Abstract
Introduction
Whether low socioeconomic status (SES) is associated with worse rheumatoid arthritis (RA) outcomes in countries with general tax-financed healthcare systems (such as Sweden) remains to be elucidated. Our aim was to investigate the influence of educational background (achieving university/college degree (high) or not (low)) on the outcomes of early RA, in terms of disease activity (DAS28), pain (VAS-pain), and functional impairment (HAQ).
Methods
We evaluated DMARD-naïve RA patients recruited in the Epidemiological Investigation of RA (EIRA) study with outcomes followed in the Swedish Rheumatology Quality (SRQ) register (N = 3021). Outcomes were categorized in three ways: 1) scores equal to/above median vs. below median; 2) DAS28-based low disease activity, good response, remission; 3) scores decreased over the median vs. less than median. Associations between educational background and outcomes were calculated by modified Poisson regressions, at diagnosis and at each of the three standard (3, 6, 12 months) follow-up visits.
Results
Patients with different educational background had similar symptom durations (195 days) and anti-rheumatic therapies at baseline, and comparable treatment patterns during follow-up. Patients with a high education level had significantly less pain and less functional disability at baseline and throughout the whole follow-up period (VAS-pain: baseline: 49 (28-67) vs. 53 (33-71), p <0.0001; 1-year visit: RR = 0.81 (95 % CI 0.73-0.90). HAQ: baseline: 0.88 (0.50-1.38) vs. 1.00 (0.63-1.50), p = 0.001; 1-year visit: 0.84 (0.77-0.92)). They also had greater chances to achieve pain remission (VAS-pain ≤20) after one year (1.17 (1.07-1.28)). Adjustments for smoking and BMI altered the results only marginally. Educational background did not influence DAS28-based outcomes.
Conclusion
In Sweden, with tax-financed, generally accessible healthcare system, RA patients with a high education level experienced less pain and less functional disability. Further, these patients achieved pain remission more often during the first year receiving standard care. Importantly, education background affected neither time to referral to rheumatologists, disease activity nor anti-rheumatic treatments.
Similar content being viewed by others
Introduction
Low socioeconomic status (SES), measured in a variety of ways (e.g., formal educational background, occupation, household income, ethnicity), has been associated with an increased risk of rheumatoid arthritis (RA), and a worse disease outcome [1, 2]. Despite several reports describing the adverse link between deprivation and prognosis [3–11], a majority of the reported studies had a cross-sectional design lacking subsequent follow up [3–6], whereas the existing longitudinal studies have focused mainly on long-term consequences (>2 years from baseline) [7–11]. In none of the previous studies has there been the opportunity to analyze the contribution of other known determinants such as the use of anti-rheumatic therapy, or smoking, on RA outcomes. Additionally, whether low SES is associated with worse RA outcomes in countries with general tax-financed healthcare systems (such as Sweden) remains to be elucidated.
Our aim was to evaluate whether SES, here measured as formal educational background, affects the chance of good control of RA during the first year in patients receiving standard care in Sweden. We used data from a well-established population-based RA cohort that has included incident cases captured before the initiation of the first disease-modifying anti-rheumatic drug (DMARD).
Methods
Study population
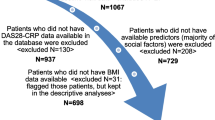
The study participants were newly diagnosed, DMARD-naive RA patients from the Epidemiological investigation of rheumatoid arthritis (EIRA) study in Sweden (previously described in detail [12]), who were included during 1996–2011, and who had clinical follow-up data from the Swedish Rheumatology Quality (SRQ) register until 2013. In total, 3,021 (92 %) of all EIRA cases were included. We excluded: EIRA patients not reported to SRQ, or despite being reported to SRQ, lacking information on all outcome variables (n = 254); patients with symptom duration longer than one year (n = 18); and one patient who lacked information on educational background. All participants gave informed consent and the study was approved by the ethical review board at Karolinska Institutet.
