Abstract
Background
While several phase III trials have investigated the role of hypofractionated radiotherapy in the definitive treatment of localized prostate cancer, prospective data reporting the outcomes of hypofractionated radiotherapy in the postoperative treatment setting are sparse. Therefore, this study is designed to assess the efficacy and treatment-related toxicity of hypofractionated salvage radiotherapy for the treatment of biochemical recurrence in men who underwent radical prostatectomy. The primary objective of this trial is to investigate whether hypofractionated radiotherapy improves biochemical control compared with conventionally fractionated radiotherapy. In addition, treatment-related toxicity, quality of life, and survival will be evaluated as secondary endpoints.
Methods
In this prospective, randomized, multi-institutional trial (the SHARE study), patients with intermediate- or high-risk prostate cancer will be randomized to receive either hypofractionated radiotherapy (65 Gy in 2.5-Gy fractions) or conventionally fractionated radiotherapy (66 Gy in 2-Gy fractions). Prostate bed irradiation or elective pelvic nodal irradiation including the prostate bed will be performed using intensity-modulated radiotherapy and daily image guidance. Treatment efficacy will be assessed using the serum tumor marker prostate-specific antigen, and toxicity will be evaluated through both physician- and patient-reported outcomes. Quality of life will also be investigated.
Discussion
This study is designed to demonstrate whether hypofractionated radiotherapy is beneficial in terms of biochemical control and toxicity compared with standard salvage radiotherapy. If hypofractionated radiotherapy is shown to be superior to conventionally fractionated radiotherapy, it will mean that improved biochemical control can be achieved, accompanied by greater patient convenience and more efficient use of medical resources.
Trial registration
ClinicalTrials.gov NCT03920033. Registered on 18 April 2019
Similar content being viewed by others
Background
After radical prostatectomy for the treatment of localized prostate cancer, approximately one-third of men will subsequently experience biochemical recurrence within a decade [1]. The risk of a rise in prostate-specific antigen (PSA) level was > 60% in patients with adverse high-risk features, such as Gleason score ≥ 8, serum PSA > 20 ng/mL, or stage of T3 or T4 [2]. Salvage radiotherapy (RT) is a potentially curative treatment option for biochemical recurrence following radical prostatectomy [3, 4].
Dose-escalated RT (76–80 Gy, 1.8–2.0 Gy per fraction) became the standard treatment for intact localized prostate cancer after several randomized trials demonstrated improved biochemical progression-free survival (bPFS) with this approach [5,6,7]. However, the potential benefit derived from dose-escalation in the postoperative setting remains to be clarified. The ASTRO/AUA guidelines recommend a minimum dose of 64–65 Gy with conventional fractionation in the postoperative setting, as the presumption is that the tumor burden is microscopic after prostatectomy, and therefore, a lower dose will be required in the postoperative setting versus the definitive setting [8]. However, several retrospective analyses have suggested that dose escalation during salvage RT may lead to improved biochemical control [9,10,11,12,13]. In a systematic review of 10,034 patients from 71 studies, the author noted that the dose response of salvage RT was similar to that of definitive RT of localized disease, and each increase of 1 Gy led to a 2% improvement in relapse-free survival [9]. Pisansky et al. evaluated 1108 patients who underwent salvage RT at 10 academic centers, demonstrating that doses > 66 Gy achieved superior biochemical control [13]. To date, the only phase III randomized clinical trial testing the dose escalation for salvage RT has been conducted by the Swiss Group for Clinical Cancer Research (SAKK). The SAKK 09/10 study compared dose-escalated RT (70 Gy in 35 fractions) versus standard-dose RT (64 Gy in 32 fractions) in the salvage setting. The initial results showed that dose escalation up to 70 Gy was associated with low rates of acute toxicity and had no impact on the recovery of early urinary continence or the prevalence of de novo incontinence [14, 15]. Freedom from biochemical failure, a primary endpoint of this trial, has not yet been reported.
