Abstract
Background and objectives
Data on the association of vitamin D levels and clinical phenotype and disease activity in systemic lupus erythematosus (SLE) is controversial. Further, the optimal dose of oral vitamin D supplementation in SLE is not clear. Thus, the present study was designed to determine the association of plasma vitamin D levels with clinical phenotype, disease variables and serology in a large, cohort of SLE from South Asia and to evaluate the short-term effect of two different dosage regimens of oral vitamin D supplementation on disease flares and plasma vitamin D levels.
Methods
This is a two-phase study. Phase I was a cross-sectional analytical study of patients from north (26.85° N) and south India (11.94° N). Plasma 25-hydroxyvitamin-D(25(OH)D) was measured, and its association with demography, serology, disease activity, Galectin-9 and CXCL-10 was analysed. In phase II, patients with SLEDAI-2KG < 10 and on stable immunosuppression were randomised to receive either high dose (weekly 60,000 U*5, followed by 60,000 U monthly) or routine dose (30,000 U monthly) oral vitamin D. Outcomes were assessed at 6 months
Results
Phase I included 702 patients with a mean age of 29.46 + 10.7 years. The median plasma vitamin D was 22.83 (13.8–31.8) ng/ml. Deficiency (< 20 ng/ml) was seen in 41.5% of patients. Patients from South India had higher vitamin D levels (27.06 ± 20.21 ng/dl) as compared to North India (17.15 ± 16.07 ng/ml) (p < 0.01). Univariate analyses demonstrated weak negative correlation of vitamin D with SLEDAI2K and positive correlation with age. Galactin-9 had modest correlation with SLEDAI2K but not with vitamin D levels. On multiple linear regression, centre of recruitment (β = 4.37) and age (β = 0.18) predicted (p < 0.05) plasma vitamin D levels.
In the phase II, 91 randomised to 2 groups completed 6 months. Median change in plasma vitamin D levels was more in high dose (9.5 versus 2.6 ng/ml; p = 0.04). There were 14 SLE flares and six minor adverse events which were equal across both groups.
Conclusion
Vitamin D deficiency is common in SLE. Geographical location of residence is the major determinant rather than the disease activity. The IFN regulated proteins reflect disease activity independent of vitamin D levels. High-dose oral vitamin D supplementation seems safe and more effective in improving vitamin D levels in SLE.
Trial registration
The second phase of this study was a registered randomised controlled trial CTRI/2019/06/019658 [registered on: 14/06/2019].
Similar content being viewed by others
Introduction
Vitamin D and its link with autoimmune inflammatory diseases is an important ongoing area of research. The two critical unaddressed questions at present are does vitamin D level determine clinical phenotype in established autoimmune diseases like systemic lupus erythematosus (SLE)? Are the current oral vitamin D supplementation protocols in individuals with SLE successful and safe in improving plasma 25-hydroxyvitamin D (25(OH)D) levels along with additional clinical benefits?
In SLE, it is unclear if the low vitamin D levels cause autoimmunity or are the result of photoprotection [1], drugs used in the treatment of lupus or due to their role as a negative acute phase reactant [2]. Besides calcium homeostasis and bone health, 25-hydroxyvitamin D (25(OH)D) is important in maintaining immune homeostasis. Vitamin D enhances chemotaxis and phagocytosis of macrophages. It reduces IL-17 release by T cells, inhibits proliferation and differentiation of B cells and decreases the production of immunoglobulins [3, 4]. Lupus, on the other hand, has macrophage dysfunction, increased IL-17 production and autoantibody production. Thus, it seems that serum 25(OH)D levels have mechanistic links to the pathogenesis of SLE [5]. Several cross-sectional studies evaluating the association of vitamin D levels with lupus phenotype, disease activity and outcome have arrived at contradicting conclusions [6,7,8,9,10].
Hence, there is a need to evaluate the associations of vitamin D levels with disease activity and clinical phenotype across varying ethnic and geographical backgrounds in a large population. The prevalence of vitamin D deficiency is high among Asians [11]. India has a unique advantage of genetic diversity, which is reasonably ascertained by their native language. The country also boasts of contrasting geographical and environmental factors, a combined view of which enables us to determine the genetic background of individuals [12]. We intend to use this diversity to establish the association of vitamin D levels with clinical phenotype in lupus.
