Abstract
Osteoarthritis (OA) is mainly characterized by the progressive destruction of articular cartilage. Mounting studies have revealed that disruption of extracellular matrix (ECM) homeostasis, aberrant chondrocyte metabolism, an increase in the number of senescent chondrocytes and abnormal activation of cell death such as chondrocyte apoptosis and autophagy, are the crucial steps in OA development. Additionally, mitochondrial dysfunction also participates in the abovementioned processes and is the key element of OA pathogenesis. Sirtuin (SIRT) is a family of nicotinamide adenine dinucleotide (NAD+)-dependent protein deacetylases that can actively participate and primarily regulate chondrocyte function in OA pathophysiological processes. Some members of the SIRT family located in mitochondria can regulate mitochondrial function and mediate mitochondrial homeostasis via deacetylation to protect chondrocytes. In addition, SIRT can maintain ECM homeostasis, regulate chondrocyte metabolism, inhibit chondrocyte apoptosis and autophagy, and prevent chondrocyte senescence in cartilage by exerting its deacetylation activity. However, the molecular mechanism of the SIRT family against the onset and development of OA remains poorly elucidated. In this review, we will discuss the potential protective role of SIRT in the progression of OA and summarize several sirtuin-activating molecules as well as their potential therapeutic applications for OA.
Similar content being viewed by others
Introduction
Osteoarthritis (OA) is the most common chronic and degenerative joint disease that affects elderly people, causing debilitating pain, mobility loss, and possibly disability, as well as a significant socioeconomic burden [1]. Cartilage degeneration has been identified as a central feature in the progression of OA. Chondrocytes are surrounded by an abundant extracellular matrix (ECM), and as the only cell type existing in cartilage, they are mainly responsible for the maintenance of the surrounding microenvironment and cartilage homeostasis.
Multiple lines of evidence indicate that chondrocyte dysfunction appears to be a crucial factor in the progression of OA [2]. In the early stage of OA, chondrocytes experience a pathological shift, increasing the production of matrix-remodelling enzymes. The synthetic capacity of chondrocytes is overwhelmed by processes that promote matrix breakdown, contributing to cartilage degradation. Moreover, the progression of OA is also attributed to abnormal chondrocyte metabolism, and emerging evidence has revealed that OA and other metabolic diseases have common pathways, including lipid metabolism [3, 4]. Recent studies have demonstrated that abnormal lipid accumulation is connected with cartilage degradation [5]. In addition, chondrocyte death is an important contributor to OA development. The senescence of chondrocytes also increases with age, resulting in diminished cellular proliferation and tissue regeneration.
Unlike many other well-vascularized tissues with higher levels of oxygenation, chondrocytes surround the lower oxygen environment. The evidence indicated that reactive oxygen species (ROS), which are a major cause of oxidative stress, were overproduced in chondrocytes in end-stage OA cartilage [6]. Mitochondrial quality control could participate in the clearance of ROS and prevent mitochondrial dysfunction through mitochondrial biogenesis, mitophagy, dynamics, mitochondrial redox and the newly discovered mitocytosis [7,8,9]. Mitochondrial dysfunction also causes chondrocyte apoptosis and autophagy, both of which contribute to cartilage degradation [4, 10, 11]. Therefore, mitochondrial function plays an important role in maintaining the homeostasis of chondrocytes.
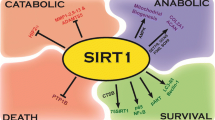
Sirtuin (SIRT) is a group of nicotinamide adenine dinucleotide-dependent histone deacetylases that can deacetylate certain proteins and play a key role in the regulation of cell physiological and pathological processes. Of the seven SIRTs, mammalian class III histone deacetylases, sirtuin 1 (SIRT1) is localized in the nucleus and cytoplasm, sirtuin 2 (SIRT2) is present in the cytoplasm; sirtuin 3 (SIRT3), sirtuin 4 (SIRT4), and sirtuin 5 (SIRT5) have a primary mitochondrial localization; and sirtuin 6 (SIRT6) and sirtuin 7 (SIRT7) are primarily found in the nucleus. In addition to deacetylase activity, the SIRT family has many functions such as demalonylase, desuccinylase, deglutarylase activity and ADP-ribosylation. For example, SIRT3-5 can lead to ADP-ribosylation, SIRT5 has strong demalonylase and desuccinylase activity, and SIRT7 plays a role in the deglutarylase activity [12,13,14].
Extensive studies have revealed that some sirtuin-activating molecules have beneficial effects on encouraging chondrocyte survival in cartilage and show promising early results for treating OA [15]. However, evidence of the benefit is currently limited by a lack of evidence testing the specificity and efficacy of these drugs. This review aims to explore the molecular mechanisms related to SIRT during the progression of OA and summarize potential therapeutic strategies targeting SIRT directly.
Accumulating evidence has recently documented that the functional impairment of chondrocytes, which hardly maintain homeostasis in response to changing stress conditions, is a crucial factor in the pathophysiology of OA [2]. The SIRT family was reported to maintain chondrocyte function by maintaining ECM homeostasis, regulating chondrocyte metabolism, preventing chondrocyte senescence, decreasing chondrocyte apoptosis and enhancing chondrocyte autophagy (Fig. 1). Mounting evidence suggests that mitochondrial dysfunction may play a role in the onset of ageing and degenerative diseases such as OA [4, 10, 16, 17]. SIRT plays a regulatory role in mediating chondrocyte mitochondrial quality control and protecting against the progression of OA (Fig. 2).