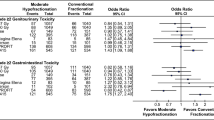
For prostate cancer, pre-clinical and clinical data have shown that an α/β ratio of a tumor is low [16,17,18]. The α/β ratio of prostate cancer is 1.4–1.9 Gy, lower than the > 3 Gy reported for the surrounding normal tissues. This suggests that RT using hypofractionation (larger fraction size and fewer fractions) would increase the probability of tumor control without increasing treatment-related toxicities. In addition, recent advances in RT techniques, such as intensity-modulated RT (IMRT) and image-guided RT, have increased the potential for normal tissue sparing and improved toxicity [19, 20]. In the definitive setting, randomized trials of patients with prostate cancer receiving hypofractionated RT (HRT) versus conventionally fractionated RT (CRT) showed non-inferior or superior cancer control with HRT [21,22,23,24,25]. However, few randomized studies have evaluated the impact of HRT in patients with biochemical recurrence after prostatectomy. Several retrospective and phase I/II studies reported that HRT was tolerable in terms of toxicity and demonstrated encouraging results for cancer control in the postoperative setting [26,27,28,29,30,31,32,33,34,35,36]. The results of HRT using modern techniques, such as IMRT, volumetric-modulated arch therapy, or helical tomotherapy, in the postoperative setting are described in Tables 1 and 2. To date, despite clinical data suggesting a dose-response relationship in the salvage RT and radiobiological aspect of a low α/β ratio of prostate cancer, no randomized controlled trials have compared HRT versus CRT in the salvage setting.
The protocol of the Salvage hypofractionated accelerated versus standard radiotherapy for biochemical recurrence after radical prostatectomy (SHARE) study is outlined here. This prospective, randomized, multi-institutional trial is designed to assess whether HRT improves biochemical control versus CRT without increasing treatment toxicity in prostate cancer patients with biochemical recurrence after radical prostatectomy. This study uses two RT dose schemes, HRT (65 Gy in 2.5-Gy fractions) versus CRT (66 Gy in 2-Gy fractions).
Methods/design
Recruitment and study design
The SHARE study is a prospective, randomized, multi-institutional trial. The protocol was approved by the institutional review boards of two participating tertiary hospitals, the Asan Medical Center and Samsung Medical Center, where it is currently ongoing. A computer-generated randomization schedule assigns the patients to either the HRT (65 Gy in 2.5-Gy fractions) or CRT (66 Gy in 2-Gy fractions) arm (Fig. 1). Random assignment is performed with a 1:1 allocation using blocked randomization, with a random block size of 4. Patients will be stratified by intermediate or high-risk according to the National Comprehensive Cancer Network (NCCN) risk classification [37] using a computer-generated random allocation sequence to ensure concealment. The clinical research nurse keeps the original random allocation sequences using the Excel file locked with a password. The process of allocation concealment from primary researchers and participants is maintained until the time of assignment. Neither the investigators nor the participants are masked to the allocated arm because blinding is not possible. For adequate participant recruitment, the investigators fully explain to potential participants the purpose, design, potential risks, and benefits of this study, as well as general ethical issues. A monthly newsletter regarding participant enrollment will be made and sent to the principal investigator and clinical research coordinators of each institution. All patients must provide written informed consent.
Flowchart of study treatments. aRisk groups defined according to the National Comprehensive Cancer Network (NCCN) guidelines. PSA, prostate-specific antigen; HRT, hypofractionated radiotherapy; CRT, conventionally fractionated radiotherapy; IMRT, intensity-modulated radiotherapy; EQD2, equivalent dose in 2-Gy fractions
As summarized in Table 3, the equivalent dose in 2-Gy fractions (EQD2) for the HRT regimen is 74.29 Gy, assuming an α/β ratio of 1.5 Gy for prostate cancer [38]. The HRT arm delivers a higher biologically effective dose (BED) than the CRT arm (173.33 Gy vs. 154 Gy). Assuming an α/β ratio of 10 Gy for acute-responding normal tissue, the BED is 81.25 Gy for the HRT arm versus 67.71 Gy for the CRT arm. Using an α/β ratio of 3 Gy for late-responding normal tissue, the HRT arm resulted in a BED of 119.17 Gy, which is slightly higher than the 110 Gy for the CRT arm.
Inclusion criteria
Eligible patients are required to have a diagnosis of histologically confirmed prostate adenocarcinoma after radical prostatectomy and must fulfill the following criteria: aged ≥ 19 years, an Eastern Cooperative Oncology Group performance status 0–1, intermediate or high risk according to the NCCN guidelines [37], and total serum PSA level after prostatectomy > 0.2 and ≤ 1.0 ng/ml. Patients should also have adequate bone marrow (absolute neutrophil count ≥ 1500 cells/mm3; hemoglobin concentration ≥ 8.0 g/dl; platelet count ≥ 50,000 cells/mm3), liver (total bilirubin < 1.5 times the maximum normal value; alanine aminotransferase or aspartate aminotransferase < 2.5 times the maximum normal value), and renal (creatinine < 2.0 ng/dl) function, as assessed by tests performed within the 6-month period prior to enrollment.
Exclusion criteria
Patients are not eligible for inclusion if they have gross nodules detected in the prostate bed; clinical, radiographic, or pathologic evidence of nodal disease; presence of distant metastasis; prior neoadjuvant chemotherapy, cryosurgery, or brachytherapy of the prostate; prior pelvic RT or chemotherapy for any other disease; and any invasive malignancy diagnosed within 5 years of entry or if they have a severe active comorbidity.