Recent studies have shown that orally supplementing vitamin D decreases progression to autoimmunity [13]. It is unclear if such supplementation will impact disease control in SLE. Moreover, the challenges of supplementing vitamin D in SLE are that the optimal safe dose that can replenish serum vitamin D levels is also not known [14]. So, before attempting to use vitamin D as an adjunct to immunosuppressive agents in SLE for disease control, it is necessary to establish the most effective route and dose of administration.
Hence, this study was designed with the following objectives. First is to study the relationship of vitamin D levels with disease variables and interferon-regulated proteins in patients with systemic lupus erythematosus (SLE) across two ethnic groups of patients from 2 different geographical locations in India. Second is to assess the effect of different dosage regimens of oral vitamin D supplementation on plasma vitamin D levels, disease status and flares at 6 months.
Materials and methods
Patients and study design
We conducted the study in two phases. Phase I was a cross-sectional study, and phase II was an interventional study. Patients with systemic lupus erythematosus who satisfied the SLICC 2012 classification criteria [15] were enrolled in the study. The patients were recruited at two centres, i.e. Lucknow (26.8467° N, 80.9462° E) and Pondicherry (11.9416° N, 79.8083° E) in India, respectively. The two areas differ in the amount of sunlight and ethnicity of people. The patients were either part of the Indian SLE inception cohort for research (INSPIRE) [16] (n = 530) or part of an oral vitamin D supplementation trial [clinical trial registry number: CTRI/2019/06/019658 [registered on: 14/06/2019] which had to be terminated prematurely due to COVID 19 pandemic (n = 172).
The respective institutional ethics committees approved the study, and we conducted the study in accordance with the declaration of Helsinki's guidelines for human research. All patients gave written informed consent.
Demographic, anthropometric and socioeconomic (SES) details per modified Kuppuswamy’s classification [17] of the patients were collected. Kuppuswamy’s classification of the socioeconomic status is a composite score which includes the education and occupation of the family head along with the income per month of the family. The parameters yield a score of 3–29 classifying the population into five SES, namely lower, upper-lower, lower-middle, upper-middle and upper socio-economic class.
Disease activity was assessed using SLE Disease Activity Index-2000 (SLEDAI-2K) [18], and damage was assessed by the Systemic Lupus International Collaborating Clinics/American College of Rheumatology (SLICC/ACR) Damage Index (SDI) [19]. All the patients who were part of the INSPIRE cohort had their blood samples collected on the day of enrolment into the cohort. The sampling was done between October 2018 and February 2022.
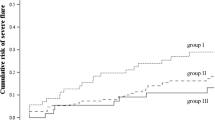
For the interventional study (phase II), SLE patients satisfying the SLICC 2012 classification criteria [15] above the age of 18 years, with SLEDAI 2KG < 10 [20] and on a stable dose of immunosuppressive drugs for 3 months prior to inclusion. All the patients who were part of the trial (phase II) were on calcium and vitamin D supplements and were recruited between January 2019 and February 2020. The patients were then randomised using permuted block randomisation method into two groups (high dose and routine dose). The high dose group was given 5 weekly oral doses of vitamin D 60,000 units followed by monthly 60,000 units for 6 months, and the routine dose group received 30,000 units monthly for the same 6 months without the weekly dose. Patients were followed up every 3 months to document disease flare as defined by the SLEDAI flare index [21]. Vitamin D levels, anti-dsDNA antibody, SLEDAI-2K and the number of flares of the patients were evaluated monthly, and the changes were compared between the two groups. The trial was terminated prematurely during the COVID pandemic (April 2020). The pictorial representation of the workflow for this study is depicted in Fig. 1.
Laboratory assessment
Anti-nuclear antibody (ANA) was tested by indirect immunofluorescence (Hep 2010, EUROImmune, Lubeck, Germany). Serum complements C3 and C4 were measured using BN™ II System nephelometer (SIEMENS Healthliners). Anti-double stranded DNA (anti-dsDNA) was measured using ELISA (EUROImmune, Lubeck, Germany). In a subset of patients, interferon-related proteins galectin 9 and CXCL 10 were measured using ELISA (R&D system, USA). Plasma vitamin D levels were measured using chemiluminescence (COBAS, Roche Diagnostics GmbH, Mannheim, Germany). Vitamin D levels of ≤ 20 ng/ ml was defined as deficiency, > 20 to < 30 ng/ml as insufficiency and ≥ 30 ng/ml as sufficient [21].