The role of the SIRT family in maintaining chondrocyte function. A SIRT in maintaining ECM homeostasis. B SIRT in regulating chondrocyte metabolism. C SIRT in preventing chondrocyte senescence. D SIRT in decreasing chondrocyte apoptosis and enhancing chondrocyte autophagy. Abbreviations: SIRT, sirtuins; SIRT1, sirtuin 1; SIRT2, sirtuin 2; SIRT3, sirtuin 3; SIRT4, sirtuin 4; SIRT5, sirtuin 5; SIRT6, sirtuin 6; SIRT7, sirtuin 7; ECM, extracellular matrix; Col2, type 2 collagen; HA, hyaluronan; MMP-13, matrix metalloproteinase-13; SOX9, SRY-Box transcription factor 9; FOXO4, forkhead box O-4; HAS2, hyaluronan synthase 2; Runx2, Runt-Related Transcription Factor 2; NAMPT, nicotinamide phosphoribosyltransferase; HIF-2α, hypoxia-inducible factor-2α; LOX-1, lectin-like oxidized low-density lipoprotein receptor-1; NF-κB, nuclear factor-κB; Mak, protein lysine malonylation; IL-1β, interleukin-1β; IL-6, interleukin-6; IL-8, interleukin-8; Bcl-2, B-cell lymphoma-2; Bax, Bcl-2-associated X; ER, endoplasmic reticulum; mTOR, mammalian target of rapamycin; PI3K, phosphoinositide 3-kinase; Akt, protein kinase B; NAD + , nicotinamide adenine dinucleotide; p-AMPK, phospho-adenosine monophosphate-activated protein kinase; MFN2, mitofusin-2; FOXO1, forkhead box O-1; ATGs, autophagy-related proteins
The role of the SIRT family in mediating mitochondrial quality control in chondrocytes. SIRT1 can deacetylate PGC-1α, and then coactivate the transcription of NRF-1 or NRF-2, enhancing TFAM expression, which this process promotes mitochondrial biogenesis. SIRT3 could deacetylate OPA1 to promote mitochondrial dynamics, deacetylate Parkin to contribute to mitophagy, and elevate the level of GSH to reduce ROS to maintain mitochondrial homeostasis in chondrocytes. Abbreviations: SIRT, sirtuins; SIRT1, sirtuin 1; SIRT3, sirtuin 3; SIRT6, sirtuin 6; p-AMPK, phospho-adenosine monophosphate-activated protein kinase; PGC-1α, peroxisome proliferator-activated receptor Coactivator-1α; NRF-1, nuclear respiratory factor 1; NRF-2, nuclear respiratory factor 2; TFAM, mitochondrial transcription factor A; NAD+, nicotinamide adenine dinucleotide; OPA1, optic atrophy-1; MFN1, mitofusin-1; MFN2, mitofusin-2; DRP1, dynamin-related protein 1; PINK1:, PTEN-induced putative kinase-1; GSH, glutathione; ROS, reactive oxygen species
The role of SIRT1, SIRT2, SIRT4, SIRT6 and SIRT7 in maintaining ECM homeostasis in OA
Disruption of ECM homeostasis is one of the key elements of OA progression. Sirtuin 1 (SIRT1) is critical in maintaining cartilage health by promoting ECM homeostasis in the regulation of the expression of ECM-related proteins. The inhibition of SIRT1 may reduce the expression of hyaluronan synthase 2 (HAS2), which, in turn, downregulates hyaluronan (HA) production [18, 19]. The reduction in HA contributes to the progression of OA. SIRT1 modulates matrix metalloproteinase 13 (MMP-13) production from chondrocytes in OA by regulating the expression of Runt-Related Transcription Factor 2 (Runx2), a promotor of MMP-13 expression [20]. On the other hand, Oh, H. et al. demonstrated that the reciprocal control of the hypoxia-inducible factor-2α (HIF-2α) and nicotinamide phosphoribosyltransferase (NAMPT)-SIRT2 pathways are required for the development of catabolic matrix metalloproteinases such as MMP-13 [21]. Moreover, SIRT1 can deacetylate forkhead box O-4 (FOXO4) and then activate SRY-Box transcription factor 9 (SOX9), which can control the expression of cartilage-specific genes, allowing cartilage to maintain its ECM homeostasis [22]. In contrast, SIRT7 appears to inhibit the transcriptional activity of SOX9. Korogi, W et. al. demonstrated that inhibition of SIRT7 increased the mRNA expression of ECM components such as collagen II and aggrecan in chondrocytes [23].
Oxidative stress has been proposed as a driver of the catabolic and anabolic signalling imbalance in cartilage that results in progressive matrix degradation. Dai, Y. et al. revealed that silencing SIRT4 induced healthy chondrocytes to downregulate aggrecan, collagen II and antioxidant enzymes, while overexpression of SIRT4 suppressed the inflammatory response and reduced oxidative stress [24]. Collins, J. An et al. demonstrated that overexpression of SIRT6 decreased catabolic signal pathways such as oxidative stress-induced accumulation of nuclear phosphorylated p65 [25].
The role of SIRT1 and SIRT5 in regulating chondrocyte metabolism in OA
The metabolic alteration of chondrocytes was reported to be another pathological factor in OA progression. When exposed to environmental stress, chondrocytes tend to change metabolic pathways involved in enhanced anaerobic glycolysis and alter lipid and amino acid metabolism [2]. At the molecular level, metabolic dysregulation in OA was linked to decreased SIRT activity. For instance, SIRT1 enhances catabolic activity and fatty acid oxidation. Papageorgiou et al. revealed that SIRT1 activated by resveratrol regulated lipid homeostasis in late-stage OA by decreasing the expression of lectin-like oxidized low-density lipoprotein receptor-1 (LOX-1) via nuclear factor-κB (NF-κB) deacetylation [26]. SIRT5 has been also proposed to regulate chondrocyte metabolism, including amino acid metabolism, the tricarboxylic acid cycle (TCA) cycle and glycolysis, and the SIRT5-mediated protein lysine malonylation (Mak) pathway was proven to regulate chondrocyte cellular metabolism in obesity-associated OA development [27]. The deletion of SIRT5 leads to an increase in the level of posttranslationally modified hundreds of metabolic proteins in cartilage, and it is possible to promote the early OA-like phenotype [28].
The role of SIRT1 and SIRT6 in preventing chondrocyte senescence in OA
Chondrocyte senescence is thought to play a crucial role in the onset of cartilage breakdown and the progression of OA. Senescence is a process in which damaged cells enter permanent cell cycle arrest and avoid apoptosis while also transforming their secretory activity into the senescence-associated secretory phenotype (SASP) [29]. The quantity of senescent chondrocytes grows with age and leads to osteoarthritis; however, removing senescent cells from articular cartilage can help prevent OA. Recent studies have shown that SIRT exerts a beneficial effect to protect chondrocytes from senescence by increasing cartilage-specific gene expression and inhibiting apoptosis.
