Abstract
Background
Knee osteoarthritis (OA) is a common painful and disabling condition that affects older individuals. Proprioceptive training programs in the form of kinesthesia, balance and agility (KBA) exercises have been reported to be beneficial for individuals with knee OA. However, the most optimal training dosage of KBA exercises is still unclear. The aim of this study is to determine the effects of different frequencies of KBA training (i.e., twice-weekly or thrice-weekly) in adults with knee OA.
Methods
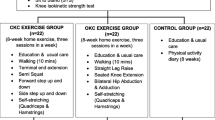
A single (assessor) blind, three-arm parallel, multi-center randomized controlled trial will be conducted. One hundred twenty adults with knee OA will be recruited from four tertiary hospitals in Northwestern Nigeria and randomly assigned into one of three intervention groups; twice-weekly KBA (n = 40), thrice-weekly KBA (n = 40), and conventional physiotherapy (n = 40) in the ratio of 1:1:1. Participants in the conventional physiotherapy group will receive two sessions of brief patient education, and sixteen sessions of ultrasound therapy, and stretching and strengthening exercises for 8 weeks. Participants in the two different KBA groups will receive KBA training according to the designed sessions for 8 weeks in addition to the conventional physiotherapy program. All groups will be assessed pre-intervention, immediately post-intervention and at 3 months, 4 months, and 6 months post-randomization. The primary outcome will be physical function (Ibadan Knee and Hip Osteoarthritis Outcome Measure) whereas the secondary outcomes will be pain intensity (Visual Analogue Scale for pain), knee stability (Knee Outcome Survey-Activities of Daily Living Scale), proprioception (electronic goniometer), and quality of life (Osteoarthritis Knee and Hip Quality of Life Questionnaire).
Discussion
The findings of this study may provide evidence on the effectiveness of KBA exercise training and the ideal number of sessions needed to achieve the highest effectiveness in adults with knee OA.
Trial registration
Pan African Clinical Trials Registry (PACTR201810713260138). Registered on 28 November 2017.
Similar content being viewed by others
Background
Osteoarthritis (OA) is a common chronic degenerative joint disorder that affects people particularly the older population [1]. It is considered to be a disorder of dynamic pathology typified by progressive loss of articular cartilage, subchondral bone sclerosis, cyst, and osteophyte formation [2]. The impact of OA is multifactorial including pain, reduced physical function and quality of life, as well as increased healthcare and socioeconomic cost [3,4,5]. OA is the leading cause of disability worldwide [6]. About 250 million people are currently affected by OA, and the burden of this disorder is expected to rise globally over the coming decades perhaps due to the combined effects of the aging and obesity epidemic, along with increasing numbers of joint injuries [3].
The knee is one of the most commonly affected joints and accounts for the majority of disability from OA particularly in the elderly [7]. Epidemiological data suggest that about 14 million US populations have symptomatic knee OA, and more than half of these individuals are less than 65 years old [8]. Although data on the prevalence of knee OA in Africa is somewhat sparse [9], numerous hospital-based studies in Nigeria have indicated that knee OA is common [10,11,12,13,14], with prevalence rates of 19.6–20.6% in people ≥ 40 years old [10, 11] and 16.3% in people ≤ 30 years old [11]. Moreover, female gender, advanced age, obesity, knee malalignment, previous knee injury, and decreased quadriceps strength were reported to be the common risk factors associated with knee OA in Nigeria [11, 13,14,15] as found in the western nations [5, 16, 17].
Knee OA poses a major health problem to the society as it accounts for more walking disability than any other condition [18]. Though to date, no specific cure for OA exists, current treatment methods including pharmacological, non-pharmacologic and surgical modalities are targeted at reducing symptoms, minimizing functional disability, and limiting disease progression [19]. Non-pharmacological methods such as education/self-management, exercise, weight loss if overweight or obese, walking aids as indicated, and thermal modalities are recommended as first-line treatment [20]. These modalities are commonly prescribed for individuals with mild to moderate knee OA.
