Abstract
Background
The role of pain sensitivity in the development and maintenance of chronic pain states, impaired executive functioning, and patient recovery is being investigated. Conditioned pain modulation (CPM) is widely used to measure musculoskeletal pain associated with central sensitization (CS). Despite the recommendations of many reviews and clinical practice guidelines that exercise programs reduce pain and disability, the overall confidence in these results is considered “critically low.” The “active ingredient” of exercise programs and the dominant factor influencing CPM remain largely unknown.
The objectives of this trial are to determine:
• If different exercises cause different results on the CPM in a subgroup of people with chronic low back pain (CLBP) who are labeled as having CS pain,
• If a program of exercise interventions for 12 weeks would alter executive functioning, quality of life (QoL), disability, and pain in persons with CLBP.
• The relationship between patient characteristics, executive functions, CPM, and QoL
Methods
The trial is a randomized, controlled, multi-center study with four experimental groups and one healthy control group. Both the researchers and the people in the study will be blinded to the results. This paper describes the protocol for a trial examining the effects of 12-week individualized, twice-weekly exercise sessions lasting 30 to 60 min in persons with CLBP, who are positive for CS. Participants will be randomized to receive either patient education with motor control exercises (MCE), superficial strengthening (SS), aerobic exercises (AE), or patient education alone. Another group comprised of healthy volunteers will serve as controls. The primary outcomes are changes in CPM outcomes as measured by the cold pressor test (CPT). The secondary objectives are to evaluate executive functioning, pain, disability, quality of life, and spine muscle strength. The outcomes will be measured at 3 months and at a 6-month follow-up.
Discussion
The outcomes of the study will help in gaining more information and evidence about exercise-induced analgesia from the perspective of CPM. Measuring exercise outcomes will aid in scientifically prescribing exercise prescriptions in people with CLBP. The study outcomes will also assist in identifying the characteristics of individuals who will respond or respond indifferently to exercises. Investigating the relationship between the study’s various outcomes could provide information for future trials.
Trial registration
Clinical Trials Registry of India (CTRI) identifier: CTRI/2022/03/041143. Registered on 16 March 2022.
Similar content being viewed by others
Administrative information
Title {1} | Effectiveness of motor control exercise, aerobic walking, and muscle strengthening programs in improving outcomes in a subgroup of population with chronic low back pain positive for central sensitization: a study protocol for a randomized controlled trial |
Trial registration {2a and 2b} | Clinical Trials Registry of India (CTRI) identifier: CTRI/2022/03/041143 |
Protocol version {3} | Issue Date: October 15, 2022 Protocol Amendment Number: 03 |
Funding {4} | The Deanship of Scientific Research, Najran University, Kingdom of Saudi Arabia, funds the article processing fee |
Author details {5a} | Conceptualization: SG Methodology: SG, ARK, SD,AK Data Collection: SG, ARK, AK Formal analysis and investigation: SG, ARK, SD,AK,RSA,AA,MM, HA Writing – SG Writing—review and editing: All authors read and approved the final manuscript |
Name and contact information for the trial sponsor {5b} | Investigator initiated clinical trial; Shankar Ganesh (Principal investigator) shankarpt@rediffmail.com |
Role of sponsor {5c} | This is research initiated by the investigator. The funders played no role in the study design and in the collection, analysis, and interpretation of data and in the writing of the manuscript |
Roles of committees {5d} | The Research Committee, comprised of the Dean, Doctoral Studies, Dean, Research & Development, Dean, Physiotherapy, Head of the Department of Physiotherapy, one internal and one external expert, and one supervisor, will oversee the trial and review the progress of the study to facilitate the smooth running of the study. The medical superintendent and clinical supervisor will be responsible for overseeing participant safety, including serious unexpected suspected adverse events and database integrity, respectively |
Introduction
Background and rationale {6a}
Chronic low back pain (CLBP) refers to low back pain (LBP) that is persistent and incapacitating for more than 3 months [1] and is unrelated to underlying illnesses such as an infection, tumor, or fracture [2]. Because the causes of most CLBP conditions are unknown, they are categorized as non-specific CLBP (NSCLBP) [3]. Studies have indicated abnormal cortical function in CLBP patients including reduced left dorsolateral prefrontal cortex activity [4]; disruption of executive functions such as multitasking ability [5], sustained attention and working memory [6, 7]; longer processing time [8]; and substantial disturbances in mental flexibility, delayed memory, and psychomotor speed [9].
The role of pain sensitivity in the development and maintenance of chronic pain states and its influence on patient recovery are unclear and thus being investigated. Impaired functioning of descending anti-nociceptive mechanisms and activation of the descending and ascending pain facilitatory pathways facilitate overall pain transmission. Central sensitization (CS) is the increased responsiveness of nociceptive neurons in the central nervous system (CNS) to their normal or subthreshold afferent input [10]. Conditioned pain modulation (CPM) is extensively used to measure CS-associated musculoskeletal pain and refers to the quantitative sensory test used to assess the functionality of endogenous pain inhibition in the CNS [11]. CPM is directly related to the cognitive performance and self-reported health-related quality of life (QoL) [12].
Although persons with chronic pain are believed to have lower CPM inhibition, Sluka (2016) reported that some individuals with fibromyalgia and healthy persons exhibit normal and abnormal responses to CPM, respectively [13]. Evidence for CPM alterations in CLBP patients is mixed, with studies revealing impaired [14], normal [15], and facilitated [16] CPM compared with healthy controls. Mlekusch et al. (2016) evaluated endogenous pain modulation by using the cold pressor test (CPT) in persons with and without LBP and reported that the CPM effect declined more rapidly in the LBP group than in the normal population [17].
Exercises reduce the overall sensitivity of the CNS [18] by activating exercise-induced endogenous analgesia and spinal inhibitory mechanisms. Some studies have concluded that a bout of aerobic exercise (AE) could reduce sensitivity to painful stimuli in healthy individuals; however, other studies have reported contradictory results, with AE producing both hyper and hypoalgesic responses [19]. A study revealed an increase and a decrease in mean pain thresholds, respectively, in patients with CLBP and chronic fatigue syndrome as a response to exercise (submaximal AE program on a bicycle ergometer) [20]. Vaegter et al. (2016) examined CPM and exercise-induced hypoalgesia (EIH) in patients with chronic musculoskeletal pain under two different training conditions (bicycling and isometric contraction): one with high pain sensitivity and the other with low pain sensitivity. A partial impairment of CPM and EIH was observed in patients with high pain sensitivity compared with that in patients with low pain sensitivity [21]. Past reviews and guidelines have barely provided sufficient details about the indications of different exercise types to be used in clinical practice.
Few studies have investigated how different exercise doses affect EIH in chronic pain patients. Other studies have compared the EIH response following an AE condition with a predefined intensity (such as 75% of the maximal heart rate) to that with a self-selected intensity [22, 23]. Furthermore, numerous studies on EIH in chronic pain populations have relied on exercise doses that might not accurately reflect clinical practice, such as AE protocols lasting for < 15 min [22,23,24] and isometric exercises at low loads (10–30% of the maximum voluntary contraction) instead of dynamic resistance exercises [25, 26].