SIRT1 has been revealed to play a role in preventing the onset of chondrocyte senescence. For example, SIRT1 suppresses the expression of SASP factors such as interleukin-6 (IL-6), interleukin-8 (IL-8) and interleukin-1β (IL-1β) [29]. Loss of SIRT1 in cartilage causes the acceleration of OA progression by aberrantly activating the p53/p21-mediated SASP [30].
SIRT6 suppression resulted in an accumulation of DNA damage and telomere dysfunction, eventually leading to cellular senescence, strongly suggesting that SIRT6 is involved in chondrocyte senescence regulation. Nagai, K et al. revealed that SIRT6 prevented premature senescence in human chondrocytes by coordinating DNA repair and preserving appropriate telomere function [31]. Several studies have also supported the idea that SIRT6 promotes DNA repair under stress and protects against telomere dysfunction through deacetylation [32]. Zhao et al. showed that Sirt6 inhibited the acetylation of p27, which is highly acetylated with a prolonged half-life during cellular senescence, leading to its degradation via the ubiquitin–proteasome pathway and postponing cellular senescence [33]. Moreover, Wu, Y et al. found that the level of SIRT6 in chondrocytes of OA patients was much lower than that in normal individuals and that overexpression of SIRT6 can slow the progression of OA by reducing chondrocyte senescence [34].
The role of SIRT1, SIRT2 and SIRT3 in decreasing chondrocyte apoptosis and enhancing autophagy in OA
A growing body of evidence implies that chondrocyte apoptosis plays a role in articular cartilage degradation. With OA development, the synthetic capabilities of articular chondrocytes are gradually overwhelmed by excessive chondrocyte apoptosis.
SIRT1 regulates apoptosis in human chondrocytes by modulating mitochondria-related apoptotic signals through B-cell lymphoma-2 (Bcl-2) and Bcl-2-associated X (Bax) translocation [35]. When the expression of SIRT1 is suppressed, the acetylation of p53 is increased, leading to dysregulation of the downstream genes Bax and Bcl-2 [36]. The aberrant activation of p53 induced by acetylation-mediated senescence is associated with a secretory phenotype, hypertrophy and apoptosis, accelerating the progression of OA [30]. When SIRT1 was increased by resveratrol, p53 was decreased, leading to alleviation of OA progression [37].
Endoplasmic reticulum (ER) stress is one of the mechanisms that mediate chondrocyte apoptosis, and it severely affects the secretory activity of chondrocytes, resulting in disordered cartilage homeostasis [38]. One of the major functions of activating SIRT is targeting ER stress, thereby reducing the death of chondrocytes. Activating the SIRT1/adenosine monophosphate-activated protein kinase (AMPK) signalling pathway may reduce chondrocyte apoptosis in the knee joints by inhibiting ER stress. Furthermore, Liu, M et al. demonstrated that mitofusin-2 (MFN2) overexpression, which was activated via the AMPK/SIRT3 signalling pathway, improved mitochondrial fusion in cells, followed by improved mitophagy and increased mitochondrial membrane potential, resulting in the prevention of mitochondria-mediated apoptosis [39]. In addition, Xu, K et al. stated that the overexpression of SIRT3 reduced chondrocyte apoptosis by blocking the phosphatidylinositol-3-kinase (PI3K)/protein kinase B (PKB/AKT)/mammalian target of rapamycin (mTOR) signalling pathway and then attenuated the extent of chondrocyte degeneration [40].
There is significant evidence suggesting that enhancing autophagy in chondrocytes can help slow the progression of OA. As the autophagy initiator primarily in the nucleus, SIRT1 can regulate the binding of transcription factors to promoter regions of the autophagy gene [41]. In addition, SIRT2 can promote the activation of autophagy by deacetylating forkhead box O-1 (FOXO1), which regulates the fusion of autophagosomes and lysosomes by interacting directly with autophagy-related proteins (ATGs) [42]. Once stress stimulates the separation of SIRT1 and SIRT2 from their substrate FOXO1, the acetylation of FOXO1 considerably increases, resulting in decreased autophagy.
The role of SIRT1, SIRT3 and SIRT6 in regulating mitochondrial dysfunction in OA
The role of SIRT1 and SIRT3 in promoting mitochondrial biogenesis in OA
In human OA chondrocytes, mitochondrial biogenesis is impaired which promotes chondrocyte procatabolic responses. Activation of the SIRT1- peroxisome proliferator-activated receptor-γ coactivator-1α (PGC-1α) pathway increases mitochondrial biogenesis in chondrocytes, thus slowing the progression of OA. The SIRT1-PGC1α pathway can lead to the stimulation of mitochondrial gene expression [43]. SIRT1 deficiency inhibits mitochondrial biogenesis, resulting in a decrease in mitochondrial function [44]. In general, the localization of PGC-1α in the nucleus was transformed when acetylated, and thus transcriptional activity was inhibited. In chondrocytes, activation of AMPK increases nuclear PGC-1α/nuclear respiratory factor 1 (NRF-1) /nuclear respiratory factor 2 (NRF-2) expression and promotes mitochondrial transcription factor A (TFAM) transport, which promotes the replication of mitochondrial DNA (mtDNA) and gene expression [45].
Additionally, overexpression of SIRT-3 stimulated mitochondrial biogenesis. In human chondrocytes, after being activated by AMPK, SIRT-3 reduced mtDNA4977 deletion and maintained mtDNA integrity [15]. When SIRT3 was silenced using siRNA in rat cardiomyoblasts (H9C2 cells), the acetylation status of TFAM was increased, corresponding to a decrease in mtDNA binding activity of TFAM and reducing transcription of mitochondrial DNA-encoded genes [46]. Further research is needed to verify whether SIRT3 directly targets TFAM in chondrocytes.
The role of SIRT1 and SIRT3 in regulating mitochondrial dynamics in OA
Mitochondrial dynamics is a network of dynamic processes to adapt to the cell cycle, involving mitochondrial fusion and fission. Fusion creates a more linked mitochondrial network that improves communication with the ER, while fission produces smaller and more distinct mitochondria that generate more ROS and promote mitophagy, two processes that are both mediated by guanosine triphosphatase (GTPase).