Statistics
Normality of data was ascertained by Kolmogorov Smirnov test. All continuous variables in this study were expressed as mean standard deviation (SD) or median interquartile range (IQR)/range as per the normality of the data. Categorical data was represented as number and percentage. Correlation among SLE disease activity scores, damage scores, levels of 25-hydroxyvitamin D3, CXCL-10, galectin-9 anti-dsDNA, serum complement components, age and disease duration was studied by Spearman’s rank correlation analysis. Association of categorical variables between two centres and between those with and without vitamin D insufficiency was tested using chi-square test or Fisher’s exact test. The continuous factors were tested by independent Student T test/Mann-Whitney U test depending upon the distribution of the variable. Using Spearman’s correlation, a multiple linear regression model was built to assess the predictors of vitamin D levels. The model included all the factors showing significant correlation (p < 0.05) with plasma vitamin D levels along with the categorical variable—study centre. Collinearity statistics was conducted. All the statistical tests were performed using SPSS V 19. Bivariate correlation was done using STATA
Results
Demography
For the phase I of the study, 702 patients with SLE were included of whom 663 (93%) were females. The mean age of the participants was 29.44 ± 10.7 years, and the median duration of disease was 16 [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36] months (Supplementary Table 1). The median vitamin D levels in the plasma was 22.83 (13.8–31.8) ng/ml with 41.5% being vitamin D deficient and 29% having sufficient vitamin D levels. One patient had vitamin D level of 109.5 ng/ml, and none had vitamin D toxicity. The median SLEDAI was 10 [4,5,6,7,8,9,10,11,12,13,14,15,16] and 69% had SLEDAI-2K of more than 4.
Effect of geographical location on vitamin D levels
To see the impact of difference in latitude on vitamin D levels, patients from the two centres were compared. Patients from north India had a longer median duration of illness 20 [37] versus 15 [23] months (p = 0.03) and higher proportion of juvenile patients (19.1%) versus the 11.3% in the south Indian centre. The median (IQR) vitamin D levels were 17.15 (16.07) ng/ml and 27.06 (20.21) ng/ml, p < 0.001, at the north and south Indian centres respectively. Vitamin D deficiency was seen in 50.33% of patients from the north Indian centre versus 34.76% in the south. Upon analysing juvenile and adult patients separately, vitamin D levels were similar among the juvenile patients from both centres (p = 0.53). Still, they were higher in the south Indian adult patients [25.5 (13.92) ng/ml] when compared to their north Indian counterparts (Table 1).
Associations of vitamin D levels with clinical and serological factors
Patients with sufficient vitamin D levels had no difference in clinical manifestations, disease activity and levels of interferon-related proteins (CXCL-10 and Galectin 9) as compared to those with insufficient and deficient levels. The only difference was in age which was higher (30.81 ± 10.4 years) in the vitamin D sufficient group as compared to those with low vitamin D levels (27.22 ± 10.6 years; p < 0.05) (Table 2).
Plasma vitamin D levels did not correlate with duration of disease, levels of anti-dsDNA, CXCL-10 and Galactin-9 (p > 0.05). However, it showed weak negative correlation with SLEDAI-2K (Spearman’s rho − 0.134, p < 0.001) and positive correlation with age (rho = 0.182, p < 0.001). SLEDAI-2K had weak negative correlation with age of the patients (rho = − 0.232, p < 0.001) and modest negative correlation with duration of illness (rho = − 0.453, p < 0.001). Galactin-9 had modest positive correlation with SLEDAI-2K (rho = 0.477, p < 0.001) (Fig. 2).
A multiple linear regression model was built taking all the variables that had significant correlation (p < 0.05) with vitamin D. The centre of treatment, which reflected the patients’ geographical location and ethnicity, was added to the model as an independent variable. When adjusted for all the variables, the centre of treatment had a β coefficient of 4.369 (p < 0.05) for predicting the plasma vitamin D levels (Supplementary Table 2).