No previous study has investigated the associations between CPM outcomes, executive functions, and QoL in CLBP patients from the perspective of exercise interventions. Additional studies investigating the effects of varied exercise types and dosage on EIH in chronic pain populations that more closely resemble those observed in clinical practice are warranted. Furthermore, knowledge about the ideal frequency and types of exercise to be recommended in an exercise prescription is limited. We postulated that studying the effect of three types of exercise interventions in a subgroup of CS-positive patients and exploring the relationship between CPM responses, CLBP-related outcomes, and executive functions would increase our understanding regarding exercise prescriptions. This is crucial because pain sensitization-targeting interventions are limited and evidence for the effectiveness of exercise interventions is inconclusive.
Objectives {7}
The primary objective of the present study is to determine if different exercise types produce varied outputs on CPM in a subgroup of CLBP patients classified as having CS pain. The secondary objectives are to evaluate if a 12-week exercise intervention program would alter executive functioning, QoL, disability, and pain and to examine the relationship between patient characteristics, executive functions, CPM, and QoL in CLBP patients.
Trial design {8}
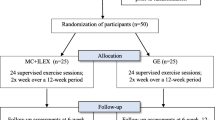
This is a randomized, controlled, double-blinded study determining how CPM changes in response to three types of active exercises in CS-positive CLBP patients. Participants will be randomized to undergo 12 weeks of the motor control exercise (MCE), superficial strengthening (SS), or AE combined with patient education or patient education alone. This active treatment concurrent control design will be used to demonstrate superiority of one exercise group over another. All patients will be allocated in a 1:1:1:1 ratio using random number tables. All participants will receive advice to stay active. Another no-pain control group will also be recruited. The intervention will be provided for 12 weeks. An independent assessor will collect data at baseline (t0), after intervention at 3 months (t1), and at the 6-month follow-up (t2). Outcome measures include CPT for measuring CPM, letter–number sequencing subtest in the Wechsler Adult Intelligence Scale-III Edition (WAIS-III), Stroop neurophysiological test, QoL assessed using the abbreviated WHOQOL-BREF questionnaire, isometric muscle strength of spine and hip muscles, the Oswestry Disability Index (ODI) questionnaire, and the Numerical Pain Rating Scale (NPRS). Table 1 and Fig. 1 present the study design and flowchart, respectively. The research ethics approval was granted by the Integral University, India (IIAHSR/DO/PT/2022/23), and Composite Regional Centre for Skill Development, Rehabilitation, and Empowerment of Persons with Disabilities, India (CRCL/Ph.D. Data Collection/2021–22/1556). The study is designed according to the Consolidated Standards of Reporting Trials (CONSORT) guidelines and reported according to the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) checklist. The study will use a 5 (between subjects − type of exercise interventions: MCE vs. AE vs. SS vs. patient education vs. no-pain control) × 3 (within subjects − time: before vs. after vs. 3 months after the intervention) mixed design.
Methods: participants, interventions, and outcomes
Study setting {9}
The study will be conducted between August 2022 and October 2023. In total, 172 participants (both male and female) aged between 18 and 59 years who have CLBP and are positive for CS-related signs and symptoms will be recruited from the Outpatient Physiotherapy Departments of the Integral University and the Composite Regional Centre for Skill Development, Rehabilitation, and Empowerment of Persons with Disabilities. Similarly, we will recruit a no-pain control population (n = 43).
Eligibility criteria {10}
The inclusion criteria for the participants are as follows: age between 18 and 59 years, male or female sex, diagnosed with NSCLBP satisfying the definition provided in the European guidelines for NSCLBP management [27], and being positive for CS-related signs and symptoms [28]. Further, using the Physical Activity Readiness Questionnaire, all participants will be screened for contraindications to exercise [29]. Table 2 presents the complete inclusion and exclusion criteria.
Who will take informed consent? {26a}
Patients will be introduced to the trial by the research team. This team will answer any questions during an in-person meeting. The primary investigator will provide information sheets about the proposed trial to all participants. The research team members will discuss the trial with the participants in light of the information provided in the information sheets. The patient will then be able to engage in an informed discussion with the primary investigator. The primary investigator will obtain the signed written consent from the patients interested in participating in the trial. The consent form will include details such as the study’s title, investigators’ names, registered information, research background, how the study will be conducted, what participants are expected to do in the study, treatment plans, and obligations. The information sheets and patient consent forms will be translated into Hindi and shared with the participants if they do not understand English.
Interventions
Explanation for the choice of comparators {6b}
The control group populations comprising the no-pain population and CS-positive patients with CLBP will help determine the effectiveness of interventions and allow us to gather valuable information for a better understanding of the impact of endogenous analgesia on pain control. The choice of a comparator is further strengthened by the results of recent recommendations that clinicians should employ standard education strategies, including exercise and physical activity, for CLBP patients [30].
Intervention description {11a}
All patients who report for CLBP management will be continuously enrolled in the study. They will undergo a standardized history taking for recording of their demographic details and will be screened for eligibility. The first author will conduct a complete physical assessment and neurological examination, and the presence of “red flags” will be closely monitored. The patients providing voluntary informed consent will be referred to the outpatient departments (OPDs) of the concerned study center where more detailed evaluations will be conducted.
In case of any doubt about a participant’s capacity to engage in the exercise program, they will be directed to a medical professional for an evaluation. The same process will continue until all participants have been recruited (n = 172). The recruited participants will then be randomized to receive one of the three exercise interventions along with patient education or patient education alone. A group comprising healthy volunteers will serve as the control group. The interventions will last for 12 weeks. Follow-up will be conducted 3 and 6 months after the intervention.
Three qualified physiotherapists (PTs) in each center will provide the interventions. All of them have a postgraduate degree in musculoskeletal physiotherapy and an average of 11 years of clinical experience. Before initiation of the study, they will attend a training session discussing the detailed treatment procedures. All PTs will be instructed to adhere to the treatment checklist provided and to complete treatment notes after each session. The participants will be instructed to avoid engaging in any other physical program during the study period and to not exercise at home during the intervention period. All the three participant groups will receive the targeted exercise interventions along with the same health education provided to group 4 participants. In order to manage time as effectively as possible, every exercise group will have 5–7 participants. The participants will be advised to continue the exercises after the treatments are over in order to support self-management.
Group 1 (AE group): This group will be subjected to a comprehensive stretching routine (lower limbs, upper limbs, and spine for 30 s in each section), 20–40 min of treadmill walking (intensity adjusted based on individual capacity and pain reports), and a 5-min local massage to relax [31]. Each walking session will start with a 5-min warm-up at a self-determined speed, followed by 20–40 min of intensive walking, and finally, a 5-min cool-down at a self-selected speed. The intensity of the walking exercise will be determined based on the heart rate and using the Borg scale. The maximum heart rate % will be calculated as 208 − (0.7 × age) [32]. The levels between 12 and 13 (moderate intensity) of the Borg scale and a range of 50–75% of maximum heart rate will be used.