Mitochondrial fusion allows matrix content to permeate throughout mitochondria, reducing the number of mitochondrial DNA mutations and oxidized proteins. This process is facilitated by optic atrophy-1 (OPA1) in the inner mitochondrial membrane, as well as mitofusin-1 (MFN1) and MFN2 in the outer mitochondrial membrane [47]. Enhancing the expression of OPA1 can promote mitochondrial fusion in chondrocytes [48]. In addition, Xu, L et al. indicated that elevated MFN2 contributes to metabolic changes and inflammation in rat chondrocytes, whereas decreased MFN2 reduces inflammation and slows OA progression [49]. SIRT3 contributes to promoting mitochondrial function by regulating mitochondrial dynamics by deacetylating OPA1 and elevating its GTPase activity [7]. In human articular chondrocytes, SIRT3 regulates mitochondrial dynamics by deacetylating and activating OPA1 to reduce chondrocyte apoptosis [50].
Mitochondrial fission is mediated by dynamin-related protein 1 (DRP1), which translocates to the outer mitochondrial membrane and forms a ring-like structure once activated to constrict and divide mitochondria [51]. Under disease conditions, the process of mitochondrial fission enhances the removal of damaged mitochondria, which promotes apoptotic programs [17]. Ding, M et al. indicated that the expression of SIRT1 negatively regulates DRP1-mediated mitochondrial fission directly via the SIRT1/PGC-1α-dependent pathway in H9C2 cells [52]. However, there have been no studies on chondrocytes, and it will be of great interest to explore the distinct functional roles of SIRT in mitochondrial fission in chondrocytes.
The role of SIRT3 in contributing to mitophagy in OA
Mitophagy may protect chondrocytes from oxidative stress by removing damaged and dysfunctional mitochondria. Mitophagy impairment causes the progressive accumulation of defective mitochondria, resulting in cartilage degeneration and OA. Parkin-mediated mitophagy is a key mechanism for clearing damaged mitochondria and improving OA chondrocyte survival [53]. PTEN-induced putative kinase-1 (PINK1), which is linked to the functional and health statuses of mitochondria, usually accumulates on the outer membrane of damaged mitochondria to recruit and activate Parkin. Parkin ubiquitinates and specifically incorporates a wide range of outer mitochondrial membrane proteins into mitophagy.
The SIRT family has recently been discovered to play a significant role in the removal of damaged mitochondria via mitophagy [43]. SIRT3 activated by metformin can reduce oxidative stress and rectify the imbalance of anabolism and catabolism induced by IL-1β via the PINK-1/Parkin signalling pathway in chondrocytes [54]. Polletta, L et al. observed that mitophagy increased in SIRT5-silenced cells and found that SIRT5 also controls mitophagy by controlling glutamine metabolism [55]. This result suggested that SIRT5 might also be a potential regulator of mitophagy, but this hypothesis needs further confirmation in OA.
The role of SIRT3 and SIRT6 in maintaining mitochondrial redox homeostasis in OA
Mitochondrial dysfunction increases the accumulation of ROS. Excessive generation of ROS can compromise the integrity and repair capacity of mtDNA, leading to an increase in mitochondrial ROS levels and increased oxidative damage. ROS were overproduced in OA cartilage due to oxidative stress more than in healthy cartilage. However, some SIRTs can maintain mitochondrial redox homeostasis and protect against mitochondrial oxidative damage by regulating the deacetylation of downstream related proteins, playing a pivotal role in mitochondrial function.
SIRT3 was proven to be a crucial regulator of promoting resistance to oxidative stress and maintaining glutathione (GSH) redox homeostasis in chondrocytes [56]. Zhu, S et al. found that SIRT3 deficiency delayed the rate of increasing glutathione content and GSH:oxidized glutathione (GSSG) ratio under oxidative stress in OA-related models [56]. Collins, J. An et al. demonstrated that enhancement of SIRT6 contributed to chondrocyte redox homeostasis by regulating antioxidant proteins of the peroxiredoxin catalytic cycle [25].
Potential therapeutic strategies for OA-targeted SIRT
Currently, some exosome cargos, such as noncoding RNAs (ncRNAs) and proteins, have been reported to deliver multiple bioactive molecules to regulate cartilage behaviour, and are promising candidates for OA treatment [57]. Recent findings suggested that targeting SIRT may be a promising approach for OA therapy (Table 1).
Inhibiting ER stress-induced chondrocyte apoptosis by activating SIRT1 may reduce cartilage degradation in OA [38]. In a rat OA model, Feng, K et al. discovered that quercetin and curcumin may reduce articular cartilage degradation and block chondrocyte apoptosis by reducing the ER stress response through SIRT1 activation [58, 59]. Additionally, safflower yellow can attenuate ER stress by activating the SIRT1/AMPK signalling pathway, thereby protecting chondrocytes and inhibiting inflammation, which suggests that targeting SIRT1 appears to be a viable treatment for OA [60].
In addition, SIRT1 also positively affects the ability of chondrocytes to synthesize ECM [18]. Wu, W. T et al. found that silymarin could improve ECM homeostasis through activation of SIRT1; thus, it may be a potential therapy for early-stage knee OA [61]. In addition, Jiang, C et al. showed that cyanidin may be able to delay the degradation of ECM by modulating the SIRT6/NF-κB signalling axis and ameliorating the progression of OA. [62].
Accumulating evidence has recently shown that cyanidin regulates a variety of mitochondrial proteins in chondrocytes to maintain mitochondrial homeostasis [7]. Wang, F. S et al. revealed that irisin retained mitochondrial biogenesis and attenuated mitophagy in IL-1β-induced inflamed chondrocytes by promoting SIRT3 signalling [50]. Wang, J et al. showed that dihydromyricetin protects rat chondrocytes from TNF-induced cartilage degradation by preserving mitochondrial homeostasis and activating SIRT3 [63]. Furthermore, Wang, C et al. also suggested that metformin could enhance SIRT3-mediated PINK1/Parkin-dependent mitophagy in chondrocytes, leading to suppression of IL-1β-induced OA-like inflammatory changes [54].
Inhibition of oxidative stress and the inflammatory response is a promising approach for OA prevention. In response to oxidative stress conditions, D'Adamo, S et al. implicated that hydroxytyrosol (HT) could regulate the level of microRNA-9 by targeting SIRT1, leading to the protective action of chondrocytes [64]. Furthermore, Zhi, L. Q et al. proposed that HT may reduce chondrocyte inflammatory responses via SIRT6-mediated autophagy [65].