Definition of education and potential confounders
Information on exposure (formal educational background) and several confounders (e.g., age at diagnosis, sex, smoking, alcohol consumption, body mass index (BMI), etc.) was collected through a self-administrated questionnaire (from the EIRA study) at baseline. Briefly, age at diagnosis was a continuous variable. Ever smokers were defined as current and former cigarette smokers while never smokers reported they had never smoked. Pack-years of smoking were calculated with one pack-year equivalent to smoking 20 cigarettes per day for one year. Ever drinking was captured by questions about present alcohol consumption and previous habitual consumption, and included both current and former drinkers. Total alcohol consumption was measured in drinks per week (1 drink = 16 g alcohol). BMI was calculated from self-reported height and weight (kg/m2). Formal educational background at diagnosis was categorized as having a university/college degree (high level of education) versus no university/college degree (low level of education). Several potential determinants of outcomes, including time to the first encounter with a rheumatologist, severity of disease at baseline, first and subsequent use of anti-rheumatic therapy, were recorded by rheumatologists and were accessible through SQR.
Outcome measures
Three clinical aspects were considered as outcome measures: the 28-joint disease activity score (DAS28), visual analog scale for pain (VAS-pain, range 0–100), and health assessment questionnaire (HAQ) score (range 0–3). Please note that in all measures, a higher score represents a poorer outcome.
We primarily classified all outcome measures into equal to/above median versus below median. We further separately categorized patients based on achievement (yes/no) of low disease activity (DAS28 ≤3.2), good response (DAS28 ≤3.2 and DAS28 decrease >1.2) and remission (DAS28 ≤2.6) according to European League Against Rheumatism (EULAR)/American College of Rheumatology (ACR) recommendations [13] and defined pain remission as ≤20 mm on a 100-mm VAS [14]. We further looked into the decrease (scores from each visit compared to the baseline level) larger than the median decrease in all outcome measures. We also investigated the influence of educational background on each component of the DAS28 (i.e., the number of tender and swollen joints out of 28 joints, the erythrocyte sedimentation rate (ESR), and the patient’s global assessment of general health).
Statistical analysis
We used modified Poisson regression to obtain the risk ratio (RR) with 95 % confidence interval (CI) of the outcomes associated with educational background [15]. Patients with university/college degree (high level of education, exposed) were compared with patients without (low level of education, unexposed), at each time point, i.e., the first three follow-up visits (3 (2.5–5.0), 6 (5.0–7.5), and 12 (7.5–18.0) months) after diagnosis.
All analyses were adjusted for potential confounders, i.e., age at diagnosis (continuous, fitted in both the linear and squared term in the model), sex (binary), pack-years of cigarettes smoking (continuous), total alcohol assumption (continuous), BMI (continuous), and outcome measure at baseline (e.g., when analyzing DAS-28-related outcomes at each of the three follow-up visits, we also adjusted for DAS28 baseline level. The same strategy was applied for the HAQ and VAS-pain). In addition, we performed analysis with additional adjustments for residential area (county), leisure time physical activity, anti-citrullinated protein/peptide antibodies (ACPA)-status, treatment at baseline, and study phase. We subsequently carried out stratified analysis based on ACPA status (ACPA-positive and ACPA-negative subgroups), and treatment (DMARDs and other treatments). All analyses were performed in SAS V.9.3.
Results
Basic characteristics of the patients are shown in Table 1. In total, 72 % of the cases were female, and 66 % were ACPA-positive. The RA patients with a low level of education were slightly older, comprised more male patients, and were more likely to be smokers, overweight, and have a less sedentary lifestyle as compared with university-educated patients; whereas in terms of ACPA status, no differences were observed between the two groups. In addition, the median symptom duration was 195 days, exactly the same for both groups of patients.
DAS28-based outcome measures showed comparable baseline levels between the exposed (patients with a university education) and unexposed (patients without a university education) groups but for VAS-pain and HAQ, slightly, although statistically significantly lower, median levels were observed among patients with a university education (VAS-pain 49 (28–67) vs. 53 (33–71), p value <0.0001, HAQ 0.88 (0.50–1.38) vs. 1.00 (0.63–1.50), p value = 0.001). We observed no significant differences in anti-rheumatic treatments initiated at baseline or during the first year of disease (Table 2).
Risk ratios for outcome measures equal to/above median
Throughout the follow-up period, patients with a high level of education had a decreased risk of having VAS-pain above the median compared with patients with a low level of education (RR (95 % CI) for the 3-month visit 0.82 (0.74–0.91); 6-month visit 0.86 (0.77–0.96); 1-year visit 0.81 (0.73–0.90)). They also had less functional impairment than patients with a low level of education (HAQ, 3-month visit 0.83 (0.75–0.91); 6-month visit 0.87 (0.78–0.97); 1-year visit 0.84 (0.77–0.92)) (Table 3). For both VAS-pain and HAQ, the results at the 3-month and 1-year visits remained significant after adjustment. No significant associations were identified between educational background and DAS28.