Group 2 (MCE group): The first stage (1st–3rd sessions) will begin with isometric contraction of the local stability muscles (e.g., lumbar multifidus, transversus abdominis) through an abdominal drawing-in maneuver in minimally loading positions (supine lying, quadruped, sitting, and standing) [33]. The participants will be trained to activate the local stability muscles from the global muscles in an individualized manner [34]. In the second stage (4th–9th sessions), additional loads will be placed on the spine through various upper and lower extremities and trunk movement patterns to recruit various trunk [local and global] muscles. In the third stage [10th–12th sessions], functional movement patterns will be incorporated into the training program [33] (Fig. 2A–C). Exercise progression will be based on patient’s fatigue, pain thresholds, or observed movement control.
Group 3 (SS group): In this group, exercises will be focused on strengthening the rectus abdominis (RA), abdominus obliquus internus (OI), abdominus obliquus externus (OE), and erector spinae (ES) [35]. Each of the exercises will include 3 sets of 15 repetitions lasting for 45–60 min per session. Each exercise will include eight levels of steadily increasing difficulty, as outlined by Koumantakis et al. (2005) [36] (Fig. 3). Exercise progression will be based on the participant’s correct performance of the previous exercise stage and the principles of graded exposure exercise [37]. If the participants were unable to advance, they would continue exercising at the same intensity level.
Group 4 (patient education group): Health education sessions will be conducted for these participants twice a week for 12 weeks. Patient education aims to increase patients’ understanding of CLBP and alleviate myths about this condition, reassure them of the ailment’s good prognosis, and offer them useful methods for self-managing their LBP and preventing recurrence and healthcare dependency. The lecture will be followed by a 10-min discussion [38].
After the application of the study intervention, the participants will be instructed to continue the exercise interventions provided at home, twice a week, and to avoid immobility. They will be asked to report their participation using a home exercise diary.
Criteria for discontinuing or modifying allocated interventions {11b}
Any changes to the protocol that may affect the conduct of the study, or the potential benefit or safety of the patient, including changes to the study’s objectives, design, patient population, sample sizes, or significant administrative aspects, will necessitate a formal amendment to the protocol after agreement from the Institutional Review Boards of the Integral University and Composite Regional Centre for Skill Development, Rehabilitation, and Empowerment of Persons with Disabilities in accordance with local regulations.
Strategies to improve adherence to interventions {11c}
All participants will be periodically followed up over telephone. Face-to-face adherence reminder will be provided during therapy sessions or outcome measurement. The participants will be reminded about the following:
-
Importance of adhering to study guidelines.
-
Instructions about interventions, dosages, and the procedure to be followed in case of a missed session.
-
Instructions about assessment and the procedure to be followed in case of a missed session.
-
Instructions about adverse events expected, if any.
-
Instructions about management of adverse events.
-
Telephonic follow-up will be conducted on days 3 and 5 if the patient fails to show up for the scheduled assessment and intervention sessions.
-
Importance of continuing exercises after the study period and maintaining a treatment diary.
Reasons for missing the sessions will be recorded, and strategies for incorporating exercises into everyday activities will be emphasized. From the time of recruitment, the participants will be encouraged to ask any questions, and their queries will be satisfactorily answered.
Relevant concomitant care permitted or prohibited during the trial {11d}
Any type of concomitant or confounding care and interventions that may influence the study outcomes will not be permitted. However, massage will be administered to the participants who develop muscle soreness after exercises. The participants will be treated with compressive garments if they complain of perceived fatigue after exercise interventions [39]. If the participants are anticipated to need an analgesic or other physiotherapy interventions during the intervention phase, they will be considered ineligible and excluded from the study.
Provisions for post-trial care {30}
If this study demonstrates the efficacy of any one type of exercise intervention post-treatment and at follow-up with a significant effect size, all participants will be prescribed that intervention to maximize its acceptability and use.
Outcomes {12}
The primary efficacy endpoint will be a minimum difference of 10% change in PPT values in CPT and a difference of ≥ 20% from baseline to week 12 in the average daily score on an 11-point (0–10) NPRS. Secondary endpoints include change from baseline to weeks 12 and 24 in number sequencing subtest, Stroop neurophysiological test, isometric muscle strength of spine and hip muscles, and the WHOQOL-BREF and ODI questionnaires.
All outcome measures will be administered or translated into Hindi for those who have difficulties reading, comprehending, and understanding English. All translations will conform to the standard guidelines for translation of patient-reported outcome measures [40].
Primary outcome measure
CPM
The CPT will be used to measure CPM. For the conditioning stimulus, the participants’ non-dominant hand will be immersed in a bucket with temperature-controlled cold water (1 °C–4 °C), monitored by a thermometer for up to 1 min. The participant has to remain with the hand immersed in water without making muscle contractions or changes in position. Withdrawal from the water will be allowed if the patient can no longer tolerate the painful stimulus. This test will be conducted in a room with controlled room temperature, humidity, lighting, and noise.
Using a digital pressure algometer, the pressure pain threshold (PPT) will be performed in the forearm regions and tibialis anterior muscle of the dominant limbs before and after 1 min of the CPT. The tibialis anterior muscle and the distal part of the dorsal forearm, which had not been immersed in water, will be evaluated because of the lack of their relationship with the participants’ musculoskeletal complaints.
The operation of the pressure algometer and PPT measurement will be explained to the patients, and a practice test will be conducted on the patients’ dominant forearm to ensure that the test has been understood. Force will gradually be increased [1 kg-force/s] until the feeling of pressure changes to pain. The PPT will be recorded in kilograms force [Kgf]. The PPT will be repeated three times and the mean will be calculated to give the baseline PPT. The efficiency of the descending nociceptive inhibitory system will be evaluated by calculating the difference between PPT values in CPT (final cost − initial value) [41].
Secondary outcomes
Executive functions will be evaluated using the letter–number sequencing subtest and the Stroop neurophysiological test.
Letter–number sequencing subtest
The letter–number sequencing subtest in WAIS-III will be used to evaluate working memory. In this task, the participants need to listen to a series of alphanumeric characters and repeat the characters back verbally in a specific order (numbers first in the ascending order, followed by letters in the alphabetical order). The test items will be presented in the same order for all participants. The researcher will read the test items aloud, at approximately 1 s per character. The participants will be asked to record their responses by speaking aloud to the researcher, and the researcher will mark the test stimuli as completely correct or incorrect. This subtest involves 21 items. The outcome is expressed as a scaled score; each correct response shall receive 1 point, and the maximum possible score is 21 [42].
Stroop neurophysiological test
The test stimuli will be presented on a computer screen. A total of 40 items will be presented in 8 rows of 5 items each. The items and the print colors will appear in a random order. The first subtask will show color words in a random order (red, blue, yellow, and green) printed in black ink. The second subtask will display solid color patches in one of these four basic colors. In the third subtask, the color words will be printed in an incongruous ink color. For example, the word yellow will be printed in red ink. The participants will be allowed to identify the colors in English/Hindi. No time limit will be assigned to complete a subtask. The time required in seconds to complete each Stroop subtask will be recorded using a stop clock (Stroop I, Stroop II, and Stroop III) [43]. The interference score is determined by subtracting the mean score of the first and second subtest from the amount of time required to complete the third subtest.
NPRS
The NPRS is a basic instrument that may be administered even to low-literate adults through a verbal face-to-face interview or telephonic interview; the adults can also self-report their responses [44]. The amount of pain felt by a patient will be subjectively estimated by marking their pain level on an 11-point, 0-to-10 NPRS, with 0 and 10 corresponding to no pain intensity and maximum pain intensity, respectively [45].
