Abstract
Background
In China, people infected with hepatitis B virus (HBV) are commonly found in areas with a high prevalence of Clonorchis sinensis, a trematode worm. Published studies have reported that the progression of hepatitis B is affected by coinfection C. sinensis.
Methods
Clinical data from a total of 72 patients with C. sinensis and HBV (as sole infection or with coinfections) and 29 healthy individuals were analysed. We also incubated the hepatic stellate cell line LX-2 with total proteins from C. sinensis adult worms (CsTPs) and HBV-positive sera. In addition, the human hepatoblastoma cell line HepG2.2.15 was treated with the antiviral drug entecavir (ETV), CsTPs and the anti-C. sinensis drug praziquantel (PZQ).
Results
Our clinical data indicated that the levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin (TB) and hyaluronic acid (HA) were significantly higher in patients with coinfection than in those infected with HBV only. In cell models, compared with the model in which LX-2 cells were incubated with HBV-positive sera (HBV group), transcripts of alpha-smooth muscle actin and types I and III collagen were significantly elevated in the models of LX-2 cells treated with CsTPs and HBV-positive sera (CsTP+HBV group), while the messenger RNA levels of tumour necrosis factor-α, interleukin (IL)-1β and IL-6 in the CsTP+HBV group were clearly lower. The HBV surface antigen and hepatitis B e-antigen levels were higher in the HepG2.2.15 cells treated with ETV and CsTPs than in those in the ETV group and in the cells administered a mixture of ETV, CsTPs and PZQ.
Conclusions
These results confirmed that C. sinensis and HBV coinfection could aggravate the progression of liver fibrosis. CsTPs might promote chronic inflammation of the liver in individuals with HBV infection, resulting in the development of hepatic fibrosis.
Graphic abstract

Similar content being viewed by others
Background
Adult Clonorchis sinensis worms inhabit the intrahepatic bile ducts of humans, causing the food-borne parasitic disease clonorchiasis [1]. It has been reported that approximately 15 million people are infected with C. sinensis globally, primarily in China, South Korea, northern Vietnam and the far east of Russia, with approximately 13 million of these cases in China, especially in Guangdong Province and the Guangxi Zhuang Autonomous Region of South China [2,3,4].
Hepatitis B virus (HBV) attacks liver cells, leading to hepatitis B. The WHO estimated that 296 million people were living with chronic hepatitis B in 2019, with 1.5 million new infections occurring each year. Approximately 15–25% of people with chronic HBV infection die from liver cirrhosis or hepatocellular carcinoma [5]; in 2019, an estimated 820,000 people died from HBV-related illnesses, presenting a serious public health problem. China belongs to the countries classified as medium prevalence areas, with an HBV surface antigen (HBsAg)-positive rate of 6.89% [6].
In China, people infected with HBV are commonly found in areas with a high prevalence of C. sinensis [7, 8]. The HBsAg-positive rate has been documented to be significantly higher in endemic areas of C. sinensis than in nonendemic areas [9, 10]. It is generally accepted that dysfunctional immune responses play an essential role in persistent HBV infection, as well as liver inflammation and hepatic fibrosis [11]. Adult parasites can trigger type 2 or mixed type 1/type 2 immune responses in the host [12]. Clonorchis sinensis infection also induces the activation of CD4+ lymphocytes, including T helper 1/2/17 (Th1/Th2/Th17) cells and regulatory T (Treg) cells, in FVB mice [13]. In our previous study, we found that patients coinfected with C. sinensis and HBV showed higher serum interleukin (IL)-6 and IL-10 levels and lower serum interferon gamma (IFN-γ) levels, suggesting that coinfection could exacerbate the imbalance of Th1/Th2 cytokines [14]. These results also indicated that C. sinensis coinfection might regulate immune responses and then affect the progression of hepatitis B as well as liver fibrosis.
In the current study, we investigated further the effects of coinfection on liver fibrosis by analysing clinical liver indices and using a cell model to detect the levels of fibrosis-related molecules and cytokines. Previously, we also found that coinfected patients presented weaker liver function and higher numbers of HBV DNA copies. In addition, combination treatment of coinfected patients with antiviral (entecavir [ETV]) and anti-C. sinensis drugs (praziquantel [PZQ]) could contribute to a reduction in viral load and facilitate the recovery of liver function. In the present study, we also analysed the effect of ETV and/or PZQ on a cell model to confirm the above effects.
Methods
Study population
The study population comprised 72 patients with HBV, C. sinensis or both infections diagnosed at the Third Affiliated Hospital of Sun Yat-sen University and 29 healthy individuals serving as healthy controls (HCs), who were enrolled in parallel. The enrolled men and women were aged ≥ 18 years. The participants were divided into four groups: (i) the coinfection group (n = 22), including patients who were positive for both C. sinensis eggs and HBsAg with HBV DNA > 20 IU/ml; (ii) the HBV group (n = 26), including patients who were HBsAg-positive with HBV DNA > 20 IU/ml; (iii) the C. sinensis group (n = 24), including patients who were positive for C. sinensis eggs only; and (iv) the HC group, including individuals matched for age and sex (n = 29). Patients with the following conditions were excluded: coinfection with hepatitis A, C, D or E, human immunodeficiency virus, Schistosoma japonicum, Schistosoma mansoni or other parasites; hepatitis B cirrhosis; alcoholic liver disease; autoimmune diseases; serious heart diseases; malignant tumours; cholestasis; diabetes. Pregnant women were also excluded.
Biochemical and serological testing
The levels of hyaluronic acid (HA), type III procollagen (PCIII), type IV collagen (COLIV) and laminin (LN) in sera were measured using a BL-9600 Micropore Plate Chemiluminescent Immunity Analyser (Bell Medical Electronics Ltd., Tianjin, China). The presence of HBV DNA was tested by real-time PCR with a lower detection limit of 20 IU/ml (Roche Diagnostics, Mannheim, Germany). Serum HBsAg and hepatitis B e-antigen (HBeAg) were detected using an electrochemiluminescence immunoassay (ECLI) kit for the COBAS-e801 system (Roche Diagnostics). The enzymatic activity levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST) and total bilirubin (TB) were tested with automated biochemical techniques (Hitachi 7600 automatic biochemical analyser; Hitachi Ltd., Tokyo, Japan).
