Abstract
Background
We conducted a single-center cohort study of rheumatoid arthritis (RA) patients from 2011 to 2020 to understand their real world treatment and outcomes, especially changes in physical function and quality of life (QOL) in elderly patients, including those aged ≥ 80 years.
Methods
For RA patients attending our outpatient clinic, we annually recorded tender and swollen joint counts, laboratory findings, therapeutic drugs, and scores from the Japanese Health Assessment Questionnaire and EuroQoL-5 Dimensions questionnaire. We examined changes in treatment and outcomes over time, by age group, in patients enrolled over a 10-year period, from 2011 to 2020.
Results
One thousand eight hundred thirty RA patients were enrolled and data were recorded once a year, and a total of 9299 patient records were evaluated. The average age of patients increased by 3.7 years during the study period; the patients aged rapidly. Intensive pharmacological treatment was more frequent in younger patients. Disease activity, physical function, and QOL showed improvement in all age groups over the study period. Physical function and QOL showed greater changes with aging, compared with disease activity. This may be due to the effects of accumulated RA damage, disability due to aging, and depression.
Conclusions
Intensive pharmacological treatment contributes to not only control of disease activity but also the improvement of physical activity and QOL, even in elderly patients. Relieving age-related physical impairment and depression may improve the QOL of very elderly RA patients.
Similar content being viewed by others
Background
Significant progress has been made since the 1990s in the drug treatment of rheumatoid arthritis (RA); outcomes have improved markedly [1, 2]. Meanwhile, it has been reported that some drugs also improve physical function and quality of life (QOL) [1, 3].
The aging of society, which is progressing globally, has diverse and significant impacts on medicine and public health [4]. Previous studies have reported a greater prevalence of RA in the elderly population, compared with the younger population, and a greater number of elderly-onset RA patients [5,6,7]. Elderly patients with RA are generally defined as elderly from the age of 60 to 75 years [8]. However, in Japan, the number of RA patients in their 70s and 80s is rapidly increasing [7, 9].
In T2T recommendations, the most important therapeutic goal in the treatment of RA is to maximize long-term, health-related QOL [10]. Physical activity and QOL generally decline with age. However, in RA patients, age-related changes compound the deterioration in physical activity and QOL caused by disease activity [11, 12].
To date, no clinical studies have examined whether advances in drug therapy can control disease activity and improve physical function and QOL in elderly and very elderly RA patients, as well as in younger RA patients.
Over a 10-year period, from 2011 to 2020, we continuously assessed treatment, disease activity, physical function, and QOL. During this time, the number of treatment options increased significantly, including biologics and targeted, synthetic disease-modifying anti-rheumatic drug (DMARD). Biological DMARD (bDMARD) for RA were available, including infliximab, etanercept, adalimumab, tocilizumab, abatacept, golimumab (launched in 2011), and certolizumab-pegol (launched in 2013). Tofacitinib, a targeted synthetic DMARD (tsDMARD), was launched in 2013. Baricitinib, a Janus kinase (JAK) inhibitor, was launched in 2017; others will be launched after 2019. This study examines the impact of the simultaneous advances in therapeutic agents and population aging on the prognosis of patients with RA.
Methods
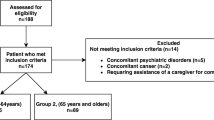
We recruited consenting patients attending our rheumatology outpatient clinic from September to December each year from 2011 to 2022 in this cohort. Patients who had been continuously visiting the clinic since the previous year or earlier were registered as a single patient record based on their age at the time of the visit, as were new outpatients.
We recorded their results from the EuroQoL-5 Dimensions (EQ5D) questionnaire [13, 14], the Japanese Health Assessment Questionnaire (JHAQ) [15, 16], visual analog scale, the number of tender and swollen joints, 28-joint Disease Activity Score C-reactive protein (DAS28-CRP) [17], and medications. We retrospectively examined changes over time in four age groups: < 60 years, 60s, 70s, and ≥ 80s.