Oswestry Disability Index
The ODI is a 10-item questionnaire used for assessing function in the activities of daily living for LBP patients. Each item in the ODI receives a score between 0 and 5. The final score will be transformed into a percentage score. We will use the modified version of the ODI where the section on employment/homemaking ability will replace the section on sex life. This modified version has a high reliability (ICC = 0.90) and responsiveness [46]. The Hindi version of the ODI is a valid and reliable instrument for measuring disability in LBP patients [47].
Quality of life
The participants’ QoL will be assessed using the abbreviated WHOQOL-BREF questionnaire. This questionnaire comprises 24 items divided across the 4 domains of physical health, psychological health, social relationships, and environmental health. Each item is rated on a 1–5 Likert scale. The mean score of items within each domain is summed up, and the scores are transformed on a scale from 0 to 100 [48]. The Hindi version of the WHOQOL questionnaire is effective for evaluating QoL in India’s healthcare settings [49].
Isometric muscle strength (spine extensors, gluteus maximus, gluteus medius, and hip lateral rotators)
Isometric muscle strength of trunk extensors, transverse abdominis, obliques, gluteus medius, gluteus maximus, and lateral hip rotators will be assessed using a pressure biofeedback unit (PBU) (Chattanooga INC). Once the PBU is inflated to 70 mm Hg, the participants will be instructed to contract the specific muscles. Readings will be taken at the completion of a 10-s contraction. Two submaximal force tests will be conducted to help the participants become familiarize with each test position, followed by two repetitions with maximum isometric contraction for each muscle group. The average of the two maximum contractions will be used for analysis [50].
-
Transversus abdominis will be tested in the prone position. The inflated cuff will be positioned beneath the abdomen at the level of the anterior superior iliac spine. The patient will be instructed to draw-in the lower abdomen without moving the upper stomach, back, or pelvis [50].
-
Abdominal obliques [bilateral OE and OI] and back extensors [ES and multifidus] will be tested in the supine lying position. The inflated cell will be placed at the level of the posterior superior iliac spine.
-
Abdominal obliques. The participants will be instructed to gently press the cell, as if to straighten the spine. For back extensors, the participants will be instructed to lift the weight off the cell [51].
-
The gluteus medius muscle will be evaluated in the side-lying position with the test leg upward. The hip will be placed in neutral adduction and extension [52], and the inflated cuff will be placed 5 cm above the lateral condyle of the femur. The participants will be asked to lift the leg against the resistance of the examiner’s hand.
-
The gluteus maximus muscle will be evaluated in the prone position with the hip in neutral and knee flexed to 90 degrees [53]. The inflated cuff will be placed 5 cm above the popliteal region and will attempt to lift the leg against the resistance of examiner’s hand.
-
The hip lateral rotator muscles will be assessed in the high sitting position [54]. The inflated cuff will be placed 5 cm above the medial malleolus. The patients will be instructed to externally rotate the hip against a resistance in an opposite direction.
Participant timeline {13}
The participant timeline is presented in Table 3.
Sample size {14}
The sample size was calculated based on the inhibitory effect of the CPT on the PPT, assuming a standard deviation of 100 kPa for the inhibitory effect across all three exercise groups. A sample size of 30 participants per group provides 87% power for an independent t-test at a 2-sided alpha of 0.05 to detect a difference in inhibition of 80 kPa [17] when assuming a minimum difference of 0.47 (equivalent to 10% change) as clinically relevant for the CPM effect [55]. Therefore, anticipating a 30% dropout rate, 43 participants will be recruited for each group.
Recruitment {15}
Various clinic- and community-based recruitment strategies will be employed to facilitate patient recruitment for the trial. Clinic-based recruitment strategies include referrals from clinicians and healthcare professionals in the study centers, as well as direct phone calls and mailings to patients from OPD records. All clinicians who agree to support the recruitment process will be provided with the detailed inclusion and exclusion criteria. The patients who agree to be contacted will be sent reminder e-mails mentioning the study requirements. Community-based recruitment strategies include web and print advertisements, flyers, and word-of-mouth referral. Advertisements will be run on Facebook and other social media platforms. Identical information regarding the inclusion criteria, estimated duration of assessment and intervention, and study contact details, including anticipated benefits, will be described in all mailings, advertisements, and flyers. All people who approach voluntarily for study participation will be inquired from where they heard about the study.
Assignment of interventions: allocation
Sequence generation {16a}
Random number tables will be used to assign treatments.
Concealment mechanism {16b}
A sequentially numbered and sealed envelope will contain details of each successive allocation to a random treatment group. An experienced neutral researcher will be provided with sealed envelopes with randomization numbers imprinted; the randomization numbers to which the intervention groups are assigned will be revealed when the envelopes are opened.
Implementation {16c}
An experienced researcher not involved in patient recruitment, providing interventions, evaluating the outcomes, or following up with any participant will perform randomization.
Assignment of interventions: blinding
Who will be blinded {17a}
The present study is designed as a randomized controlled trial. The intervention groups will be blinded from one another and outcome assessors. All outcome measures will be determined by an independent researcher blinded to treatment allocation. The assessor will attend training sessions on assessment procedures where the proposed assessment methods will be discussed in detail. The participants will be instructed to not disclose their intervention allocation to the outcome assessor. They will be informed that the effect of different active exercise programs will be evaluated so that they are unaware of any expected treatment group benefit. Another experienced researcher will feed the collected data into the computer. The researcher conducting the statistical analysis will not be present when the measurements are taken. All physiotherapists providing interventions will be blinded to the results of evaluations, measurements, and questionnaires.
Procedure for unblinding if needed {17b}
Complete blinding of investigators and participants will be attempted. The actual allocation will not be disclosed to members outside the research team. Unmasking will be permitted only under special circumstances in which knowledge of the allocated treatment is necessary for further patient care. The primary investigator will take decisions regarding unblinding in consultation with a physician.
Data collection and management
Plans for assessment and collection of outcomes {18a}
All participants will be allotted unique study identifiers independent of any external source data. Using paper forms, data will be initially collected during one-on-one sessions with the participants. All data will be collected in a face-to-face interaction and stored in a secured location. The research team will collaboratively manage the data, and a statistical analyst unaware of the grouping situation or intervention measures will analyze the data.
Plans to promote participant retention and complete follow-up {18b}
To promote retention, feedback on measured outcomes will be provided and patient education and self-management materials regarding CLBP will be distributed. In addition, all participants will be thanked for their participation and reminded of their progress in the study, upcoming data collection, and contribution to the study results. The protocol will take a flexible approach to the study schedule, and every effort will be made to resolve any conflicts that may arise. Moreover, family support will be sought, and participants will be taught to incorporate treatment into their daily life.
