Abstract
Background
Mosquito and human behaviour interaction is a key determinant of the maximum level of protection against malaria that can be provided by insecticide-treated nets (ITNs). Nevertheless, scant literature focuses on this interaction, overlooking a fundamental factor for efficient malaria control. This study aims to estimate malaria transmission risk in a Burkina Faso village by integrating vector biting rhythms with some key information about human habits.
Methods
Indoor/outdoor human landing catches were conducted for 16 h (16:00–08:00) during 8 nights (September 2020) in Goden village. A survey about net usage and sleeping patterns was submitted to half the households (October–December 2020). A subsample of collected specimens of Anopheles gambiae sensu lato was molecularly processed for species identification, Plasmodium detection from heads-thoraxes and L1014F pyrethroid-resistance allele genotyping. Hourly mosquito abundance was statistically assessed by GLM/GAM, and the entomological inoculation rate (EIR) was corrected for the actual ITN usage retrieved from the questionnaire.
Results
Malaria transmission was mainly driven by Anopheles coluzzii (68.7%) followed by A. arabiensis (26.2%). The overall sporozoite rate was 2% with L1014F estimated frequency of 0.68 (N = 1070 out of 15,201 A. gambiae s.l. collected). No major shift in mosquito biting rhythms in response to ITN or differences between indoor and outdoor catches were detected. Impressive high biting pressure (mean 30.3 mosquitoes/person/hour) was exerted from 20:00 to 06:00 with a peak at 4:00. Human survey revealed that nearly all inhabitants were awake before 20:00 and after 7:00 and at least 8.7% had no access to bednets. Adjusting for anthropological data, the EIR dropped from 6.7 to 1.2 infective bites/person/16 h. In a scenario of full net coverage and accounting only for the human sleeping patterns, the daily malaria transmission risk not targetable by ITNs was 0.69 infective bites.
Conclusions
The high mosquito densities and interplay between human/vector activities means that an estimated 10% of residual malaria transmission cannot be prevented by ITNs in the village. Locally tailored studies, like the current one, are essential to explore the heterogeneity of human exposure to infective bites and, consequently, to instruct the adoption of new vector control tools strengthening individual and community protection.
Graphical Abstract

Similar content being viewed by others
Background
The World Health Organisation (WHO) recommends the use of insecticide-treated nets (ITNs) for malaria vector control. The current WHO policy aims to reach “universal coverage” in endemic countries—a benchmarked 80% net access/usage in each community—through cyclic 3-year mass distribution campaigns [1,2,3]. It has been estimated that in sub-Saharan countries, which account for 95% of the global malaria burden, ITNs contributed 68% of the 663 million prevented clinical cases from 2000 to 2015 in Africa [4, 5]. This achievement relies on the combination of individual and community protection exerted by the physical and chemical barrier of the nets, which hampers vectors’ human blood-feeding behaviour: major African malaria vectors are anthropophilic species with a biting peak mostly coinciding with human sleeping hours (i.e. central hours of the night) [6,7,8,9,10,11,12].
Despite ITNs' incontestable success, their effectiveness in sub-Saharan Africa is heterogeneous. There are 10 countries where a stall in the progress against malaria has been registered since 2015, and disease incidence remains very high despite the large bed net coverage [5, 13,14,15,16,17,18].
Among many causal factors for this scenario, a crucial role is played by vector insecticide resistance, which undermines ITNs’ community protection by reducing mosquito exposure to lethal doses of the pyrethroids in net fibres. Indeed, many physiological resistance mechanisms have been reported in all major African malaria vectors: target-site mutation (e.g. L1014F mutation), increased metabolic detoxification activity/efficacy (e.g. P450 monooxygenases), cuticular thickening or changing in hydrocarbon content and binding/sequestration mechanisms [19,20,21,22,23,24,25,26,27,28,29,30]. Furthermore, some vector species exhibit different forms of behavioural resistance (or behavioural plasticity) comprising changes in biting behaviour that facilitate the avoidance of the insecticidal barrier, such as flexibility in the spectrum of host choice (opportunistic behaviour) and/or blood feeding at places and times when humans are less likely to be protected by nets (i.e. outdoors and at dusk/dawn) [21, 31,32,33].
There is a limited understanding of the extent and impact of behavioural resistance among major vector species in sub-Saharan countries. Most reports focus on East Africa and mainly refer to Anopheles arabiensis (with very little evidence for Anopheles gambiae sensu stricto and A. funestus); information about West African vector species is currently incomplete [12, 33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52]. Considering that changes in biting behaviour can increase human-vector contact, an efficient malaria control strategy must consider both entomological and anthropological factors and how they interact. In fact, the interplay between mosquito and human behaviour is considered one of the main causes of residual malaria transmission [53, 54], defined as a persistent parasite transmission despite a fully operational net coverage [54,55,56]. Recent systematic reviews [12, 57] highlighted sparse published data on human activities during the mosquito biting period with only few field reports pairing mosquitoes and human behaviour. The lack of attention to the degree of overlap between mosquito activity and human exposure to bites may affect the accuracy of ITN efficacy estimates. This interaction deserves further investigations as in different settings it can contribute to undermining the protection of ITNs.
Against this background, our study area—the village of Goden in central Burkina Faso—represents an interesting field setting for two major reasons. First, Goden is a rural area severely affected by malaria, like many areas of Burkina Faso, which is among the countries with the highest malaria burden despite mass ITN implementation. Second, we have data on local vectors’ infectivity, behaviour and insecticide resistance over the 10 years of ITN usage in the village [39, 58, 59]. In the context of the present study, we aimed to investigate possible factors sustaining malaria transmission risk in the village focusing on the interplay between human and vector behaviours. To this end, we conducted a deep investigation of malaria vector biting rhythms over 16 h (from 16:00 to 08:00) and integrated the entomological data with key information about human sleeping patterns and net usage retrieved from a questionnaire submitted to village households.
Methods
Study area
The survey was carried out in Goden, a rural village (12°25ʹ N, 1° 21ʹ W) located in the central region of Burkina Faso in a Sudanese savannah area, 35 km east of the capital city of Ouagadougou. The region is characterized by holoendemic malaria mainly caused by Plasmodium falciparum (total malaria cases: 1,011,892; incidence: 354/1000 inhabitants [60, 61]) with a peak during the rainy season, which roughly starts in June and ends in October.
The village comprises around 145 compounds and is inhabited by approximately 900–1000 people (Bogodogo, Health District survey 2021, unpublished), mostly belonging to the Mossi ethnic group and devoted to agriculture and rearing of domestic animals (e.g. cows, pigs, dogs, goats and chickens) in their compounds. The village is also occasionally populated by settlements of Fulani, a historically nomadic ethnic group whose livelihood focuses on cattle rearing. As in the rest of the country, Goden has received a large and relatively stable supply of ITNs since 2010. Although specific data on the actual ITN coverage and usage in the study village are not available, the national survey Enquête sur les indicateurs du paludisme au Burkina Faso (2015 and 2018) [62, 63] reported that, in the Central region, about 55%, 86% and 79% of households received at least one ITN, respectively, in the first three distribution campaigns (2010, 2013 and 2016), with net usage between 55 and 60%. Roughly 3,800,000 ITNs were distributed during these campaigns, corresponding to about 96% household coverage (data unpublished, courtesy of Dr. Wamdaogo Moussa Guelbeogo).