Statistical analysis
Patient backgrounds enrolled in each year were summarized. The overall patient population was also summarized by age group. The DAS28-CRP, JHAQ, and EQ5D data were also analyzed using a linear mixed effects model to account for the longitudinal repeated measures. The model assumed random intercepts for patients and included age and year as the fixed effects. We set the significance level at 5% (two-sided) and report two-sided p values. Trends in DAS28-CRP, HAQ score, and EQ-5D score are plotted by year and by age group.
Ethical considerations
This study was approved by the Ethics Committee of Japanese Red Cross Kyoto Daiichi Hospital. Because it is a retrospective, observational study, the written consent of the patients was not required.
Results
Annual change in the number of patients by age group
Fewer than 10 patients per years did not consent to the recording of their data; we consider that this had negligible impact. Over a 10-year period, 1830 RA patients were enrolled and data were recorded once a year, and a cumulative total of 9299 patient records were evaluated. There were 2957 patients aged in their 70s, 2619 patients aged in their 60s, 2459 patients younger than 60, and 1264 patients older than 80 years (very elderly). In a comparison between 2011 and 2020, the average age increased (from 63.9 years to 67.6 years), but the percentage of females did not change over the 10 years (mean, 76.7%). At our hospital, the number of outpatients with RA increased annually; however, when we look at the percentage of each age group by year, we observe that those younger than 60 years old and those aged in their 60s accounted for 30.1% and 34.6%, respectively, in 2011 but decreased to 23.8% and 22.9%, respectively, in 2020. RA patients aged in their 70s accounted for 27.3% in 2011 and increased to 36.1% in 2020. The number of RA patients aged in their 80s increased 3.7-fold (from 52 in 2011 to 194 in 2020); the percentage doubled from 8.1% to 17.2% (Table 1).
Changes in therapeutic agents over time
In 2011, methotrexate (MTX) was widely used in Japan as an anchor DMARD. Trends in treatment over the 10 years show that the frequency of MTX administration decreased from 67.8%, in 2011, to 60.1%, in 2017, to 54.9%, in 2020. A comparison of the percentage of MTX use by age group shows that the decline mainly reflects a decrease in the elderly, 70 years and older. The average dosage of MTX did not change significantly, remaining constant at 7.44–7.76 mg/week after 2012, when the national dosage limit was relaxed from 8 mg/week to 16 mg/week. The frequency of prednisolone (PRED) administration ranged from 30.8 to 28.6%, and the dose ranged from 4.20 to 4.53 mg/day, both of which did not change significantly over the 10-year period. The frequency of administration of biologics, as a whole, did not change over time. However, there were changes in the type of biologics administered. The use of tumor necrosis factor (TNF) α inhibitors decreased from 75.3 to 49.8%, while the use of interleukin (IL) 6 receptor inhibitors and of abatacept increased. In 2020, tsDMARDs were administered to 55 patients (4.9%) (Table 1).
Comparison of therapeutic drugs by age
The average frequency of MTX administration over 10 years was 60.6% and the average dose was 7.60 mg/week. Both frequency and dosage tended to decrease in elderly patients, with only 5.13 mg/week being administered to 40.8% of patients over 80 years of age. PRED was administered to 20.6% of patients aged < 60 years, which increased to 51.3% in patients aged ≥ 80 years; there was no difference in dose between the age groups. The frequency of biologics administration decreased with age. IL6 receptor inhibitors, in particular, accounted for 27.5% of all biologics administered in patients aged < 70 years but decreased markedly to 5% in patients aged ≥ 80 years. The proportion of patients receiving abatacept increased in elderly patients, accounting for 21.0% of all biologics in patients aged ≥ 70 years, and 36.8% of all biologics in patients aged ≥ 80 years. There was no difference between age groups in the frequency and type of tsDMARD administered (Table 2).