Data management {19, 27}
Participants’ personal information and confidentiality will be protected during all trial phases. All participant data including all reports, data collection, process, and administrative forms will be housed in lockable file cabinets in restricted-access zones and shall be identifiable solely by a coded ID [identification] number. The participant’s unique number identifier, and not their names, will be displayed in all the data. Forms, lists, logbooks, appointment books, and any other listings that link participant ID numbers to other identifying information will be kept in a closed, separate file in a restricted area. Only the primary investigator will know the name associated with the number. All data collected will be converted into the electronic format and will be stored in password-protected files in a secure place at the main study centers from where the data were collected. The data will be accessible to only the research team. All personal data will be stored separately from other data and treated as confidential, will be accessible to only selected research team members, and will not be shared. The data will be retained for 5 years after study completion. Without the participant’s explicit consent, the participant’s study information will not be disclosed outside of the study.
Statistical methods
Statistical methods for primary and secondary outcomes {20a,b}
The Shapiro–Wilk test will be used to assess the normality of the distribution of the data. A one-way analysis of variance (ANOVA) will be used to compare baseline characteristics between the groups. Descriptive statistics will be used to calculate the mean values of all outcome variables collected. A repeated measure ANOVA statistic will be used to evaluate the effect of three types of exercise interventions on CPM, neurophysiological outcomes, pain, disability, strength measures, and QoL. The study will use a 5 (between subjects – type of exercise interventions: AE vs. MCE vs. SS vs. patient education vs. no-pain control) × 3 (within subjects – time: before vs. after vs. 3 months after the intervention) mixed design. Tukey’s post hoc analysis will be conducted to establish differences between the groups. Effect size will be estimated by dividing the mean difference in outcomes between the intervention and control groups by the combined standard deviation of the two groups [56].
The primary outcome will undergo a per-protocol analysis. Pearson correlation analysis will be performed to determine the relationship between patient characteristics (Table 4), CPM, executive functioning, pain, strength measures, disability, and QoL. Multiple linear regression analysis will be used to deduce the characteristics of individuals responding positively to exercise interventions. For all measurements, p will be considered significant, if it is < 0.05. The data collected will be analyzed using SPSS (Statistical Program for the Social Sciences) 16.0 (IBM Corp., Armonk, NY).
The results will be considered clinically significant if a minimum difference of 10% change in PPT values in CPT is maintained at 6 months. Based on a previous study results [57] and a standardized mean score of 10 [58] on the letter–number sequencing subtask of WAIS-III, the mean reaction time for the Stroop interference effect will be fixed at approximately 230 s for the treatment to be considered successful. A reduction of 2 points on the NPRS [59], a cut-off value of 13, and a difference of 8 and 4 points will be considered as the minimal clinically important difference for the ODI [60], WHOQOL-BREF [61], and isometric muscle strength [62] respectively, which would indicate the success of the therapeutic intervention used.
Methods for handling protocol non-adherence and statistical methods for handling missing data {20c}
The research team will undertake all measures to minimize missing of data, and reasons for missing data, if any, will be ascertained using sensitivity analyses. Likelihood-based methods will be used if these reasons are rational. If the data are found to not miss at random, selection models and pattern-mixture models will be used. The intent-to-treat analysis will be used to evaluate our objectives based on the groups to which the participants are originally assigned after data transformation was performed.
Adverse event reporting and harms {22}
Therapeutic safety will be monitored on the basis of patient symptoms. Changes in pain, CPM, muscle soreness, and lumbar function degradation will be meticulously documented in the case report form.
Frequency and plans for auditing trial conduct {23}
We intend to conduct an audit every 6 weeks to examine all parts of research processes including participant enrolment, consent, eligibility, and allocation to study groups, as well as adherence to trial interventions, reporting of harms, accuracy, and ensuring timeliness of data collection.
Dissemination plans {31a}
The study results will be published in peer-reviewed indexed journals and distributed to the participants, healthcare professionals, the general public, and other relevant parties.
Publication {31b}
The results will be published irrespective of the outcome. Authorship shall be determined in accordance with the International Committee of Medical Journal Editors’ criteria. The authors have no limits on publication.
Discussion
Although physical exercises have been considered as the foundation of management of musculoskeletal pain conditions with proven benefits [63], the precise mechanisms underlying the effects remain unclear [64]. Traditional explanations based on biomechanics and corresponding changes in loading of the musculoskeletal system regarding why exercise improves pain and disability in chronic musculoskeletal pain fail to consider the complete biopsychosocial spectrum of factors [65]. Exercise prescription is usually based on the preferences and expertise of the individual clinician. Because exercise prescription directly impacts intervention outcomes, analyzing the exercise parameters in patients along the chronic pain spectrum is crucial.
The study will offer the following benefits. First, it will help in acquiring more information and evidence about exercise-induced analgesia from the CPM perspective. Second, investigating the relationship between executive functions, CPM, and QoL will provide further inputs for high-quality randomized controlled trials in the future. Third, measuring the outcomes of exercises will help in scientifically prescribing different exercise types. The study outcomes will also help in identifying the characteristics of individuals responding or responding indifferently to exercises; this will avoid wastage of health resources or assist in directing the non-responsive individuals to other alternative interventions.
Study strengths
The study intends to investigate only those outcome measures that have good psychometric properties, have been used extensively in research, and can be measured quickly. We will only recruit participants aged between 18 and 59 years as a previous study has hinted at a decline in endogenous pain modulatory and CPM functions with advancing age [66]. Studying the association between executive functioning, CPM, and exercises will be a major addition to the results as a previous study has indicated that this relationship is selectively sensitive and the positive effect observed on animals do not translate in humans [67]. Further, we will apply the optimal exercise dose in each group based on the methodology used in previous works.
Study limitations
Limiting the study to CS-positive participants will limit the generalization of the results. Long-term effects of exercises on CPM will not be evaluated, and the results may not be applicable to the older population. The role of confounding factors such as gender, body mass index, and level of physical activities will not be considered in this study. Future studies should evaluate the role of potential confounders associated with the CPM response.
Trial status
Protocol version number: 3 (October 15, 2022).
First day of recruitment: October 17, 2022.
Expected end of recruitment: January 17, 2023.
Availability of data and materials {29}
The datasets used and/or analyzed during the current study will be available from the corresponding author on reasonable request.
Change history
01 June 2023
A Correction to this paper has been published: https://doi.org/10.1186/s13063-023-07370-5
Abbreviations
- AE:
-
Aerobic exercise
- ANOVA:
-
Analysis of variance
- CLBP:
-
Chronic low back pain
- CNS:
-
Central nervous system
- CONSORT:
-
Consolidated Standards of Reporting Trials
- CPM:
-
Conditioned pain modulation
- CPT:
-
Cold pressor test
- CS:
-
Central sensitization
- EIH:
-
Exercise-induced hypoalgesia
- ES:
-
Erector spinae
- LBP:
-
Low back pain
- MCE:
-
Motor control exercise
- NPRS:
-
Numerical Pain Rating Scale
- NSCLBP:
-
Non-specific chronic low back pain
- ODI:
-
Oswestry Disability Index
- OE:
-
Obliquus externus
- OI:
-
Obliquus internus
- PBU :
-
Pressure biofeedback
- PPT:
-
Pressure pain threshold
- QoL:
-
Quality of life
- RA:
-
Rectus abdominis
- SD:
-
Standard deviation
- SPIRIT:
-
Standard Protocol Items: Recommendations for Interventional Trials
- SPSS:
-
Statistical Program for the Social Sciences
- SS:
-
Superficial strengthening
- TrA:
-
Transversus abdominis
References
Bogduk N. Management of chronic low back pain. MJA. 2004;180(2):79–83.