Exercise therapy is probably the most widely prescribed intervention for knee OA. Evidence suggests that exercise therapy, even though its effects are modest, is beneficial for individuals with knee OA [21, 22], hence universally endorsed by many treatment guidelines [23,24,25,26,27]. The most recent systematic review and meta-analysis found high-quality evidence that land-based exercise programs provide positive benefits for pain and quality of life and moderate-quality evidence of improved functional disability in individuals with knee OA [21]. While several forms of exercise interventions for this disabling condition exist, most conventionally fall into strengthening, aerobic, flexibility and skills/balance or proprioceptive exercises [28].
Proprioceptive exercises are commonly prescribed for individuals with knee OA, with the goals of improving joint proprioceptive acuity (position sense and motion sense [kinesthesia]) and dynamic stability [29] as these components are commonly altered in these individuals [30,31,32,33]. Moreover, there is evidence to suggest that proprioceptive training performed in both weight-bearing and non-weight-bearing positions can enhance proprioceptive acuity, and reduce pain as well as functional disability in individuals with knee OA [29, 34, 35].
Kinesthesia, balance and agility (KBA) is a form of proprioceptive training that has been gaining interest among researchers in the management of knee OA and knee-related injuries. This exercise training is typically designed to improve dynamic joint stability and neuromuscular control using a series of physical activities that challenge the individual’s neuromuscular system to maintain balance and coordination [36]. KBA techniques are commonly used in the rehabilitation and prevention of knee ligamentous injury [37,38,39,40] and ankle instability [41, 42]. However, in recent years, KBA has been also applied in the management of individuals with knee OA. The benefits of this intervention in knee osteoarthritic condition were first reported in a case study of a physically active, elderly woman with bilateral knee OA [43]. After receiving a 6-week, twice-weekly KBA plus therapeutic exercise program, the patient’s symptoms resolved rapidly and was able to return to recreational sports.
So far, to our knowledge, only six randomized controlled trials (RCTs) [36, 44,45,46,47,48] investigated the effects of KBA exercises among individuals with knee OA. Two trials [36, 44] applied 8 weeks, three times per week of KBA plus resistance training, and found no superior benefits of this combination on Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain and physical function compared to resistance training alone. A similar result was also reported in another trial [45] that applied 6–8 weeks, two times per week of KBA plus resistance training. On the contrary, superiority results were reported with 8 weeks, three times per week of KBA plus resistance training compared to resistance training alone in one [46] of the earlier trials. This is also in line with another earlier trial [47] that found higher positive effects of KBA training alone on perceived pain and functional capacity when compared to non-treatment. However, when the treatment sessions of KBA training were increased to five times per week for 4 weeks [48], no superiority effects were observed over strength training on perceived pain and most symptoms. While the results of these studies are promising, the question of what is the ideal number of sessions (dosage) of structured KBA exercises that can be expected to produce the desired therapeutic outcomes however remains to be addressed. Moreover, no study has combined or compared KBA training with a conventional physiotherapy consisting of education/self-management, thermotherapy, and stretching and strengthening exercises among individuals with knee OA despite these methods are endorsed as the first-line management [20].
It is conceivable that the small to moderate effect sizes detected in exercise-based RCTs on knee OA may be due to insufficient dose used [20]. It has recently been suggested that evidence-based proprioceptive training should consider training frequency of at least three times per week, for 30 to 40 min per session to achieve the highest effectiveness [34]. The frequency and number of sets to be performed therefore should be taken into consideration when designing proprioceptive-based training programs for knee OA individuals as these exercise programs may appear challenging especially among older individuals. Thus, this study will be conducted to determine which frequency of structured KBA exercise training (i.e., twice-weekly or thrice-weekly) will produce superior therapeutic outcomes in adults with knee OA. The primary outcome will be physical function whereas secondary outcomes will be pain intensity, knee stability, proprioception, and quality of life.
Methods
Study design
This study will be a single (assessor) blind, three-arm parallel, multi-center RCT. The outline of the study protocol is shown in Fig. 1. The protocol for this study is reported in accordance with the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) 2013 Checklist (Additional file 1).