In the phase II, a total of 172 patients were enrolled, with 87 in the high dose group and 85 in the routine dose group. The baseline features of all the patients in both the groups were similar (Supplementary Table 3). Due to the disruption in healthcare service during the COVID-19 pandemic, 6-month follow-up was available only for 91 individuals (44 in high dose and 47 in routine dose).
At 6 months, the median improvement in the plasma vitamin D levels was higher in high dose group 9.5 (14.5) ng/ml versus 2.6 (14.6) ng/ml in the routine dose group (p = 0.04). In the high dose group, 28 (63.6%) were vitamin D sufficient as opposed to 22 (46.8%) in the routine dose group at the end of 6 months (p = 0.02). There were 14 flares during the 6 months of follow-up with 5 major and 9 minor flares. The incidence of flare was similar across both the groups (Table 3). There were 6 non-serious adverse events in 5 patients in the study, including headache n = 1, vomiting n = 4 and diarrhoea n = 1 (3 in each group). There was no case of vitamin D toxicity.
Discussion
In this study on a reasonably large number of patients with SLE, we found that plasma vitamin D level was insufficient in over 41% of individuals. The vitamin D levels depended on the patients’ geographical location and had no relationship to disease activity, autoantibody status or IFN-related proteins. The two study centres Lucknow (26.8467° N, 80.9462° E) and Pondicherry (11.9416° N, 79.8083° E) are located along similar longitude but differ significantly in their distance from the equator (latitudes). The patients recruited at the southern centre had higher vitamin D levels, and the proportion of those who were vitamin D deficient was also substantially lower. This trend was similar in both juvenile and adult patients.
A systematic review [23] and meta-analysis [24] have identified that patients with lupus have lower plasma vitamin D levels and a higher incidence of vitamin D deficiency compared to healthy controls. Data from India [25] and other southeast Asian countries [26] have shown extremely low vitamin D levels in the healthy population. The mean weighted vitamin D levels reported among the healthy people in India was 19.34 ± 12.08 ng/mL. A random effect meta-analysis showed that the weighted pooled prevalence of vitamin D deficiency was 67% [95% CI: 61–73%] in the community [26]. These figures are similar to the values reported in the present study. It is possible that the metadata [23, 24] on SLE overestimated the vitamin D deficiency in lupus, as the majority of the studies recruited hospital-based healthy controls. The hospital-based recruitment could have led to selection bias, and the healthy controls may not represent the general population. On the other hand, the two systematic reviews on vitamin D deficiency in the healthy population [25, 26] were mainly a synthesis of community-based studies which are likely to have systematically sampled subjects avoiding selection bias.
Even though we have not compared the vitamin D levels of our patients with those of healthy controls, the available data points to the possibility that patients with lupus may have a similar burden of vitamin D deficiency compared to their matched healthy counterparts in the community. Further, the systematic review from India [25] has also clearly identified that people from the southern part of India had higher vitamin D levels, similar to the present study findings. However, since all the patients in our study were on daily calcium supplements, which has 250 IU of vitamin D3, there is a possibility that the deficiency in our cohort was partially corrected.
The ultraviolet B (UV-B) radiation from sunlight with a wavelength between 290 and 315 nm converts 7-dehydrocholesterol to pre-vitamin D3 in the skin. This pre-vitamin D 3 is rapidly converted to cholecalciferol (vitamin D3) [27]. Less than 1% of the UV-B from the sun reaches the earth. The availability of 1% of the UV-B radiation entering the earth’s atmosphere is further determined by the distance the rays must travel to reach the earth’s surface. During winters and in areas that are away from the equator, the distance travelled by UV rays is comparatively longer. This reduces UV-B rays’ availability during winters and as one moves away from the equator [28]. The same principle is observed in our study. Patients in both the centres were recruited at equal proportions in summer and winter thus, the factor determining vitamin D levels primarily seems to be the place of residence.