Change in disease activity by age group
The rate of change of DAS28CRP varied from year to year between 2011 and 2020. However, the average for all patients decreased significantly each year, from 2.66 to 1.93 (p < 0.001). Similar improvement was shown by all age groups, including the ≥ 80 years group (Fig. 1A). The average DAS28CRP score was lowest in the < 60 years age group, at 2.16. It deteriorated linearly with age, the average score rising to 2.26 (≥ 60 years), to 2.34 (in the 70 years), to 2.51 (≥ 80 years). To consider the magnitude of change in DAS28-CRP, we assigned a value of 1 to the difference between patients aged < 60 years and those aged in their 60s. In terms of this index, the difference between patients aged in their 60s and those aged in their 70s is 0.74. The difference between patients aged in their 70s and those older than 80 years is 1.61 (Fig. 2A).
Annual trends and changes in RA treatment outcomes from 2011–2020 for each age group. A Annual change of mean DAS28-CRP values, for all patients and for each age group. B Annual change of mean JHAQ scores, for all patients and for each age group. C Annual change of mean EQ5D values, for all patients and for each age group. Abbreviations: DAS28, 28-joint Disease Activity Score; JHAQ, Japan Health Assessment Questionnaire; EQ5D, EuroQol-5 Dimensions questionnaire
Changes of RA treatment outcomes by age groups. A Changes in mean DAS28-CRP values, by age group, for the entire period and for each year. B Changes in mean JHAQ scores, by age group, for the entire period and for each year. C Changes in mean EQ5D values, by age group, for the entire period and for each year. Abbreviations: DAS28, 28-joint Disease Activity Score; JHAQ, Japan Health Assessment Questionnaire; EQ5D, EuroQol-5 Dimensions questionnaire
Change in JHAQ by age group
The JHAQ score is a measure of physical activity. Annual changes in the average score for all age groups showed a significant improvement (from 0.72 to 0.56) over the past 10 years (p < 0.001). Patients aged > 80 years showed an improvement from 1.29 to 1.10 (Fig. 1B). The lowest score was 0.245, for those aged < 60 years. The score increased with age to 0.50 (60s), to 0.73 (70s), to 1.03 (80s and older). For patients aged in their 60s and 70s, the magnitude of change was 1.71 times greater than for younger patients; for older patients, it was 3.48 times greater (Fig. 2B).
Change in EQ5D by age group
The EQ5D score was chosen as a measure of QOL. Annual change in this score was slow but significant, improving over the 10 years from 0.749 to 0.785 (p < 0.001). This trend was similar for all age groups. Although patients aged in their 80s did not necessarily show a linear increase in EQ5D score, there was no difference among the ages when comparing the differences between 2011 and 2020 (Fig. 1C). The mean EQ5D score for each age group differed slightly for those aged in their 60s (0.80), compared with those younger than 60 (0.81). It significantly worsened for those aged in their 70s (0.75) and 80s (0.67) (p < 0.001 for each). As was found for the JHAQ score, the magnitude of change in the EQ5D score differed only slightly between patients aged in their 60s and those younger than 60. However, there was a marked deterioration with increasing age. The magnitude of change was 3.9-fold greater for patients aged in their 60s and 70s, and was 6.58-fold greater for patients aged in their 70s and older (Fig. 2C).
Discussion
Lower treatment efficacy in elderly-onset RA and elderly RA patients, compared with younger patients, has been reported by many studies that have examined therapeutic agents and outcomes. It has been reported that elderly patients have higher risks of adverse reactions, including infections, and lower rates of drug retention [8, 18]. Moreover, most reports define “elderly” as the age range from 60–75 years old. There is little data on the patient population older than 80 years, which is expected to increase in our aging society. Recent advances in drugs and therapeutic strategies have improved the outcomes of RA [1, 2]. However, to date, there is no satisfactory answer to the question of whether, in elderly patients, these advances have outweighed the effects of aging on disease activity control and functional prognosis. Japan is the most aged country in the world [19], and the present cohort study followed treatment options and outcomes for 10 years in a population that included patients older than 80 years. It is expected to provide some answers to the clinical questions raised above.