Entomological collections, specimen processing and molecular analysis
Host-seeking mosquitoes were collected by human landing catch (HLC) inside and outside three houses of three different compounds, from 16:00 to 08.00, for 8 nights from 9 to 25 September 2020. In each house, two volunteers rotated each hour between indoor and outdoor positions. Each couple of volunteers also rotated between compounds across the nights of sampling. During the sampling period, the volunteers performing the collections were the only human hosts present in the houses and no ITNs or any other form of vector control was used.
All collected mosquitoes were morphologically identified under stereomicroscope [64], separated by species and gender. A subsample of Anopheles gambiae s.l. females was selected to represent mosquito variability in each compound, house, date, position of samplings (indoors/outdoors) and collection time. The subsample was then processed as follows: heads-thoraces were separated from abdomens and individually stored in tubes containing desiccant until the DNA extraction by DNAZOL protocol (Molecular Research Centre, Cincinnati, OH, USA) [65]. Head-thorax extracted DNA was used as template for: (1) species identification by SINE-PCR protocol [66]; (2) real-time PCR genotyping of L1014F (kdr-w) mutation [67], the most common insecticide-resistance associated allele in the sodium-gated voltage-channel gene; (3) Plasmodium sporozoite DNA detection by real-time PCR [68]. To account for the potential contamination of head-thorax by an earlier infected blood meal, the abdomen of positive heads-thoraxes was also processed by PCR for Plasmodium DNA detection. Notably, it has been shown that molecularly detectable traces of Plasmodium can be still found in heads-thoraxes of 44% of experimentally infected females up to 6 days post-infection [69]. Therefore, a conservative calculation of sporozoite rate (SR) was applied under the assumption that the specimens analysed (all unfed) may have been infected in the last blood meal:
SR = HT + (0.56*HTAB)/N total specimens tested, where: HT is the number of Plasmodium-positive females in head-thorax only; HTAB is the number of Plasmodium-positive females in both head-thorax and abdomen; 0.56 is the corrective factor for Plasmodium positivity imputable to sporozoite stages in head and thorax. This factor is complementary to the 44% of specimens found infected in head/thorax by molecular traces of other life stages.
Finally, the entomological inoculation rate (EIR) of each species was calculated based on its abundance (GAM model described in “Statistical analyses”) and SR. The total EIR of malaria vectors was obtained as a sum of the EIR of each major species to account for their relative contribution to malaria transmission in the village. To estimate a more realistic EIR, considering actual human exposure to mosquito infective bites, we introduced a corrective factor calculated based on information on net usage and human habits retrieved from the questionnaires.
Questionnaire
Representatives of 160 houses, organized in 80 compounds (two houses per compound), were anonymously interviewed by four technicians from the Centre National de Formation et Recherche sur le Paludisme (CNRFP) using a questionnaire designed to collect general information about bednet use and human habits. The interviews were carried out twice a month between 6:30 am and 9:30 a.m. from 5 October to 18 December 2020. Household representatives were interviewed once, apart from 16 who were mistakenly interviewed twice on different dates (5 October and 18 December).
The questionnaire comprised 24 questions about bednet presence, physical integrity and usage as well as human activities and number of inhabitants (Additional file 1: S1a); eight of these, used to fulfil the aim of the present work, were thematically split as follows:
Section A, questions about net availability and human sleeping habits.
-
Q16. Do you have a bednet in the house?
-
Q17. How many nets per person are present in the house?
-
Q22. At what time do you go to sleep?
-
Q23. At what time do you usually wake up?
Section B, questions about the number of inhabitants sleeping in the house and net usage the night before the interview.
-
Q3. How many people slept in the house last night?
-
Q2. How many children?
-
Q6. How many people slept under a bednet? (i.e. number of protected people)
-
Q7. How many people used the same bednet?
The questionnaire was translated from English to French, one of the official languages of Burkina Faso, to facilitate the investigators’ understanding of the text. For the houses interviewed twice, a mean value was considered for the answers given in Section B, as the number of people sleeping in a house can vary among different nights [70]. The answers to Q22 and Q23 were instead considered independently, since slightly different bedtimes and wake-up times were given between different dates of survey.
The number of unprotected people in each household was estimated by subtracting the “number of people that have slept under a net” (Q6) from the “number of people that have slept in the house” (Q3). In this process, the answers given to Q17, “number of available nets per inhabitants”, and to Q7, “number of people sleeping under the same net”, were considered as control questions. For some questionnaires (32 out of 176), the estimated number of unprotected people was considered unreliable, because the number of available nets was too low with respect to the number of people sleeping in the house. For these houses, the number of unprotected people was estimated assigning a range of minimum and maximum values. The percentage of unprotected people was then proportionally added to the awake households in each hour to estimate, respectively, the minimum and maximum “corrective factor” by which to adjust the EIR. This was done to estimate the actual EIR on the base of net usage and human sleeping patterns in the village.
The number of nets present in each house was extrapolated from question Q17, also considering the total of people sleeping in the house (Q3), the number of people that have slept under a net (Q6) and the number of unprotected people (estimated as previously described).
Statistical analyses
A negative binomial generalised linear model (GLM) was fitted to the total number of A. gambiae s.l. females collected during the sampling period to estimate the average number of mosquitoes that were present in the 16-h sampling, position (IN/ OUT), house (1–3) and date of collection (see Additional file 2).
To investigate biting rhythms at species level, a generalized additive model (GAM) was fitted to the number of females for each species collected hourly by HLC indoors (IN) and outdoors (OUT) in each time frame (see Additional file 3). Since only a subsample of specimens was identified at the species level, the proportion for each species in the analysed subsample was used to estimate the overall number of females in each time frame.
Given the discrete nature of the response variable, in the case of over-dispersed data, a negative binomial was chosen as reference distribution in both GLM and GAM models.
GLM structure was:
where \({Y}_{i}\) is the total number of collected mosquitoes, \({\beta }_{0}\) is the model intercept, \({\beta }_{1-4}\) represents the parametric coefficient for the linear effect, \({\left[\mathrm{house}\right]}_{k}\) represents a factor variable with three levels (the three sampled houses, k = 1,2,3), \({[\mathrm{position}]}_{j}\) is a dummy variable with two levels (samples collected inside or outside the houses, j = 1,2), \({[\mathrm{date}]}_{h}\) represents the date of the sampling (factor with 8 levels, h = 1,…,8), and \({[\mathrm{hour}]}_{z}\) represents the time interval of the collection (z = 1,…,16), and \(\varepsilon\) is the error term for the i-th observation.
GAM model structure was:
where Yi is the rounded proportion of mosquitoes collected, \(f\) is a smooth function estimated using penalized likelihood maximization (with a smooth parameter estimated by restricted maximum likelihood) [71] for the h-th species in the i-th position; \({\left[\mathrm{position}\right]}_{j}\) represents a dummy variable with two levels (samples collected inside or outside the houses, j = 1,2) and \({\left[\mathrm{species}\right]}_{h}\) is also a factor with two levels (h = 1,2). Finally, \({\beta }_{hj}\) is the model’s parametric coefficient for the combined linear effect of the j-th position and the h-th species, while \(\varepsilon\) is the error term for the i-th observation.
Chi-square test was employed to investigate differences in the sporozoite rate and L1014F mutant allele frequency between the species of the complex.
Finally, descriptive statistics were employed to extrapolate average values for each question in the questionnaire, obtaining some general information about net usage and human habits in the village.