Collection of total proteins from C. sinensis adults before and after treatment with PZQ
Freshly collected adult worms of C. sinensis were gently rinsed several times with phosphate-buffered saline (PBS, pH 7.2) supplemented with penicillin and streptomycin (100 U/ml and 100 μg/ml, respectively; Gibco Life Technologies, Thermo Fisher Scientific, Waltham, MA, USA) and identified using previously reported protocols [15]. The worms were then lysed in 1 ml of PBS at an oscillation frequency of 30 Hz for 10 min. The supernatant containing total proteins extracted from C. sinensis adults (CsTPs) was harvested and centrifuged at 4000 rpm for 15 min at 4 °C. CsTPs were filtered through a sterile 0.22-μm syringe filter and stored at − 80 °C after quantification until use [16]. The protein concentration was detected using a BCA Protein Assay Kit (Thermo Fisher Scientific).
PZQ is a pyrazinoquinoline compound that is effective for treating patients with trematode infections, including C. sinensis, and is commonly used to treat patients with such infections. It has been proposed that this compound may affect the tegument and musculature of the worm. In this study, 1 mg of PZQ (GKH Pharmaceutical, Ltd., Guangzhou, China) was dissolved in 1 ml of PBS containing 60% dimethyl sulfoxide and then diluted with PBS to final concentrations of 0.1, 1 and 10 μg/ml, respectively [17, 18]. The PZQ solutions were successively filtered through a sterile 0.22-μm syringe filter. Ten active C. sinensis adult worms that had been cleaned were treated with the different concentrations of PZQ in Dulbecco's Modified Eagle Medium (DMEM; Gibco Life Technologies, Thermo Fisher Scientific) in vitro for 12, 24 or 48 h. CsTPs from the treated adults were collected using the methods mentioned above.
Coeffects of CsTPs and HBV on human hepatic stellate cell line LX-2
LX-2 cells (1 × 104 cells/ml) were incubated with different concentrations of CsTPs (0, 20, 40, 80 μg/ml) or HBV-positive sera with different numbers of HBV DNA copies (0, 1.0 × 108, 2.0 × 108 or 4.0 × 108 HBV DNA IU/ml) for 24 h in a round-bottomed 96-well plate (Costar®; Corning Ltd., Corning, NY, USA). LX-2 cells in 0.5 μg/ml bovine serum albumin (BSA; MBCHEM, Shanghai, China) in RPMI 1640 medium (Gibco Life Technologies, Thermo Fisher Scientific) were used as blank controls, and LX-2 cells in RPMI 1640 medium with HBV-negative sera from healthy individuals were used as negative controls. Cell proliferation was assessed by measuring optical density at 450 nm (OD450) using the Cell Counting Kit 8 Assay (CCK-8 assay; Dojindo Laboratories, Kumamoto, Japan) to determine the optimal concentration of CsTPs or HBV DNA copies with the strongest effects.
An aliquot of 2.0 × 105/ml viable LX-2 cells in RPMI 1640 medium was seeded into 6-well cell culture clusters and incubated for 24 h at 37 °C under 5% CO2 in an incubator with HBV-positive sera (2.0 × 108 HBV DNA IU/ml), CsTPs (40 μg/ml) or both (CsTP+HBV group). LX-2 cells in RPMI 1640 medium treated with HBV-positive sera (2.0 × 108 HBV DNA IU/ml) and 0.5 μg/ml BSA) were used as a control group (BSA+HBV group). Cells incubated with PBS or HBV-negative sera in RPMI 1640 medium were used as a blank control. Total RNA was extracted from LX-2 cells from each group using TRIzol reagent (TransGen Biotech Co. Ltd., Beijing, China). Complementary DNAs (cDNAs) were then synthesized using a TransScript All-in-One First-Strand cDNA Synthesis SuperMix for qPCR (One-Step gDNA Removal Kit; TransGen Biotech Co. Ltd.) from 1 μg of total RNA according to the manufacturer’s protocol. Quantitative real-time PCR (Q-PCR) was performed on a CFX96 Real-Time PCR Detection System (Bio-Rad Laboratories, Hercules, CA, USA) using TransStart Top/Tip Green qPCR SuperMix (TransGen Biotech Co. Ltd.). The PCR cycling conditions were: a denaturation step at 94 °C for 30 s, followed by 40 cycles of 94 °C for 5 s, 60 °C for 30 s, 95 °C for 5 s, with a final cycle at 60 °C for 10 s. The messenger RNA (mRNA) levels of alpha-smooth muscle actin (α-SMA), types I and III collagen, tumour necrosis factor alpha (TNF-α), IL-1β and IL-6 were analysed by calculating 2−ΔΔCt and normalizing to β-actin mRNA. All primers for Q-PCR are shown in Additional file 1: Table S1. All assays were performed in triplicate and repeated twice.
HBsAg, HBeAg and HBV DNA copies of the treated hepatoma cell line HepG2.2.15
The HepG2.2.15 cell line is characterized by stable HBV expression and replication in the culture system. It is an effective model for screening for anti-HBV drugs in vitro and studying the structure, function, gene expression and regulation of HBV DNA [19]. Moreover, it has been documented that anti-helminth drugs such as albendazole could affect the enzymatic activity of excretory-secretory products of cestodes [20]. In this study, HepG2.2.15 cells were employed to analyse the effects of ETV with or without CsTPs pretreated with PZQ on HBV.