When considering the change in the numbers of RA patients from 2011 to 2020, two factors need to be considered. First, the Department of Rheumatology was established in our hospital in 2004; the increase in patients since 2010 may have been due to the expansion of the department. Thus, the increased number of patients during this period does not necessarily imply that the number of RA patients in the region increased. Second, our hospital is located in an area with a particularly large elderly population, even by Japanese standards. In Higashiyama Ward, the proportion of residents aged ≥ 65 was estimated to be 32.9% in 2020, compared with 28.6% in Japan as a whole [20]. This implies that the effects of aging shown by this study may be more pronounced in Japan as a whole, where the population is aging rapidly. The average age of the RA patients included in this study increased by 3.8 years over the 10-year period. The annual number of patients aged in their 70s increased from 27.3% to 36.1%; the annual number of patients aged 80 years and older increased from 8.1 to 17.2%, which indicates that the RA patient population is aging rapidly.
In general, it is known that the proportion of males increases in elderly-onset RA patients [8, 18]; in this study, there was no change in the sex ratio. This may be because the increase number of male RA patients was offset by an increase in deaths; the estimated 2020 average life expectancy of males in Japan is 81.64 years, 6.1 years shorter than that of females (87.74 years) [20].
When we examine changes in the choice of therapeutic agents and outcomes over the past 10 years, we believe intensive drug therapy was used whenever possible, taking into account the patient's age and physical and social situation. MTX is said to be an anchor drug for RA. In this study, MTX was the mainstay of RA treatment, used in more than 60% of patients, although at a lower dosage than in Europe and the United States. The frequency of MTX use decreased after the age of 70, especially in patients aged ≥ 80 years (40.8%). The amount of MTX used also decreased. PRED was used more frequently in elderly patients, but the dosage (4.41–4.91 mg/day) did not differ depending on the age. MTX has serious side effects, as previously reported, which are especially to be avoided in elderly patients. It is presumed that low-dose steroids were selected as alternative treatments [8, 21, 22]. The usage of biologics, as a whole, tended to decrease with aging; especially IL6 receptor inhibitors were avoided in patients older than 80s. On the contrary, the use of abatacept increased in very old patients. This may be due to evidence in favor of abatacept, compared with IL6 receptor inhibitors and TNF inhibitors, regarding the risk of severe infection [23].
Disease activity in RA improved almost linearly in all age groups over the 10-year period. Considering that there was no change in all ages with respect to MTX dosage during the 10 years, it is assumed that there was no significant change in the severity of the patients. Therefore, we believe that this is mainly due to the emergence of new therapeutic agents and the penetration of intensive therapeutic strategies. Treatment outcomes by age group showed that disease activity deteriorated almost linearly from the < 60 years group to the ≥ 80 years group. This is probably related to the fact that the frequency of use of highly effective drugs, such as MTX and biologics, decreases with age. However, improvement in disease activity over the past decade was generally similar between patients aged > 80 years and those younger than 60 years, which indicates that advances in intensive drug therapy have improved outcomes in elderly patients and younger patients equally.
Physical function, as assessed by the JHAQ, and QOL, as indicated by EQ5D, also improved in all age groups over the decade. This indicates that tight control of disease activity in RA is useful for improving physical function and QOL in both young and elderly patients. However, the pattern of change by age group for both differed slightly from that of disease activity. The magnitude of change in deterioration increased with age. Several causal factors must be considered. In terms of physical function, it is important to consider the deterioration caused by residual joint destruction, and the irreversible component of a health questionnaire [11, 24]. Joint deformities and contractures caused by RA will persist, even after achieving remission with treatments. Second, age-related changes that are not related to RA, such as osteoarthritis, osteoporosis, and sarcopenia, increase in prevalence with age and contribute to functional impairment [11, 25]. Psychological depression is believed to be a third factor contributing to deterioration of QOL. It is well known that RA patients are prone to depression [26], which is exacerbated by aging and associated physical disabilities [27]. The psychological burden of RA may be increased by age-related changes in the home and social environment. These three problems, which worsen HAQ and QOL in late-stage elderly RA patients, are expected to have an increasing impact. Non-pharmacological approaches, such as physical care and psychological support, should be provided along with pharmacotherapy for these patients [28, 29].