Risk ratios for DAS28 remission, VAS-pain remission
We observed no associations between educational background and DAS28 remission, low disease activity or good response, except for good response at the 1-year visit (1.10 (1.01–1.20); this did not remain significant after adjustment for potential confounders) and for remission at the 1-year visit (1.12 (1.02–1.24)). Neither did we observe any significant associations for DAS28 components (ESR, C-reactive protein (CRP), and patient global assessment) in relation to educational background (data not shown). Higher education was associated with 15–25 % greater chance of achieving VAS-pain remission (3-month visit: 1.25 (1.13–1.38); 6-month visit: 1.14 (1.02–1.28); 1-year visit: 1.17 (1.07–1.28)). The results, however, did not remain significant at the 6-month visit after adjustment (Table 4).
Risk ratios for outcome measures decrease over the median
Higher education was not associated with increased chance of improvement (more than the median) in VAS-pain (Table 4). Thus, patients with a university education had less pain at baseline and had equivalent decrease to patients without, leading to better pain outcomes at follow up. For HAQ, patients with a university education had a greater chance of improvement in physical function at the 1-year visit (1.11(1.02–1.20)); after adjustment the result was also significant at the 3-month visit (1.11 (1.02–1.21)).
In addition to all the analyses above, we performed analysis with extra adjustments for residential area, leisure time physical activity, ACPA-status, treatment at baseline and study phase, but the results did not alter substantially and those variables were not kept in the final analyses. We subsequently carried out the stratified analysis based on ACPA status, but found no differences between the two subgroups. We also performed stratified analysis based on treatments, and again found no differences.
Discussion
In this population-based cohort with early RA, receiving standard care in a country with a tax-financed, generally accessible healthcare system, educational background affect neither the time to diagnosis nor treatment during the first year. Furthermore, we found that educational background was not associated with disease activity (DAS28), but patients with a high educational level had slightly less pain (VAS-pain) and less functional disability (HAQ) at baseline and during the first year receiving standard care. Consequently, they were also more likely to achieve pain remission and improvements in functional impairment.
Methodological advantages of our study are its large sample size, the population-based design, the inclusion of incident cases, and the extensive information available. These features made it possible to adjust for several potential confounders. The general welfare system in Sweden provides health care to all citizens irrespective of SES, and the similar symptom duration observed among patients with different educational levels indicates that the system does not systematically favor earlier attention to individuals with higher education. Limitations in this study include self-reported educational background, which could have introduced non-differential misclassification. This misclassification was probably small as participants can be expected to remember their highest achieved education relatively easily. Not all EIRA study patients were followed in the clinical quality register, SRQ. However, the proportion of university-educated patients in the EIRA study was very similar (23 % and 20 %) regardless of inclusion in the SRQ.
To some extent our results confirm previous findings on the relationship between low SES and worse disease outcome for some subjective measures [3, 6–11]. However, unlike previous reports, where fewer outcome measures were examined, we carried out a comprehensive investigation with both subjective (VAS-pain, VAS-global, tender joint count, HAQ) and objective outcomes (swollen joint count and the inflammatory marker, ESR). We were also able to record prescription of different anti-rheumatic therapies, and more importantly, adjusted for several potential confounders. Interestingly, we found that levels of education affected neither time to diagnosis nor prescribed anti-rheumatic treatments, and that patients with a low educational level were not inferior in terms of good disease control, but rather the perceived pain control and functional capacity. These results are consistent with the long-term results of the BARFOT study in which 2,800 patients with early RA were followed up in southern Sweden, with no significant effects found between socioeconomic status and treatment or outcomes (DAS28 and EULAR response) [16]. In this context it is important to note that the HAQ questionnaire is a patient-reported outcome (PROM), thus, it relies exclusively on how the patient perceives functional impairment [17]. The same applies for the VAS-pain scale, and it’s possible that educational background influences how one interprets such measures. Another possible explanation for the differing results for the subjective outcomes, or PROMs, could be unmeasured confounding, e.g., those with a low educational level might have a more strenuous workload. Given similar disease activity, patients with physically demanding jobs may experience and report more pain and disability in relation to their daily activities. Moreover, although patients with a high educational level had significantly lower VAS-pain at baseline than patients with a low educational level, from a statistical point of view, it should be noted that the difference between 49 and 53 on a 100-mm VAS is probably of limited clinical relevance. For the HAQ, the median values were 0.88 and 1.00, respectively, and it has previously been concluded that a difference >0.2 is needed for clinical relevance [18].