Results
Species identification, infectivity rate and L1014F mutation genotyping
During the 8 nights of sampling, 15,201 A. gambiae s.l. females were collected landing on human volunteers. In the subsample of 1070 molecularly identified specimens, 68.7% were Anopheles coluzzii (A.co; N = 735); 26.2% A. arabiensis (A.ar; N = 280); 3.7% A. gambiae s.s. (A.ga; N = 40); 0.3% and 0.2% A.co/A.ar (N = 3) and A.co/A.ga (N = 2) hybrids, respectively. Ten specimens (0.9%) were not successfully identified by PCR. Overall, the heads-thoraxes of 27 specimens were positive for Plasmodium. falciparum, 1 for a mixed infection (presence of both P. falciparum and Plasmodium vivax/P. ovale/P. malariae) and 1 for P. vivax, P. ovale or P. malariae. Of 27 specimens positive for P. falciparum in heads-thoraxes (A. coluzzii: 3.7%; A. arabiensis: 0.7%; χ2 = 5.38; p = 0.02), 17 were also positive in the abdomens. By applying the conservative approach described in Methods section, SRs of 2.7% and 0.5% were estimated for A. coluzzii and A. arabiensis, respectively (χ2 = 2.96; p = 0.09). No intra-specific differences were detected in corrected SRs indoors vs. outdoors (A.co: 3.0% indoors, 2.3% outdoors, χ2 = 0.11, p = 0.74; A.ar: 0% indoors, 0.9% outdoors, phi = 0.07, p = 0.51).
The frequency of L1014F mutation was 0.68 (n = 326) in the vector population, significantly higher in A. arabiensis (89%; n = 127) than in A. coluzzii (53%; n = 199) (χ2 = 88.06, P < 0.0001, Table 1).
Vector abundance, biting behaviour and entomological inoculation rate
Results highlight a significant effect of date, house and time of collection on A. gambiae s.l. abundance (GLM = 62% deviance explained; Additional file 2: S2a). However, the relative species proportion stayed consistent between sampling dates and houses (Additional file 2: S2b). No difference was detected between mosquito collections indoors and outdoors (Additional file 2: S2a).
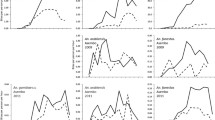
A median of 14.4 and 5.4 mosquitoes/person/hour (m/p/h) is estimated during the 16-h sampling for A. coluzzii and A. arabiensis, respectively. Individual species analysis also highlights different temporal trends of biting activity for A. coluzzii and A. arabiensis (GAM 65.9% deviance explained; Table 2a, Fig. 1; see Additional file 3 for GAM output and 95% confidence intervals of hourly abundances). Anopheles coluzzii exerted an increasing biting pressure, with a peak between 00:00–04:00 and an equal activity between indoors and outdoors across most sampling hours, with the exception of the 19:00–21:00 and 06:00–08:00 periods, when the species is more abundant indoors (12.3 m/p indoors vs. 8.7 outdoors and 6.7 m/p indoors vs. 2.3 outdoors, respectively). Conversely, A. arabiensis shows a roughly homogeneous biting activity between 21:00 and 04:00, with a higher biting pressure exerted outdoors in most time points (i.e. 19:00–05:00: cumulatively 65.3 m/p indoors and 101.4 outdoors; 6:00–08.00: 0.5 m/p indoors and 0.08 outdoors).
Hourly vector species biting activity. Anopheles arabiensis and A. coluzzii female temporal trends predicted by GAM throughout the 16 h of human landing catches carried out indoors (IN, red) and outdoors (OUT, green) in Goden village. The smooth graphs are derived from predicted coefficients of mosquito hourly abundances. The mean values and confidence intervals of the temporal trends are represented as continuous lines and dashed areas, respectively (see also Additional file 3: S3b)
Considering the different abundance and infectivity of the two species, for the malaria vectors in the village an overall EIR of 6.7 infective bites/exposed person (mean of 0.4 infective bites/person/hour; Table 2b) throughout the 16 h-sampling period was estimated. This EIR corresponds to the maximum of malaria transmission risk for a human volunteer constantly exposed to mosquito bites throughout the biting period.
Questionnaire and corrected EIR
Of the 176 questionnaires collected, 6 were excluded because of inconsistencies between the answers, probably because of a misunderstanding between the interviewer and the respondent (see Additional file 1: S1b for questionnaire limitations). The results here reported are retrieved from 170 questionnaires submitted to 157 house representatives (given that 16 of them were interviewed twice, see “Methods”) for an estimated population of 424 individuals. House representatives interviewed were 95% males and 5% females, all over the age of 22. Results of descriptive analyses reveal a median presence of two residents per house, with about 75% of houses composed of one to four inhabitants. Lack of nets is reported in only 3% of the houses, while in 97% at least one ITN is reported and 13% of houses had 2–3 nets. In 75% of houses, the same net was shared by up to two people, in line with the distribution policy [72]; in the rest of the houses, up to five people slept under the same net. Thus, based on the estimated number of inhabitants in the houses interviewed (N = 424), the percentage of unprotected people (i.e. people not using the net) ranged from 8.7 to 20.8%. Finally, 84% of respondents across the house (N = 170) mentioned going to sleep between 20:00 and 22:00 and 90% reported waking up between 5:00 and 7:00 (Table 3).
By combining the self-reported human sleeping patterns with the estimated percentages of unprotected people, we calculated minimum and maximum hourly human exposure rates (Table 3), which were then used as corrective factors of hourly EIR (Table 4).
The corrected estimated risk of malaria transmission during the 16-h sampling period ranges from 1.2 infective bites/person (when a minimum of 8.7% of people not using the net is considered, Fig. 2; Table 4) to 1.9 (when a maximum of 20.8% unprotected people is considered, Table 4). ITNs thus prevent at least 80% of malaria transmission risk, providing a fundamental contribution to individual protection since commonly used from 20:00 to 06:00 when biting pressure reaches an impressive high value of 30.3 mosquitoes/person/h (Table 2a). However, between 16:00–18:00 and 7:00–8:00 (namely when 100% of inhabitants are awake) mosquitoes have a cumulative diurnal biting activity of two bites/person (Table 2b), which accounts for a total of 0.06 infective bites/person (Fig. 2).
Hourly entomological inoculation rates and human exposure to bites. Entomological inoculation rates (EIR) and percentage of human exposure to malaria vector bites during the 16 h of human landing catches in Goden village. Shaded areas: proportion of subjects exposed to bites. This is calculated for each time frame by summing the proportion of houses with people awake (dark grey area) with the minimum proportion of subjects going to sleep without an ITN (i.e. unprotected; light grey area). Blue line: uncorrected EIR; red line: corrected EIR based on minimum human exposure level
Discussion
This study reports a persistent high malaria transmission risk in a village of Burkina Faso, despite over 10 years of ITN mass distribution. Compared to the previous HLC study conducted in the same village in 2015 (indoor/outdoor collections from 21:00 to 04:00) [58], a strong reduction in SR is observed in both A. coluzzii and A. arabiensis, likely due to an efficient individual protection exerted by ITNs (A. coluzzii: 2015 SR = 6%, 2020 = 2.7%; A. arabiensis: 2015 SR = 5.5%, 2020 SR = 0.5%). Nonetheless, the high mosquito biting rate observed in this study is indicative of a reduced killing effect of ITNs, which may compromise the community protection commonly expected when bednet coverage is > 50% [36, 73,74,75,76]. This threshold value is expected to be largely achieved, considering a median of two residents per house and that 95% of interviewed houses had at least one ITN.