Study setting
The study will be conducted at four tertiary hospitals in Kano city, Kano State, Northwestern Nigeria; Muhammad Abdullahi Wase Teaching Hospital (MAWTH), Murtala Muhammad Specialist Hospital (MMSH), Aminu Kano Teaching Hospital (AKTH), and National Orthopedic Hospital Dala (NOHD). These centers were chosen to have the required number of participants.
Training of physiotherapists/research assistants
Prior to the commencement of the study, two licensed physiotherapists with at least 2 years of clinical experience will be recruited as research assistants in each of the four hospitals. One physiotherapist will be responsible for eligibility and outcome (baseline and follow-up) assessments. This physiotherapist will be blinded to group allocation. The other physiotherapist will be responsible for treatment. All the physiotherapists will receive a 2-day training on the study procedures by the lead investigator (AIA).
Participants’ recruitment and eligibility
Participants for this study will be consecutive patients with knee OA referred to the physiotherapy department by the general practitioners in the four tertiary hospitals. Also, recruitment adverts using local posters with the contact of the primary investigator will be pasted at various notice boards in the selected hospitals. To be eligible for the study, participants must meet the clinical criteria for the diagnosis of knee OA according to the American College of Rheumatology (ACR) criteria for unilateral or bilateral symptomatic knee OA [48] in addition to being male or female of 30 to 65 years old. They will be excluded if they have any history of knee, hip, or ankle surgery prior to the study, peripheral vascular disease, local or systemic infection, deformity in lower limbs, rheumatic disease other than OA, high-risk health status for exercise, unresolved balance or neurological disorder, and history of a lower extremity exercise program for a minimum of six weeks prior to enrollment.
Baseline assessment
Patients will be assesed for eligibility by the physiotherapists at the four recruiting hospitals through history taking physical examination, and evaluation of self-report questionnaires. After ensuring eligibility, participants will be given oral and written information regarding the procedures and potential risks of the study. Written informed consent will be then sought and obtained. Baseline socio-demographic and clinical variables such as age, gender, marital status, education level, occupational status, height, weight, body mass index, duration of knee pain, and side affected will be collected using a prepared proforma. Baseline self-report outcome assessments will include physical function, pain intensity, knee stability, and quality of life. Baseline objective outcome assessment will be proprioception measurement. The flow of participants is depicted in Fig. 2.
Randomization and blinding
After completing the baseline assessment, the participants will be randomized into three intervention groups; twice-weekly KBA, thrice-weekly KBA, and conventional physiotherapy (control) in the ratio of 1:1:1. The randomization will be performed using an online randomization generator (http://www.randomization.com) by utilizing block randomization with a block size of 3 and 6. A third party not involved in the study will perform the randomization process. Allocation of participants will be concealed using consecutive numbered, sealed, and opaque envelopes. The outcome assessors (physiotherapists) will be blinded to the group allocation and will not be involved in administering the interventions. The participants will be told they are in a “twice weekly KBA” or “thrice-weekly KBA” or “conventional physiotherapy,” but the type of intervention will not be specified. Conversely, due to the nature of the interventions, it will be difficult to blind the physiotherapists providing the treatments. Unbinding conditions will be only permissible when there is a medical emergency.
Interventions
Participants in the conventional physiotherapy group will receive brief patient education, ultrasound therapy, and stretching and strengthening exercises. The program will be delivered twice weekly for 8 weeks except for the education program which will be provided in two sessions. The stretching exercises will be performed as warm-up and cool-down. Participants in the twice-weekly KBA group will receive two sessions per week of the KBA exercise training for 8 weeks whereas participants in the thrice-weekly KBA will receive three sessions per week of the same exercise training as for the twice-weekly KBA group. Both the two KBA exercise training groups will receive the same intervention program as described for the conventional physiotherapy group prior to receiving the KBA exercise training. All exercises will be delivered individually under the supervision of the treating physiotherapists. All lower-extremity exercises will be performed bilaterally. The participants will be instructed to perform exercises consistent with their group allocation two times per day at home to encourage self-management. They will be encouraged also to perform a walking exercise of 30 min per day at least 3 to 4 days per week at home. To enhance compliance with the home program, a leaflet with descriptions and pictures of the exercises will be provided to the participants. However, exercises that are more challenging or those requiring the strict supervision of the therapist will be not advised for the home program.