A total of 5.0 × 104 viable HepG2.2.15 cells seeded into 12-well plates containing 200 μl of DMEM were treated with one of the following treatments: (i) 30 nmol/ml ETV (Selleck Chemicals, Houston, TX, USA); (ii) 30 nmol/ml ETV and 40 μg/ml CsTPs (ETV+CsTPs); (iii) 40 μg/ml CsTPs; (iv) 0.5 μg/ml BSA and 30 nmol/ml ETV (ETV+BSA); or (v) ETV (30 nmol/ml) and CsTPs (40 μg/ml) pretreated with 0.1, 1 or 10 μg/ml PZQ (ETV+CsTP+PZQ), for 12, 24 or 48 h at 37 °C in 5% CO2 in an incubator. The concentrations of ETV, CsTPs and BSA used were based on our published study [16]. Finally, HBsAg, HBeAg and HBV DNA copies in the supernatants from each group were analysed using ECLI and Q-PCR. All assays were performed in triplicate and repeated twice.
Statistical analysis
All data are presented as the mean ± standard error (SE) or the median and range. Data analyses were carried out using GraphPad Prism software 7.0 (GraphPad Software, San Diego, CA, USA). One-sided paired Student’s t-test was used. The Kruskal‒Wallis rank test or one-way analysis of variance test was conducted for comparisons with more than two groups. P-values < 0.05 were considered to be statistically significant.
Results
Clinical characteristics of the study groups
Patients in both the C. sinensis group and the HBV group were found to have higher serum levels of ALT, AST, HA and PCIII than those in the HC group (P < 0.05, respectively). Serum levels of ALT, AST, TB and HA were significantly higher in the coinfection group than in both the HBV group and the C. sinensis group (P < 0.05). There was no difference in the number of HBV DNA copies or PCIII, LN and COLIV levels between the coinfection group and the HBV group (P > 0.05). The clinical data are shown in detail in Table 1.
Proliferation assay of LX-2 cells
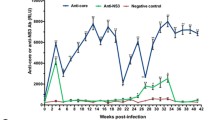
LX-2 cells were cultured with different concentrations (0, 20, 40 or 80 μg/ml) of CsTPs or with HBV-positive sera with different HBV DNA copy numbers (0, 1.0 × 108, 2.0 × 108 or 4.0 × 108 HBV DNA IU/ml, respectively). The highest OD450 value of LX-2 cells was recorded following the incubation of the cells with 40 μg/ml CsTPs or with serum containing 2 × 108 IU/ml HBV DNA, according to the CCK-8 assay, suggesting the strongest proliferation (Fig. 1). In addition, no significant difference in cell proliferation was observed in the 0.5 μg/ml BSA-treated group. Subsequently, 40 μg/ml CsTPs and serum containing 2 × 108 IU/ml HBV DNA were employed to investigate the coeffects of CsTPs and HBV on LX-2 cells. Cells incubated with 0.5 μg/ml BSA were used as a control.
Cell proliferation of human hepatic stellate cell line LX-2 determined using the CCK-8 assay. LX-2 cells were cultured with different concentrations of CsTPs (a), HBV DNA-positive sera (b) or a mixture of CsTPs and HBV DNA-positive sera (c) for 24 h. Cells treated with phosphate-buffered saline or 0.5 µg/ml BSA were used as controls. Data are presented as mean values ± standard errors (SEs). Statistical significance was analysed by one-sided paired Student’s t-test, and asterisks indicate significance vs the Control group at *P < 0.05, ***P < 0.001 BSA, Bovine serum albumin; CsTPs total proteins extracted from adult Clonorchis sinensis; HBV, hepatitis B virus
mRNA levels of molecules related to hepatic fibrosis in treated LX-2 cells
The mRNA levels of α-SMA and types I and III collagen were significantly higher in both the CsTP group and the HBV group than in the HBV-negative group and the BSA control groups (P < 0.05). Transcripts of α-SMA and types I and III collagen were significantly elevated in the CsTP+HBV group compared with the HBV group (P < 0.05). The mRNA levels of α-SMA and types I and III collagen were higher in the CsTP+HBV group than in the BSA+HBV group, with the first two factors showing significant increases (P < 0.01) (Fig. 2).
mRNA levels of α-SMA (a), collagen I (b) and collagen III (c) in LX-2 cells by Q-PCR. LX-2 cells were stimulated by CsTPs, HBV positive serum, or a mixture of CsTPs and HBV positive serum (CsTP+HBV). LX-2 cells treated with HBV negative sera, BSA, or a mixture of BSA and HBV positive serum (BSA+HBV) were used as control groups. Specific primers were used to amplify the transcripts of related molecules from total RNAs of the LX-2 cells from each group by Q-PCR. mRNA levels were normalized relative to the β-actin expression. Data were shown as the mean values ± standard errors. Analysis by one-way ANOVA test indicated significant differences among the different groups (*P < 0.05, **P < 0.01, ***P < 0.001 vs the control group. +P < 0.05, ++P < 0.01, +++P < 0.001 vs the CsTP+HBV group)
mRNA levels of related inflammatory cytokines in treated LX-2 cells
Compared with the levels of TNF-α and IL-1β mRNA in the blank controls (cells incubated with HBV-negative sera or PBS), those in the HBV group and the BSA+HBV group were clearly elevated (P < 0.01), but not in the CsTP group (P > 0.05). The levels of IL-6 transcripts in all groups were substantially increased compared with those in the blank control group. Compared with the CsTP+HBV group, the HBV group had strongly increased levels of TNF-α, IL-1β and IL-6 mRNA (P < 0.01). In addition, the transcription levels of TNF-α and IL-1β in the BSA+HBV group were significantly elevated compared with those in the CsTP+HBV group (P < 0.001). There was no significant difference in the levels of TNF-α, IL-1β and IL-6 mRNA between the HBV group and the BSA+HBV group (Fig. 3).