Conclusion
With the precise mechanisms partly elucidated in recent studies, SIRT may represent good candidates for the treatment of OA. SIRT is essential for maintaining cartilage homeostasis by regulating ECM homeostasis and chondrocyte metabolism, preventing chondrocyte senescence, decreasing chondrocyte apoptosis and enhancing chondrocyte autophagy. In addition, SIRT can deacetylate a range of targets in the regulation of mitochondrial function in mitochondrial biogenesis, mitophagy, mitochondrial dynamics and antioxidant pathways. Furthermore, recent studies have revealed that many sirtuin-activating molecules may have beneficial effects on chondrocyte survival and cartilage anabolism. Several small-molecule effectors targeting SIRT are promising in clinical trials and preclinical assessments of OA. However, the progression of treatment for OA from the laboratory to the clinic needs additional investigation, which should specifically focus on SIRT and the related molecular pathways in the future.
Availability of data and materials
Not applicable.
Abbreviations
- OA:
-
Osteoarthritis
- ECM:
-
Extracellular matrix
- ROS:
-
Reactive oxygen species
- SIRT:
-
Sirtuins
- SIRT1:
-
Sirtuin 1
- SIRT2:
-
Sirtuin 2
- SIRT3:
-
Sirtuin 3
- SIRT4:
-
Sirtuin 4
- SIRT5:
-
Sirtuin 5
- SIRT6:
-
Sirtuin 6
- SIRT7:
-
Sirtuin 7
- HAS2:
-
Hyaluronan synthase 2
- HA:
-
Hyaluronan
- MMP-13:
-
Matrix metalloproteinase 13
- Runx2:
-
Runt-Related Transcription Factor 2
- HIF-2α:
-
Hypoxia-inducible factor-2α
- NAMPT:
-
Nicotinamide phosphoribosyltransferase
- FOXO4:
-
Forkhead box O-4
- SOX9:
-
SRY-Box transcription factor 9
- LOX-1:
-
Lectin-like oxidized low-density lipoprotein receptor-1
- NF-κB:
-
Nuclear factor-κB
- TCA:
-
Tricarboxylic acid cycle
- Mak:
-
Protein lysine malonylation
- SASP:
-
Senescence-associated secretory phenotype
- IL-6:
-
Interleukin-6
- IL-8:
-
Interleukin-8
- IL-1β:
-
Interleukin-1β
- Bcl-2:
-
Genes B-cell lymphoma-2
- Bax:
-
Bcl-2-associated X
- ER:
-
Endoplasmic reticulum
- AMPK:
-
Adenosine monophosphate-activated protein kinase
- MFN2:
-
Mitofusin-2
- PI3K:
-
Phosphatidylinositol-3-kinase
- PKB/AKT:
-
Protein kinase B
- mTOR:
-
Mammalian target of rapamycin
- FOXO1:
-
Forkhead box O-1
- ATG:
-
Autophagy-related proteins
- PGC-1α:
-
Peroxisome proliferator-activated receptor-γ coactivator-1α
- NRF-1:
-
Nuclear respiratory factor 1
- NRF-2:
-
Nuclear respiratory factor 2
- TFAM:
-
Mitochondrial transcription factor A
- mtDNA:
-
Mitochondrial DNA
- GTPase:
-
Guanosine triphosphatase
- OPA1:
-
Optic atrophy-1
- MFN1:
-
Mitofusin-1
- DRP1:
-
Dynamin-related protein 1
- PINK1:
-
PTEN-induced putative kinase-1
- GSH:
-
Glutathione
- GSSG:
-
Oxidized glutathione
- HT:
-
Hydroxytyrosol
References
Martel-Pelletier J, Barr AJ, Cicuttini FM, et al. Osteoarthritis Nat Rev Dis Primers. 2016;2:16072. https://doi.org/10.1038/nrdp.2016.72[publishedOnlineFirst:2016/10/14].
Zheng L, Zhang Z, Sheng P, et al. The role of metabolism in chondrocyte dysfunction and the progression of osteoarthritis. Ageing Res Rev. 2021;66: 101249. https://doi.org/10.1016/j.arr.2020.101249[publishedOnlineFirst:2021/01/01].
Courties A, Sellam J, Berenbaum F. Metabolic syndrome-associated osteoarthritis. Curr Opin Rheumatol. 2017;29(2):214–22. https://doi.org/10.1097/bor.0000000000000373[publishedOnlineFirst:2017/01/11].
Blanco FJ, June RK 2nd. Cartilage metabolism, mitochondria, and osteoarthritis. J Am Acad Orthop Surg. 2020;28(6):e242–4. https://doi.org/10.5435/jaaos-d-19-00442[publishedOnlineFirst:2019/11/07].
Papathanasiou I, Anastasopoulou L, Tsezou A. Cholesterol metabolism related genes in osteoarthritis. Bone. 2021;152: 116076. https://doi.org/10.1016/j.bone.2021.116076[publishedOnlineFirst:2021/06/27].
Ansari MY, Ahmad N, Haqqi TM. Oxidative stress and inflammation in osteoarthritis pathogenesis: Role of polyphenols. Biomed Pharmacother. 2020;129: 110452. https://doi.org/10.1016/j.biopha.2020.110452[publishedOnlineFirst:2020/08/10].
Chen Y, Wu YY, Si HB, et al. Mechanistic insights into AMPK-SIRT3 positive feedback loop-mediated chondrocyte mitochondrial quality control in osteoarthritis pathogenesis. Pharmacol Res. 2021;166: 105497. https://doi.org/10.1016/j.phrs.2021.105497[publishedOnlineFirst:2021/02/21].
Liu D, Cai ZJ, Yang YT, et al. Mitochondrial quality control in cartilage damage and osteoarthritis: new insights and potential therapeutic targets. Osteoarthritis Cartilage. 2022;30(3):395–405. https://doi.org/10.1016/j.joca.2021.10.009[publishedOnlineFirst:2021/10/30].
Jiao H, Jiang D, Hu X, et al. Mitocytosis, a migrasome-mediated mitochondrial quality-control process. Cell. 2021;184(11):2896-910.e13. https://doi.org/10.1016/j.cell.2021.04.027[publishedOnlineFirst:2021/05/29].