The study has several limitations. The living environment of elderly patients and their treatment choices for RA are influenced by economic, cultural, and political factors; therefore, regional differences are likely to be significant. This study was conducted at a single hospital in Japan for a limited period of time; it may not necessarily apply to different social situations or time periods. Second, this study did not examine several variables that may have a significant impact on physical function and QOL, such as comorbidities and socioeconomic status. How these variables relate to the age and disease activity presented here is a very important question that will have to be examined in the future. Third, the number of physicians who treated the patients was limited; their treatment strategies and drug choices may not have always been standardized. However, it can be inferred from the aforementioned medication details that the RA patients registered in this study were treated intensively to achieve the treatment target.
Conclusions
With global population aging, the numbers of RA patients with elderly onset and those aged 80 years and older will increase. Our results show that control of disease activity with DMARDs, based on T2T, can contribute to improvements in physical activity and QOL in late-stage elderly patients with RA. However, for improving the QOL of these patients, the effects of accumulated RA damage, disability due to aging, and depression (due to various factors) must be approached as important issues for future RA treatment.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- bDMARDs:
-
Biological disease-modifying anti-rheumatic drugs
- DMARD:
-
Disease-modifying anti-rheumatic drug
- EQ5D:
-
EuroQoL-5 Dimensions questionnaire
- ESR:
-
Erythrocyte sedimentation rate
- HAQ:
-
Health Assessment Questionnaire
- IL6R:
-
Interleukin-6 receptor
- JHAQ:
-
Japanese Health Assessment Questionnaire
- MTX :
-
Methotrexate
- PRED:
-
Prednisolone
- QOL:
-
Quality of life
- RA:
-
Rheumatoid arthritis
- TNF:
-
Tumor necrosis factor
- T2T:
-
Treat to Target
- tsDMARDs, :
-
Targeted synthetic disease-modifying anti-rheumatic drugs
References
Gullick NJ, Ibrahim F, Scott IC, Vincent A, Cope AP, Garrood T, et al. Real world long-term impact of intensive treatment on disease activity, disability and health-related quality of life in rheumatoid arthritis. BMC Rheumatol. 2019;3:6.
Bakker MF, Jcobs JWG, Verstappen SMM, Bijlsma JWJ. Tight control in the treatment of rheumatoid arthritis: efficacy and feasibility. Ann Rheum Dis. 2007;66(SuppleIII):iii56–60.
Kobelt G, Eberhardt K, Geborek P. TNF inhibitors in the treatment of rheumatoid arthritis in clinical practice: costs and outcomes in a follow up study of patients with RA treated with etanercept or infliximab I southern Sweden. Ann Rheum Dis. 2004;63:4–10.
National Institute of Aging, National Institute of Health, World Health Organaization. Grobal Health and Aging, NIH Publication No.11-7737; 2011. https://www.who.int/ageing/publications/global_health.pdf
Kobak S, Bes C. An autum tale: geriatric rheumatoid arthritis. Ther Adv Musculoskel Dis. 2018;10:3–18.
Safili S, Kolahi AA, Hoy D, Smith E, Bettampadi D, Mansournia MA, et al. Global, regional and national burden of rheumatoid arthritis 1990-2017: a systemic analysis of the Global Burden of Disease study 2017. Ann Rheum Dis. 2019;78:1463–71.
Kojima M, Nakayama T, Tsutani K, Igarashi A, Kojima T, Suzuki S, et al. Epidemiological characteristics of rheumatoid arthritis in Japan: prevalence estimates using a nationwide population-based questionnaire survey. Mod Rheumatol. 2020;30:941–7.
Lahaye C, Tatar Z, Dubost JJ, Yournadre A, Soubrier M. Management of inflammatory rheumatic conditions in the elderly. Rheumatology. 2019;58:748–64.
Imanaka T, Shichikawa K, Inoue K, Shimaoka Y, Takenaka Y, Wakitani S. Increase in age at onset of rheumatoid arthritis in Japan over 30 year period. Ann Rheum Dis. 1997;56:313–6.
Smolen JS, Breedveld FC, Burmester GR, Bykerk V, Dougados M, Emery P, et al. Treating rheumatoid arthritis to target: 2014 update of the recommendations of an international task force. Ann Rheum Dis. 2016;75:3–15.