Vector population in the village is dominated by A. coluzzii, which has the highest SR, consistent with its intense biting pressure during the entire sampling period (from 16:00 to 8:00) and its well-known anthropophilic preferences [10, 11, 35, 39, 77]. As opposed to A. coluzzii, A. arabiensis shows a lower SR and biting density, indicating its role as secondary malaria vector in the village. This is congruent with the infectivity levels already detected for A. arabiensis in the study area in previous reports [39, 58] as well as with literature evidence describing the generalist host choice behaviour of this species [11, 36, 39, 78,79,80,81,82]. Nevertheless, A. arabiensis should not be considered a vector of negligible importance, since its plastic biting behaviour makes it a resilient species to vector control tools, as shown by its widely recognised role in maintaining residual transmission in many East sub-Saharan countries, where other major anthropophilic vectors (i.e. A. gambiae and A. funestus) are strongly affected by indoor vector control interventions [38, 45, 55, 74, 83,84,85,86,87,88,89,90,91].
The results from this study do not conclusively indicate a marked alteration of biting rhythms—e.g. diversion toward early/late peaks—in response to net presence for A. coluzzii or A. arabiensis. In fact, A. coluzzii shows an increasing biting pressure up to 04:00 (although not significantly between 00:00 and 04:00, see Additional file 3: S3b), which was not observed in 2015 in the same village (when homogeneous biting activity was observed from 21:00 to 04:00, [58]) or in two other studies conducted after ITN implementation in Burkina Faso and Bioko Island [49, 50]. Conversely, A. arabiensis does not show a biting peak during central hours of the night (consistently with observations in 2015) [58], but this cannot be clearly associated to bednet presence, given the heterogeneous biting patterns reported for this species from other settings before and after ITN introduction [7, 41,42,43, 45, 92,93,94,95]. A slight preference for outdoor biting is observed only for A. arabiensis, while A. coluzzii does not exhibit any strong choice for biting location, as also observed in 2015.
Finally, from the epidemiological perspective, due to the dominance of A. coluzzii over A. arabiensis during the sampling period (end of rainy season), the dynamics of malaria transmission risk in the village is manly driven by A. coluzzii infectivity rates and biting patterns. In absence of protection by bednets, this implies that the probability for an exposed human host to receive a bite from an infective mosquito is higher during the central part of the night and does not vary indoors versus outdoors throughout the 16-h sampling period.
The association of entomological data and questionnaires on self-reported human behaviour throughout the mosquito biting period enables an integrated interpretation of malaria transmission dynamics in the context of ITN coverage. This approach indicated that the highest vector biting pressure is still exerted in the hours when humans are sleeping indoors (20:00–06:00), as observed in other regions of Burkina Faso [96] and other sub-Saharan countries [12, 57, 97, 98]. However, some studies showed marked diversion in biting time toward dusk or dawn after ITN/indoor residual spraying intervention indicating a variability in vector response according to geographical context [33, 41, 43, 46,47,48, 52, 56, 99,100,101,102,103,104]. The very high density of biting mosquitoes (around 20 females/person/hour) and the lack of a marked evasive behaviour in response to the net presence (early/late biting peak and mostly outdoor biting) are probably due to physiological resistance mechanisms to pyrethroid insecticides existing in the two species. The presence of phenotypic pyrethroid resistance in the overall vector population, although not directly recorded in this study, is evidenced by a high frequency of L1014F kdr resistance allele, which is the most widely screened target site resistance mutation. However, the level of L1014F allele frequency observed in this study is higher in A. arabiensis than in A. coluzzii. A longitudinal analysis of this mutation in Goden (from year 2011 to 2020; Perugini et al., unpublished) reveals opposite trends of frequencies in the two species, decreasing in A. coluzzii (from 0.72 to 0.56; χ2 = 38.74; p < 0.0001) and increasing in A. arabiensis (from 0.39 to 0.89; χ2 = 187.54, p < 0.0001). This suggests that L1014F frequency reduction in A. coluzzii can be compensated by the introduction of other target-site mutations [105] and/or that other different physiological resistance mechanisms can occur independently between the two species. Moreover, some forms of behavioural resistance/plasticity can contribute to further reduce bednet insecticidal pressure in both A. coluzzii and A. arabiensis [21, 33, 56], as in the case of the flexibility in host choice previously observed in Goden [39]. Collectively, this also results in a non-negligible human biting pressure (2 b/p) in the hours when people are awake (i.e. 16:00–18:00 and 7:00–8:00) and thus not protected by bednets, according with questionnaire results.
Results also highlight a dramatic gap in human protection that can be hard to minimise, even considering a scenario of full net coverage and accounting only for the human sleeping patterns. In fact, during the 16-h sampling, the exposure of awake inhabitants led to a risk of 0.69 i/b/p (i.e. 20.7 infective bites/person/month). In total, 10.3% of malaria transmission cannot be prevented by full coverage with ITNs in this setting. This gap in protection provides a hard core of residual malaria transmission in Goden, probably concurring to sustain the high level of parasite circulation despite over 10 years of bednet usage. This non-preventable exposure to bites is certainly a crucial element contributing to reducing the chances to reach the threshold EIR value of one infective bite/person/year required to proceed toward a feasible elimination of the disease [38, 106].
However, use of respondent-dependent methods, such as questionnaires, comes with embedded limitations. This is particularly true in our case, where the questionnaire was administered within an entomological study not tailored to describing human behaviour (extensively discussed in Additional file 1: S1b). In fact, individual data to quantify the temporal and spatial distribution of human exposure, as described by Monroe et al. [57], were not available. Our questionnaire relied on a single person being the respondent for all people of the household; in addition, no information was collected about the time spent indoors by inhabitants outside the ITN. Moreover, the proportion of unprotected people was obtained triangulating answers about net usage, number of inhabitants and number of available nets in each house. This approach did not allow the capture of micro-level behaviours (such as getting in and out of bed, removing an ITN or moving outdoors during the night) which combine to create additional gaps in protection potentially increasing the exposure to infective bites. Therefore, our measure of human exposure to mosquito bites is likely to be an underestimation. Nevertheless, this questionnaire offered the opportunity to extrapolate some reliable general information, e.g. range of unprotected people and human sleeping patterns, which are extremely useful in supporting interpretation of entomological data, and to assess an actual malaria transmission risk in the village. Finally, it is notable that the residual malaria transmission risk detected in the present study is likely to be affected by overlooked variables, from both anthropological and entomological perspectives. Indeed, in the study of Guglielmo and colleagues [107], the variables “gender”, “age” and “seasonality” had the greatest impact on the risk of human exposure to bites and it was shown that, even in the same week, this risk can vary up to 10 times depending on social events that lead people to be more active outdoors. Moreover, Sangbakembi-Ngounou and colleagues [108] have also described a non-negligible diurnal biting activity of malaria vectors (A. gambiae, A. coluzzii, A. arabiensis and A. pharoensis) indoors in an urban area of the Central African Republic. These studies highlight the difficulties in providing accurate estimations of residual malaria transmission risk and how, across different settings, the current vector control interventions are insufficient to eliminate transmission.
Conclusions
In this study, a deep investigation across the mosquito biting window (16:00–08:00) has been paired with a survey on key information about human habits and net usage in a rural village of Burkina Faso. Results show that, although in the village the highest transmission risk is still occurring when most of the human population is protected under the nets, there is substantial residual malaria transmission—corresponding to 0.69 infective bites/person/day—which persists even considering full net coverage. This is paradigmatic of the problem of residual malaria transmission, which has been already extensively addressed by WHO [54] and tackled in some reviews and reports [55, 56, 109]. WHO emphasises the need to adopt integrated approaches to study malaria transmission dynamics and to generate additional evidence on the local residual malaria transmission. The magnitude of residual malaria transmission can vary greatly from one epidemiological context to another, according to both local entomological and anthropological factors [107, 108]; in some settings, the residual malaria transmission substantially limits the impact of current intervention strategies. Local tailored studies, as the current one in Goden, are essential to explore the heterogeneity of human exposure to infective bites and, consequently, to instruct the adoption of new vector control approaches [55, 110,111,112] by strengthening individual and community protection.