Habiballa L, Salmonowicz H, Passos JF. Mitochondria and cellular senescence: Implications for musculoskeletal ageing. Free Radic Biol Med. 2019;132:3–10. https://doi.org/10.1016/j.freeradbiomed.2018.10.417[publishedOnlineFirst:2018/10/20].
Ansari MY, Ahmad N, Voleti S, et al. Mitochondrial dysfunction triggers a catabolic response in chondrocytes via ROS-mediated activation of the JNK/AP1 pathway. J Cell Sci 2020;133(22) doi: https://doi.org/10.1242/jcs.247353 [published Online First: 2020/10/25]
Du J, Zhou Y, Su X, et al. Sirt5 is a NAD-dependent protein lysine demalonylase and desuccinylase. Science. 2011;334(6057):806–9. https://doi.org/10.1126/science.1207861[publishedOnlineFirst:2011/11/15].
Di Emidio G, Falone S, Artini PG, et al. Mitochondrial Sirtuins in Reproduction. Antioxidants (Basel) 2021;10(7) doi: https://doi.org/10.3390/antiox10071047 [published Online First: 2021/07/03]
Bao X, Liu Z, Zhang W, et al. Glutarylation of Histone H4 Lysine 91 Regulates Chromatin Dynamics. Mol Cell. 2019;76(4):660-75.e9. https://doi.org/10.1016/j.molcel.2019.08.018[publishedOnlineFirst:2019/09/23].
Chen LY, Wang Y, Terkeltaub R, et al. Activation of AMPK-SIRT3 signaling is chondroprotective by preserving mitochondrial DNA integrity and function. Osteoarthritis Cartilage. 2018;26(11):1539–50. https://doi.org/10.1016/j.joca.2018.07.004[publishedOnlineFirst:2018/07/23].
Coleman MC, Goetz JE, Brouillette MJ, et al. Targeting mitochondrial responses to intra-articular fracture to prevent posttraumatic osteoarthritis. Sci Transl Med 2018;10(427) doi: https://doi.org/10.1126/scitranslmed.aan5372 [published Online First: 2018/02/14]
Ansari MY, Novak K, Haqqi TM. ERK1/2-mediated activation of DRP1 regulates mitochondrial dynamics and apoptosis in chondrocytes. Osteoarthritis Cartilage. 2022;30(2):315–28. https://doi.org/10.1016/j.joca.2021.11.003[publishedOnlineFirst:2021/11/13].
Caon I, Parnigoni A, Viola M, et al. Cell Energy Metabolism and Hyaluronan Synthesis. J Histochem Cytochem. 2021;69(1):35–47. https://doi.org/10.1369/0022155420929772[publishedOnlineFirst:2020/07/07].
Han N, Wang Z, Li X. Melatonin alleviates d-galactose-decreased hyaluronic acid production in synovial membrane cells via Sirt1 signalling. Cell Biochem Funct. 2021;39(4):488–95. https://doi.org/10.1002/cbf.3613[publishedOnlineFirst:2021/01/13].
Terauchi K, Kobayashi H, Yatabe K, et al. The NAD-Dependent Deacetylase Sirtuin-1 Regulates the Expression of Osteogenic Transcriptional Activator Runt-Related Transcription Factor 2 (Runx2) and Production of Matrix Metalloproteinase (MMP)-13 in Chondrocytes in Osteoarthritis. Int J Mol Sci 2016;17(7) doi: https://doi.org/10.3390/ijms17071019 [published Online First: 2016/07/02]
Oh H, Kwak JS, Yang S, et al. Reciprocal regulation by hypoxia-inducible factor-2α and the NAMPT-NAD(+)-SIRT axis in articular chondrocytes is involved in osteoarthritis. Osteoarthritis Cartilage. 2015;23(12):2288–96. https://doi.org/10.1016/j.joca.2015.07.009[publishedOnlineFirst:2015/07/27].
Ma ZX, Xu H, Xiang W, et al. Deacetylation of FOXO4 by Sirt1 stabilizes chondrocyte extracellular matrix upon activating SOX9. Eur Rev Med Pharmacol Sci. 2021;25(2):626–35. https://doi.org/10.26355/eurrev_202101_24621[publishedOnlineFirst:2021/02/13].
Korogi W, Yoshizawa T, Karim MF, et al. SIRT7 is an important regulator of cartilage homeostasis and osteoarthritis development. Biochem Biophys Res Commun. 2018. https://doi.org/10.1016/j.bbrc.2018.01.129[publishedOnlineFirst:2018/02/07].
Dai Y, Liu S, Li J, et al. SIRT4 suppresses the inflammatory response and oxidative stress in osteoarthritis. Am J Transl Res 2020;12(5):1965–75. [published Online First: 2020/06/09]
Collins JA, Kapustina M, Bolduc JA, et al. Sirtuin 6 (SIRT6) regulates redox homeostasis and signaling events in human articular chondrocytes. Free Radic Biol Med. 2021;166:90–103. https://doi.org/10.1016/j.freeradbiomed.2021.01.054[publishedOnlineFirst:2021/02/19].
Papageorgiou AA, Goutas A, Trachana V, et al. Dual Role of SIRT1 in Autophagy and Lipid Metabolism Regulation in Osteoarthritic Chondrocytes. Medicina (Kaunas) 2021;57(11) doi: https://doi.org/10.3390/medicina57111203 [published Online First: 2021/11/28]
Zhu S, Batushansky A, Jopkiewicz A, et al. Sirt5 Deficiency Causes Posttranslational Protein Malonylation and Dysregulated Cellular Metabolism in Chondrocytes Under Obesity Conditions. Cartilage 2021;13(2_suppl):1185s-99s. doi: https://doi.org/10.1177/1947603521993209 [published Online First: 2021/02/12]
Liu H, Rosol TJ, Sathiaseelan R, et al. Cellular carbon stress is a mediator of obesity-associated osteoarthritis development. Osteoarthritis Cartilage. 2021;29(9):1346–50. https://doi.org/10.1016/j.joca.2021.04.016[publishedOnlineFirst:2021/05/14].