Dropout criteria
Patients shall be free to withdraw their consent once given but shall not suffer any disadvantage in terms of medical practice for the withdrawal. Any participant with medical problems or unexpected serious complications occurring during treatment or follow-up period that means the study protocol cannot be completed will be analyzed on an intention-to-treat basis.
Treatment implementation
Androgen deprivation therapy (ADT) is prescribed at the discretion of the investigator and/or physicians; administration of luteinizing hormone-releasing hormone agonists and/or anti-androgens is permitted in both treatment arms.
For RT planning, a computed tomography (CT) scan of the pelvis with a slice thickness of 2.5 mm will be obtained in all patients. Participants will be scanned in a supine position immobilized with an ankle pillow and instructed to make the bladder volume constant (empty or retain a certain amount of urine); a rectal balloon will be inserted prior to CT simulation and each treatment. There will be no routine bowel preparation. Clinical target volume (CTV) includes the prostate bed according to the Radiation Therapy Oncology Group (RTOG) contouring consensus guidelines [39]. At the discretion of the treating clinician, the pelvic lymph nodes can be included in the target volume. The planning target volume (PTV) is defined as an expansion of the CTV by 7 mm in all dimensions, other than posteriorly which will be 3–5 mm. The critical organs that are contoured include the rectum, bladder, femoral heads, penile bulb, and small bowel. The entire rectum is contoured from the anus to the rectosigmoid flexure. All patients will be treated with IMRT, and ≥ 95% of the PTV must receive the prescription dose. The use of daily image-guided techniques is strongly recommended but not mandatory.
Patients assigned to the HRT arm will receive 65 Gy of radiation in 26 fractions of 2.5 Gy (five fractions per week); for the CRT arm, 66 Gy of radiation will be administered in 33 fractions of 2 Gy (five fractions per week). The two arms differ only in the fractionation scheme. In cases of elective irradiation of the pelvic lymph nodes, 45–50 Gy will be administered using a simultaneously integrated boost technique in both arms.
Data collection and follow-up period
Patient data will be collected according to the schedule shown in Fig. 2, i.e., prior to initiating RT, weekly during RT, every 3 months for the first 2 years after RT, every 6 months for years 3–5, and then annually thereafter. The following patient data will be recorded in case report forms: urologic/gastrointestinal (GI) toxicities using the Common Toxicity Criteria for Adverse Events (CTCAE v5.0), patient-reported outcomes, QoL, and PSA levels. A pop-up sticker note will be generated automatically on the electronic medical record system to improve adherence to intervention protocols and follow-up laboratory tests. These outcome data will be aggregated as median and interquartile range. If tumor recurrence or metastases are suspected, pelvic magnetic resonance imaging, CT, and/or bone scans can be performed at the discretion of the investigator.
To ensure patient data protection, separate identification codes will be given to all patients. Data will password-protected and only accessible by investigators. All data will be deleted 3 years after the end of the study.
Assessment of primary and secondary endpoints
The primary endpoint is to investigate whether HRT improves 5-year bPFS versus CRT in patients with biochemical recurrence after radical prostatectomy. Biochemical progression-free survival is counted from the date of the salvage radiotherapy to biochemical progression, clinical progression, or death of any cause. Biochemical progression after RT is defined as detectable PSA after salvage RT. Secondary endpoints are to compare acute and late toxicities based on CTCAE v5.0 and QoL and to determine 5-year distant metastasis-free survival (DMFS) and cancer-specific survival (CSS).
Sample size considerations and statistical analysis
The trial is powered to assess the superiority of HRT when compared with CRT. Power calculations are based on an absolute increase in bPFS of 15% (from 50 to 65%) at 5 years following HRT compared with CRT according to the dose-response relationship described by King [9]. By postulating a minimum 5-year follow-up period and allowing 5% for loss, at least 144 patients per treatment arm (288 patients in total) are required, which achieves 80% power, with a two-sided α of 0.05. Subgroup analyses will be performed based on the risk group (intermediate vs. high-risk group), RT field size (prostate bed only vs. elective pelvic nodal irradiation), and use of ADT.
Statistical analysis will be conducted according to the intention-to-treat approach. Survival data, PSA value, toxicity, and QoL information will be collected even though participants discontinue the planned treatment. Multiple imputation method will be used for handling missing data. The chi-square test and Student’s t test will be used for categorical and continuous variables of patient characteristics, respectively. Time to biochemical progression will be calculated from the end of RT. The Kaplan–Meier method will be applied to estimate bPFS curves, and the log-rank test will be used to compare the curves between the two study arms. The Kaplan-Meier method and log-rank test will be used to investigate DMFS and CSS. Acute toxicity outcomes and QoL will be estimated using the chi-square test, and late toxicity outcomes will be determined using the Kaplan-Meier method.
