Abstract
Background
Delayed graft function, or the requirement for dialysis due to poor kidney function, is a frequent complication of deceased donor kidney transplantation that is associated with inferior outcomes. Intravenous fluids with a high chloride content, such as isotonic sodium chloride (0.9% saline), are widely used in transplantation but may increase the risk of poor kidney function. The primary objective of the BEST-Fluids trial is to compare the effect of a balanced low-chloride crystalloid, Plasma-Lyte 148 (Plasmalyte), versus 0.9% saline on the incidence of DGF in deceased donor kidney transplant recipients. This article describes the statistical analysis plan for the trial.
Methods and design
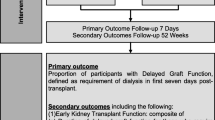
BEST-Fluids is an investigator-initiated, pragmatic, registry-based, multi-centre, double-blind, randomised controlled trial. Eight hundred patients (adults and children) in Australia and New Zealand with end-stage kidney disease admitted for a deceased donor kidney transplant were randomised to intravenous fluid therapy with Plasmalyte or 0.9% saline in a 1:1 ratio using minimization. The primary outcome is delayed graft function (dialysis within seven days post-transplant), which will be modelled using a log-binomial generalised linear mixed model with fixed effects for treatment group, minimization variables, and ischaemic time and a random intercept for study centre. Secondary outcomes including early kidney transplant function (a ranked composite of dialysis duration and the rate of graft function recovery), treatment for hyperkalaemia, and graft survival and will be analysed using a similar modelling approach appropriate for the type of outcome.
Discussion
BEST-Fluids will determine whether Plasmalyte reduces the incidence of DGF and has a beneficial effect on early kidney transplant outcomes relative to 0.9% saline and will inform clinical guidelines on intravenous fluids for deceased donor kidney transplantation. The statistical analysis plan describes the analyses to be undertaken and specified before completion of follow-up and locking the trial databases.
Trial registration
Australian New Zealand Clinical Trials Registry ACTRN12617000358347. Prospectively registered on 8 March 2017
ClinicalTrials.gov identifier NCT03829488. Registered on 4 February 2019
Similar content being viewed by others
Background
Delayed graft function (DGF) in kidney transplantation is the requirement for dialysis due to poor kidney function in the first week post-transplant [1]. It is a frequent complication of kidney transplants from deceased donors and is associated with inferior outcomes for transplant recipients and higher costs [2,3,4,5].
Intravenous (IV) fluids given during and after transplant surgery are critical for the maintenance of intravascular volume and adequate perfusion of the kidney transplant graft. The most commonly used IV fluid is isotonic sodium chloride (‘normal’ or 0.9% saline) [6], which is known to contain a high content of chloride relative to human plasma [7]. Infusion of 0.9% saline causes a predictable hyperchloremic metabolic acidosis [8, 9], especially when administered in high volumes such as those frequently used in transplant patients. Hyperchloremia may increase the risk of acute kidney injury [10,11,12] and therefore DGF, via renal vasoconstriction and kidney tissue oedema [13]. In addition, acidosis caused by 0.9% saline has been associated with a higher risk of developing hyperkalaemia [14] and therefore the potential for cardiovascular instability and arrhythmias. Whether using a low-chloride balanced crystalloid—designed to more closely reflect the electrolyte concentrations found in human plasma—can reduce the risk of DGF and improve other kidney transplant outcomes is unknown [15].
The BEST-Fluids trial is an investigator-initiated, pragmatic, registry-based, multi-centre, double-blind, randomised controlled trial comparing two approaches to intravenous fluid management in deceased donor kidney transplantation. The primary objective is to compare the effect of Plasmalyte with the effect of 0.9% saline on the incidence of DGF in deceased donor kidney transplant recipients. The secondary objectives are to determine whether perioperative IV therapy using Plasmalyte, compared with 0.9% saline, [1] improves the recovery of graft function in the first week after transplantation, [2] reduces the number of dialysis treatments required, and the duration of dialysis dependence after transplantation, [3] reduces the incidence and severity of hyperkalemia, [4] improves graft survival and death-censored graft survival at 12 months, [5] improves graft function up to 12 months post-transplant, [6] improves health-related quality of life, [7] reduces hospital length of stay and health-related costs, and [8] is cost-effective [16].
The trial was designed to recruit 800 participants (both adults and children) with end-stage kidney disease (ESKD) receiving a deceased donor kidney transplant at participating renal transplant units in Australia and New Zealand. The primary outcome is DGF, defined as requirement for dialysis within 7 days of kidney transplant. This article describes the statistical analysis plan (SAP) for the trial which was written in accordance with the guidelines for SAPs by Gamble et al. [17].