Coryell PR, Diekman BO, Loeser RF. Mechanisms and therapeutic implications of cellular senescence in osteoarthritis. Nat Rev Rheumatol. 2021;17(1):47–57. https://doi.org/10.1038/s41584-020-00533-7[publishedOnlineFirst:2020/11/20].
Xu M, Feng M, Peng H, et al. Epigenetic regulation of chondrocyte hypertrophy and apoptosis through Sirt1/P53/P21 pathway in surgery-induced osteoarthritis. Biochem Biophys Res Commun. 2020;528(1):179–85. https://doi.org/10.1016/j.bbrc.2020.04.097[publishedOnlineFirst:2020/06/06].
Nagai K, Matsushita T, Matsuzaki T, et al. Depletion of SIRT6 causes cellular senescence, DNA damage, and telomere dysfunction in human chondrocytes. Osteoarthritis Cartilage. 2015;23(8):1412–20. https://doi.org/10.1016/j.joca.2015.03.024[publishedOnlineFirst:2015/03/31].
Kawahara TL, Michishita E, Adler AS, et al. SIRT6 links histone H3 lysine 9 deacetylation to NF-kappaB-dependent gene expression and organismal life span. Cell. 2009;136(1):62–74. https://doi.org/10.1016/j.cell.2008.10.052[publishedOnlineFirst:2009/01/13].
Zhao G, Wang H, Xu C, et al. SIRT6 delays cellular senescence by promoting p27Kip1 ubiquitin-proteasome degradation. Aging (Albany NY). 2016;8(10):2308–23. https://doi.org/10.18632/aging.101038[publishedOnlineFirst:2016/10/31].
Wu Y, Chen L, Wang Y, et al. Overexpression of Sirtuin 6 suppresses cellular senescence and NF-κB mediated inflammatory responses in osteoarthritis development. Sci Rep. 2015;5:17602. https://doi.org/10.1038/srep17602[publishedOnlineFirst:2015/12/08].
Takayama K, Ishida K, Matsushita T, et al. SIRT1 regulation of apoptosis of human chondrocytes. Arthritis Rheum. 2009;60(9):2731–40. https://doi.org/10.1002/art.24864[publishedOnlineFirst:2009/08/29].
Yan S, Wang M, Zhao J, et al. MicroRNA-34a affects chondrocyte apoptosis and proliferation by targeting the SIRT1/p53 signaling pathway during the pathogenesis of osteoarthritis. Int J Mol Med. 2016;38(1):201–9. https://doi.org/10.3892/ijmm.2016.2618[publishedOnlineFirst:2016/06/02].
Zhou Z, Deng Z, Liu Y, et al. Protective Effect of SIRT1 Activator on the Knee With Osteoarthritis. Front Physiol. 2021;12: 661852. https://doi.org/10.3389/fphys.2021.661852[publishedOnlineFirst:2021/05/01].
Rellmann Y, Eidhof E, Dreier R. Review: ER stress-induced cell death in osteoarthritic cartilage. Cell Signal. 2021;78: 109880. https://doi.org/10.1016/j.cellsig.2020.109880[publishedOnlineFirst:2020/12/12].
Liu M, Li X, Huang D. Mfn2 Overexpression Attenuates Cardio-Cerebrovascular Ischemia-Reperfusion Injury Through Mitochondrial Fusion and Activation of the AMPK/Sirt3 Signaling. Front Cell Dev Biol. 2020;8: 598078. https://doi.org/10.3389/fcell.2020.598078[publishedOnlineFirst:2020/11/17].
Xu K, He Y, Moqbel SAA, et al. SIRT3 ameliorates osteoarthritis via regulating chondrocyte autophagy and apoptosis through the PI3K/Akt/mTOR pathway. Int J Biol Macromol. 2021;175:351–60. https://doi.org/10.1016/j.ijbiomac.2021.02.029[publishedOnlineFirst:2021/02/09].
Xu C, Wang L, Fozouni P, et al. SIRT1 is downregulated by autophagy in senescence and ageing. Nat Cell Biol. 2020;22(10):1170–9. https://doi.org/10.1038/s41556-020-00579-5[publishedOnlineFirst:2020/09/30].
Yue J, Aobulikasimu A, Sun W, et al. Targeted regulation of FoxO1 in chondrocytes prevents age-related osteoarthritis via autophagy mechanism. J Cell Mol Med. 2022. https://doi.org/10.1111/jcmm.17319[publishedOnlineFirst:2022/05/14].
Tang BL. Sirt1 and the Mitochondria. Mol Cells. 2016;39(2):87–95. https://doi.org/10.14348/molcells.2016.2318[publishedOnlineFirst:2016/02/03].
Imai S, Guarente L. NAD+ and sirtuins in aging and disease. Trends Cell Biol. 2014;24(8):464–71. https://doi.org/10.1016/j.tcb.2014.04.002[publishedOnlineFirst:2014/05/03].
Gomes AP, Price NL, Ling AJ, et al. Declining NAD(+) induces a pseudohypoxic state disrupting nuclear-mitochondrial communication during aging. Cell. 2013;155(7):1624–38. https://doi.org/10.1016/j.cell.2013.11.037[publishedOnlineFirst:2013/12/24].
Bagul PK, Katare PB, Bugga P, et al. SIRT-3 Modulation by Resveratrol Improves Mitochondrial Oxidative Phosphorylation in Diabetic Heart through Deacetylation of TFAM. Cells 2018;7(12) doi: https://doi.org/10.3390/cells7120235 [published Online First: 2018/11/30]
Eisner V, Picard M, Hajnóczky G. Mitochondrial dynamics in adaptive and maladaptive cellular stress responses. Nat Cell Biol. 2018;20(7):755–65. https://doi.org/10.1038/s41556-018-0133-0[publishedOnlineFirst:2018/06/29].
Zhang J, Hao X, Chi R, et al. Moderate mechanical stress suppresses the IL-1β-induced chondrocyte apoptosis by regulating mitochondrial dynamics. J Cell Physiol. 2021;236(11):7504–15. https://doi.org/10.1002/jcp.30386[publishedOnlineFirst:2021/04/07].
Xu L, Wu Z, He Y, et al. MFN2 contributes to metabolic disorders and inflammation in the aging of rat chondrocytes and osteoarthritis. Osteoarthritis Cartilage. 2020;28(8):1079–91. https://doi.org/10.1016/j.joca.2019.11.011[publishedOnlineFirst:2020/05/18].