Brief patient education
Prior to exercise training, the participants will receive a brief education lasting approximately 15 to 20 min. The program will be delivered by the therapist responsible for exercise training. It will be provided in a group of 3 to 5 or more participants to save time and effort. The key topics to be addressed include (1) understanding of knee OA, (2) lifestyle and physical activity/exercise, (3) diet and weight control, (4) self-management skills including active coping and pacing as well as correct use of medications (e.g., paracetamol), and (5) ergonomics and joint protection.
Ultrasound therapy (UST)
The affected knee of the participants will be treated with UST using direct contact technique. A coupling medium (ultrasonic gel) will be used. The treatment parameters to be used include (1) frequency = 1MHz, (2) pulse width = 2.0 W/cm2, (3) pulse rest time = 1:1 (continuous mode), and (4) treatment time = 7 min. The UST will precede the stretching and strengthening exercises.
Stretching and strengthening exercises
Participants will perform 3 lower-extremity stretching and strengthening exercises commonly prescribed for individuals with knee OA as described in previous studies [45, 49]. Progression for the strengthening exercises will be made by increasing the number of sets from 15 s hold to 30 s hold when the 15 s hold is no longer challenging, and the patient is performing an activity with ease and good form. However, the exercise will be discontinued if the patient reports an exacerbation of symptoms. Details of the stretching and strengthening exercises are provided in Table 1.
Kinesthesia, balance and agility exercises
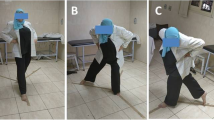
The exercise regimen of KBA will be done by performing a series of walking-based agility and balance exercises. The exercise protocol was adapted from previous studies [42, 44, 45] but with slight modifications regarding the training intensity and addition of visual manipulation for some selected walking-based agility exercises. The participants will perform agility exercises before proceeding to static and dynamic balance exercises. For the agility exercises, participants will begin each exercise with a walking pace of approximately 15 steps and progress to a maximum of approximately 75 steps [44, 45]. For balance training, participants will start with exercises while standing on a hard surface or floor and then proceed to exercises while standing on a form surface (Balance Soft Mat, BigMall, Nigeria). The form provides a more difficult task compared to the hard floor. Static balance exercises will be performed before progressing to dynamic balance exercises. For example, static balance will begin with a one-leg stand on a hard floor before progressing to a one-leg stand on the trainer foam [45]. The dynamic balance exercises will be progressed in the same manner but will require perturbations in different directions to be provided by the physiotherapist. The progression of each balance exercise to the next will be based on the participant’s ability by starting with the less stressful and challenging ones and increasing the number of repetitions. Participants will perform at least 3 sets of each exercise, and there will be 10 to 20 s rest between each exercise. All exercises will be progressed according to the individual’s tolerance and abilities within the structure of the program. If an exercise proved very difficult, the duration of the exercise will be adjusted based on the patient’s ability but no activity will be eliminated. However, the exercise will be discontinued if the patient reports an exacerbation of symptoms. The details of the KBA exercises are presented in Table 2.
Outcome assessments and follow-ups
The primary outcome will be physical function whereas the secondary outcomes will be pain intensity, knee stability, proprioception, and quality of life. Similar to previous trials on knee OA, if only one knee of the patient is affected, the evaluation of the outcomes will be done for this knee. If the patient has bilateral affectation of which only one meets the ACR criterion [48], only this knee will be evaluated. However, if the patient is having bilateral affectation according to the ACR criterion, the more painful knee will be selected for outcome evaluation.