Another factor that positively correlated with higher vitamin D levels was the age of the patient. It is well known that elderly individuals have lower vitamin D levels [29]. With increasing age, there is a decrease in the concentration of 7-dehydrocholesterol and a reduced response to UV radiation on the skin. Both these factors result in a lower vitamin D level in elderly individuals. In contrast to this theory, we found a positive correlation between vitamin D levels with age. This positive correlation in our study could be because > 90% of our patients were between 25 and 40 years old, an age group where bone mineral density (BMD) and vitamin D levels peak in adults [30, 31]. Moreover, the β coefficient was very small (0.181) for age, suggesting a negligible effect of this variable in reality.
The association studies of vitamin D levels with disease activity in lupus and interferons are variable and have produced contradicting results. While some of the studies have found an association of low vitamin D with specific clinical phenotypes, higher disease activity [6, 7] and cardiovascular co-morbidity [31] and metabolic syndrome [9] in SLE, a few others have failed to establish such associations [8, 10, 32]. The contrast may be due to the result of varying geographical, genetic and treatment-related factors [33]. Or it could be due to the small sample size that was collected over different seasons and not accounting for confounders like BMI, socio-economic status, ethnicity and sex, all of which can influence both SLE disease activity [34, 35] and vitamin D levels [36].
Increased interferon (IFN) expression in SLE modestly reflects disease activity measured by SLEDAI. Murine models of lupus have demonstrated association of low vitamin D levels with type-1 IFN gene expression and endothelial dysfunction [37]. Several human studies have in univariate analyses shown significant negative correlation of SLEDAI with IFN-α and IFN signatures [6, 38, 39]. Galectin-9 and CXCL-10 are IFN-related proteins which have proven to closely reflect IFN-related gene expression in SLE [40]. In our study, we found both Galectin-9 and CXCL-10 levels to correlate significantly with SLEDAI. This finding is similar to most other reported studies [41, 42], reemphasising the vital role of IFN in the pathogenesis of lupus. Few studies have shown significant inverse correlation of IFN alpha levels and IFN gene signature with vitamin D levels in SLE [6, 38]. However, we found no association of galectin-9 and CXCL-10 with plasma vitamin D levels, possibly because of a larger sample size and accounting for various confounding variables. Others have also reported similar non association of IFN alpha with vitamin D levels in SLE [43].
In our prospective RCT which included 91 patients followed up to 6 months, the group who received high dose vitamin D had a higher chance of achieving sufficiency in vitamin D levels than those receiving routine dose. However, no difference was observed in terms of improvement in disease activity or prevention of lupus flare. A recently published study showed improvement in disease activity (SLEDAI-2K) and fatigue at 12 months of cholecalciferol supplementation [14]. Another study on juvenile SLE patients reported improvement in vitamin D levels and bone microarchitecture among those who received cholecalciferol for 24 weeks [44]. There has been no study showing decrease in IFN gene expression with vitamin D supplementation despite achieving adequate serum levels [45]. All these studies, including the current study, emphasise that vitamin D levels can normalise with oral supplementation and is safe. However, the effect on lupus activity and IFN signature are still not established. This could be because of the variable duration of several studies and the use of background immunosuppressive agents whose effect might be so high that added impact of vitamin D may not be evident.
The strength of our study is the large sample size with details about the usual confounders for vitamin D levels. Moreover, the samples were collected at the beginning of recruitment into the cohort, thus decreasing the effect of background immunosuppressive agents. The sample collection in both the centres was conducted round the year, which negates the effect of seasonal variation in vitamin D levels. However, the effect of drugs administered before their entry into the cohort and the patients’ dietary habits are not accounted for. Still, as the patients had a short duration of symptoms, this factor may not have influenced our results. Another drawback is we have not collected data on vascular health and atherosclerotic disease. This association seems to be strong from recently published studies. Another drawback was the premature termination of the trial due to the COVID pandemic. Larger sample size with a longer duration of follow-up would be required to obtain meaningful data on the effect of vitamin D supplementation on disease activity. With the current study’s data, it would be important to determine the effect of ethnicity, vitamin D receptor polymorphisms and alternate methods of vitamin D administration in lupus.
Conclusion
Vitamin D deficiency is common in SLE, and the prevalence may be similar to that encountered in the community. The geographical location of residence is the primary determinant of plasma vitamin D levels rather than the disease activity. The IFN-regulated proteins galectin-9 and CXCL-10 reflect disease activity independent of vitamin D levels. High-dose oral vitamin D supplementation seems safe and more effective in improving vitamin D levels in SLE, but its role in modifying disease progress will need further studies.