Grabois M. Management of chronic low back pain. Am J Phys Med Rehabil. 2005;84(suppl):S29–41.
Hayden JA, Wilson MN, Riley RD, Iles R, Pincus T, Ogilvie R. Individual recovery expectations and prognosis of outcomes in non-specific low back pain: prognostic factor review. Cochrane Database Syst Rev. 2019;2019(11):CD011284. https://doi.org/10.1002/14651858.CD011284.pub2. PMID: 31765487; PMCID: PMC6877336.
Seminowicz DA, Wideman TH, Naso L, et al. Effective treatment of chronic low back pain in humans reverses abnormal brain anatomy and function. J Neurosci. 2011;31(20):7540–50. https://doi.org/10.1523/JNEUROSCI.5280-10.2011.
Coté KA, Moldofsky H. Sleep, daytime symptoms, and cognitive performance in patients with fibromyalgia. J Rheumatol. 1997;24(10):2014–23.
Gimse R, Björgen IA, Tjell C, Tyssedal JS, Bø K. Reduced cognitive functions in a group of whiplash patients with demonstrated disturbances in the posture control system. J Clin Exp Neuropsychol. 1997;19(6):838–49. https://doi.org/10.1080/01688639708403764.
Grace GM, Nielson WR, Hopkins M, Berg MA. Concentration and memory deficits in patients with fibromyalgia syndrome. J Clin Exp Neuropsychol. 1999;21(4):477–87. https://doi.org/10.1076/jcen.21.4.477.876.
Schiltenwolf M, Akbar M, Hug A, et al. Evidence of specific cognitive deficits in patients with chronic low back pain under long-term substitution treatment of opioids. Pain Physician. 2014;17(1):9–20.
Melkumova KA, Podchufarova EV, Iakhno NN. [Peculiarities of cognitive functions in patients with chronic back pain] .Zh Nevrol Psikhiatr Im S S Korsakova. 2009;109(11):20-4. Russian. PMID: 20032949.
Loeser JD, Treede RD. The Kyoto protocol of IASP basic pain terminology. Pain. 2008;137(3):473–7. https://doi.org/10.1016/j.pain.2008.04.025. Epub 2008 Jun 25 PMID: 18583048.
Kennedy DL, Kemp HI, Ridout D, Yarnitsky D, Rice ASC. Reliability of conditioned pain modulation: a systematic review. Pain. 2016;157(11):2410–9. https://doi.org/10.1097/j.pain.0000000000000689.PMID:27559835;PMCID:PMC5228613.
Coppieters I, Ickmans K, Cagnie B, Nijs J, De Pauw R, Noten S, Meeus M. Cognitive performance is related to central sensitization and health-related quality of life in patients with chronic whiplash-associated disorders and fibromyalgia. Pain Physician. 2015;18(3):E389-401 . PMID: 26000686.
Sluka KA. Mechanisms and management of pain for the physical therapist. 2nd ed. Seattle, WA: IASP Press; 2016.
Correa JB, Costa LO, de Oliveira NT, Sluka KA, Liebano RE. Central sensitization and changes in conditioned pain modulation in people with chronic nonspecific low back pain: a case-control study. Exp Brain Res. 2015;233:2391–9.
Julien N, Goffaux P, Arsenault P, Marchand S. Widespread pain in fibromyalgia is related to a deficit of endogenous pain inhibition. Pain. 2005;114:295–302.
Rabey M, Poon C, Wray J, Thamajaree C, East R, Slater H. Pronociceptive and anti-nociceptive effects of a conditioned pain modulation protocol in participants with chronic low back pain and healthy control subjects. Man Ther. 2015;20:763–8.
Mlekusch S, Neziri AY, Limacher A, Jüni P, Arendt-Nielsen L, Curatolo M. Conditioned pain modulation in patients with acute and chronic low back pain. Clin J Pain. 2016;32(2):116–21. https://doi.org/10.1097/AJP.0000000000000238.
Littlewood C, Malliaras P, Bateman M, Stace R, May S, Walters S. The central nervous system–an additional consideration in “rotator cuff tendinopathy” and a potential basis for understanding response to loaded therapeutic exercise. Man Ther. 2013;18(6):468–72. https://doi.org/10.1016/j.math.2013.07.005. Epub 2013 Aug 6 PMID: 23932100.
Naugle KM, Fillingim RB, Riley JL. 3rd A meta-analytic review of the hypoalgesic effects of exercise. J Pain. 2012;13(12):1139–50.
Meeus M, Roussel NA, Truijen S, Nijs J. Reduced pressure pain thresholds in response to exercise in chronic fatigue syndrome but not in chronic low back pain: an experimental study. J Rehabil Med. 2010;42(9):884–90. https://doi.org/10.2340/16501977-0595. PMID: 20878051.
Vaegter HB, Handberg G, Graven-Nielsen T. Hypoalgesia after exercise and the cold pressor test is reduced in chronic musculoskeletal pain patients with high pain sensitivity. Clin J Pain. 2016;32:58–69.
Van Oosterwijck J, Nijs J, Meeus M, Lefever I, Huybrechts L, Lambrecht L, Paul L. Pain inhibition and postexertional malaise in myalgic encephalomyelitis/chronic fatigue syndrome: an experimental study. J Intern Med. 2010;268(3):265–78. https://doi.org/10.1111/j.1365-2796.2010.02228.x. Epub 2010 Mar 3 PMID: 20412374.
Van Oosterwijck J, Nijs J, Meeus M, Van Loo M, Paul L. Lack of endogenous pain inhibition during exercise in people with chronic whiplash associated disorders: an experimental study. J Pain. 2012;13(3):242–54. https://doi.org/10.1016/j.jpain.2011.11.006. Epub 2012 Jan 24 PMID: 22277322.
Malfliet A, Pas R, Brouns R, De Win J, Hatem SM, Meeus M, Ickmans K, van Hooff RJ, Nijs J. Cerebral blood flow and heart rate variability in chronic fatigue syndrome: a randomized cross-over study. Pain Physician. 2018;21(1):E13–24. PMID: 29357332.
Lannersten L, Kosek E. Dysfunction of endogenous pain inhibition during exercise with painful muscles in patients with shoulder myalgia and fibromyalgia. Pain. 2010;151(1):77–86. https://doi.org/10.1016/j.pain.2010.06.021. PMID: 20621420.
Tour J, Löfgren M, Mannerkorpi K, Gerdle B, Larsson A, Palstam A, Bileviciute-Ljungar I, Bjersing J, Martin I, Ernberg M, Schalling M, Kosek E. Gene-to-gene interactions regulate endogenous pain modulation in fibromyalgia patients and healthy controls-antagonistic effects between opioid and serotonin-related genes. Pain. 2017;158(7):1194–203. https://doi.org/10.1097/j.pain.0000000000000896.PMID:28282362;PMCID:PMC5472004.
Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, Mannion AF, Reis S, Staal JB, Ursin H, Zanoli G, COST B13 Working Group on Guidelines for Chronic Low Back Pain. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006;15 Suppl 2(Suppl 2):S192-300. https://doi.org/10.1007/s00586-006-1072-1. PMID: 16550448; PMCID: PMC3454542.