Availability of data and materials
Data supporting the conclusions of this article are included within the article and its additional files. The datasets used and analysed during the present study are available from the corresponding author upon reasonable request.
Abbreviations
- ITN:
-
Insecticide-treated bednet
- WHO:
-
World Health Organisation
- HLC:
-
Human landing catch
- SR:
-
Sporozoite rate
- HT:
-
Plasmodium-positive females in head-thorax only
- HTAB:
-
Plasmodium-positive females in both head-thorax and abdomen
- HBR:
-
Human biting rate
- EIR:
-
Entomological inoculation rate
- cEIR:
-
Corrected entomological inoculation rate
- CNRFP:
-
Centre National de Recherche et de Formation sur le Paludisme
References
Bertozzi-Villa A, Bever CA, Koenker H, Weiss DJ, Vargas-Ruiz C, Nandi AK, et al. Maps and metrics of insecticide-treated net access, use, and nets-per-capita in Africa from 2000–2020. Nat Commun. 2021;12:3589.
Koenker H, Arnold F, Ba F, Cisse M, Diouf L, Eckert E, et al. Assessing whether universal coverage with insecticide-treated nets has been achieved: is the right indicator being used? Malar J. 2018;17:355.
WHO. World Malaria Report 2010. 2011.
Bhatt S, Weiss DJ, Cameron E, Bisanzio D, Mappin B, Dalrymple U, et al. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature. 2015;526:207–11.
WHO. Word Malaria Report 2021. World Health Organ. 2022.
Molineaux L, Gramiccia G. Le projet Garki. Geneva, Switzerland: World Health Organization; 1980.
Lemasson J-J, Fontenille D, Lochouarn L, Dia I, Simard F, Ba K, et al. Comparison of behavior and vector efficiency of Anopheles gambiae and An. arabiensis (Diptera: Culicidae) in Barkedji, a Sahelian Area of Senegal. J Med Entomol. 1997;34:396–403.
Quiñones ML, Lines JD, Thomson MC, Jawara M, Morris J, Greenwood BM. Anopheles gambiae gonotrophic cycle duration, biting and exiting behaviour unaffected by permethrin-impregnated bednets in the Gambia. Med Vet Entomol. 1997;11:71–8.
Wanji S, Tanke T, Atanga SN, Ajonina C, Nicholas T, Fontenille D. Anopheles species of the Mount Cameroon region: biting habits, feeding behaviour and entomological inoculation rates. Trop Med Int Health. 2003;8:643–9.
Carnevale P, Robert V, Manguin S, Corbel V, Fontenille D, Garros C, Rogier C. Les anophèles: biologie, transmission du Plasmodium et lutte antivectorielle. IRD Editio. Actiques I, editor. Marseille; 2009.
Sinka ME, Bangs MJ, Manguin S, Coetzee M, Mbogo CM, Hemingway J, et al. The dominant Anopheles vectors of human malaria in Africa, Europe and the Middle East: occurrence data, distribution maps and bionomic précis. Parasit Vectors. 2010;3:117.
Sherrard-Smith E, Skarp JE, Beale AD, Fornadel C, Norris LC, Moore SJ, et al. Mosquito feeding behavior and how it influences residual malaria transmission across Africa. Proc Natl Acad Sci. 2019;116:15086–95.
Jagannathan P, Muhindo MK, Kakuru A, Arinaitwe E, Greenhouse B, Tappero J, et al. Increasing incidence of malaria in children despite insecticide-treated bed nets and prompt anti-malarial therapy in Tororo, Uganda. Malar J. 2012;11:435.
Coulibaly D, Travassos MA, Kone AK, Tolo Y, Laurens MB, Traore K, et al. Stable malaria incidence despite scaling up control strategies in a malaria vaccine-testing site in Mali. Malar J. 2014;13:374.
Mwesigwa J, Okebe J, Affara M, Di Tanna GL, Nwakanma D, Janha O, et al. On-going malaria transmission in The Gambia despite high coverage of control interventions: a nationwide cross-sectional survey. Malar J. 2015;14:314.
Obala AA, Mangeni JN, Platt A, Aswa D, Abel L, Namae J, et al. What is threatening the effectiveness of insecticide-treated bednets? A case-control study of environmental, behavioral, and physical factors associated with prevention failure. PLoS ONE. 2015;10:e0132778.
Assouho KF, Adja AM, Guindo-Coulibaly N, Tia E, Kouadio AMN, Zoh DD, et al. Vectorial transmission of malaria in major districts of Côte d’Ivoire. J Med Entomol. 2020;57:908–14.
Topazian HM, Gumbo A, Brandt K, Kayange M, Smith JS, Edwards JK, et al. Effectiveness of a national mass distribution campaign of long-lasting insecticide-treated nets and indoor residual spraying on clinical malaria in Malawi, 2018–2020. BMJ Glob Health. 2021;6:e005447.
Awolola TS, Oduola OA, Strode C, Koekemoer LL, Brooke B, Ranson H. Evidence of multiple pyrethroid resistance mechanisms in the malaria vector Anopheles gambiae sensu stricto from Nigeria. Trans R Soc Trop Med Hyg. 2009;103:1139–45.
Wood OR, Hanrahan S, Coetzee M, Koekemoer LL, Brooke BD. Cuticle thickening associated with pyrethroid resistance in the major malaria vector Anopheles funestus. Parasit Vectors. 2010;3:67.
Ranson H, N’Guessan R, Lines J, Moiroux N, Nkuni Z, Corbel V. Pyrethroid resistance in African anopheline mosquitoes: what are the implications for malaria control? Trends Parasitol. 2011;27:91–8.
Nkya TE, Akhouayri I, Kisinza W, David J-P. Impact of environment on mosquito response to pyrethroid insecticides: facts, evidences and prospects. Insect Biochem Mol Biol. 2013;43:407–16.
Balabanidou V, Kampouraki A, MacLean M, Blomquist GJ, Tittiger C, Juárez MP, et al. Cytochrome P450 associated with insecticide resistance catalyzes cuticular hydrocarbon production in Anopheles gambiae. Proc Natl Acad Sci. 2016;113:9268–73.
Bonizzoni M, Afrane Y, Dunn WA, Atieli FK, Zhou G, Zhong D, et al. Comparative transcriptome analyses of deltamethrin-resistant and -susceptible Anopheles gambiae mosquitoes from Kenya by RNA-Seq. PLoS ONE. 2012;7:e44607.
Ingham VA, Wagstaff S, Ranson H. Transcriptomic meta-signatures identified in Anopheles gambiae populations reveal previously undetected insecticide resistance mechanisms. Nat Commun. 2018;9:5282.
Minetti C, Ingham VA, Ranson H. Effects of insecticide resistance and exposure on Plasmodium development in Anopheles mosquitoes. Curr Opin Insect Sci. 2020;39:42–9.
Ingham VA, Anthousi A, Douris V, Harding NJ, Lycett G, Morris M, et al. A sensory appendage protein protects malaria vectors from pyrethroids. Nature. 2020;577:376–80.