Discussion
By increasing the radiobiological dose delivered to the prostate, HRT has the potential to shorten the duration of treatment, thereby improving patient convenience and reducing healthcare costs. In the past two decades, HRT in the intact prostate cancer setting has been evaluated in randomized controlled trials, demonstrating this approach as a safe and effective alternative to CRT. However, the efficacy and toxicity of HRT in the postoperative treatment setting remain to be validated. Several retrospective or phase I/II studies of HRT in the postoperative setting have used heterogeneous dose schemes and toxicity scoring systems, making it difficult to interpret the results. No data from randomized studies of HRT in the management of patients with biochemical recurrence after radical prostatectomy are currently available.
Biochemical control after HRT using modern RT techniques in the postoperative setting has been seen to be favorable in several studies. The studies by Tandberg et al., Kruser et al., and Lewis et al. used a HRT scheme of 65 Gy in 2.5-Gy fractions (EQD2 = 74.29 Gy; α/β ratio = 1.5 Gy), demonstrating a 4-year bPFS of 78.4, 67, and 75%, respectively [30, 31, 33]. In particular, Tandberg et al. retrospectively compared oncologic outcomes between HRT (n = 167) and CRT (n = 294) [30]. With a median follow-up of 52 months, 4-year bPFS was 78.4% after HRT and 64.8% after CRT (P = 0.0038). On multivariate analysis, there was a trend for decreased risk of biochemical progression in the HRT group compared with the CRT group (P = 0.059). Cuccia et al. reported a 3-year bPFS of 73% in 75 patients treated with salvage or adjuvant aims, but the prescribed dose (63.8 Gy in 2.2-Gy fractions; EQD2, 67.45 Gy) was relatively low compared with those used in other HRT studies [32]. The phase I/II study by Macchia et al. used RT with the 62.5 Gy in 2.5-Gy fractions scheme (EQD2 = 71.43 Gy) and reported a 5-year bPFS of 86.5% [28]. However, the study included a relatively small number of patients receiving RT with a salvage aim (18 of 124 patients). Therefore, to date, significant heterogeneity in the dose scheme and treatment aims (both salvage and adjuvant) means that it is difficult to draw conclusions regarding the oncologic treatment outcomes of salvage HRT.
Genitourinary (GU) and GI toxicities are considered to be key obstacles to the administration of HRT for prostate cancer in the postoperative setting. Although different toxicity scoring systems used in previous studies have made it difficult to assess the safety of HRT in the postoperative setting, most have demonstrated a tolerable toxicity profile [26,27,28, 30, 31, 33,34,35,36]. Kruser et al. (65 Gy in 2.5-Gy fractions) reported low rates of toxicity (one acute grade 3 GU toxicity, no acute grade 3 GI toxicities, and no late grade 3 toxicities) in 108 salvage RT patients [33]. Tandberg et al. evaluated HRT (65 Gy in 2.5-Gy fractions) in 167 patients and CRT (66 Gy in 1.8–2.0-Gy fractions) in 294 patients to determine any differences in toxicity between the two treatment groups [30]. The results showed that acute grade ≥ 2 GU toxicity was more common after HRT (22 vs. 8% in the CRT group, P = 0.0001), but HRT was not associated with late grade ≥ 2 GU toxicity on multivariate analysis. In the study by Barra et al., late grade 3 GU toxicity was recorded in 3.3% of 64 patients who received RT with a dose scheme of 62.5 Gy in 2.5-Gy fractions [34]. Alongi et al. reported no toxicities ≥ grade 3 in 39 patients who received RT with a median dose of 70 Gy in 2.5-Gy fractions [35]. A single acute grade 4 GU toxicity event was reported by Macchia et al. (62.5 Gy in 2.5-Gy fractions) [28]. In the Lewis et al. study, toxicity events > grade 3 were unusual in patients with a median dose of 65 Gy in 2.5-Gy fractions, although a relatively high rate of late GU toxicity was seen, noting a 4-year actuarial rate of late grade 3 GU toxicity of 28%, which was exclusively gross hematuria [31]. With a median follow-up of 48 months, most cases of grade 3 GU toxicity resolved, with only 7% persisting at the last follow-up visit. Analyses of bladder dose volume and PTV volume revealed no significant differences between patients with and without grade 3 GU toxicity. The authors suggested that potential explanations for the high rate of late GU toxicity could include the longer follow-up times and differences in treatment imaging and radiation delivery versus other studies, although the precise reason was not clear. Acute and late toxicities associated with HRT in the postoperative setting were relatively acceptable in most studies.