mRNA levels of TNF-α (a), IL-1β (b) and IL-6 (c) in LX-2 cells by Q-PCR. LX-2 cells were incubated with CsTPs, HBV positive serum, or a mixture of CsTPs and HBV positive serum (CsTP+HBV). Cells treated with HBV negative sera, PBS, or a mixture of BSA and HBV positive serum (BSA+HBV) were used as controls. Specific primers were used to amplify the transcripts of related molecules from total RNAs of LX-2 cells in each group by Q-PCR. mRNA levels were normalized relative to β-actin expression. Data were shown as the mean values ± standard errors. Statistical significance was analyzed by one-way ANOVA test (*P < 0.05, **P < 0.01, ***P < 0.001 vs control group; +P < 0.05, ++P < 0.01, +++P < 0.001 vs the CsTP+HBV group)
HBsAg, HBeAg and HBV DNA copy levels of treated HepG2.2.15 cells
After 12, 24 and 48 h of incubation, HBsAg and HBeAg levels were significantly higher in the culture supernatants of HepG2.2.15 cells in the ETV+CsTP group than in those of the ETV group or the ETV+BSA group (P < 0.05). Moreover, HBsAg and HBeAg levels were predominantly lower in all ETV+CsTP+PZQ groups than in the ETV+CsTP group (P < 0.01). There was no significant difference between the ETV group and the ETV+BSA group (Fig. 4a, b).
Detection of HBsAg, HBeAg and HBV DNA copies in the supernatant of HepG2.2.15 cells. HepG2.2.15 cells were incubated with ETV, CsTPs, a mixture of ETV and CsTPs (ETV+CsTP), a mixture of ETV and BSA (ETV+BSA) or a mixture of ETV and CsTPs, respectively pretreated with 0.1, 1 or 10 μg/ml PZQ (ETV+CsTP[PZQ]). In the supernatants of HepG2.2.15 cells, levels of HBsAg (a) and HBeAg (b) were detected by electrochemiluminescence immunoassay, and HBV DNA copies (c) were detected by Q-PCR, at the indicated time points (12, 24 and 48 h). Data were presented as mean values ± SEs. Analysis by one-way ANOVA test indicated significant differences among the different groups at ***P < 0.001 vs the ETV+CsTP group. BeAg, HBV e-antigen; HBsAg, HBV surface antigen; ETV, entecavir; PZQ, praziquantel
HBV DNA copies in the supernatant of cells in the ETV+CsTP group increased slightly compared with those in the ETV group or the ETV+CsTP + PZQ (1 μg/ml) group at 12, 24 and 48 h after administration, but there was no significant difference among the three groups. Moreover, there was no significant difference in HBV DNA copies between the ETV group and the ETV+BSA group (Fig. 4c).
Discussion
In the present study, our clinical data indicated that the levels of ALT, AST, TB and HA were significantly higher in patients with coinfection than in HBV-infected patients. In the cell models, the results showed that transcripts of α-SMA and types I and III collagen were significantly elevated in the CsTP+HBV group compared with the HBV group. The levels of TNF-α, IL-1β and IL-6 mRNA in the CsTP + HBV group were clearly lower than those in the HBV group. HBsAg and HBeAg levels in the ETV+CsTP group were higher than those in the ETV group and in the ETV+CsTP+PZQ group.
The serum marker enzymes ALT and AST are known to be important diagnostic factors for hepatic diseases, and their increased activity in the circulation reflects damage and leakage of hepatocytes. A high TB level is a sign of liver disease. Analysis of the ALT, AST and TB levels in sera from patients demonstrated that C. sinensis and HBV coinfection could weaken liver function more than HBV infection alone, which further confirmed our previous finding [14]. Our analysis showed that the levels of HA and COLIV were higher in the coinfection group than in the HBV group, but HA increased significantly. The serum indices of HA, LN, PC III and COL IV can effectively reflect the condition of liver injury and fibrosis, and they are commonly used as clinical indicators to reflect liver fibrosis [21]. HA is a component of the extracellular matrix (ECM) of the liver [22], and serum HA levels correlate well with the severity of liver dysfunction in patients with chronic liver disease [23, 24]. It has been reported that almost 90% of circulating HA is degraded in the liver by Ito cells and sinusoidal cells and, therefore, hepatic dysfunction deteriorates HA clearance [25]. It has been repeatedly found that HA is the most sensitive marker among the four serum indicators of liver fibrosis [26,27,28]. We found that the HA level was significantly higher in the coinfection group than in the HBV group or the C. sinensis group. These results suggested that coinfection might aggravate the progression of liver fibrosis.
Hepatic stellate cells (HSCs) localize to the perisinusoidal space between hepatocytes and sinusoidal endothelial cells. In response to liver injury, inflammatory mediators promote HSC activation. Once activated, HSCs become proliferative, subsequently differentiate into myofibroblasts and then accumulate ECM that drives the fibrogenic process [29]. HSCs play a central role in liver fibrosis by generating fibrotic mediators [30, 31]. When quiescent HSCs were activated by various liver stimuli, a new myofibroblastic phenotype with increased expression of ECM proteins, including collagen I and collagen III and α-SMA, was obtained [32, 33]. Activated human HSCs can produce inflammatory cytokines, such as TNF-α, IL-1β and IL-6. These inflammatory cytokines are potent pleiotropic cytokines that can trigger multiple signalling pathways involved in inflammation, proliferation and apoptosis [34,35,36]. Moreover, they are essential for liver inflammation, and sustained liver inflammation leads to liver fibrosis. Therefore, in the current study, the human HSC cell line LX-2 [37] was employed to investigate the effects of coinfection on liver fibrosis in vitro.
It has been documented that some antigens from parasites can play important roles in proinflammatory or anti-inflammatory activities [38,39,40]. We previously revealed that CsTPs could promote the production of Th2 cytokines, including IL-13 and IL-4, both in vitro and in vivo, and ultimately resulted in the development of liver fibrosis [16]. During the parasitic period, proteins from the tegument of adult worms, eggs and excretory-secretory proteins excluded from worm bodies and proteins from the decomposition of dead worms all participate in the interaction between the worms and the host, so CsTPs were employed to carry out the investigation in vitro.
