mean ± SD) or median and range, while categorical variables are expressed as proportion (%). An independent t-test (or Mann–Whitney U test) was used to compare the continuous variables, while the Χ2 test (or Fisher’s exact test) was used for categorical variables as appropriate. Multivariate logistic regression analyses were performed to identify the independent risk factors for CHIP after the adjustment for various confounders. All statistical analyses were assessed with the Statistical Package for Social Sciences (SPSS version 24.0; IBM Corp., Armonk, NY, USA). p values < 0.05 were considered statistically significant.
Results
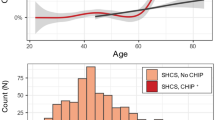
Association between CHIP and BD development
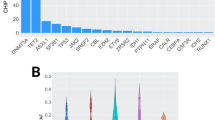
Blood samples were collected from 5004 healthy controls (control group) and 117 BD patients (BD group). We identified CHIP in 13.9% of the control group and 11.1% of the BD group, indicating that there was no significant difference between the two groups (Fig. 1). In patients with BD, five variants (DNMT3A, TET2, ASXL1, STAG2, and IDH2) were detected in our cohort, and DNMT3A mutations were the most common (7.5%), followed by TET2 mutations (1.9%).
CHIP and disease activity of BD
Patients with BD and CHIP were older and had a higher platelet count, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) level and lower albumin level at diagnosis than BD patients without CHIP (Table 1). Patients with a higher baseline ESR showed a higher CHIP-positive tendency than those with a lower baseline ESR (4.0%, 8.0%, 13.3%, and 28.6%, respectively; p trend = 0.067; Fig. 2A). Patients with a higher baseline CRP level showed a significantly higher CHIP-positive rate than those with a lower baseline CRP level (0.0%, 10.0%, 19.2%, and 27.9%, respectively; p trend = 0.015; Fig. 2B). Patients with a higher baseline albumin level showed a significantly lower CHIP-positive rate than those with a lower baseline albumin level (23.8%, 9.4%, 16.0%, and 2.6%, respectively; p trend = 0.035; Fig. 2C). Older patients showed a significantly higher CHIP positivity rate than younger patients (0.0%, 6.5%, 15.4%, and 23.3%, respectively; p trend = 0.003; Fig. 2D).
A univariate logistic analysis was performed to determine independent factors associated with CHIP in patients with BD. Older age at blood sampling (odds ratio [OR], 1.090; 95% CI, 1.030–1.153; p = 0.003), high platelet count at diagnosis (OR, 1.000; 95% CI, 1.000–1.000; p = 0.012), and high ESR at diagnosis (OR, 1.027; 95% CI, 1.009–1.046; p = 0.004) were positively associated with CHIP (Table 2). A high albumin level (OR, 0.228; 95% CI, 0.058–0.887; p = 0.033) was negatively associated with CHIP (Table 2). Age at blood sampling was the only independent factor for CHIP after multivariate logistic analysis including various confounders (OR, 1.099; 95% CI, 1.020–1.184; p = 0.013) (Table 2).
CHIP and long-term clinical outcomes of BD
The development of CHIP in patients with BD was not associated with medical acceleration, surgical requirement, BD-related hospitalisation, or BD-related emergency room visits (Table 1). Moreover, CHIP was not an independent risk factor for poor clinical composite outcomes, including medical acceleration, surgery, hospitalisation, or emergency room visits, in patients with BD, in the Cox regression analysis (data not shown).
There was one patient with aplastic anaemia and two patients with myelodysplastic syndrome in our cohort. However, there was no CHIP mutation in the three patients.
Discussion
To our knowledge, this is the first report to describe the development of CHIP in patients with BD and analysing the association between CHIP and inflammation in BD. We determined that the rate of CHIP in BD patients was not increased compared to the general population. The DNMT3A and TET2 mutations were dominant in the control and BD groups. The CHIP rate significantly increased with age at the time of blood sampling. Furthermore, it was associated with a higher CRP level and ESR but negatively with albumin level at diagnosis. Finally, it was not associated with the clinical outcomes of BD.