Methods and design
The full SAP, given in Additional file 1, was written and reviewed by the study statistician and clinical investigators from the BEST-Fluids Trial Steering Committee (TSC). Contributors to the SAP were blinded to treatment allocations and treatment-related study results and will remain so until the data are locked and the final data extracted for analysis. Planned analyses will be performed in accordance with the intention-to-treat principle. Minimization based on three donor characteristics (deceased donor type [donation after brain death, donation after circulatory death], machine perfusion (no, yes), and Australian Kidney Donor Risk Index [KDRI] tertile) and study centre was used to allocate treatments. The main analyses of the primary and secondary outcomes will adjust for these characteristics in addition to ischaemic time.
The primary outcome DGF will be analysed using a log-binomial generalised linear mixed model (GLMM) with fixed effects for treatment group, the three minimisation variables based on donor and transplant characteristics (deceased donor type, machine perfusion, KDRI tertile), and ischemic time, and a random intercept for study centre. The effect of treatment will be reported as a risk ratio (RR, Plasmalyte vs 0.9% saline) and 95% confidence limits from the GLMM analysis. Should the GLMM log-binomial model fail to converge, model simplifying strategies will be adopted in the first instance: adding very small centres to larger ones based on geographic location, excluding machine perfusion as a fixed effect due to the very small number of participants receiving kidneys stored by this method. In the event of intractable convergence issues, a generalised estimating equation (GEE) model (log-binomial; secondarily, Poisson) with exchangeable correlation structure and robust standard errors will be used [18]. Details of supporting and sensitivity analyses of the primary outcome can be found in Additional file 1.
A range of secondary outcomes were measured. Binary secondary outcomes will be analysed and reported using the same approach as for the primary outcome. Other secondary outcomes (continuous, time-to-event, ordinal) will be analysed using similar methods appropriate for the type of outcome.
In addition to detailed descriptions of planned analyses of primary, secondary, exploratory, and safety outcomes, the SAP details planned subgroup analyses where subgroups are formed by the minimization variables and ischaemic time, a comprehensive approach to addressing missing data on the primary and secondary outcomes, and lists changes to outcomes and analyses since publication of the final version of the trial protocol.
Conclusion
The BEST-Fluids trial will determine whether Plasmalyte has a beneficial effect on early kidney transplant outcomes relative to 0.9% saline via a reduction in the incidence of DGF and other important outcomes. These results will provide definitive data that will inform clinical practice and guidelines on the use of intravenous fluids for deceased donor kidney transplantation.
Trial status
At the time of initial submission of this article, the BEST-Fluids trial was in the final weeks of follow-up. Recruitment ceased in August 2020. Due to data entry and screening processes at the ANZDATA Registry, data lock is anticipated to be in August/September 2022.
Availability of data and materials
Not applicable since this article describes the statistical methods for the BEST-Fluids trial and does not report any results based on trial data.
Change history
07 February 2022
A Correction to this paper has been published: https://doi.org/10.1186/s13063-022-06050-0
Abbreviations
- DGF:
-
Delayed graft function
- IV:
-
Intravenous
- ESKD:
-
End-stage kidney disease
- SAP:
-
Statistical analysis plan
- TSC:
-
Trial steering committee
- KDRI:
-
Kidney donor risk index
- GLMM:
-
Generalised linear mixed model
References
Mallon DH, Summers DM, Bradley JA, Pettigrew GJ. Defining delayed graft function after renal transplantation: simplest is best. Transplantation. 2013;96(10):885–9. https://doi.org/10.1097/TP.0b013e3182a19348.
Butala NM, Reese PP, Doshi MD, Parikh CR. Is delayed graft function causally associated with long-term outcomes after kidney transplantation? Instrumental variable analysis. Transplantation. 2013;95(8):1008–14. https://doi.org/10.1097/TP.0b013e3182855544.
Hagenmeyer EG, Haussler B, Hempel E, Grannas G, Kalo Z, Kilburg A, et al. Resource use and treatment costs after kidney transplantation: impact of demographic factors, comorbidities, and complications. Transplantation. 2004;77(10):1545–50. https://doi.org/10.1097/01.TP.0000121763.44137.FA.
Wu WK, Famure O, Li Y, Kim SJ. Delayed graft function and the risk of acute rejection in the modern era of kidney transplantation. Kidney Int. 2015;88(4):851–8. https://doi.org/10.1038/ki.2015.190.
Yarlagadda SG, Coca SG, Formica RNJ, Poggio ED, Parikh CR. Association between delayed graft function and allograft and patient survival: a systematic review and meta-analysis. Nephrol Dial Transplant. 2009;24(3):1039–47. https://doi.org/10.1093/ndt/gfn667.