Availability of data and materials
All the data will be made available upon reasonable request to the corresponding author.
References
Cusack C, Danby C, Fallon JC, Ho WL, Murray B, Brady J, et al. Photoprotective behaviour and sunscreen use: impact on vitamin D levels in cutaneous lupus erythematosus. Photodermatol Photoimmunol Photomed. 2008;24(5):260–7.
Waldron JL, Ashby HL, Cornes MP, Bechervaise J, Razavi C, Thomas OL, et al. Vitamin D: a negative acute phase reactant. J Clin Pathol. 2013;66(7):620–2.
Baeke F, Takiishi T, Korf H, Gysemans C, Mathieu C. Vitamin D: modulator of the immune system. Curr Opin Pharmacol. 2010;10(4):482–96.
Chen S, Sims GP, Chen XX, Gu YY, Chen S, Lipsky PE. Modulatory effects of 1,25-dihydroxyvitamin D3 on human B cell differentiation. J Immunol Baltim Md 1950. 2007;179(3):1634–47.
Hassanalilou T, Khalili L, Ghavamzadeh S, Shokri A, Payahoo L, Bishak YK. Role of vitamin D deficiency in systemic lupus erythematosus incidence and aggravation. Auto-Immun Highlights. 2017;9(1):1.
Mandal M, Tripathy R, Panda AK, Pattanaik SS, Dakua S, Pradhan AK, et al. Vitamin D levels in Indian systemic lupus erythematosus patients: association with disease activity index and interferon alpha. Arthritis Res Ther. 2014;16(1):R49.
Mok CC, Birmingham DJ, Ho LY, Hebert LA, Song H, Rovin BH. Vitamin D deficiency as marker for disease activity and damage in systemic lupus erythematosus: a comparison with anti-dsDNA and anti-C1q. Lupus. 2012;21(1):36–42.
Souto M, Coelho A, Guo C, Mendonça L, Argolo S, Papi J, et al. Vitamin D insufficiency in Brazilian patients with SLE: prevalence, associated factors, and relationship with activity. Lupus. 2011;20(10):1019–26.
Chew C, Reynolds JA, Lertratanakul A, Wu P, Urowitz M, Gladman DD, et al. Lower vitamin D is associated with metabolic syndrome and insulin resistance in systemic lupus: data from an international inception cohort. Rheumatol Oxf Engl. 2021;60(10):4737–47.
Toloza SMA, Cole DEC, Gladman DD, Ibañez D, Urowitz MB. Vitamin D insufficiency in a large female SLE cohort. Lupus. 2010;19(1):13–9.
Jiang Z, Pu R, Li N, Chen C, Li J, Dai W, et al. High prevalence of vitamin D deficiency in Asia: A systematic review and meta-analysis. Crit Rev Food Sci Nutr. 2021;1–10.
Bose A, Platt DE, Parida L, Drineas P, Paschou P. Integrating linguistics, social structure, and geography to model genetic diversity within India. Mol Biol Evol. 2021;38(5):1809–19.
Hahn J, Cook NR, Alexander EK, Friedman S, Walter J, Bubes V, et al. Vitamin D and marine omega 3 fatty acid supplementation and incident autoimmune disease: VITAL randomized controlled trial. BMJ. 2022;376:e066452.
Magro R, Saliba C, Camilleri L, Scerri C, Borg AA. Vitamin D supplementation in systemic lupus erythematosus: relationship to disease activity, fatigue and the interferon signature gene expression. BMC Rheumatol. 2021;5:53.
Petri M, Orbai AM, Alarcón GS, Gordon C, Merrill JT, Fortin PR, et al. Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum. 2012;64(8):2677–86.
Shobha V, Aggarwal A, Rajasekhar L, Jain A, Gupta R, Das B, et al. Indian SLE Inception cohort for Research (INSPIRE): the design of a multi-institutional cohort. Rheumatol Int. 2021;41(5):887–94.
Wani RT. Socioeconomic status scales-modified Kuppuswamy and Udai Pareekh’s scale updated for 2019. J Fam Med Prim Care. 2019;8(6):1846–9.