We found that the mRNA levels of α-SMA, collagen I and collagen III in the LX-2 cells stimulated by either CsTPs or HBV-positive sera could be significantly increased compared with those in the control groups (HBV-negative group and BSA group). It has been documented that the HBV X protein and HBsAg can directly upregulate the expression of α-SMA and collagen I [41, 42]. We previously found that CsTPs could also directly stimulate the proliferation of LX-2 cells and activate them [43, 44]. This change might result in the levels of α-SMA and types I and III collagen being notably elevated in response to mixtures of CsTPs and HBV-positive sera compared with those in the HBV group or BSA+HBV group. However, there was no difference between the HBV group and the BSA+HBV group. When quiescent HSCs were activated by various liver stimuli, a new myofibroblastic phenotype with increased ECM protein expression, including the expression of types I and III collagen and α-SMA, was obtained [33, 45]. Our results demonstrated that molecules from either HBV or C. sinensis could activate HSCs and improve the generation of ECM components. Moreover, the activation effect of HSCs induced by a mixture of HBV and CsTPs was more conspicuous compared to that of the other groups. Combined with the finding that HA levels in sera from the HBV and C. sinensis coinfection group were significantly higher, this result suggested that coinfection could aggravate the development of hepatic fibrosis.
During activation, HSCs lose the ability to express hepatocyte growth factor but they do produce several other growth factors, cytokines and chemokines, such as IL-6, TNF-α, transforming growth factor beta (TGF-β), monocyte chemotactic protein 1 and cytokine-induced neutrophil chemoattractant, that participate in the initiation and progression of liver disease [46]. Incubation of quiescent HSCs with lipopolysaccharide (LPS) increases the synthesis of the proinflammatory cytokines IL-6, TNF-α and IL-1β [47, 48]. In our study, the levels of TNF-α, IL-1β and IL-6 mRNA in LX-2 cells from the HBV group increased substantially in comparison with those from the blank control groups (LX-2 cells treated with HBV-negative sera or BSA). In the acute phase of an infection, plasma levels of the inflammatory cytokines TNF-α, IL-1β and IL-6 increase, followed by enhanced secretion of acute-phase proteins that contribute to antimicrobial defence. Based on this result, we suggest that HBV proteins could act as stimuli and clearly promote the generation of proinflammatory cytokines in LX-2 cells. Our previous study showed that Th2-type cytokines increased in the liver tissue of CsTP-immunized mice [16]. Th2-type cytokines have more of an anti-inflammatory response, and this increase might explain why there was no significant difference in the transcriptional levels of TNF-α and IL-1β between the CsTP group and the blank group and why the levels of proinflammatory cytokines in the CsTP+HBV group were significantly lower than those in the HBV group. IL-6 is the major inducer of hepatic acute phase proteins, and its synthesis and secretion are induced during inflammatory conditions, such as following the stimulation of Toll-like receptor (TLR)-4 by LPS or upon stimulation of cells by IL-1 or TNF-α [49]. Our results showed that the transcriptional level of IL-6 in the CsTP group was significantly elevated in comparison with that in the blank control group. Combined with our previous finding [16], these results suggested that the increase in IL-6 was mainly due to CsTPs acting as pathogen-associated molecular patterns rather than being induced by IL-1 or TNF-α.
IL-6 can directly induce the transition of HSCs towards myofibroblast-like cells and promote collagen secretion in HSCs [50]. During liver fibrosis, HSCs are a cellular source of IL-6 [51], which may might partly contribute to the elevation of α-SMA and type I and III collagens in HBV-positive sera and/or CsTP-treated LX-2 cells. Our results showed that the levels of proinflammatory cytokines in the CsTP+HBV group were lower than those in the HBV group, while the levels of liver fibrosis-related molecules in the CsTP+HBV group were higher than those in the HBV group. Excessive proinflammatory responses can lead to uncontrolled tissue damage, while Th2 responses counteract inflammatory cytokine-mediated microbicidal action. Hepatic fibrosis is the wound-healing response of the liver to many causes of chronic injury. This result suggested that CsTPs might weaken the inflammatory response and perpetuate chronic inflammation in the liver so that coinfection could exacerbate the development of hepatic fibrosis. Clonorchis sinensis infection might lead to the chronicity of HBV infection. This finding should be further confirmed in the future.
We previously found that compared to sera of coinfected patients treated with only one cycle of ETV, sera of coinfected patients treated with a combined antiviral drug (ETV) and anti-C. sinensis drug (PZQ) (combination therapy) had lower levels of HBV DNA copies and TB levels [52]. In the present study, a HepG2.2.15 cell model was adopted to explore the efficacy of different treatment strategies in vitro. HepG2.2.15 cells stably transfected with the HBV genome have been frequently used in studies of HBV infection and drug treatment [53]. ETV, an inhibitor of HBV DNA polymerase, is an antiviral medication used in the treatment of HBV infection. ETV treatment has been approved as a safe and effective nucleoside therapy in patients with HBeAg-positive chronic hepatitis [54]. In the cytoplasm, HBsAg connects with the HBV genome and creates a complete viral particle. Decreased HBsAg synthesis leads to the intracellular inhibition of virus production [55]. HBeAg is a serologic marker associated with high levels of viral replication and infectivity, and HBV DNA is a quantitative virologic marker reflecting HBV replication level. In vitro, our results showed that the levels of HBsAg and HBeAg were predominantly elevated in the ETV+CsTP group compared with the ETV group. The level of HBV DNA copies was higher in the ETV+CsTP group than in the ETV group, but the difference was not statistically significant. This result demonstrated that CsTPs could weaken the effects of ETV. A possible dissociation between HBeAg and HBV DNA levels has been detected previously [56]. In addition, the immune response is necessary for the inhibition of HBV DNA replication [57, 58]. Therefore, conspicuous changes in HBV DNA copies could not be observed in the cell model, possibly explaining why there was no significant difference in HBV DNA copies between the ETV+CsTP group and the ETV+CsTP+PZQ group. The levels of HBsAg and HBeAg were significantly lower in the ETV+CsTP+PZQ group than in the ETV+CsTP group at 12, 24 and 48 h after administration. PZQ is the preferred drug against C. sinensis and other parasitic flatworm infections [59]. It has been documented that PZQ can inhibit lactate dehydrogenase activity of Cotylophoron cotylophorum and Taenia asiatica in vitro [60, 61]. It has also recently been documented that PZQ activates a transient receptor potential melastatin ion channel (TRPMPZQ) in schistosomes by engaging a hydrophobic ligand binding pocket within the voltage sensor-like domain of the channel to cause calcium entry and worm paralysis [62]. The homologues in C. sinensis might be influenced by PZQ, which successively reversed the effects of CsTPs on the expression of HBsAg and HBeAg in the supernatant of HepG2.2.15 cells. These results also suggested that CsTPs might directly affect HepG2.2.15 cells but does not depend on the immune response. The involved mechanism should be further investigated.