Sokka T, Krishnan E, Hakkinen A, Hannonen P. Functional disability in rheumatoid arthritis patients compared with a community population in Finland. Arthritis Rheum. 2003;48:59–63.
Fukuda W, OmotoA OT, Sakashita A, Ido A, Kadoya M, et al. Effect of aging on estimates of disease activity and physical function in patients with rheumaoid arthritis. Clin Rheumatol. 2015;27:14–20.
EuroQol Research Foundation. EQ-5D-3L User Guide; 2018. Available from: https://euroqol.org/publications/user-guides
Tsuchiya A, Ikeda S, Ikegami N, Nishimura S, Sakai I, Fukuda T, et al. Estimating an EQ-5D population value set: the case of Japan. Health Econ. 2002;11:341–53. https://doi.org/10.1002/hec.673.
Bruce B, Fries JF. The Health Assessment Questionair (HAQ). Clin Exp Rheumatol. 2005;23:S14–8.
Matsuda Y, Singh G, Yamanaka H, Tanaka E, Urano W, Taniguchi A, et al. Validation of Japanese version of the Stanford Health Assessment Questionair in 3763 patients with rheumatoid arthritis. Arthritis Rheum. 2003;49:784–8.
Wells G, Becker JC, Teng J, Dougados M, Schiff M, Smolen J, et al. Validation of the 28-joint Disease Activity Score (DAS28) and European League Against Rheumatism response criteria based on C-reactive protein against disease progression in patients with rheumatoid arthritis, and comparison with the DAS28 based on erythrocyte sedimentation rate. Ann Rheum Dis. 2009;68:954–60.
Soubrier M, Mathieu S, Payet S, Dubost J, Ristori J. Elderly-onset rheumatoid arthritis. Joint Bone Spine. 2010;77:290–6.
D'Ambrogio E. Japan’s aging society. Briefing in European Parliamentary Research Service; 2020. https://www.europarl.europa.eu/RegData/etudes/BRIE/2020/659419/EPRS_BRI(2020)659419_EN.pdf
Statistics of Japan, https://www.e-stat.go.jp/en/stat-search/files?page=1&layout=datalist&toukei=00200521&tstat=000001049104&cycle=0&tclass1=000001049105&tclass2val=0. Accessed 16 Mar 2022.
Ogasawara M, Tamura N, Onuma S, Kusaoi M, Sekiya F, Matsudaira R, et al. Observational cross-sectional study revealing less aggressive treatment in Japanese elderly than nonelderly patients with rheumatoid arthritis. J Clin Rheumatol. 2010;16:370–4.
Tutuncu Z, Reed G, Kremer J, Kavanaugh A. Do patients with older-onset rheumatoid arthritis receive less aggressive treatment? Ann Rheum Dis. 2006;65:1226–9.
Ebina K, Hashimoto M, Yamamoto W, Hirano T, Hara R, Katayama M, et al. Drug tolerability and reasons for discontinuation of seven biologics in elderly patients with rheumatoid arthritis -The ANSWER cohort study. PLoS One. 2019;14:e0216624.
van der Heijdi D, Landewe R, van Vollenhoven R, Fatenejad S, Klareskog L. Level of radiographic damage and radiographic progression are determinants of physical function: a longitudinal analysis of the TEMPO trial. Ann Rheum Dis. 2008;67:1267–70.
Fukuda W, Omoto A, Ohta T, Majima S, Kimura T, Tanaka T, et al. Low body mass index is associated with impaired quality of life in patients with rheumatoid aruthritis. Int J Rheum Dis. 2013;16:297–302.
Macham F, Reyner L, Steer S, Hotopf M. The prevalence of depression in rheumatoid arthritis: a systemic review and meta-analysis. Rheumatology. 2013;52:2136–48.
Katchamart W, Narongroeknawin P, Chanapai W, Thaweeratthakul P. Health-related quality of life in patients with rheumatoid arthritis. BMC Rheumatol. 2019;3:34.