Bombardier C, Gladman DD, Urowitz MB, Caron D, Chang CH. Derivation of the SLEDAI. A disease activity index for lupus patients. The Committee on Prognosis Studies in SLE. Arthritis Rheum. 1992;35(6):630–40.
Gladman D, Ginzler E, Goldsmith C, Fortin P, Liang M, Urowitz M, et al. The development and initial validation of the Systemic Lupus International Collaborating Clinics/American College of Rheumatology damage index for systemic lupus erythematosus. Arthritis Rheum. 1996;39(3):363–9.
Touma Z, Gladman DD, Su J, Anderson N, Urowitz MB. A novel lupus activity index accounting for glucocorticoids: SLEDAI-2K glucocorticoid index. Rheumatol Oxf Engl. 2018;57(8):1370–6.
Buyon JP, Petri MA, Kim MY, Kalunian KC, Grossman J, Hahn BH, et al. The effect of combined estrogen and progesterone hormone replacement therapy on disease activity in systemic lupus erythematosus: a randomized trial. Ann Intern Med. 2005;142(12 Pt 1):953–62.
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911–30.
Islam MA, Khandker SS, Alam SS, Kotyla P, Hassan R. Vitamin D status in patients with systemic lupus erythematosus (SLE): a systematic review and meta-analysis. Autoimmun Rev. 2019;18(11):102392.
Wang XR, Xiao JP, Zhang JJ, Wu YG. Decreased serum/plasma vitamin D levels in SLE patients: a meta-analysis. Curr Pharm Des. 2018;24(37):4466–73.
Selvarajan S, Gunaseelan V, Anandabaskar N, Xavier AS, Srinivasamurthy S, Kamalanathan SK, et al. Systematic review on vitamin D level in apparently healthy Indian population and analysis of its associated factors. Indian J Endocrinol Metab. 2017;21(5):765–75.
Siddiqee MH, Bhattacharjee B, Siddiqi UR, MeshbahurRahman M. High prevalence of vitamin D deficiency among the South Asian adults: a systematic review and meta-analysis. BMC Public Health. 2021;21(1):1823.
Bikle DD. Vitamin D metabolism, mechanism of action, and clinical applications. Chem Biol. 2014;21(3):319–29.
Webb AR, Kline L, Holick MF. Influence of season and latitude on the cutaneous synthesis of vitamin D3: exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin. J Clin Endocrinol Metab. 1988;67(2):373–8.
Gallagher JC. Vitamin D and aging. Endocrinol Metab Clin N Am. 2013;42(2):319–32.
Shivane VK, Sarathi V, Lila AR, Bandgar T, Joshi SR, Menon PS, et al. Peak bone mineral density and its determinants in an Asian Indian population. J Clin Densitom. 2012;15(2):152–8.
Patni R. Normal BMD values for Indian females aged 20–80 years. J -Life Health. 2010;1(2):70–3.
Mok CC, Birmingham DJ, Leung HW, Hebert LA, Song H, Rovin BH. Vitamin D levels in Chinese patients with systemic lupus erythematosus: relationship with disease activity, vascular risk factors and atherosclerosis. Rheumatol Oxf Engl. 2012;51(4):644–52.
Muñoz-Ortego J, Torrente-Segarra V, Prieto-Alhambra D, Salman-Monte TC, Carbonell-Abello J. Prevalence and predictors of vitamin D deficiency in non-supplemented women with systemic lupus erythematosus in the Mediterranean region: a cohort study. Scand J Rheumatol. 2012;41(6):472–5.
Rizk A, Gheita TA, Nassef S, Abdallah A. The impact of obesity in systemic lupus erythematosus on disease parameters, quality of life, functional capacity and the risk of atherosclerosis. Int J Rheum Dis. 2012;15(3):261–7.
Alarcón GS, Calvo-Alén J, McGwin G, Uribe AG, Toloza SMA, Roseman JM, et al. Systemic lupus erythematosus in a multiethnic cohort: LUMINA XXXV. Predictive factors of high disease activity over time. Ann Rheum Dis. 2006;65(9):1168–74.
Wei J, Zhu A, Ji JS. A comparison study of vitamin D deficiency among older adults in China and the United States. Sci Rep. 2019;9(1):19713.