As phase III trials have demonstrated the benefits of ADT in the definitive RT setting, the addition of ADT to salvage RT may be beneficial in some patients. However, the optimal timing, duration, and type of hormone treatment remain to be determined. Two phase III trials advocated the use of ADT for patients who received salvage RT. The RTOG-9601 trial, a placebo-controlled phase III study, demonstrated that the addition of 24 months’ ADT with daily bicalutamide to salvage RT resulted in significantly higher rates of overall survival (76.3 vs. 71.3% in patients receiving placebo; P = 0.04), and a lower incidence of metastatic prostate cancer (14.5 vs. 23%, respectively; P = 0.005), and death from prostate cancer (5.8 vs. 13.4%, respectively; P < 0.001) at 12 years [40]. Another randomized trial, GETUG-AFU 16, has also shown the superiority of adding 6 months of goserelin to salvage RT [41, 42]. After a median follow-up of 112 months, the 10-year progression-free survival was significantly better in the ADT arm versus RT alone (64 vs. 49%, respectively; P < 0.0001). The RADICALS trial randomly assigned patients to adjuvant RT or salvage RT, with or without ADT, and the NRG Oncology/RTOG 0534 SPPORT trial randomly assigned patients to salvage RT to the prostate bed, salvage RT to the prostate bed with ADT, or salvage RT to the prostate bed and the pelvic lymph nodes with ADT. The results of these trials could provide further evidences concerning the administration of postoperative ADT. To date, it is uncertain whether ADT in combination with salvage HRT improves biochemical control. In the trial outlined here, the authors will conduct subgroup analyses according to the use of ADT and examine the benefit derived from combined therapy. We anticipate that HRT will demonstrate favorable biochemical control and acceptable toxicity in prostate cancer patients with biochemical recurrence after radical prostatectomy. If HRT is seen to be superior to CRT, it will indicate the benefit of escalating dose delivery to the prostate bed, which will also improve patients’ convenience and reduce healthcare costs.
Trial status
The current protocol is version 1.6 as of 4 February 2021. Patient recruitment began in August 2019 and is expected to be completed by March 2022.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PSA:
-
Prostate-specific antigen
- RT:
-
Radiotherapy
- bPFS:
-
Biochemical progression-free survival
- SAKK:
-
Swiss Group for Clinical Cancer Research
- IMRT:
-
Intensity-modulated radiotherapy
- HRT:
-
Hypofractionated radiotherapy
- CRT:
-
Conventionally fractionated radiotherapy
- QoL:
-
Quality of life
- NCCN:
-
National Comprehensive Cancer Network
- EQ D2:
-
Equivalent dose in 2-Gy fractions
- BED:
-
Biologically effective dose
- ADT:
-
Androgen deprivation therapy
- CT:
-
Computed tomography
- CTV:
-
Clinical target volume
- PTV:
-
Planning target volume
- GI:
-
Gastrointestinal
- CTCAE:
-
Common Toxicity Criteria for Adverse Events
- DMFS:
-
Distant metastasis-free survival
- CSS:
-
Cancer-specific survival
- GU:
-
Genitourinary
References
Roehl KA, Han M, Ramos CG, Antenor JA, Catalona WJ. Cancer progression and survival rates following anatomical radical retropubic prostatectomy in 3,478 consecutive patients: long-term results. J Urol. 2004;172(3):910–4. https://doi.org/10.1097/01.ju.0000134888.22332.bb.
Sundi D, Tosoian JJ, Nyame YA, Alam R, Achim M, Reichard CA, et al. Outcomes of very high-risk prostate cancer after radical prostatectomy: validation study from 3 centers. Cancer. 2019;125(3):391–7. https://doi.org/10.1002/cncr.31833.
Trock BJ, Han M, Freedland SJ, Humphreys EB, DeWeese TL, Partin AW, et al. Prostate cancer-specific survival following salvage radiotherapy vs observation in men with biochemical recurrence after radical prostatectomy. JAMA. 2008;299(23):2760–9. https://doi.org/10.1001/jama.299.23.2760.
Freedland SJ, Rumble RB, Finelli A, Chen RC, Slovin S, Stein MN, et al. Adjuvant and salvage radiotherapy after prostatectomy: American Society of Clinical Oncology clinical practice guideline endorsement. J Clin Oncol. 2014;32(34):3892–8. https://doi.org/10.1200/JCO.2014.58.8525.