Grigoraki L, Cowlishaw R, Nolan T, Donnelly M, Lycett G, Ranson H. CRISPR/Cas9 modified An. gambiae carrying kdr mutation L1014F functionally validate its contribution in insecticide resistance and combined effect with metabolic enzymes. PLOS Genet. 2021;17:e1009556.
Clarkson CS, Miles A, Harding NJ, O’Reilly AO, Weetman D, Kwiatkowski D, et al. The genetic architecture of target-site resistance to pyrethroid insecticides in the African malaria vectors Anopheles gambiae and Anopheles coluzzii. Mol Ecol. 2021;30:5303–17.
Black WC, Snell TK, Saavedra-Rodriguez K, Kading RC, Campbell CL. From global to local—new insights into features of pyrethroid detoxification in vector mosquitoes. Insects. 2021;12:276.
Sokhna C, Ndiath MO, Rogier C. The changes in mosquito vector behaviour and the emerging resistance to insecticides will challenge the decline of malaria. Clin Microbiol Infect. 2013;19:902–7.
Gatton ML, Chitnis N, Churcher T, Donnelly MJ, Ghani AC, Godfray HCJ, et al. The importance of mosquito behavioural adaptations to malaria control in Africa. Evolution. 2013;67:1218–30.
Carrasco D, Lefèvre T, Moiroux N, Pennetier C, Chandre F, Cohuet A. Behavioural adaptations of mosquito vectors to insecticide control. Curr Opin Insect Sci. 2019;34:48–54.
Bøgh C, Pedersen EM, Mukoko DA, Ouma JH. Permethrin-impregnated bednet effects on resting and feeding behaviour of lymphatic filariasis vector mosquitoes in Kenya. Med Vet Entomol. 1998;12:52–9.
Lefèvre T, Gouagna LC, Dabiré KR, Elguero E, Fontenille D, Renaud F, et al. Beyond nature and nurture: Phenotypic plasticity in blood-feeding behavior of Anopheles gambiae s.s. when humans are not readily accessible. Am J Trop Med Hyg. 2009;81:1023–9.
Killeen GF, Smith TA. Exploring the contributions of bed nets, cattle, insecticides and excitorepellency to malaria control: a deterministic model of mosquito host-seeking behaviour and mortality. Trans R Soc Trop Med Hyg. 2007;101:867–80.
Ndenga BA, Mulaya NL, Musaki SK, Shiroko JN, Dongus S, Fillinger U. Malaria vectors and their blood-meal sources in an area of high bed net ownership in the western Kenya highlands. Malar J. 2016;15:76.
Killeen GF, Kiware SS, Okumu FO, Sinka ME, Moyes CL, Massey NC, et al. Going beyond personal protection against mosquito bites to eliminate malaria transmission: population suppression of malaria vectors that exploit both human and animal blood. BMJ Glob Health. 2017;2:e000198.
Pombi M, Calzetta M, Guelbeogo WM, Manica M, Perugini E, Pichler V, et al. Unexpectedly high Plasmodium sporozoite rate associated with low human blood index in Anopheles coluzzii from a LLIN-protected village in Burkina Faso. Sci Rep. 2018;8:1–10.
Kreppel KS, Viana M, Main BJ, Johnson PCD, Govella NJ, Lee Y, et al. Emergence of behavioural avoidance strategies of malaria vectors in areas of high LLIN coverage in Tanzania. Sci Rep. 2020;10:14527.
Kenea O, Balkew M, Tekie H, Gebre-Michael T, Deressa W, Loha E, et al. Human-biting activities of Anopheles species in south-central Ethiopia. Parasit Vectors. 2016;9:527.
Bayoh MN, Walker ED, Kosgei J, Ombok M, Olang GB, Githeko AK, et al. Persistently high estimates of late night, indoor exposure to malaria vectors despite high coverage of insecticide treated nets. Parasit Vectors. 2014;7:380.
Milali MP, Sikulu-Lord MT, Govella NJ. Bites before and after bedtime can carry a high risk of human malaria infection. Malar J. 2017;16:91.
Mwesigwa J, Achan J, Di Tanna GL, Affara M, Jawara M, Worwui A, et al. Residual malaria transmission dynamics varies across The Gambia despite high coverage of control interventions. PLoS ONE. 2017;12:e0187059.
Hakizimana E, Karema C, Munyakanage D, Githure J, Mazarati JB, Tongren JE, et al. Spatio-temporal distribution of mosquitoes and risk of malaria infection in Rwanda. Acta Trop. 2018;182:149–57.
Braimah N, Drakeley C, Kweka E, Mosha F, Helinski M, Pates H, et al. Tests of bednet traps (Mbita traps) for monitoring mosquito populations and time of biting in Tanzania and possible impact of prolonged insecticide treated net use. Int J Trop Insect Sci. 2005;25:208–13.
Moiroux N, Gomez MB, Pennetier C, Elanga E, Djènontin A, Chandre F, et al. Changes in Anopheles funestus biting behavior following universal coverage of long-lasting insecticidal nets in Benin. J Infect Dis. 2012;206:1622–9.
Sougoufara S, Diédhiou SM, Doucouré S, Diagne N, Sembène PM, Harry M, et al. Biting by Anopheles funestus in broad daylight after use of long-lasting insecticidal nets: a new challenge to malaria elimination. Malar J. 2014;13:125.
Reddy MR, Overgaard HJ, Abaga S, Reddy VP, Caccone A, Kiszewski AE, et al. Outdoor host seeking behaviour of Anopheles gambiae mosquitoes following initiation of malaria vector control on Bioko Island, Equatorial Guinea. Malar J. 2011;10:184.
Epopa PS, Collins CM, North A, Millogo AA, Benedict MQ, Tripet F, et al. Seasonal malaria vector and transmission dynamics in western Burkina Faso. Malar J. 2019;18:113.
Wamae PM, Githeko AK, Otieno GO, Kabiru EW, Duombia SO. Early biting of the Anopheles gambiae s.s. and its challenges to vector control using insecticide treated nets in western Kenya highlands. Acta Trop. 2015;150:136–42.
Degefa T, Githeko AK, Lee M-C, Yan G, Yewhalaw D. Patterns of human exposure to early evening and outdoor biting mosquitoes and residual malaria transmission in Ethiopia. Acta Trop. 2021;216:105837.
The Malaria Elimination Initiative. Entomological Surveillance Planning Tool (ESPT). San Francisco: Institute for Global Health Sciences, University of California, San Francisco. 2020.
WHO. Control of residual malaria parasite transmission: guidance note. World Health Organ. Tech. Rep. Ser. 2014.
Killeen GF. Characterizing, controlling and eliminating residual malaria transmission. Malar J. 2014;13:330.
Carnevale P, Manguin S. Review of issues on residual malaria transmission. J Infect Dis. 2021;223:S61-80.
Monroe A, Moore S, Koenker H, Lynch M, Ricotta E. Measuring and characterizing night time human behaviour as it relates to residual malaria transmission in sub-Saharan Africa: a review of the published literature. Malar J. 2019;18:6.
Perugini E, Guelbeogo WM, Calzetta M, Manzi S, Virgillito C, Caputo B, et al. Behavioural plasticity of Anopheles coluzzii and Anopheles arabiensis undermines LLIN community protective effect in a Sudanese-savannah village in Burkina Faso. Parasit Vectors. 2020;13:277.
Calzetta M, Perugini E, Seixas G, Sousa CA, Guelbeogo WM, Sagnon N, et al. A novel nested polymerase chain reaction assay targeting Plasmodium mitochondrial DNA in field-collected Anopheles mosquitoes. Med Vet Entomol. 2018;32:372–7.