Benucci M, Rogai V, Atzeni F, Hammen V, Sarzti-Puttini P, Migliore A. Cross associated with rheumatoid arthritis in Italy: past, present, and future. Clin Econ Outcomes Res. 2016;8:33–4.
Omura S, Fukuda W, Yanagida T, Kadoya M, Omoto A, Kawahito Y. Influence of rheumatoid arthritis on long-term care requirements in the elderly. Clin Rhematol. 2019;31:15–23.
Acknowledgements
The authors would like to thank Enago (www.enago.jp) for the English language review.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
W.F. wrote the main manuscript text and M.K. (Masatoshi Kadoya); A.O., T.Y., Y.I., A.S., and H.K. collected and organizing data. K.U. and S.M. were responsible for statistical supervision. M.K. (Masataka Kohno), and Y.K. supervise the clinical aspect of the study. All authors reviewed the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Japanese Red Cross Kyoto Daiichi Hospital. In this study, we evaluated only information that is collected in usual medical practice, and we substituted the agreement acquisition in the document with posting based on ‘Ethical Guidelines for Epidemiological Research’ (in Japan).
Consent for publication
Not applicable.
Competing interests
WF has received speaker’s fee from Chugai Pharmaceutical Co., Eisai Co., Ltd., Eli Lilly Japan K.K., AbbVie GK, Ono Pharmaceutical Co. Ltd., Astellas Pharma Inc., UCB Japan Co. Ltd., Pfizer Japan Inc., Asahikasei Pharma Co., Daiichi-Sankyo Inc., Mitsubishi Tanabe Pharma Co. (less than $10,000 each). AO received speaker’s fees from AbbVie GK, Chugai, Eizai Co., Ltd., Ono Pharmaceutical Co. Ltd., Daiichi-Sankyo Inc., Astellas Pharma Inc., Mitsubishi-Tanabe Pharma Co., Pfizer Japan Inc., Asahikasei Pharma Co., Novartis, Gilead Science Inc., Janssen Pharmaceutical K.K., GlaxoSmithKline K.K., and Eli Lilly Japan K.K. (less than $10,000 each). SM has received speaker’s fee from Bristol Myers Squibb Co. (less than $10,000). MK (Masataka Kohno) has received speaker’s fee from AbbVie GK, Astellas Pharma Inc., Bristol Myers Squibb Co., Chugai Pharmaceutical Co., Ltd. Daiichi Sankyo Co., Eli Lilly Japan K.K, Janssen Pharmaceutical K.K., Mitsubishi Tanabe Pharma Co., Asahikasei Pharma Co., Pfizer Japan Inc., Sanofi Japan K.K., Nippon Boehringer Ingelheim Co. Ltd., UCB Japan Co. Ltd., Eisai Co. Ltd., GlaxoSmithKline K.K. (less than $10,000 each). YK has received research grants from AbbVie GK, Asahi Kasei Pharma Corp., Astellas Pharma Inc., Ayumi Pharmaceutical Corp., Boehringer Ingelheim Japan, Inc., Bristol Myers Squibb Co., Chugai Pharmaceutical Co. Ltd., Daiichi-Sankyo, Inc., Eisai Co., Ltd., Mitsubishi Tanabe Pharma Co., Pfizer Japan Inc., Takeda Pharmaceutical Co., Ltd., and Teijin Pharma Ltd. YK has received speaker’s fee from AbbVie GK, Ayumi Pharmaceutical Corp., Boehringer Ingelheim Japan, Inc., , Chugai Pharmaceutical Co., Ltd., Eisai Co., Ltd., Eli Lilly Japan K.K., GlaxoSmithKline K.K., Pfizer Japan Inc., Takeda Pharmaceutical Co., Ltd., and Teijin Pharma Ltd. (less than $10,000 each). MK (Masatoshi Kadoya), TY, YI, AS, HK, and KU have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fukuda, W., Kadoya, M., Omoto, A. et al. Treatment of rheumatoid arthritis and its outcomes in an aging society: a single-center cohort study in Japan from 2011 to 2020. Arthritis Res Ther 24, 190 (2022). https://doi.org/10.1186/s13075-022-02883-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-022-02883-x