Zietman AL, DeSilvio ML, Slater JD, Rossi CJ Jr, Miller DW, Adams JA, et al. Comparison of conventional-dose vs high-dose conformal radiation therapy in clinically localized adenocarcinoma of the prostate: a randomized controlled trial. JAMA. 2005;294(10):1233–9. https://doi.org/10.1001/jama.294.10.1233.
Dearnaley DP, Jovic G, Syndikus I, Khoo V, Cowan RA, Graham JD, et al. Escalated-dose versus control-dose conformal radiotherapy for prostate cancer: long-term results from the MRC RT01 randomised controlled trial. Lancet Oncol. 2014;15(4):464–73. https://doi.org/10.1016/S1470-2045(14)70040-3.
Heemsbergen WD, Al-Mamgani A, Slot A, Dielwart MF, Lebesque JV. Long-term results of the Dutch randomized prostate cancer trial: impact of dose-escalation on local, biochemical, clinical failure, and survival. Radiother Oncol. 2014;110(1):104–9. https://doi.org/10.1016/j.radonc.2013.09.026.
Pisansky TM, Thompson IM, Valicenti RK, D’Amico AV, Selvarajah S. Adjuvant and salvage radiotherapy after prostatectomy: ASTRO/AUA Guideline Amendment 2018-2019. J Urol. 2019;202(3):533–8. https://doi.org/10.1097/JU.0000000000000295.
King CR. The dose-response of salvage radiotherapy following radical prostatectomy: a systematic review and meta-analysis. Radiother Oncol. 2016;121(2):199–203. https://doi.org/10.1016/j.radonc.2016.10.026.
Ohri N, Dicker AP, Trabulsi EJ, Showalter TN. Can early implementation of salvage radiotherapy for prostate cancer improve the therapeutic ratio? A systematic review and regression meta-analysis with radiobiological modelling. Eur J Cancer. 2012;48(6):837–44. https://doi.org/10.1016/j.ejca.2011.08.013.
Bernard JR Jr, Buskirk SJ, Heckman MG, Diehl NN, Ko SJ, Macdonald OK, et al. Salvage radiotherapy for rising prostate-specific antigen levels after radical prostatectomy for prostate cancer: dose-response analysis. Int J Radiat Oncol Biol Phys. 2010;76(3):735–40. https://doi.org/10.1016/j.ijrobp.2009.02.049.
King CR, Spiotto MT. Improved outcomes with higher doses for salvage radiotherapy after prostatectomy. Int J Radiat Oncol Biol Phys. 2008;71(1):23–7. https://doi.org/10.1016/j.ijrobp.2007.09.047.
Pisansky TM, Agrawal S, Hamstra DA, Koontz BF, Liauw SL, Efstathiou JA, et al. Salvage radiation therapy dose response for biochemical failure of prostate cancer after prostatectomy-a multi-institutional observational study. Int J Radiat Oncol Biol Phys. 2016;96(5):1046–53. https://doi.org/10.1016/j.ijrobp.2016.08.043.
Ghadjar P, Hayoz S, Bernhard J, Zwahlen DR, Holscher T, Gut P, et al. Acute toxicity and quality of life after dose-intensified salvage radiation therapy for biochemically recurrent prostate cancer after prostatectomy: first results of the randomized trial SAKK 09/10. J Clin Oncol. 2015;33(35):4158–66. https://doi.org/10.1200/JCO.2015.63.3529.
Ghadjar P, Hayoz S, Bernhard J, Zwahlen DR, Stein J, Holscher T, et al. Impact of dose intensified salvage radiation therapy on urinary continence recovery after radical prostatectomy: results of the randomized trial SAKK 09/10. Radiother Oncol. 2018;126(2):257–62. https://doi.org/10.1016/j.radonc.2017.10.025.
Brenner DJ, Hall EJ. Fractionation and protraction for radiotherapy of prostate carcinoma. Int J Radiat Oncol Biol Phys. 1999;43(5):1095–101. https://doi.org/10.1016/S0360-3016(98)00438-6.
Brenner DJ, Martinez AA, Edmundson GK, Mitchell C, Thames HD, Armour EP. Direct evidence that prostate tumors show high sensitivity to fractionation (low alpha/beta ratio), similar to late-responding normal tissue. Int J Radiat Oncol Biol Phys. 2002;52(1):6–13. https://doi.org/10.1016/S0360-3016(01)02664-5.
Miralbell R, Roberts SA, Zubizarreta E, Hendry JH. Dose-fractionation sensitivity of prostate cancer deduced from radiotherapy outcomes of 5,969 patients in seven international institutional datasets: alpha/beta = 1.4 (0.9-2.2) Gy. Int J Radiat Oncol Biol Phys. 2012;82(1):e17–24. https://doi.org/10.1016/j.ijrobp.2010.10.075.