All outcomes will be assessed pre-intervention, immediately post-intervention and at 3 months, 4 months, and 6 months post-randomization. Participants missing their regular appointments will be given makeup appointments until they reach the required sessions for each group. This will be done by contacting them through phone calls. All participants will be advised to refrain from other interventions during the trial except for those taking medications as prescribed by their physician and this information will be collected.
Physical function
The physical function of the participants will be assessed with the Hausa version of the Ibadan Knee and Hip Osteoarthritis Outcome Measure (IKHOAM) [50]. It is a 33-item instrument with 3 domains consisting of activity limitations, participation restrictions, and physical performance tests to assess physical function. Each item is rated on a Likert scale that ranges from 0 to 5. The measure is a Nigerian culture and environment-friendly clinical instrument developed for individuals with knee OA [51]. To obtain the patient’s percentage perceived level of physical function, the participant’s scores obtained are divided by the total possible score (232) and then multiplied by 100. Lower scores indicate a lower level of physical functioning [51]. The Hausa IKHOAM has been shown to have adequate internal consistency (0.64–0.95) and construct validity [50].
Pain intensity
The Visual Analogue Scale for pain (VAS-pain) will be used to assess participants’ pain severity. It represents the intensity dimension by a 100 mm bidirectional plain line with anchor points of “no pain” (0 mm) and “worst possible pain” (100 mm) located at either end of the line [52]. Participants will be asked to rate their current level of pain by marking anywhere along the 100mm line that best indicates thier knee pain. The VAS-pain has been commonly used to evaluate pain intensity in osteoarthritic knee pain. The Hausa version of the VAS-pain has adequate alternate forms reliability (r = 0.93) [53] and construct validity [54] and will be used in this study.
Knee stability
Participants’ subjective reports of knee stability will be measured with the Knee Outcome Survey-Activities of Daily Living Scale (KOS-ADLS). It is a 14-item questionnaire that assesses symptom-related and specific functional limitations [55]. Six items assess knee symptoms (pain, stiffness, swelling, instability, weakness, and limping), and eight items assess functional limitations (walking, stairs ascent/descent, standing, kneeling, squatting, sitting, and rising from a sitting position) experienced in the last 1 to 2 days during the performance of daily activities. Each item is scored on a 6-point Likert scale (0–5 points) [56]. The score is transformed to a 0–100 point scale with the highest score indicating the absence of symptoms and functional limitations [55]. For the purpose of this study, only the item pertaining to knee instability symptoms will be evaluated. The KOS-ADLS has been shown to have excellent internal consistency (0.92–0.93), test-retest reliability (intraclass correlation coefficient [ICC] = 0.97), and adequate construct validity [55].
Proprioception
The participants’ knee proprioceptive range of motion will be measured using an electrogoniometer (Ergotest Technology, Norway; range: 15–320°). The use of an electrogoniometer for measuring the relative position of the knee joint has been shown to be a reliable method for assessing joint proprioception [57]. To measure the proprioceptive range of motion, the participants will be asked to wear shorts for ease of attachment of the electrogoniometer to the knee joint [58]. The participants’ eyes will be blinded to eliminate visual feedback. They will be asked to sit on a high plinth with the hip at an angle of 80° flexion in such a way that the distal hamstrings and knee joint are hanging freely at a resting position of 85° knee flexion. A thin foam will be wrapped around the tested knee to minimize cutaneous sensation feedback from the attachment of the electrogoniometer [59]. While keeping the knee in a neutral position, the electrogoniometer will be placed on the lateral side of the knee joint and its axis coinciding with the flexion/extension axis of the knee [60]. The goniometer will be kept in place using an elastic strap wrapped around the cushion padding. Participants will be instructed to bend the knee to a resting position of 85° of flexion and in this position, they will be instructed to bend from the resting position to the target angle (TA) of 70° and hold there for 5 s, then return to the resting position (85° of flexion) [61, 62]. The participants will be then asked to repeat the procedure of bending the knee from the resting position of 85° and say “YES” on perceiving they reached the target position of 70° and hold. This angle will be noted on the electrogoniometer and documented as the perceived angle (PA). The difference between TA and PA is the absolute angular error (AAE), which will be documented [61]. This procedure will be repeated three times and the average of the three readings will be calculated and recorded as the error for each participant [57]. The inter-rater (between assessors) and intra-rater (within assessors) reliability of the electrogoniometer used in the present study will be evaluated.