Conclusions
Collectively, the clinical liver indices, including ALT, AST, TB and HA, were significantly higher in patients with coinfection than in HBV-infected patients. Moreover, α-SMA and types I and III collagen were dominantly elevated in the LX-2 cell model treated with CsTPs and HBV-positive sera. Taken together, these findings confirm that C. sinensis and HBV coinfection could aggravate the progression of liver fibrosis. The present study showed that the levels of TNF-α, IL-1β and IL-6 mRNA were clearly lower in the HepG2.2.15 cell model incubated with CsTPs and HBV-positive sera. Combined with the observation coinfection could exacerbate the imbalance of Th1/Th2 cytokine in our previous study, these results suggest that coinfection might promote hepatic fibrosis by perpetuating chronic liver inflammation. Moreover, CsTPs could weaken the effects of ETV on HepG2.2.15 cell. Our study will broaden our understanding of the relationship between C. sinensis and HBV. Therefore, the importance of C. sinensis infection in hepatitis B patients should be realized. Our research also provids useful information for physicians to carry out individualized treatment in hepatitis B patients in endemic areas of C. sinensis.
Availability of data and materials
The data supporting the conclusions of this article are included within the article.
Abbreviations
- ALT:
-
Alanine aminotransaminase
- AST:
-
Aspartate aminotransferase
- CsTPs:
-
Total proteins extracted from adult C. sinensis
- COLIV:
-
Type IV collagen
- ECLI:
-
Electrochemiluminescence immunoassay
- ECM:
-
Extracellular matrix
- ETV:
-
Entecavir
- HA:
-
Hyaluronic acid
- HBeAg:
-
Hepatitis B e-antigen
- HBsAg:
-
Hepatitis B surface antigen
- HBV:
-
Hepatitis B virus
- HSCs:
-
Hepatic stellate cells
- IL-1β:
-
Interleukin-1β
- LN:
-
Laminin
- LPS:
-
Lipopolysaccharide
- PBS:
-
Phosphate-buffered saline
- PCIII:
-
Type III procollagen
- PZQ:
-
Praziquantel
- Q-PCR:
-
Quantitative real-time PCR
- α-SMA:
-
Alpha-smooth muscle actin
- TB:
-
Total bilirubin
- TNF-α:
-
Tumour necrosis factor-α
- TLR:
-
Toll-like receptor
References
Qian M-B, Utzinger J, Keiser J, Zhou X-N. Clonorchiasis. Lancet. 2016;387:800–10.
Deng ZH, Fang YY, Zhang QM, Mao Q, Pei FQ, Liu MR. The control of clonorchiasis in Guangdong province, southern China. Acta Trop. 2020;202:105246.
Na BK, Pak JH, Hong SJ. Clonorchis sinensis and clonorchiasis. Acta Trop. 2020;203:105309.
Wang D, Young ND, Korhonen PK, Gasser RB. Clonorchis sinensis and clonorchiasis: the relevance of exploring genetic variation. Adv Parasitol. 2018;100:155–208.
Nelson NP, Easterbrook PJ, McMahon BJ. Epidemiology of hepatitis B virus infection and impact of vaccination on disease. Clin Liver Dis. 2016;20:607–28.
Wang H, Men P, Xiao Y, Gao P, Lv M, Yuan Q, et al. Hepatitis B infection in the general population of China: a systematic review and meta-analysis. BMC Infect Dis. 2019;19:811.
Shi Y, Jiang Z, Yang Y, Zheng P, Wei H, Lin Y, et al. Clonorchis sinensis infection and co-infection with the hepatitis B virus are important factors associated with cholangiocarcinoma and hepatocellular carcinoma. Parasitol Res. 2017;116:2645–9.
Gao Y, Li Y, Liu X, Zhang T, Yu G, Wang Y, et al. High prevalence of Clonorchis sinensis infections and coinfection with hepatitis virus in riverside villages in northeast China. Sci Rep-Uk. 2020;10:11749.
Xie F. Clinical significance of Clonorchis sinensis antibodies dectection in HBV. Chinese J Parasitic Dis Control. 2005;2:95–8 (in Chinese).
Mou H, Wang L, Wang J, Jin B, Jin H. Discussion on clonorchiasis and HBV. Heilongjiang Med J Pharm. 2009;32:94.
Meng Z, Chen Y, Lu M. Advances in targeting the innate and adaptive immune systems to cure chronic hepatitis B virus infection. Front Immunol. 2020;10:3127. https://doi.org/10.3389/fimmu.2019.03127.
Koda S, Zhu X, Zheng K, Yan C. Molecular mechanisms of Clonorchis sinensis-host interactions and implications for vaccine development. Front Cell Dev Biol. 2022;9:781768. https://doi.org/10.3389/fcell.2021.781768.
Kong D, Li X, Zhang B, Yan C, Tang R, Zheng K. The characteristics of CD4(+)T-helper cell subset differentiation in experimental Clonorchis sinensis-infected FVB mice. Iran J Basic Med Sci. 2020;23:1538–43.
Li W, Dong H, Huang Y, Chen T, Kong X, Sun H, et al. Clonorchis sinensis co-infection could affect the disease state and treatment response of HBV patients. Plos Neglect Trop D. 2016;10:e4806.