O'Malley CM, Frumento RJ, Bennett-Guerrero E. Intravenous fluid therapy in renal transplant recipients: results of a US survey. Transplant Proc. 2002;34(8):3142–5. https://doi.org/10.1016/S0041-1345(02)03593-5.
Weinberg L, Collins N, Van Mourik K, Tan C, Bellomo R. Plasma-Lyte 148: A clinical review. World J Crit Care Med. 2016;5(4):235–50. https://doi.org/10.5492/wjccm.v5.i4.235.
Lobo DN, Awad S. Should chloride-rich crystalloids remain the mainstay of fluid resuscitation to prevent 'pre-renal' acute kidney injury? Kidney Int. 2014;86(6):1096–105. https://doi.org/10.1038/ki.2014.105.
Wilcox CS. Regulation of renal blood flow by plasma chloride. J Clin Investig. 1983;71(3):726–35. https://doi.org/10.1172/JCI110820.
Krajewski ML, Raghunathan K, Paluszkiewicz SM, Schermer CR, Shaw AD. Meta-analysis of high- versus low-chloride content in perioperative and critical care fluid resuscitation. Br J Surg. 2015;102(1):24–36. https://doi.org/10.1002/bjs.9651.
Self WH, Semler MW, Wanderer JP, Wang L, Byrne DW, Collins SP, et al. Balanced crystalloids versus saline in noncritically ill adults. New Engl J Med. 2018;378(9):819–28. https://doi.org/10.1056/NEJMoa1711586.
Semler MW, Self WH, Wanderer JP, Ehrenfeld JM, Wang L, Byrne DW, et al. Balanced crystalloids versus saline in critically ill adults. New Engl J Med. 2018;378(9):829–39. https://doi.org/10.1056/NEJMoa1711584.
Chowdhury AH, Cox EF, Francis ST, Lobo DN. A randomized, controlled, double-blind crossover study on the effects of 2-L infusions of 0.9% saline and plasma-lyte(R) 148 on renal blood flow velocity and renal cortical tissue perfusion in healthy volunteers. Ann Surg. 2012;256(1):18–24. https://doi.org/10.1097/SLA.0b013e318256be72.
Weinberg L, Harris L, Bellomo R, Ierino F, Story D, Eastwood G, et al. Effects of intraoperative and early postoperative normal saline or Plasma-Lyte 148® on hyperkalaemia in deceased donor renal transplantation: a double-blind randomized trial. Br J Anaesth. 2017;119(4):606–15. https://doi.org/10.1093/bja/aex163.
Wan S, Roberts MA, Mount P. Normal saline versus lower-chloride solutions for kidney transplantation. Cochrane Database Syst Rev. 2016; Issue 8. Art. No.: CD010741:Art. No.: CD010741.
Collins MG, Fahim MA, Pascoe EM, Dansie KB, Hawley CM, Clayton PA, et al. Study Protocol for Better Evidence for Selecting Transplant Fluids (BEST-Fluids): a pragmatic, registry-based, multi-center, double-blind, randomized controlled trial evaluating the effect of intravenous fluid therapy with Plasma-Lyte 148 versus 0.9% saline on delayed graft function in deceased donor kidney transplantation. Trials. 2020;21(1):428.
Gamble C, Krishan A, Stocken D, Lewis S, Juszczak E, Doré C, et al. Guidelines for the content of statistical analysis plans in clinical trials. JAMA. 2017;318(23):2337–43. https://doi.org/10.1001/jama.2017.18556.
Pedroza C, Truong VTT. Estimating relative risks in multicenter studies with a small number of centers — which methods to use? A simulation study. Trials. 2017;18(1):512. https://doi.org/10.1186/s13063-017-2248-1.