Quality of life
The quality of life of the participants will be measured using the mini Osteoarthritis Knee and Hip Quality of Life Questionnaire (OAKHQOL) [63]. It is a 20-item questionnaire derived from the original 40-item questionnaire developed by Rat et al. [64]. The questionnaire consists of five dimensions subscales: physical activities, mental health, pain, social support, and social functioning; and three independent items addressing sexual life, professional life, and fear of being dependent. Each item is measured on a numerical rating scale from 0 to 10 and the mean item score becomes the corresponding dimension score [63]. The mini OAKHQOL has been shown to have adequate internal consistency (0.78–0.95), test-retest reliability (ICC = 0.66–0.89), and factorial validity in subjects with knee and hip OA [65].
As no Hausa versions of the KOS-ADLS and OAKHQOL are available for use, these questionnaires will be translated from English into Hausa language using guidelines for the process of cross-cultural adaptation of self-report measures [66]. This is to ensure that reliable data is collected and participants who are unable to complete English measures are not excluded in the trial [54]. However, English versions of IKHOAM, VAS-pain, KOS-ADLS, and OAKHQOL will be applied to those willing to respond in English.
Adverse events
Based on the findings of our pilot study (unpublished data), no serious adverse events were reported with the KBA exercise training program. However, all participants will be informed during recruitment of the possibility of experiencing common adverse events related to exercise interventions such as muscle pull, soreness, or cramp. They will be educated that these symptoms are temporary and self-limiting. Nonetheless, in case of any serious adverse events such as exacerbating joint pain, discernible joint swelling, and excessive fatigue, they will be advised to report such events immediately to the primary investigator or treating therapists for assessment and prompt action. Any adverse events will be recorded and reported to the research ethics committee of Aminu Kano Teaching Hospital, or National Orthopaedic Hospital Dala, or Kano State Ministry of Health, Nigeria.
Sample size estimation
Based on the results of our pilot study (unpublished data), using the effect size of 0.185 for between-group difference in the primary outcome (physical function measured by IKHOAM), a priori sample size was calculated assuming a statistical power of 90%, an alpha of 5% (two-tailed), and an effect size of 0.47. The calculations suggested a sample size of 102 would be needed. However, while anticipating a 20% attrition rate (n = 20), a total sample size of 120 will be needed with 40 participants per group. The calculations were performed with the G-power 3.1.9.2 software (University of Dusseldorf, Dusseldorf, Germany) [67].
Statistical analysis
An independent statistician who will be blinded to the study procedures will conduct all statistical analyses. The normality test of the data will be verified with the Shapiro–Wilk test and visual inspection of distribution plots. To account for potential missing data in datasets, per-protocol (PP) and intention-to-treat (ITT) approaches will be considered for the data analysis. For the PP approach, only participants who completed all treatment sessions will be included in the analysis. For the ITT approach, multivariate imputation by chained equations will be employed [68]. Descriptive statistics of mean and standard deviation will be used to summarize all continuous variables while frequency and percentages will be used to summarize all categorical variables. Mixed between-within subject ANOVA will be used to assess interaction effect (group x time), main effects for time, and between-subjects effect if the data is normally distributed. However, Friedman’s ANOVA and Kruskal–Wallis test will be used to analyze within-group change and between-group difference, respectively, if the data is not normally distributed. Post hoc analysis using Bonferroni correction will be conducted for any significant between-group difference observed. Effect size will be also computed to determine the magnitude of change in outcomes. All data will be analyzed using SPSS version 23 (IBM Co., Armonk, NY, USA) at an alpha level of 0.05.
Data management
After baseline assessment, all participants will be recognized only by their initials and numbers. Data will be stored using paper files, computer hard drive, and electronically to have a backup copy. All data values will be double-checked by assessors to check for errors and missing values before analysis.