Ageing, the strongest risk factor for CHIP development in patients with BD, is widely accepted and considered the biggest contributor to the accumulation of somatic mutations. Its intrinsic mechanisms include haematopoietic stem cell–induced age-dependent DNA damage, telomere attrition, and epigenetic dysregulation involving DNMT3A and TET2 [17]. Interestingly, in addition to intrinsic mechanisms, various environmental stressors such as cytotoxic stress, autoimmunity, and infection contribute to CHIP emergence [18]. Here, we investigated the association between CHIP and elevated levels of inflammatory factors in patients with BD. Although the significance disappeared after the adjustment for age, ESR, CRP, and albumin levels were confirmed as highly correlated with CHIP in patients with BD by univariate logistic regression analysis. Inflammatory markers, including white blood cell and neutrophil counts, ESR, and CRP level, were not elevated in the general population with CHIP in a previous study [19]. However, CHIP carriers have higher CRP levels among patients with prior coronary artery disease [20]. In line with the results of previous studies, our results support the theory that CHIP is regulated by chronic inflammation, reflecting higher serum ESR and CRP and albumin levels in CHIP( +) BD patients. Regarding elevated platelet numbers in CHIP( +) patients, similar results were reported in a previous study (294,000/µL vs. 241,000/µL, p = 0.021) [21]. Regarding long-term clinical outcomes, CHIP could not predict medical acceleration, surgical requirement, BD-related hospitalisation, or BD-related emergency room visits. We appreciate the reviewer’s comment. There were some limitations in our study. First, there was a lack of validation using an independent cohort. Second, this study had low statistical power due to the small number of cases. Third, there is the possibility of other unknown variants associated with BD. We added these issues in the “Discussion” section.
Conclusions
In summary, our study found that older age and degree of inflammation in BD might be associated with CHIP emergence.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ANCA:
-
Anti-neutrophil cytoplasmic antibody
- BD:
-
Behçet’s disease
- CHIP:
-
Clonal haematopoiesis of indeterminate potential
- CI:
-
Confidence interval
- CRP:
-
C-reactive protein
- ESR:
-
Erythrocyte sedimentation rate
- OR:
-
Odds ratio
- TET2 :
-
Ten eleven translocation-2
- UC:
-
Ulcerative colitis
- VAF:
-
Variant allele frequency
References
Jan M, Ebert BL, Jaiswal S. Clonal hematopoiesis. Semin Hematol. 2017;54(1):43–50.
Genovese G, Kahler AK, Handsaker RE, Lindberg J, Rose SA, Bakhoum SF, Chambert K, Mick E, Neale BM, Fromer M, et al. Clonal hematopoiesis and blood-cancer risk inferred from blood DNA sequence. N Engl J Med. 2014;371(26):2477–87.
Jaiswal S, Natarajan P, Silver AJ, Gibson CJ, Bick AG, Shvartz E, McConkey M, Gupta N, Gabriel S, Ardissino D, et al. Clonal hematopoiesis and risk of atherosclerotic cardiovascular disease. N Engl J Med. 2017;377(2):111–21.
Zhang Q, Zhao K, Shen Q, Han Y, Gu Y, Li X, Zhao D, Liu Y, Wang C, Zhang X, et al. Tet2 is required to resolve inflammation by recruiting Hdac2 to specifically repress IL-6. Nature. 2015;525(7569):389–93.
Fuster JJ, MacLauchlan S, Zuriaga MA, Polackal MN, Ostriker AC, Chakraborty R, Wu CL, Sano S, Muralidharan S, Rius C, et al. Clonal hematopoiesis associated with TET2 deficiency accelerates atherosclerosis development in mice. Science. 2017;355(6327):842–7.
Steensma DP. Clinical consequences of clonal hematopoiesis of indeterminate potential. Blood Adv. 2018;2(22):3404–10.
Savola P, Lundgren S, Keranen MAI, Almusa H, Ellonen P, Leirisalo-Repo M, Kelkka T, Mustjoki S. Clonal hematopoiesis in patients with rheumatoid arthritis. Blood Cancer J. 2018;8(8):69.
Arends CM, Weiss M, Christen F, Eulenberg-Gustavus C, Rousselle A, Kettritz R, Eckardt KU, Chan W, Hoyer K, Frick M, et al. Clonal hematopoiesis in patients with anti-neutrophil cytoplasmic antibody-associated vasculitis. Haematologica. 2020;105(6):e264–7.
Zhang CRC, Nix D, Gregory M, Ciorba MA, Ostrander EL, Newberry RD, Spencer DH, Challen GA. Inflammatory cytokines promote clonal hematopoiesis with specific mutations in ulcerative colitis patients. Exp Hematol. 2019;80(36–41):e33.