Wortel RC, Incrocci L, Pos FJ, van der Heide UA, Lebesque JV, Aluwini S, et al. Late side effects after image guided intensity modulated radiation therapy compared to 3D-conformal radiation therapy for prostate cancer: results from 2 prospective cohorts. Int J Radiat Oncol Biol Phys. 2016;95(2):680–9. https://doi.org/10.1016/j.ijrobp.2016.01.031.
Goenka A, Magsanoc JM, Pei X, Schechter M, Kollmeier M, Cox B, et al. Improved toxicity profile following high-dose postprostatectomy salvage radiation therapy with intensity-modulated radiation therapy. Eur Urol. 2011;60(6):1142–8. https://doi.org/10.1016/j.eururo.2011.08.006.
Hoffman KE, Voong KR, Levy LB, Allen PK, Choi S, Schlembach PJ, et al. Randomized trial of hypofractionated, dose-escalated, intensity-modulated radiation therapy (IMRT) versus conventionally fractionated IMRT for localized prostate cancer. J Clin Oncol. 2018;36(29):2943–9. https://doi.org/10.1200/JCO.2018.77.9868.
Catton CN, Lukka H, Gu CS, Martin JM, Supiot S, Chung PWM, et al. Randomized trial of a hypofractionated radiation regimen for the treatment of localized prostate cancer. J Clin Oncol. 2017;35(17):1884–90. https://doi.org/10.1200/JCO.2016.71.7397.
Arcangeli G, Saracino B, Arcangeli S, Gomellini S, Petrongari MG, Sanguineti G, et al. Moderate hypofractionation in high-risk, organ-confined prostate cancer: final results of a phase III randomized trial. J Clin Oncol. 2017;35(17):1891–7. https://doi.org/10.1200/JCO.2016.70.4189.
Incrocci L, Wortel RC, Alemayehu WG, Aluwini S, Schimmel E, Krol S, et al. Hypofractionated versus conventionally fractionated radiotherapy for patients with localised prostate cancer (HYPRO): final efficacy results from a randomised, multicentre, open-label, phase 3 trial. Lancet Oncol. 2016;17(8):1061–9. https://doi.org/10.1016/S1470-2045(16)30070-5.
Dearnaley D, Syndikus I, Mossop H, Khoo V, Birtle A, Bloomfield D, et al. Conventional versus hypofractionated high-dose intensity-modulated radiotherapy for prostate cancer: 5-year outcomes of the randomised, non-inferiority, phase 3 CHHiP trial. Lancet Oncol. 2016;17(8):1047–60. https://doi.org/10.1016/S1470-2045(16)30102-4.
Katayama S, Striecker T, Kessel K, Sterzing F, Habl G, Edler L, et al. Hypofractionated IMRT of the prostate bed after radical prostatectomy: acute toxicity in the PRIAMOS-1 trial. Int J Radiat Oncol Biol Phys. 2014;90(4):926–33. https://doi.org/10.1016/j.ijrobp.2014.07.015.
Saldi S, Bellavita R, Lancellotta V, Palumbo I, Lupattelli M, Chierchini S, et al. Acute toxicity profiles of hypofractionated adjuvant and salvage radiation therapy after radical prostatectomy: results of a prospective study. Int J Radiat Oncol Biol Phys. 2019;103(1):105–11. https://doi.org/10.1016/j.ijrobp.2018.08.016.
Macchia G, Siepe G, Capocaccia I, Nguyen NP, Schiavina R, Cammelli S, et al. Hypofractionated postoperative IMRT in prostate carcinoma: a phase I/II study. Anticancer Res. 2017;37(10):5821–8. https://doi.org/10.21873/anticanres.12025.
Gladwish A, Loblaw A, Cheung P, Morton G, Chung H, Deabreu A, et al. Accelerated hypofractioned postoperative radiotherapy for prostate cancer: a prospective phase I/II study. Clin Oncol (R Coll Radiol). 2015;27(3):145–52. https://doi.org/10.1016/j.clon.2014.12.003.
Tandberg DJ, Oyekunle T, Lee WR, Wu Y, Salama JK, Koontz BF. Postoperative radiation therapy for prostate cancer: comparison of conventional versus hypofractionated radiation regimens. Int J Radiat Oncol Biol Phys. 2018;101(2):396–405. https://doi.org/10.1016/j.ijrobp.2018.02.002.
Lewis SL, Patel P, Song H, Freedland SJ, Bynum S, Oh D, et al. Image guided hypofractionated postprostatectomy intensity modulated radiation therapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2016;94(3):605–11. https://doi.org/10.1016/j.ijrobp.2015.11.025.