Dissemination
The results of this study will be submitted for publication to an international peer-reviewed journal irrespective of whether the results are positive, negative, or inconclusive.
Discussion
There is evidence to suggest proprioceptive deficits in individuals with knee OA and that neuromuscular training programs targeting to improve proprioception are beneficial among these individuals [29,30,31,32,33,34]. The effectiveness of KBA as a proprioceptive training program in individuals with knee OA has been recently tested in clinical trials [36, 44,45,46,47,48], however, clinicians need to know the ideal dosage of KBA associated with the highest effectiveness as results of these previous trials were mixed. The present study will be aiming to determine the effects of a structured KBA exercise training program with different frequencies of treatment sessions (i.e., twice-weekly or thrice-weekly) on physical function, pain intensity, knee stability, proprioception, and quality of life in adults with knee OA. The outcomes will be evaluated at 8 weeks, 3 months, 4 months, and 6 months after randomization. We hope to follow-up the patients for a year if the 6-month follow-up results suggest this would be useful.
The findings of this study may provide evidence on the effectiveness of the KBA exercise training and the ideal number of sessions needed to achieve the highest effectiveness, which may guide clinical practice and minimize waste of time and resources.
Potential factors that could account for the limitations of the present study may include the lack of blinding of the treating therapists due to the nature of the interventions. Furthermore, because the present study is a multi-center trial employing the services of different treatment therapists with different skills and expertise, we cannot rule out the possibility of differential treatment. However, the assessor blind, three-arm RCT design with concealed allocation can be considered as the strengths of our study.
Trial status
Recruitment of participants is on-going since February 2018 and is expected to be completed by June 2021 (PACTR201810713260138, registered on 28 November 2017). However, due to the COVID-19 pandemic, recruitment may not be completed until December 2021.
Availability of data and materials
The full protocol for the study will be made available by the corresponding author on request.
Abbreviations
- AAE:
-
Absolute angular error
- ACR:
-
American College of Rheumatology
- AKTH:
-
Aminu Kano Teaching Hospital
- ANOVA:
-
Analysis of variance
- IKHOAM:
-
Ibadan Knee and Hip Osteoarthritis Outcome Measure
- KBA:
-
Kinesthesia, balance and agility
- KOS-ADLS:
-
Knee Outcome Survey-Activities of Daily Living Scale
- MAWTH:
-
Muhammad Abdullahi Wase Teaching Hospital
- MCID:
-
Minimal clinically important difference
- MMSH:
-
Murtala Muhammad Specialist Hospital
- NOHD:
-
National Orthopedic Hospital Dala
- PA:
-
Perceived angle
- PACTR:
-
Pan African Clinical Trials Registry
- PR:
-
Proprioceptive
- OA:
-
Osteoarthritis
- OAKHQOL:
-
Osteoarthritis Knee and Hip Quality of Life Questionnaire
- RCT:
-
Randomized controlled trial
- SPIRIT:
-
Standard Protocol Items: Recommendations for Interventional Trials
- TA:
-
Target angle
- UST:
-
Ultrasound therapy
- VAS:
-
Visual Analogue Scale
- WOMAC:
-
Western Ontario and McMaster Universities Osteoarthritis Index
References
Shane Anderson A, Loeser RF. Why is osteoarthritis an age-related disease? Best Pract Res Clin Rheumatol. 2010;24(1):15–26. https://doi.org/10.1016/j.berh.2009.08.006.
Charlesworth J, Fitzpatrick J, Perera NKP, Orchard J. Osteoarthritis- a systematic review of long-term safety implications for osteoarthritis of the knee. BMC Musculoskelet Disord. 2019;20(1):151. https://doi.org/10.1186/s12891-019-2525-0.
Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393(10182):1745–59. https://doi.org/10.1016/S0140-6736(19)30417-9.
Litwic A, Edwards MH, Dennison EM, Cooper C. Epidemiology and burden of osteoarthritis. Br Med Bull. 2013;105(1):185–99. https://doi.org/10.1093/bmb/lds038.