Despite accumulating evidence demonstrating the contrasting etiology between the two serologically defined RA groups based on ACPA [19], our findings showed no apparent difference in relation to ACPA-status. Several studies have reported low rates of DMARDs use in RA patients in general (30–52 %) [20–24]. One study consisting of 93,143 patients found that individuals with low income or SES received fewer DMARDs prescriptions [25]. Our findings in a country with evenly accessible healthcare, however, did not support that educational background affects the prescription of treatments, with similarly high rates of treatment with DMARDs, NSAIDs, corticosteroids, and biologic agents both at baseline and during the first year, among patients with distinct educational backgrounds.
Conclusions
To summarize, we found that higher-educated newly diagnosed RA patients had less pain and less functional impairment at diagnosis and throughout the follow-up period, although those statistically significant differences were of limited clinical relevance. Consequently, the patients with a higher level of education had a slightly greater chance of achieving pain remission, and improvement in physical function. Our study demonstrates that RA patients with different educational levels have the same opportunity to access healthcare including treatment; and that in this context, educational background has a very limited influence on the disease course.
Abbreviations
- ACPA:
-
anti-citrullinated protein/peptide antibodies
- BMI:
-
body mass index
- DAS28:
-
the 28-joint disease activity score
- DMARD:
-
disease-modifying anti-rheumatic drug
- EIRA:
-
Epidemiological investigation of rheumatoid arthritis
- EULAR:
-
European League Against Rheumatism
- ESR:
-
erythrocyte sedimentation rate
- HAQ:
-
health assessment questionnaire
- NSAID:
-
non-steroidal anti-inflammatory drug
- PROM:
-
patient-reported outcome measures
- RA:
-
rheumatoid arthritis
- RR:
-
risk ratio
- SES:
-
socioeconomic status
- SRQ:
-
Swedish Rheumatology Quality Register
- VAS:
-
visual analog scale
References
Calixto OJ, Anaya JM. Socioeconomic status. The relationship with health and autoimmune diseases. Autoimmun Rev. 2014;13:641–54.
Symmons DP. Environmental factors and the outcome of rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2003;17:717–27.
Camacho EM, Verstappen SM, Symmons DP. Association between socioeconomic status, learned helplessness, and disease outcome in patients with inflammatory polyarthritis. Arthritis Care Res (Hoboken). 2012;64:1225–32.
Marra CA, Lynd LD, Esdaile JM, Kopec J, Anis AH. The impact of low family income on self-reported health outcomes in patients with rheumatoid arthritis within a publicly funded health-care environment. Rheumatology (Oxford). 2004;43:1390–7.
Martin KR, Shreffler J, Schoster B, Callahan LF. Associations of perceived neighborhood environment on health status outcomes in persons with arthritis. Arthritis Care Res (Hoboken). 2010;62:1602–11.
Massardo L, Pons-Estel BA, Wojdyla D, Cardiel MH, Galarza-Maldonado CM, Sacnun MP, et al. Early rheumatoid arthritis in Latin America: low socioeconomic status related to high disease activity at baseline. Arthritis Care Res (Hoboken). 2012;64:1135–43.
ERAS Study Group. Socioeconomic deprivation and rheumatoid disease: what lessons for the health service? ERAS Study Group. Early Rheumatoid Arthritis Study. Ann Rheum Dis 2000, 59:794-799.
Harrison MJ, Farragher TM, Clarke AM, Manning SC, Bunn DK, Symmons DP. Association of functional outcome with both personal- and area-level socioeconomic inequalities in patients with inflammatory polyarthritis. Arthritis Rheum. 2009;61:1297–304.
Harrison MJ, Tricker KJ, Davies L, Hassell A, Dawes P, Scott DL, et al. The relationship between social deprivation, disease outcome measures, and response to treatment in patients with stable, long-standing rheumatoid arthritis. J Rheumatol. 2005;32:2330–6.
Jacobi CE, Mol GD, Boshuizen HC, Rupp I, Dinant HJ, Van Den Bos GA. Impact of socioeconomic status on the course of rheumatoid arthritis and on related use of health care services. Arthritis Rheum. 2003;49:567–73.