Acknowledgements
Trial Steering Committee: Steven J. Chadban (Co-chair), Royal Prince Alfred Hospital & University of Sydney, Sydney, Australia; Michael Collins (Co-chair), Auckland City Hospital & University of Auckland, Auckland, New Zealand; Philip A. Clayton, ANZDATA Registry, Royal Adelaide Hospital & University of Adelaide, Adelaide, Australia; Patrick T. Coates, Royal Adelaide Hospital & University of Adelaide, Adelaide, Australia; Zoltan Endre, Prince of Wales Hospital & University of New South Wales, Sydney, Australia; Magid A. Fahim, Princess Alexandra Hospital, Metro North Hospital and Health Service & University of Queensland, Brisbane, Australia; Carmel M. Hawley, Princess Alexandra Hospital, the Translational Research Institute & University of Queensland, Brisbane, Australia; Kirsten Howard, Sydney School of Public Health, University of Sydney, Sydney, Australia; Martin Howell, Sydney School of Public Health, University of Sydney, Sydney, Australia; Kathy Kable, Westmead Hospital, Sydney, Australia; Charani Kiriwandeniya, University of Queensland, Brisbane, Australia; Jerome Laurence, Royal Prince Alfred Hospital & University of Sydney, Sydney, Australia; Wai H. Lim, Sir Charles Gairdner Hospital & University of Western Australia, Perth, Australia; Colin McArthur, Department of Critical Care Medicine, Auckland City Hospital, Auckland, New Zealand; Rachael McConnochie, Auckland City Hospital, Auckland, New Zealand; Steven McTaggart, Children’s Health Queensland Hospital and Health Service & The University of Queensland, Australia; Peter Mount, Austin Health & University of Melbourne, Melbourne, Australia; Elaine M. Pascoe, University of Queensland, Brisbane, Australia; Helen Pilmore, Auckland City Hospital & University of Auckland, Auckland, New Zealand; Donna Reidlinger, University of Queensland, Brisbane, Australia; Laura Robison, University of Queensland, Brisbane, Australia; Julie Varghese, University of Queensland, Brisbane, Australia; Liza A. Vergara, University of Queensland, Brisbane, Australia; Laurence Weinberg, Austin Health & University of Melbourne, Melbourne, Australia; and Germaine Wong, Westmead Hospital & University of Sydney, Sydney, Australia.
Funding
The BEST-Fluids trial is funded by an Australian Government Medical Research Future Fund (MRFF) Rare Cancers, Rare Diseases and Unmet Needs Grant 2018 (APPID 1152390); a Health Research Council of New Zealand Project Grant 2017 (17/414); Better Evidence And Translation in Chronic Kidney Disease (BEATCKD) grants in 2016 and 2017 (allocated from NHMRC Program Grant 2014 – CIA Craig APP ID 1092957); and Royal Australasian College of Physicians/Jacquot Research Establishment Fellowship Grants in 2017 and 2018. The trial is also supported by the manufacturer of Plasmalyte, Baxter Healthcare (Deerfield, IL, USA) who provided in kind support via a Baxter Investigator Initiated Research Grant (Medication Delivery) 2017 to provide 930 boxes of trial fluids. The funders had no role in the conception, design, or conduct of the trial, the statistical analysis plan or the preparation, approval, and decision to submit this manuscript for publication.
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed to the statistical analysis plan. EP and MC drafted the manuscript. EP is the senior statistician on the trial. MC and SC are the lead principal investigators of the trial. All authors contributed to revising the manuscript and read and approved the final version for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval for the BEST-Fluids trial was obtained from the Northern A Health and Disability Ethics Committee (approval number 17/NTA/62), for New Zealand, and from the Sydney Local Health District Human Research Ethics Committee, Royal Prince Alfred Hospital (approval numbers X17–0201 and HREC/17/RPAH/308), for Australia. The study has received local governance approvals at each of the participating sites. Protocol amendments are submitted to and approved by the ethics committees prior to implementation. Written informed consent has been obtained from all participants in the study. For children, consent has been obtained from parents or guardians, with assent sought from adolescents and children where appropriate.
Consent for publication
Consent for publication is not applicable since there are no identifying images or other personal or clinical details of participants presented.
Competing interests
MC has received research support from Baxter Healthcare Pty Ltd., the manufacturer of Plasmalyte, through a Baxter Investigator Initiated Research grant that provided fluids for this trial (commercial value of US $36,270). EP is an employee of the Sponsor, The University of Queensland. DJ has received consultancy fees, research grants, speaker’s honoraria, and travel sponsorships from Baxter Healthcare and Fresenius Medical Care, consultancy fees from Astra Zeneca and AWAK, speaker’s honoraria and travel sponsorships from ONO, and BI & Lilly, and travel sponsorships from ONO and Amgen. CH has received research grants from Baxter and NHMRC related to the current project. The other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: "Following the publication of the original article, we were notified that an incorrect additional file was published alongside the paper.
Supplementary Information
Additional file 1.
BEST-Fluids SAP v1.00_signed.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pascoe, E.M., Chadban, S.J., Fahim, M.A. et al. Statistical analysis plan for Better Evidence for Selecting Transplant Fluids (BEST-Fluids): a randomised controlled trial of the effect of intravenous fluid therapy with balanced crystalloid versus saline on the incidence of delayed graft function in deceased donor kidney transplantation. Trials 23, 52 (2022). https://doi.org/10.1186/s13063-021-05989-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-021-05989-w