Reynolds JA, Rosenberg AZ, Smith CK, Sergeant JC, Rice GI, Briggs TA, et al. Brief Report: Vitamin D deficiency is associated with endothelial dysfunction and increases type I interferon gene expression in a murine model of systemic lupus erythematosus. Arthritis Rheumatol Hoboken NJ. 2016;68(12):2929–35.
Abdel Galil SM, El-Shafey AM, Abdul-Maksoud RS, El-Boshy M. Interferon alpha gene expression and serum level association with low vitamin D levels in Egyptian female patients with systemic lupus erythematosus. Lupus. 2018;27(2):199–209.
Abo-Shanab AM, Kholoussi S, Kandil R, Dorgham D. Cytokines, 25-OH vit D and disease activity in patients with juvenile-onset systemic lupus erythematosus. Lupus. 2021;30(3):459–64.
van den Hoogen LL, van Roon JAG, Mertens JS, et al. Galectin-9 is an easy to measure biomarker for the interferon signature in systemic lupus erythematosus and antiphospholipid syndrome. Annals of the Rheumatic Diseases. 2018;77:1810-4.
Matsuoka N, Fujita Y, Temmoku J, Furuya MY, Asano T, Sato S, et al. Galectin-9 as a biomarker for disease activity in systemic lupus erythematosus. PLoS One. 2020;15(1):e0227069.
Mehta P, Singh P, Aggarwal A. Serum and urinary galectin-9 and C-X-C motif chemokine ligand 10. Lupus. 2022;31(4):482–7.
Schneider L, Colar da Silva AC, Werres Junior LC, Alegretti AP, Pereira dos Santos AS, Santos M, et al. Vitamin D levels and cytokine profiles in patients with systemic lupus erythematosus. Lupus. 2015;24(11):1191–7.
Lima GL, Paupitz JA, Aikawa NE, Alvarenga JC, Pereira RMR. A randomized double-blind placebo-controlled trial of vitamin D supplementation in juvenile-onset systemic lupus erythematosus: positive effect on trabecular microarchitecture using HR-pQCT. Osteoporos Int. 2018;29(3):587–94.
Aranow C, Kamen DL, Dall’Era M, Massarotti EM, Mackay MC, Koumpouras F, et al. Double-blind randomized placebo-controlled trial of the effect of vitamin D3 on the interferon signature in patients with systemic lupus erythematosus. Arthritis Rheumatol Hoboken NJ. 2015;67(7):1848–57.
Acknowledgements
The authors would like to acknowledge the selfless contribution of our patients, Ms. Priyanka and Ms. Dhivya, for the laboratory work and Mr. Deepak for assistance in data entry.
Funding
This work was supported by the Department of Biotechnology, India [BT/PR23111/MED/30/1852/2017 sanctioned on 31.08.2018].
The funding agency provided critical feedbacks during the planning of the study but had no role in data collection, patient recruitment and data analysis.
Author information
Authors and Affiliations
Contributions
AA and VSN designed the study. KC, VSN and AA recruited the patients. SA, DK, AK and ST followed up the patients across both the centres, collected the data and updated the database. SA, DK, PS, SM and AK helped in data retrieval and cleaning. PD and SM conducted the ELISA for IFN-related proteins. KC and AA analysed the data. KC drafted the manuscript, and AA and VSN critically reviewed and edited it. All the authors agree to all the contents in the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The respective institutional ethics committees (JIPMER and SGPGI) JIP/IEC/2018/003 approved the study, and we conducted the study in accordance with the declaration of Helsinki’s guidelines for human research. All patients gave written informed consent.
Consent for publication
All the participants have provided written consent for the conduct of the study and anonymised publication of the information.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
Baseline variables of the cohort.
Additional file 2: Supplementary Table 2.
Multiple linear regression model for predicting vitamin D levels in the cohort.
Additional file 3: Supplementary Table 3.
Baseline parameters of randomised patients.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kavadichanda, C., Singh, P., Maurya, S. et al. Clinical and serological association of plasma 25-hydroxyvitamin D (25(OH)D) levels in lupus and the short-term effects of oral vitamin D supplementation. Arthritis Res Ther 25, 2 (2023). https://doi.org/10.1186/s13075-022-02976-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-022-02976-7