Ouédraogo A, Tiono AB, Diarra A, Sanon S, Yaro JB, Ouedraogo E, et al. Malaria morbidity in high and seasonal malaria transmission area of Burkina Faso. PLoS ONE. 2013;8:e50036.
Ministry of Health of Burkina Faso. Annuaire statistique 2020. Ouagadougou: Conseil National de la Statistique, Burkina Faso; 2021. https://www.sante.gov.bf/fileadmin/user_upload/storages/annuaire_statistique_ms_2020_signe.pdf.
Institut National de la Statistique et de la Démographie (INSD), Programme d’Appui au Développement Sanitaire (PADS), Programme National de Lutte contre le Paludisme (PNLP) et ICF. Enquête sur les Indicateurs du Paludisme au Burkina Faso,2014. Rockville, Maryland, USA, 2015.
Institut National de la Statistique et de la Démographie (INSD), Programme d’Appui au Développement Sanitaire (PADS), Programme National de Lutte contre le Paludisme (PNLP) et ICF. Enquête sur les indicateurs du paludisme au Burkina Faso, 2017–2018. Rockville, Maryland, USA, 2018.
Gillies MT, Coetzee M. A supplement to the Anophelinae of Africa south of the Sahara (Afrotropical region). Johannesburg: The South African Institute for Medical Research; 1987.
Rider MA, Byrd BD, Keating J, Wesson DM, Caillouet KA. PCR detection of malaria parasites in desiccated Anopheles mosquitoes is uninhibited by storage time and temperature. Malar J. 2012;11:193.
Santolamazza F, Mancini E, Simard F, Qi Y, Tu Z, della Torre A. Insertion polymorphisms of SINE200 retrotransposons within speciation islands of Anopheles gambiae molecular forms. Malar J. 2008;7:163.
Bass C, Nikou D, Donnelly MJ, Williamson MS, Ranson H, Ball A, et al. Detection of knockdown resistance (kdr) mutations in Anopheles gambiae: a comparison of two new high-throughput assays with existing methods. Malar J. 2007;6:111.
Bass C, Nikou D, Blagborough AM, Vontas J, Sinden RE, Williamson MS, et al. PCR-based detection of Plasmodium in Anopheles mosquitoes: a comparison of a new high-throughput assay with existing methods. Malar J. 2008;7:177.
Hendershot AL, Esayas E, Sutcliffe AC, Irish SR, Gadisa E, Tadesse FG, et al. A comparison of PCR and ELISA methods to detect different stages of Plasmodium vivax in Anopheles arabiensis. Parasit Vectors. 2021;14:473.
Guglielmo F, Ranson H, Sagnon N, Jones C. The issue is not ‘compliance’: exploring exposure to malaria vector bites through social dynamics in Burkina Faso. Anthropol Med. 2021;28:508–25.
Wood SN, Pya N, Säfken B. Smoothing parameter and model selection for general smooth models. J Am Stat Assoc. 2016;111:1548–63.
Global Malaria Programme (GMP) WHO. Achieving and maintaining universal coverage with long-lasting insecticidal nets for malaria control. Tech. Rep. 2017.
Hawley WA, Phillips-Howard PA, ter Kuile FO, Terlouw DJ, Vulule JM, Ombok M, et al. Community-wide effects of permethrin-treated bed nets on child mortality and malaria morbidity in western Kenya. Am J Trop Med Hyg. 2003;68:121–7.
Russell TL, Lwetoijera DW, Maliti D, Chipwaza B, Kihonda J, Charlwood JD, et al. Impact of promoting longer-lasting insecticide treatment of bed nets upon malaria transmission in a rural Tanzanian setting with pre-existing high coverage of untreated nets. Malar J. 2010;9:187.
Killeen GF, Smith TA, Ferguson HM, Mshinda H, Abdulla S, Lengeler C, et al. Preventing childhood malaria in Africa by protecting adults from mosquitoes with insecticide-treated nets. PLoS Med. 2007;4:e229.
Govella NJ, Okumu FO, Killeen GF. Short report: insecticide-treated nets can reduce malaria transmission by mosquitoes which feed outdoors. Am J Trop Med Hyg. 2010;82:415–9.
Athrey G, Cosme LV, Popkin-Hall Z, Pathikonda S, Takken W, Slotman MA. Chemosensory gene expression in olfactory organs of the anthropophilic Anopheles coluzzii and zoophilic Anopheles quadriannulatus. BMC Genomics. 2017;18:751.
Bøgh C, Clarke SE, Pinder M, Sanyang F, Lindsay SW, Clarke NE, et al. Effect of passive zooprophylaxis on malaria transmission in the Gambia. J Med Entomol. 2001;38:822–8.
Tirados I, Costantini C, Gibson G, Torr SJ. Blood-feeding behaviour of the malarial mosquito Anopheles arabiensis: implications for vector control. Med Vet Entomol. 2006;20:425–37.
Torr SJ, Della Torre A, Calzetta M, Costantini C, Vale GA. Towards a fuller understanding of mosquito behaviour: use of electrocuting grids to compare the odour-orientated responses of Anopheles arabiensis and An. quadriannulatus in the field. Med Vet Entomol. 2008;22:93–108.
Mayagaya VS, Nkwengulila G, Lyimo IN, Kihonda J, Mtambala H, Ngonyani H, et al. The impact of livestock on the abundance, resting behaviour and sporozoite rate of malaria vectors in southern Tanzania. Malar J. 2015;14:17.
Main BJ, Lee Y, Ferguson HM, Kreppel KS, Kihonda A, Govella NJ, et al. The genetic basis of host preference and resting behavior in the major African malaria vector, Anopheles arabiensis. PLoS Genet. 2016;12(9):e1006303.
Mbogo CM, Mwangangi JM, Nzovu J, Gu W, Yan G, Gunter JT, et al. Spatial and temporal heterogeneity of Anopheles mosquitoes and Plasmodium falciparum transmission along the kenyan coast. Am J Trop Med Hyg. 2003;68:734–42.
Lindblade KA, Gimnig JE, Kamau L, Hawley WA, Odhiambo F, Olang G, et al. Impact of sustained use of insecticide-treated bednets on malaria vector species distribution and culicine mosquitoes. J Med Entomol. 2006;43:428–32.
Bayoh MN, Mathias DK, Odiere MR, Mutuku FM, Kamau L, Gimnig JE, et al. Anopheles gambiae: historical population decline associated with regional distribution of insecticide-treated bed nets in western Nyanza Province, Kenya. Malar J. 2010;9:62.
Russell TL, Govella NJ, Azizi S, Drakeley CJ, Kachur SP, Killeen GF. Increased proportions of outdoor feeding among residual malaria vector populations following increased use of insecticide-treated nets in rural Tanzania. Malar J. 2011;10:80.
Mutuku FM, King CH, Mungai P, Mbogo C, Mwangangi J, Muchiri EM, et al. Impact of insecticide-treated bed nets on malaria transmission indices on the south coast of Kenya. Malar J. 2011;10:356.
Kitau J, Oxborough RM, Tungu PK, Matowo J, Malima RC, Magesa SM, et al. Species shifts in the Anopheles gambiae complex: do LLINs successfully control Anopheles arabiensis? PLoS ONE. 2012;7:e31481.
Derua YA, Alifrangis M, Hosea KM, Meyrowitsch DW, Magesa SM, Pedersen EM, et al. Change in composition of the Anopheles gambiae complex and its possible implications for the transmission of malaria and lymphatic filariasis in north-eastern Tanzania. Malar J. 2012;11:188.