Smart KM, Blake C, Staines A, Doody C. The discriminative validity of “nociceptive”, “peripheral neuropathic”, and “central sensitization” as mechanisms-based classifications of musculoskeletal pain. Clin J Pain. 2011;27(8):655–63. https://doi.org/10.1097/AJP.0b013e318215f16a. PMID: 21471812.
Mahler DA. ASCM's Guidelines for Exercise Testing and Prescription. Malvern, PA, USA: Williams & Wilkins; 1995.
George SZ, Fritz JM, Silfies SP, Schneider MJ, Beneciuk JM, Lentz TA, Gilliam JR, Hendren S, Norman KS. Interventions for the management of acute and chronic low back pain: revision 2021. J Orthop Sports Phys Ther. 2021;51(11):CPG1–60. https://doi.org/10.2519/jospt.2021.0304. PMID: 34719942.
American College of Sports Medicine, Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, Minson CT, Nigg CR, Salem GJ, Skinner JS. American College of Sports Medicine position stand Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41(7):1510–30. https://doi.org/10.1249/MSS.0b013e3181a0c95c. PMID: 19516148.
Tanaka H, Monahan KD, Seals DR. Age-predicted maximal heart rate revisited. J Am Coll Cardiol. 2001;37(1):153–6. https://doi.org/10.1016/S0735-1097(00)01054-8.
Rabin A, Shashua A, Pizem K, Dickstein R, Dar G. A clinical prediction rule to identify patients with low back pain who are likely to experience short-term success following lumbar stabilization exercises: a randomized controlled validation study. J Orthop Sports Phys Ther. 2014;44(1):6-B13. https://doi.org/10.2519/jospt.2014.4888. Epub 2013 Nov 21 PMID: 24261926.
Costa LO, Maher CG, Latimer J, Hodges PW, Herbert RD, Refshauge KM, McAuley JH, Jennings MD. Motor control exercise for chronic low back pain: a randomized placebo-controlled trial. Phys Ther. 2009;89(12):1275–86. https://doi.org/10.2522/ptj.20090218. Epub 2009 Nov 5 PMID: 19892856.
Kisner C, Colby LA, Borstad J. Therapeutic Exercise: Foundations and Techniques. Philadelphia: F.A. Davis Company; 2018.
Koumantakis GA, Watson PJ, Oldham JA. Trunk muscle stabilization training plus general exercise versus general exercise only: randomized controlled trial of patients with recurrent low back pain. Phys Ther. 2005;85(3):209–25. PMID: 15733046.
Vlaeyen JW, de Jong J, Geilen M, Heuts PH, van Breukelen G. Graded exposure in vivo in the treatment of pain-related fear: a replicated single-case experimental design in four patients with chronic low back pain. Behav Res Ther. 2001;39(2):151–66. https://doi.org/10.1016/s0005-7967(99)00174-6. PMID: 11153970.
Zhang Y, Wan L, Wang X. The effect of health education in patients with chronic low back pain. J Int Med Res. 2014;42(3):815–20. https://doi.org/10.1177/0300060514527059. Epub 2014 Apr 29 PMID: 24781721.
Dupuy O, Douzi W, Theurot D, Bosquet L, Dugué B. An evidence-based approach for choosing post-exercise recovery techniques to reduce markers of muscle damage, soreness, fatigue, and inflammation: a systematic review with meta-analysis. Front Physiol. 2018;9:403. https://doi.org/10.3389/fphys.2018.00403. Published 2018 Apr 26.
Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000;25(24):3186–91.
Bittencourt JV, de Melo Magalhães Amaral AC, Rodrigues PV, Corrêa LA, Silva BM, Reis FJJ, Nogueira LAC. Diagnostic accuracy of the clinical indicators to identify central sensitization pain in patients with musculoskeletal pain. Arch Physiother. 2021;11(1):2. https://doi.org/10.1186/s40945-020-00095-7. PMID: 33431039; PMCID: PMC7798197.
Ryan JJ, Lopez SJ. Wechsler Adult Intelligence Scale-III. In: Dorfman WI, Hersen M, editors. Understanding psychological assessment. perspectives on individual differences. Boston: Springer; 2001. https://doi.org/10.1007/978-1-4615-1185-4_2.
Valentijn SA, van Boxtel MP, van Hooren SA, Bosma H, Beckers HJ, Ponds RW, Jolles J. Change in sensory functioning predicts change in cognitive functioning: results from a 6-year follow-up in the maastricht aging study. J Am Geriatr Soc. 2005;53(3):374–80. https://doi.org/10.1111/j.1532-5415.2005.53152.x. PMID: 15743277.
Sharma S, Palanchoke J, Reed D, Haxby AJ. Translation, cross-cultural adaptation and psychometric properties of the Nepali versions of numerical pain rating scale and global rating of change. Health Qual Life Outcomes. 2017;15(1):236. https://doi.org/10.1186/s12955-017-0812-8.PMID:29202878;PMCID:PMC5715544.
Roach KE, Brown MD, Dunigan KM, Kusek CL, Walas M. Test-retest reliability of patient reports of low back pain. J Orthop Sports Phys Ther. 1997;26(5):253–9. https://doi.org/10.2519/jospt.1997.26.5.253. PMID: 9353688.
Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine (Phila Pa 1976). 2000;25(24):3115–24. https://doi.org/10.1097/00007632-200012150-00006. Erratum in: Spine 2001 Apr 1;26(7):847. PMID: 11124727.
Sinha K, Nijhawan MA, Grover M. Hindi translation and Psychometric Evaluation of the Oswestry Disability Index (ODI) version 2.1a. Int J Physiother Res. 2014;2(6):743–50.
Harper A, Power M. WHOQOL User Manual. World Health Organization Edinburgh. 1999.
Saxena S, Chandiramani K, Bhargava R. WHOQOL-Hindi: a questionnaire for assessing quality of life in health care settings in India. World Health Organization Quality of Life. Natl Med J India. 1998;11:160–5.
Cairns MC, Harrison K, Wright C. Pressure biofeedback: a useful tool in the quantification of abdominal muscular dysfunction? Physiotherapy. 2000;86(3):127–38. https://doi.org/10.1016/S0031-9406(05)61155-8.
Magalhães E, Fukuda TY, Sacramento SN, Forgas A, Cohen M, Abdalla RJ. A comparison of hip strength between sedentary females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2010;40(10):641–7. https://doi.org/10.2519/jospt.2010.3120. PMID: 20508327.
Kumar S, Negi MPS, Sharma VP, Shukla R. The spinal column and abdominal pressure changes and their relationship with pain severity in patients with low back pain. Niger J Med Rehabil. 2008;13(1):1-6.
Bittencourt NF, Ocarino JM, Mendonça LD, Hewett TE, Fonseca ST. Foot and hip contributions to high frontal plane knee projection angle in athletes: a classification and regression tree approach. J Orthop Sports Phys Ther. 2012;42(12):996–1004. https://doi.org/10.2519/jospt.2012.4041. Epub 2012 Sep 18 PMID: 22990391.