McEntegart A, Morrison E, Capell HA, Duncan MR, Porter D, Madhok R, et al. Effect of social deprivation on disease severity and outcome in patients with rheumatoid arthritis. Ann Rheum Dis. 1997;56:410–3.
Bengtsson C, Berglund A, Serra ML, Nise L, Nordmark B, Klareskog L, et al. Non-participation in EIRA: a population-based case-control study of rheumatoid arthritis. Scand J Rheumatol. 2010;39:344–6.
Aletaha D, Landewe R, Karonitsch T, Bathon J, Boers M, Bombardier C, et al. Reporting disease activity in clinical trials of patients with rheumatoid arthritis: EULAR/ACR collaborative recommendations. Ann Rheum Dis. 2008;67:1360–4.
Wolfe F, Michaud K. Assessment of pain in rheumatoid arthritis: minimal clinically significant difference, predictors, and the effect of anti-tumor necrosis factor therapy. J Rheumatol. 2007;34:1674–83.
Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6.
Andersson ML, Bergman S, Soderlin MK. The effect of socioeconomic class and immigrant status on disease activity in rheumatoid arthritis: data from BARFOT, a Multi-Centre Study of Early RA. Open Rheumatol J. 2013;7:105–11.
Lillegraven S, Kvien TK. Measuring disability and quality of life in established rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2007;21:827–40.
Wells GA, Tugwell P, Kraag GR, Baker PR, Groh J, Redelmeier DA. Minimum important difference between patients with rheumatoid arthritis: the patient’s perspective. J Rheumatol. 1993;20:557–60.
Daha NA, Toes RE. Rheumatoid arthritis: Are ACPA-positive and ACPA-negative RA the same disease? Nat Rev Rheumatol. 2011;7:202–3.
Edwards CJ, Arden NK, Fisher D, Saperia JC, Reading I, Van Staa TP, et al. The changing use of disease-modifying anti-rheumatic drugs in individuals with rheumatoid arthritis from the United Kingdom General Practice Research Database. Rheumatology (Oxford). 2005;44:1394–8.
Grijalva CG, Chung CP, Stein CM, Mitchel Jr EF, Griffin MR. Changing patterns of medication use in patients with rheumatoid arthritis in a Medicaid population. Rheumatology (Oxford). 2008;47:1061–4.
Khanna R, Smith MJ. Utilization and costs of medical services and prescription medications for rheumatoid arthritis among recipients covered by a state Medicaid program: a retrospective, cross-sectional, descriptive, database analysis. Clin Ther. 2007;29:2456–67.
Schmajuk G, Schneeweiss S, Katz JN, Weinblatt ME, Setoguchi S, Avorn J, et al. Treatment of older adult patients diagnosed with rheumatoid arthritis: improved but not optimal. Arthritis Rheum. 2007;57:928–34.
Widdifield J, Bernatsky S, Paterson JM, Thorne JC, Cividino A, Pope J, et al. Quality care in seniors with new-onset rheumatoid arthritis: a Canadian perspective. Arthritis Care Res (Hoboken). 2011;63:53–7.
Schmajuk G, Trivedi AN, Solomon DH, Yelin E, Trupin L, Chakravarty EF, et al. Receipt of disease-modifying antirheumatic drugs among patients with rheumatoid arthritis in Medicare managed care plans. JAMA. 2011;305:480–6.
Acknowledgements
We thank the EIRA study group, the EIRA data collectors, and the EIRA study participants. This study was financially supported by grants from the Swedish Medical Research Council; from the Swedish Research Council for Health, Working Life and Welfare, the AFA foundation, Vinnova, King Gustaf V’s 80-year foundation, the Swedish Rheumatic Foundation, and the Swedish Foundation for Strategic Research. The funding sources had no role in the reporting of results or in the decisions about submission/publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
All authors of this research paper have directly participated in the planning (LA, LK, SS, XJ), analysis (XJ, MECS, CB, LA), interpretation (XJ, MECS, SS, LA, LK, CB) and writing (XJ, MECS, SS, LA, LK, CB) of the study and all authors have read and approved the final version for submission.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Jiang, X., Sandberg, M.E.C., Saevarsdottir, S. et al. Higher education is associated with a better rheumatoid arthritis outcome concerning for pain and function but not disease activity: results from the EIRA cohort and Swedish rheumatology register. Arthritis Res Ther 17, 317 (2015). https://doi.org/10.1186/s13075-015-0836-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-015-0836-6