Wang X, Chen W, Huang Y, Sun J, Men J, Liu H, et al. The draft genome of the carcinogenic human liver fluke Clonorchis sinensis. Genome Biol. 2011;12:R107.
Zhao L, Shi M, Zhou L, Sun H, Zhang X, He L, et al. Clonorchis sinensis adult-derived proteins elicit Th2 immune responses by regulating dendritic cells via mannose receptor. PLoS Negl Trop Dis. 2018;12:e6251.
Chai J. Praziquantel treatment in trematode and cestode infections: an update. Infect Chemother. 2013;45:32–43.
Hines-Kay J. Transcriptional analysis of Schistosoma mansoni treated with sub-lethal doses of the anthelmintic drug praziquantel. MSc thesis. Albuquerque: University of New Mexico; 2011.
Xiao Y, Liu C, Tang W, Zhang H, Chen X. Evans blue inhibits HBV replication through a dual antiviral mechanism by targeting virus binding and capsid assembly. Front Microbiol. 2019;10:2638. https://doi.org/10.3389/fmicb.2019.02638.
Adnani Sadati SJ, Farahnak A, Molaei Rad MB, Golestani A, Eshraghiyan MR. A comparison between the effects of albendazole and mebendazole on the enzymatic activity of excretory/secretory products of Echinococcus granulosus protoscoleces in vitro. Iran J Public Health. 2016;45:223–9.
Li Z, Cao H, Yao M, Lei X. Effect of acupuncture combined with Shenqi Yigan Decoction on liver function and T cell subsets in patients with HBV-induced liver fibrosis. Am J Transl Res. 2021;13:3409–17.
Königshofer P, Hofer BS, Brusilovskaya K, Simbrunner B, Petrenko O, Wöran K, et al. Distinct structural and dynamic components of portal hypertension in different animal models and human liver disease etiologies. Hepatology. 2022;75:610–22.
Enomoto H, Bando Y, Nakamura H, Nishiguchi S, Koga M. Liver fibrosis markers of nonalcoholic steatohepatitis. World J Gastroentero. 2015;21:7427–35.
Matsumoto T, Aoki T, Shimizu T, Park KH, Shiraki T, Sakuraoka Y, et al. Prognostic significance of preoperative hyaluronic acid level in patients with hepatocellular carcinoma. HPB (Oxford). 2022;24:525–34.
Wong VS, Hughes V, Trull A, Wight DGD, Petrik J, Alexander GJM. Serum hyaluronic acid is a useful marker of liver fibrosis in chronic hepatitis C virus infection. J Viral Hepatitis. 1998;5:187–92.
Gudowska M, Gruszewska E, Panasiuk A, Cylwik B, Flisiak R, Świderska M, et al. Hyaluronic acid concentration in liver diseases. Clin Exp Med. 2016;16:523–8.
Tran A, Hastier P, Barjoan EM, Demuth N, Pradier C, Saint-Paul MC, et al. Non invasive prediction of severe fibrosis in patients with alcoholic liver disease. Gastroenterol Clin Biol. 2000;24:626–30.
Jin H, Li Z. Correlation between serum hyaluronic acid and HBV DNA levels in patients with hepatitis B-associated cirrhosis. Shijie Huaren Xiaohua Zazhi. 2012;20:229–32.
Li D, He L, Guo H, Chen H, Shan H. Targeting activated hepatic stellate cells (aHSCs) for liver fibrosis imaging. Ejnmmi Res. 2015;5:71.
Sherman MH. Stellate cells in tissue repair, inflammation, and cancer. Annu Rev Cell Dev Biol. 2018;34:333–55.
Puche JE, Saiman Y, Friedman SL. Hepatic stellate cells and liver fibrosis. Compr Physiol. 2013;3:1473–92.
Mallat A, Lotersztajn S. Cellular mechanisms of tissue fibrosis 5 novel insights into liver fibrosis. Am J Physiol Cell Physiol. 2013;305:789–99.
Parola M, Pinzani M. Liver fibrosis: Pathophysiology, pathogenetic targets and clinical issues. Mol Aspects Med. 2019;65:37–55.
Friedman SL. Hepatic stellate cells: protean, multifunctional, and enigmatic cells of the liver. Physiol Rev. 2008;88:125–72.
Yang YM, Seki E. TNFα in liver fibrosis. Curr Pathobiol Rep. 2015;3:253–61.
Robert S, Gicquel T, Bodin A, Lagente V, Boichot E. Characterization of the MMP/TIMP imbalance and collagen production induced by IL-1β or TNF-α release from human hepatic stellate cells. PLoS ONE. 2016;11:e153118.
Xu L, Hui AY, Albanis E, Arthur MJ, O’Byrne SM, Blaner WS, et al. Human hepatic stellate cell lines, LX-1 and LX-2: new tools for analysis of hepatic fibrosis. Gut. 2005;54:142–51.
Sun S, Li H, Yuan Y, Wang L, He W, Xie H, et al. Preventive and therapeutic effects of Trichinella spiralis adult extracts on allergic inflammation in an experimental asthma mouse model. Parasit Vectors. 2019;12:326.
Wangala B, Gantin RG, Voßberg PS, Vovor A, Poutouli WP, Komlan K, et al. Inflammatory and regulatory CCL and CXCL chemokine and cytokine cellular responses in patients with patent mansonella perstans filariasis. Clin Exp Immunol. 2019;196:111–22.
McDonald EA, Kurtis JD, Acosta L, Gundogan F, Sharma S, Pond-Tor S, et al. Schistosome egg antigens elicit a proinflammatory response by trophoblast cells of the human placenta. Infect Immun. 2013;81:704–12.
Guo G, Tan D, Zhu P, Liu F. Hepatitis B virus X protein promotes proliferation and upregulates TGF-beta1 and CTGF in human hepatic stellate cell line, LX-2. Hepatobil Pancreat Dis Int. 2009;8:59–64.
Liu X, Zhu S, You H, Cong M, Liu T, Wang B, et al. Hepatitis B virus infects hepatic stellate cells and affects their proliferation and expression of collagen type I. Chinese Med J-Peking. 2009;122:1455–61.