Cumbo C, Tarantini F, Zagaria A, Anelli L, Minervini CF, Coccaro N, Tota G, Impera L, Parciante E, Conserva MR, et al. Clonal hematopoiesis at the crossroads of inflammatory bowel diseases and hematological malignancies: a biological link? Front Oncol. 2022;12:873896.
Sakane T, Takeno M, Suzuki N, Inaba G. Behcet’s disease. N Engl J Med. 1999;341(17):1284–91.
Suzuki Y, Hagiwara T, Kobayashi M, Morita K, Shimamoto T, Hibi T. Long-term safety and effectiveness of adalimumab in 462 patients with intestinal Behcet’s disease: results from a large real-world observational study. Intest Res. 2021;19(3):301–12.
Wang X, Peng Y, Gao J, Han S, Li Y. Risk of malignancy in Behcet disease: a meta-analysis with systematic review. Medicine (Baltimore). 2019;98(44):e17735.
Mori Y, Iwamoto F, Ishida Y, Kuno T, Kobayashi S, Yoshida T, Yamaguchi T, Sato T, Sudo M, Ichikawa D, et al. Long-term outcome after surgery in a patient with intestinal Behcet’s disease complicated by myelodysplastic syndrome and trisomy 8. Intest Res. 2020;18(4):469–75.
International Team for the Revision of the International Criteria for Behcet’s D. The International Criteria for Behcet’s Disease (ICBD): a collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J Eur Acad Dermatol Venereol. 2014;28(3):338–47.
Cheon JH, Kim ES, Shin SJ, Kim TI, Lee KM, Kim SW, Kim JS, Kim YS, Choi CH, Ye BD, et al. Development and validation of novel diagnostic criteria for intestinal Behcet’s disease in Korean patients with ileocolonic ulcers. Am J Gastroenterol. 2009;104(10):2492–9.
Park SJ, Bejar R. Clonal hematopoiesis in aging. Curr Stem Cell Rep. 2018;4(3):209–19.
Kristinsson SY, Bjorkholm M, Hultcrantz M, Derolf AR, Landgren O, Goldin LR. Chronic immune stimulation might act as a trigger for the development of acute myeloid leukemia or myelodysplastic syndromes. J Clin Oncol. 2011;29(21):2897–903.
Mooney L, Goodyear CS, Chandra T, Kirschner K, Copland M, Petrie MC, Lang NN. Clonal haematopoiesis of indeterminate potential: intersections between inflammation, vascular disease and heart failure. Clin Sci (Lond). 2021;135(7):991–1007.
Busque L, Sun M, Buscarlet M, Ayachi S, Feroz Zada Y, Provost S, Bourgoin V, Mollica L, Meisel M, Hinterleitner R, et al. High-sensitivity C-reactive protein is associated with clonal hematopoiesis of indeterminate potential. Blood Adv. 2020;4(11):2430–8.
Guermouche H, Ravalet N, Gallay N, Deswarte C, Foucault A, Beaud J, Rault E, Saindoy E, Lachot S, Martignoles JA, et al. High prevalence of clonal hematopoiesis in the blood and bone marrow of healthy volunteers. Blood Adv. 2020;4(15):3550–7.
Acknowledgements
This study was supported by a faculty research grant of Yonsei University College of Medicine for 2012 (6-2012-0163).
Funding
None.
Author information
Authors and Affiliations
Contributions
JHP and HGA designed the study, interpreted the data, and wrote the manuscript. JHP, HGA, ISP, MHK, JHK, SWK, and YIK conducted the experiments and analysed the data. EYL and JHC conceived and designed the study, interpreted the data, and critically revised the manuscript for important intellectual content. The authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All patients provided informed consent in accordance with the Declaration of Helsinki guidelines. This study was approved by the ethics committee of the Seoul National University Hospital Healthcare System Gangnam Center (no. 1980–121-1056), Institutional Review Board of Seoul National University (no. 1606–116-772), and Severance Hospital (no. 2012–0039-030).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Park, J., An, H., Lim, J. et al. Interplay between chronic inflammation and clonal haematopoiesis of indeterminate potential in Behçet’s disease. Arthritis Res Ther 25, 33 (2023). https://doi.org/10.1186/s13075-023-03014-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-023-03014-w