Mwangangi JM, Mbogo CM, Orindi BO, Muturi EJ, Midega JT, Nzovu J, et al. Shifts in malaria vector species composition and transmission dynamics along the Kenyan coast over the past 20 years. Malar J. 2013;12:13.
Charlwood JD, Kessy E, Yohannes K, Protopopoff N, Rowland M, LeClair C. Studies on the resting behaviour and host choice of Anopheles gambiae and An. arabiensis from Muleba, Tanzania. Med Vet Entomol. 2018;32:263–70.
Dukeen MYH, Omer SM. Ecology of the malaria vector Anopheles arabiensis Patton (Diptera: Culicidae) by the Nile in northern Sudan. Bull Entomol Res. 1986;76:451–67.
Fontenille D, Lochouarn L, Diatta M, Sokhna C, Dia I, Diagne N, et al. Four years’ entomological study of the transmission of seasonal malaria in Senegal and the bionomics of Anopheles gambiae and A. arabiensis. Trans R Soc Trop Med Hyg. 1997;91:647–52.
Mendis C, Jacobsen JL, Gamage-Mendis A, Bule E, Dgedge M, Thompson R, et al. Anopheles arabiensis and An. funestus are equally important vectors of malaria in Matola coastal suburb of Maputo, southern Mozambique. Med Vet Entomol. 2000;14:171–80.
Yohannes M, Haile M, Ghebreyesus TA, Witten KH, Getachew A, Byass P, et al. Can source reduction of mosquito larval habitat reduce malaria transmission in Tigray, Ethiopia? Trop Med Int Health. 2005;10:1274–85.
Soma DD, Zogo B, Taconet P, Somé A, Coulibaly S, Baba-Moussa L, et al. Quantifying and characterizing hourly human exposure to malaria vectors bites to address residual malaria transmission during dry and rainy seasons in rural Southwest Burkina Faso. BMC Public Health. 2021;21:1–9.
Djènontin A, Bouraima A, Soares C, Egbinola S, Cottrell G. Human biting rhythm of Anopheles gambiae Giles, 1902 (Diptera: Culicidae) and sleeping behaviour of pregnant women in a lagoon area in Southern Benin. BMC Res Notes. 2021;14:1–7.
Huho B, Briët O, Seyoum A, Sikaala C, Bayoh N, Gimnig J, et al. Consistently high estimates for the proportion of human exposure to malaria vector populations occurring indoors in rural Africa. Int J Epidemiol. 2013;42:235–47.
Mbogo CNM, Baya NM, Ofulla AVO, Githure JI, Snow RW. The impact of permethrin-impregnated bednets on malaria vectors of the Kenyan coast. Med Vet Entomol. 1996;10:251–9.
Yohannes M, Boelee E. Early biting rhythm in the afro-tropical vector of malaria, Anopheles arabiensis, and challenges for its control in Ethiopia. Med Vet Entomol. 2012;26:103–5.
Pates H, Curtis C. Mosquito behavior and vector control. Annu Rev Entomol. 2005;50:53–70.
Zemene E, Belay DB, Tiruneh A, Lee MC, Yewhalaw D, Yan G. Malaria vector dynamics and utilization of insecticide-treated nets in low-transmission setting in Southwest Ethiopia: implications for residual transmission. BMC Infect Dis. 2021;21:1–11.
Ojuka P, Boum Y, Denoeud-Ndam L, Nabasumba C, Muller Y, Okia M, et al. Early biting and insecticide resistance in the malaria vector Anopheles might compromise the effectiveness of vector control intervention in Southwestern Uganda. Malar J. 2015;14:148.
Cooke MK, Kahindi SC, Oriango RM, Owaga C, Ayoma E, Mabuka D, et al. “A bite before bed”: exposure to malaria vectors outside the times of net use in the highlands of western Kenya. Malar J. 2015;14:1–15.
Williams J, Cowlishaw R, Sanou A, Ranson H, Grigoraki L. In vivo functional validation of the V402L voltage gated sodium channel mutation in the malaria vector An. gambiae. Pest Manag Sci. 2022;78:1155–63.
Beier JC, Killeen GF, Githure JI. Short report: Entomologic inoculation rates and Plasmodium falciparum malaria prevalence in Africa. Am J Trop Med Hyg. 1999;61:109–13.
Guglielmo F, Sanou A, Churcher T, Ferguson HM, Ranson H, Sherrard-Smith E. Quantifying individual variability in exposure risk to mosquito bites in the Cascades region, Burkina Faso. Malar J. 2021;20:44.
Sangbakembi-Ngounou C, Costantini C, Longo-Pendy NM, Ngoagouni C, Akone-Ella O, Rahola N, et al. Diurnal biting of malaria mosquitoes in the Central African Republic indicates residual transmission may be “out of control.” Proc Natl Acad Sci U S A. 2022;119:1–11.
Okumu F, Finda M. Key characteristics of residual malaria transmission in two districts in south-eastern Tanzania—implications for improved control. J Infect Dis. 2021;223:S143–54.
Paton DG, Childs LM, Itoe MA, Holmdahl IE, Buckee CO, Catteruccia F. Exposing Anopheles mosquitoes to antimalarials blocks Plasmodium parasite transmission. Nature. 2019;567:239–43.
Murray GPD, Lissenden N, Jones J, Voloshin V, Toé KH, Sherrard-Smith E, et al. Barrier bednets target malaria vectors and expand the range of usable insecticides. Nat Microbiol. 2020;5:40–7.
Sougoufara S, Ottih EC, Tripet F. The need for new vector control approaches targeting outdoor biting Anopheline malaria vector communities. Parasit Vectors. 2020;13:1–15.
Acknowledgements
We are grateful to the inhabitants of Goden village and CNRFP technicians for their collaboration during the whole course of this study.
Funding
The study was supported by Sapienza University of Rome, projects “Avvio alla Ricerca 2021” no. AR22117A76DC0132.
Author information
Authors and Affiliations
Contributions
WMG, EP, HR, AdT and MP conceived the study. WMG organized and supervised field collections. EP and EG carried out molecular analyses. EP, CP and MP analysed the entomological data. FG, EP and MP analysed the anthropological data. EP, AdT and MP drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study has been conducted upon the ethical approval of “Comité d’éthique pour la recherche en santé”, in agreement with Ministry of Health of Burkina Faso (approval no. 2020-7-134, issued on 1 July 2020). Volunteers chosen for mosquito samplings were local collaborators trained by CNRFP in performing landing collections in the village for several years. After the study, medical follow-up was conducted on the volunteers for 2 weeks. None showed any malaria symptoms. To ensure empty houses during HLC, the inhabitants of those houses were moved to another safe place and rewarded for their time. All mosquito collectors and inhabitants involved as household representatives were informed about the details of the study and signed informed consent to participate in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: S1.
a. Questionnaire, full version. b. Questionnaire limitations.
Additional file 2: S2.
a. GLM output. b. Species abundances according to date and position of sampling.
Additional file 3: S3.
a. GAM output. b. GAM predicted coefficients of A. coluzzii and A. arabiensis hourly abundances.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Perugini, E., Guelbeogo, W.M., Guglielmo, F. et al. The interplay between malaria vectors and human activity accounts for high residual malaria transmission in a Burkina Faso village with universal ITN coverage. Parasites Vectors 16, 101 (2023). https://doi.org/10.1186/s13071-023-05710-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13071-023-05710-7