Wang X, Hu F, Hu X, Chen W, Huang Y, Yu X. Proteomic identification of potential Clonorchis sinensis excretory/secretory products capable of binding and activating human hepatic stellate cells. Parasitol Res. 2014;113:3063–71.
Shang M, Sun H, Wu Y, Gong Y, Tang Z, Meng F, et al. In vivo and in vitro studies using Clonorchis sinensis adult-derived total protein (CsTP) on cellular function and inflammatory effect in mouse and cell model. Parasitol Res. 2020;119:1641–52.
Jiang D, Jiang Z, Han F, Zhang Y, Li Z. HGF suppresses the production of collagen type III and α-SMA induced by TGF-β1 in healing fibroblasts. Eur J Appl Physiol. 2008;103:489–93.
Pinzani M, Marra F. Cytokine receptors and signaling in hepatic stellate cells. Semin Liver Dis. 2001;21:397-416. https://doi.org/10.1055/s-2001-17554.
Chen Y, Zeng Z, Shen X, Wu Z, Dong Y, Cheng JC. MicroRNA-146a-5p negatively regulates pro-inflammatory cytokine secretion and cell activation in lipopolysaccharide stimulated human hepatic stellate cells through inhibition of toll-like receptor 4 signaling pathways. Int J Mol Sci. 2016;17:1076. https://doi.org/10.3390/ijms17071076.
Hu N, Wang C, Dai X, Zhou M, Gong L, Yu L, et al. Phillygenin inhibits LPS-induced activation and inflammation of LX2 cells by TLR4/MyD88/NF-κB signaling pathway. J Ethnopharmacol. 2020;248:112361.
Kishimoto T. IL-6: from its discovery to clinical applications. Int Immunol. 2010;22:347–52.
Nieto N. Oxidative-stress and IL-6 mediate the fibrogenic effects of rodent kupffer cells on stellate cells. Hepatology. 2006;44:1487–501.
Xiang D, Sun W, Ning B, Zhou T, Li X, Zhong W, et al. The HLF/IL-6/STAT3 feedforward circuit drives hepatic stellate cell activation to promote liver fibrosis. Gut. 2018;67:1704.
Li W, Dong H, Huang Y, Chen T, Kong X, Sun H, et al. Clonorchis sinensis co-infection could affect the disease state and treatment response of HBV patients. PLoS Negl Trop Dis. 2016;10:e4806.
Hu X, Jiang J, Ni C, Xu Q, Ye S, Wu J, et al. HBV integration-mediated cell apoptosis in HepG2 2 15. J Cancer. 2019;10:4142–50.
Chang T, Gish RG, de Man R, Gadano A, Sollano J, Chao Y, et al. A comparison of entecavir and lamivudine for HBeAg-positive chronic hepatitis B. New Engl J Med. 2006;354:1001–10.
Lapinski TW, Pazgan-Simon M, Plesniak R, Sobala-Szczygiel B. Loss of HBsAg in patients with high levels of HBV DNA during treatment with nucleoside or nucleotide analogs. Hepatitis Monthly. 2020;20(10). https://doi.org/10.5812/hepatmon.106951.
Chen P, Xie Q, Lu X, Yu C, Xu K, Ruan B, et al. Serum HBeAg and HBV DNA levels are not always proportional and only high levels of HBeAg most likely correlate with high levels of HBV DNA: a community-based study. Medicine (Baltimore). 2017;96:e7766. https://doi.org/10.1097/MD.0000000000007766.
Du D, Jia Z, Li G, Zhou Y. HBV DNA vaccine with adjuvant cytokines induced specific immune responses against HBV infection. World J Gastroenterol. 2003;9:108.
Wang A, Guan S, Yang K, Zhang H, Sun B, Pan Y, et al. Study of IFN-inducible double-stranded RNA dependent protein kinase on antiviral activity of HBV in vitro. Chinese Pharmacol Bull. 2015;12:1254–8.
Rim H, Lyu K, Lee J, Joo K. Clinical evaluation of the therapeutic efficacy of praziquantel (Embay 8440) against Clonorchis sinensis infection in man. Ann Trop Med Parasitol. 1981;75:27–33.
Veerakumari L, Munuswamy N. In vitro effect of some anthelmintics on lactate dehydrogenase activity of cotylophoron cotylophorum (Digenea: paramphistomidae). Vet Parasitol. 2000;91:129–40.
Zu-yun C, Jia-lin D, Jiang H. Effect of praziquantel, albendazole and mebendazole on recombinant lactate dehydrogenase of Taenia asiatica. Chinese J Public Health. 2010;26:553–4.
Park S, Friedrich L, Yahya NA, Rohr CM, Chulkov EG, Maillard D, et al. Mechanism of praziquantel action at a parasitic flatworm ion channel. Sci Transl Med. 2021;13:j5832.
Acknowledgements
We are thankful to all volunteers who participated in this study.
Funding
This work was supported by grants from the National Key Research and Development Program of China (No. 2021YFC2300800, 2021YFC2300802), the National Natural Science Foundation of China (81902082), the Open Foundation of Key Laboratory of Tropical Translational Medicine of Ministry of Education, Hainan Medical University (2021TTM007), and the Natural Science Foundation of Guangdong Province (2018A0303130025).
Author information
Authors and Affiliations
Contributions
HD and LZ performed the experiments and prepared the manuscript. MS collected the samples. HS and GL analysed and interpreted the results. BH, XY and YH designed the study and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Clinical Research Ethics Committee of the Third Affiliated Hospital, Sun Yat-sen University, Guangzhou, China (permission number 0204501), and informed consent forms were signed by all participants according to the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Table S1. Primer sequences for Q-PCR
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dong, H., Zhao, L., Sun, H. et al. Coinfection of Clonorchis sinensis and hepatitis B virus: clinical liver indices and interaction in hepatic cell models. Parasites Vectors 15, 460 (2022). https://doi.org/10.1186/s13071-022-05548-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13071-022-05548-5