Robinson RL, Nee RJ. Analysis of hip strength in females seeking physical therapy treatment for unilateral patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2007;37(5):232–8. https://doi.org/10.2519/jospt.2007.2439. PMID: 17549951.
Ng TS. Racial differences in experimental pain sensitivity and conditioned pain modulation: a study of Chinese and Indians. J Pain Res. 2019;17(12):2193–200. https://doi.org/10.2147/JPR.S197803. PMID:31410053;PMCID:PMC6643485.
Ferreira ML, Herbert RD. What does ‘clinically important’ really mean? Aust J Physiother. 2008;54(4):229–30. https://doi.org/10.1016/s0004-9514(08)70001-1. PMID: 19025502.
Pilli R, Naidu M, Pingali UR, Shobha JC, Reddy AP. A computerized Stroop test for the evaluation of psychotropic drugs in healthy participants. Indian J Psychol Med. 2013;35(2):180–9. https://doi.org/10.4103/0253-7176.116251.
Silva MA. Development of the WAIS-III: A Brief Overview, History, and Description. Grad J Couns Psychol. 2008;1(1):11 Available at: http://epublications.marquette.edu/gjcp/vol1/iss1/11.
Suzuki H, Aono S, Inoue S, Imajo Y, Nishida N, Funaba M, Harada H, Mori A, Matsumoto M, Higuchi F, Nakagawa S, Tahara S, Ikeda S, Izumi H, Taguchi T, Ushida T, Sakai T. Clinically significant changes in pain along the Pain Intensity Numerical Rating Scale in patients with chronic low back pain. PLoS One. 2020;15(3):e0229228. https://doi.org/10.1371/journal.pone.0229228 . PMID: 32126108; PMCID: PMC7053735.
Johnsen LG, Hellum C, Nygaard OP, Storheim K, Brox JI, Rossvoll I, Leivseth G, Grotle M. Comparison of the SF6D, the EQ5D, and the Oswestry Disability Index in patients with chronic low back pain and degenerative disc disease. BMC Musculoskelet Disord. 2013;26(14):148. https://doi.org/10.1186/1471-2474-14-148 . PMID:23622053;PMCID:PMC3648434.
Su CT, Ng HS, Yang AL, Lin CY. Psychometric evaluation of the Short Form 36 Health Survey (SF-36) and the World Health Organization Quality of Life Scale Brief Version (WHOQOL-BREF) for patients with schizophrenia. Psychol Assess. 2014;26(3):980–9. https://doi.org/10.1037/a0036764.
Oliveira IO, Pilz B, Santos RLG Junior, Vasconcelos RA, Mello W, Grossi DB. Reference values and reliability for lumbopelvic strength and endurance in asymptomatic subjects. Braz J Phys Ther. 2018;22(1):33–41. https://doi.org/10.1016/j.bjpt.2017.09.008.
Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;1(1):011279. https://doi.org/10.1002/14651858.CD011279.pub2. Update in: Cochrane Database Syst Rev. 2017 Apr 24;4:CD011279. PMID: 28087891; PMCID: PMC6469540.
Nijs J, Kosek E, Van Oosterwijck J, Meeus M. Dysfunctional endogenous analgesia during exercise in patients with chronic pain: to exercise or not to exercise? Pain Physician. 2012;15(3 Suppl):E205-13. PMID: 22786458.
Booth J, Moseley GL, Schiltenwolf M, Cashin A, Davies M, Hübscher M. Exercise for chronic musculoskeletal pain: a biopsychosocial approach. Musculoskeletal Care. 2017;15(4):413–21. https://doi.org/10.1002/msc.1191. Epub 2017 Mar 30 PMID: 28371175.
Hackett J, Naugle KE, Naugle KM. The decline of endogenous pain modulation with aging: a meta-analysis of temporal summation and conditioned pain modulation. J Pain. 2020;21(5–6):514–28. https://doi.org/10.1016/j.jpain.2019.09.005. Epub 2019 Sep 25 PMID: 31562994.
Black JE, Isaacs KR, Anderson BJ, Alcantara AA, Greenough WT. Learning causes synaptogenesis, whereas motor activity causes angiogenesis, in cerebellar cortex of adult rats. Proc Natl Acad Sci U S A. 1990;87(14):5568–72. https://doi.org/10.1073/pnas.87.14.5568.PMID:1695380;PMCID:PMC54366.
Acknowledgements
This work is acknowledged under Integral University manuscript number IU/R&D/2023-MCN0001807
The authors are thankful to the Deanship of Scientific Research at Najran University for funding this work under the Research Groups Funding Programme grant code (NU/RG/MRC/12/4).
Data sharing statement {31c}
No later than 3 years after the collection of the 6-month post-randomization data, we will deliver a completely deidentified data set to an appropriate data archive for sharing purposes.
Funding
The article processing charge is funded by the Deanship of Scientific Research at Najran University under the Research Groups Funding Programme grant code (NU/RG/MRC/12/4).
Author information
Authors and Affiliations
Contributions
Conceptualization: SG. Methodology: SG, ARK, SD, AK. Data Collection: SG, ARK, AK. Formal analysis and investigation: SG, ARK, SD, AK, RSA, AA, MM, HA. Writing: SG. Writing—review and editing: All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate {21a, 24, 25}
The study and protocol are developed according to the Declaration of Helsinki guidelines. The protocol has been approved by the institute ethics committee, Integral University (IIAHSR/DO/PT/2022/23) and Composite Regional Centre for Skill Development, Rehabilitation, and Empowerment of Persons with Disabilities (CRCL/Ph.D.Data Collection/2021–22/1556) and registered under access code CTRI/2022/03/041143 in the Clinical Trial Registry of India (CTRI). Date of registration: 16 March 22.
This protocol, the template informed consent forms contained in the Supplementary file (local language and English versions), participant education and recruitment materials, and other requested documents will be reviewed and approved by the institutional review boards/ethical committees of both study centers for scientific content and compliance with applicable human subjects’ regulations. The clinical trial registry and the ethics committee will be notified of any modifications to the trial protocol. No data monitoring committee has been established because there are no expected adverse outcomes other than possible brief soreness after the exercises. After initial assessment and approval, the local ethical committees will conduct a minimum annual review of the protocol. The investigator will provide safety and progress updates to the ethical committees at least once per year and within 3 months of the study’s termination or conclusion at their site.
Participation in the study is voluntary, and no incentives/rewards will be offered for participation in the study. The invitation to participate will briefly state the background and objectives of the study along with the distribution of results plan. Participants who provide their consent will be allowed to participate in the study. Those who decline to participate will be excluded from further process and will have a choice to state the reason for declining. The prospective participants will have access to the e-mail ID and phone number of the first/corresponding author should they wish to have any questions answered. Participants are free to exit the study at any point of time.
Consent for publication
All authors provided their consent for publication.
Competing interests {28}
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: the name of an author was mistakenly duplicated in the original authorship list.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ganesh, G.S., Khan, A.R., Das, S.P. et al. Effectiveness of motor control exercise, aerobic walking, and muscle strengthening programs in improving outcomes in a subgroup of population with chronic low back pain positive for central sensitization: a study protocol for a randomized controlled trial. Trials 24, 319 (2023). https://doi.org/10.1186/s13063-023-07316-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-023-07316-x