Cuccia F, Mortellaro G, Serretta V, Valenti V, Tripoli A, Gueci M, et al. Hypofractionated postoperative helical tomotherapy in prostate cancer: a mono-institutional report of toxicity and clinical outcomes. Cancer Manag Res. 2018;10:5053–60. https://doi.org/10.2147/CMAR.S182016.
Kruser TJ, Jarrard DF, Graf AK, Hedican SP, Paolone DR, Wegenke JD, et al. Early hypofractionated salvage radiotherapy for postprostatectomy biochemical recurrence. Cancer. 2011;117(12):2629–36. https://doi.org/10.1002/cncr.25824.
Barra S, Belgioia L, Marcenaro M, Callegari S, Pastorino A, Trapani L, et al. Moderate hypofractionated radiotherapy after prostatectomy for cancer patients: toxicity and clinical outcome. Cancer Manag Res. 2018;10:473–80. https://doi.org/10.2147/CMAR.S146131.
Alongi F, Cozzi L, Fogliata A, Iftode C, Comito T, Clivio A, et al. Hypofractionation with VMAT versus 3DCRT in post-operative patients with prostate cancer. Anticancer Res. 2013;33(10):4537–43.
Cozzarini C, Fiorino C, Di Muzio N, Valdagni R, Salonia A, Alongi F, et al. Hypofractionated adjuvant radiotherapy with helical tomotherapy after radical prostatectomy: planning data and toxicity results of a Phase I-II study. Radiother Oncol. 2008;88(1):26–33. https://doi.org/10.1016/j.radonc.2008.03.021.
NCCN Clinical Practice Guidelines in Oncology: Prostate cancer. Version 4. 2019. http://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf. Accessed Jan 2021.
Fowler JF. 21 years of biologically effective dose. Br J Radiol. 2010;83(991):554–68. https://doi.org/10.1259/bjr/31372149.
Michalski JM, Lawton C, El Naqa I, Ritter M, O’Meara E, Seider MJ, et al. Development of RTOG consensus guidelines for the definition of the clinical target volume for postoperative conformal radiation therapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2010;76(2):361–8. https://doi.org/10.1016/j.ijrobp.2009.02.006.
Shipley WU, Seiferheld W, Lukka HR, Major PP, Heney NM, Grignon DJ, et al. Radiation with or without antiandrogen therapy in recurrent prostate cancer. N Engl J Med. 2017;376(5):417–28. https://doi.org/10.1056/NEJMoa1607529.
Carrie C, Hasbini A, de Laroche G, Richaud P, Guerif S, Latorzeff I, et al. Salvage radiotherapy with or without short-term hormone therapy for rising prostate-specific antigen concentration after radical prostatectomy (GETUG-AFU 16): a randomised, multicentre, open-label phase 3 trial. Lancet Oncol. 2016;17(6):747–56. https://doi.org/10.1016/S1470-2045(16)00111-X.
Carrie C, Magne N, Burban-Provost P, Sargos P, Latorzeff I, Lagrange JL, et al. Short-term androgen deprivation therapy combined with radiotherapy as salvage treatment after radical prostatectomy for prostate cancer (GETUG-AFU 16): a 112-month follow-up of a phase 3, randomised trial. Lancet Oncol. 2019;20(12):1740–9. https://doi.org/10.1016/S1470-2045(19)30486-3.
Acknowledgements
Not applicable
Funding
This study was supported by a grant (No. 2019-0154) from the Asan Institute for Life Sciences, Asan Medical Center, Seoul, Republic of Korea.
The funder had no role in the study design, data collection, management, analysis and their interpretation, decision to publish, or preparation of the manuscript.
Due to a shortage of budget, the coordinating center, steering committee, endpoint adjudication committee, and data management team could not be made for this trial. After discussion with the local institutional review board regarding this issue, an annual audit will be done by each institutional review board instead.
Author information
Authors and Affiliations
Contributions
YSK developed the trial and revised the trial protocol. GP drafted the manuscript. GP and JSL are responsible for the statistical analysis. YJK, HA, and WP reviewed the trial protocol. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval to conduct this study (version 1.6 on 4 February 2021) was granted by the Institutional Review Board of the Seoul Asan Medical Center (S2019-0333). It is mandatory to obtain informed consent from patients only by the principal investigator in each hospital prior to recruitment.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Park, G., Kim, Y.J., Ahn, H. et al. Salvage hypofractionated accelerated versus standard radiotherapy for the treatment of biochemical recurrence after radical prostatectomy (SHARE): the protocol of a prospective, randomized, open-label, superiority, multi-institutional trial. Trials 22, 728 (2021). https://doi.org/10.1186/s13063-021-05708-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-021-05708-5