Wang FS, Kuo CW, Ko JY, et al. Irisin Mitigates Oxidative Stress, Chondrocyte Dysfunction and Osteoarthritis Development through Regulating Mitochondrial Integrity and Autophagy. Antioxidants (Basel) 2020;9(9) doi: https://doi.org/10.3390/antiox9090810 [published Online First: 2020/09/05]
Lee YJ, Jeong SY, Karbowski M, et al. Roles of the mammalian mitochondrial fission and fusion mediators Fis1, Drp1, and Opa1 in apoptosis. Mol Biol Cell. 2004;15(11):5001–11. https://doi.org/10.1091/mbc.e04-04-0294[publishedOnlineFirst:2004/09/10].
Ding M, Feng N, Tang D, et al. Melatonin prevents Drp1-mediated mitochondrial fission in diabetic hearts through SIRT1-PGC1α pathway. J Pineal Res. 2018;65(2): e12491. https://doi.org/10.1111/jpi.12491[publishedOnlineFirst:2018/03/27].
Ansari MY, Khan NM, Ahmad I, et al. Parkin clearance of dysfunctional mitochondria regulates ROS levels and increases survival of human chondrocytes. Osteoarthritis Cartilage. 2018;26(8):1087–97. https://doi.org/10.1016/j.joca.2017.07.020[publishedOnlineFirst:2017/08/13].
Wang C, Yang Y, Zhang Y, et al. Protective effects of metformin against osteoarthritis through upregulation of SIRT3-mediated PINK1/Parkin-dependent mitophagy in primary chondrocytes. Biosci Trends. 2019;12(6):605–12. https://doi.org/10.5582/bst.2018.01263[publishedOnlineFirst:2018/12/26].
Polletta L, Vernucci E, Carnevale I, et al. SIRT5 regulation of ammonia-induced autophagy and mitophagy. Autophagy. 2015;11(2):253–70. https://doi.org/10.1080/15548627.2015.1009778[publishedOnlineFirst:2015/02/24].
Zhu S, Makosa D, Miller B, et al. Glutathione as a mediator of cartilage oxidative stress resistance and resilience during aging and osteoarthritis. Connect Tissue Res. 2020;61(1):34–47. https://doi.org/10.1080/03008207.2019.1665035[publishedOnlineFirst:2019/09/17].
Wu Y, Li J, Zeng Y, et al. Exosomes rewire the cartilage microenvironment in osteoarthritis: from intercellular communication to therapeutic strategies. Int J Oral Sci. 2022;14(1):40. https://doi.org/10.1038/s41368-022-00187-z[publishedOnlineFirst:2022/08/05].
Feng K, Ge Y, Chen Z, et al. Curcumin Inhibits the PERK-eIF2α-CHOP Pathway through Promoting SIRT1 Expression in Oxidative Stress-induced Rat Chondrocytes and Ameliorates Osteoarthritis Progression in a Rat Model. Oxid Med Cell Longev. 2019;2019:8574386. https://doi.org/10.1155/2019/8574386[publishedOnlineFirst:2019/06/22].
Qiu L, Luo Y, Chen X. Quercetin attenuates mitochondrial dysfunction and biogenesis via upregulated AMPK/SIRT1 signaling pathway in OA rats. Biomed Pharmacother. 2018;103:1585–91. https://doi.org/10.1016/j.biopha.2018.05.003[publishedOnlineFirst:2018/06/06].
Wang C, Gao Y, Zhang Z, et al. Safflower yellow alleviates osteoarthritis and prevents inflammation by inhibiting PGE2 release and regulating NF-κB/SIRT1/AMPK signaling pathways. Phytomedicine. 2020;78: 153305. https://doi.org/10.1016/j.phymed.2020.153305[publishedOnlineFirst:2020/09/02].
Wu WT, Chen YR, Lu DH, et al. Silymarin modulates catabolic cytokine expression through Sirt1 and SOX9 in human articular chondrocytes. J Orthop Surg Res. 2021;16(1):147. https://doi.org/10.1186/s13018-021-02305-9[publishedOnlineFirst:2021/02/22].
Jiang C, Sun ZM, Hu JN, et al. Cyanidin ameliorates the progression of osteoarthritis via the Sirt6/NF-κB axis in vitro and in vivo. Food Funct. 2019;10(9):5873–85. https://doi.org/10.1039/c9fo00742c[publishedOnlineFirst:2019/08/30].
Wang J, Wang K, Huang C, et al. SIRT3 Activation by Dihydromyricetin Suppresses Chondrocytes Degeneration via Maintaining Mitochondrial Homeostasis. Int J Biol Sci. 2018;14(13):1873–82. https://doi.org/10.7150/ijbs.27746[publishedOnlineFirst:2018/11/18].
D’Adamo S, Cetrullo S, Guidotti S, et al. Hydroxytyrosol modulates the levels of microRNA-9 and its target sirtuin-1 thereby counteracting oxidative stress-induced chondrocyte death. Osteoarthritis Cartilage. 2017;25(4):600–10. https://doi.org/10.1016/j.joca.2016.11.014[publishedOnlineFirst:2016/12/05].
Zhi LQ, Yao SX, Liu HL, et al. Hydroxytyrosol inhibits the inflammatory response of osteoarthritis chondrocytes via SIRT6-mediated autophagy. Mol Med Rep. 2018;17(3):4035–42. https://doi.org/10.3892/mmr.2017.8353[publishedOnlineFirst:2017/12/30].
Acknowledgements
Not applicable.
Funding
This study was funded by the National Natural Science Foundation of China (Program No. 81974347), China Postdoctoral Science Foundation (No.2021M702351), Medical Science and Technology Project of Health Commission of Sichuan Provincial (No.21PJ040).
Author information
Authors and Affiliations
Contributions
K.S. and Y.W. wrote the manuscript. Y.Z., J.X., L.W. and M.L. edited the manuscript and designed the figures. B.S. contributed to the manuscript design. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sun, K., Wu, Y., Zeng, Y. et al. The role of the sirtuin family in cartilage and osteoarthritis: molecular mechanisms and therapeutic targets. Arthritis Res Ther 24, 286 (2022). https://doi.org/10.1186/s13075-022-02983-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-022-02983-8