Silverwood V, Blagojevic-Bucknall M, Jinks C, Jordan JL, Protheroe J, Jordan KP. Current evidence on risk factors for knee osteoarthritis in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2015;23(4):507–15. https://doi.org/10.1016/j.joca.2014.11.019.
Chu CR, Millis MB, Olson SA. Osteoarthritis: from palliation to prevention: AOA critical issues. J Bone Joint Surg Am. 2014;96(15):e130. https://doi.org/10.2106/JBJS.M.01209.
Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163–96. https://doi.org/10.1016/S0140-6736(12)61729-2.
Deshpande BR, Katz JN, Solomon DH, Yelin EH, Hunter DJ, Messier SP, et al. Number of persons with symptomatic knee osteoarthritis in the US: impact of race and ethnicity, age, sex, and obesity. Arthritis Care Res. 2016;68(12):1743–50. https://doi.org/10.1002/acr.22897.
Usenbo A, Kramer V, Young T, Musekiwa A. Prevalence of arthritis in Africa: a systematic review and meta-analysis. PLoS One. 2015;10(8):e0133858. https://doi.org/10.1371/journal.pone.0133858.
Akinpelu AO, Alonge TO, Adekanla BA, Odole AC. Prevalence and pattern of symptomatic knee osteoarthritis in Nigeria: a community-based study. Internet J Allied Health Sci Pract. 2009;7(3):10.
Akinpelu A, Maduagwu S, Odele A, Alonge T. Prevalence and pattern of knee osteoarthritis in a North Eastern Nigerian rural community. East Afr Orthop J. 2011;5(1):48–54.
Ebong WW. Osteoarthritis of the knee in Nigerians. Ann Rheum Dis. 1985;44(10):682–4. https://doi.org/10.1136/ard.44.10.682.
Ibrahim D, Borodo M, Adelowo O. Clinical pattern of knee osteoarthritis in patients seen at rheumatology clinic of Aminu Kano Teaching Hospital, Northwestern Nigeria. Afr J Rheum. 2014;2(1):13–7.
Akinpelu A, Alonge O, Adekanla B, Odole A. Pattern of osteoarthritis seen in physiotherapy facilities in Ibadan and Lagos, Nigeria. Afr J Biomed Res. 2007;10(2):111–5.
Adebusoye L, Ogunbode A, Alonge T. Magnitude of knee osteoarthritis and associated risk factors among adult patients presenting in a family practice clinic in Nigeria. J Med Tropics. 2013;15(2):144–50.
Greene MA, Loeser RF. Aging-related inflammation in osteoarthritis. Osteoarthritis Cartilage. 2015;23(11):1966–71. https://doi.org/10.1016/j.joca.2015.01.008.
Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med. 2010;26(3):355–69. https://doi.org/10.1016/j.cger.2010.03.001.
King LK, Kendzerska T, Waugh EJ, Hawker GA. Impact of osteoarthritis on difficulty walking: a population-based study. Arthritis Care Res. 2018;70(1):71–9. https://doi.org/10.1002/acr.23250.
Choquette D, Raynauld JP, Rich E. Basic principles in osteoarthritis treatment. In: Reginster JY, Pelletier JP, Martel-Pelletier J, Henrotin Y, Crasborn L, editors. Osteoarthritis: Clinical and Experimental Aspects. Berlin, Heidelberg: Springer Berlin Heidelberg; 1999. p. 356–70.
Nelson AE, Allen KD, Golightly YM, Goode AP, Jordan JM. A systematic review of recommendations and guidelines for the management of osteoarthritis: the chronic osteoarthritis management initiative of the US bone and joint initiative. Semin Arthritis Rheum. 2014;43(6):701–12. https://doi.org/10.1016/j.semarthrit.2013.11.012.
Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee: a Cochrane systematic review. Br J Sports Med. 2015;49(24):1554–7. https://doi.org/10.1136/bjsports-2015-095424.
Briani RV, Ferreira AS, Pazzinatto MF, Pappas E, De Oliveira SD, Azevedo FMD. What interventions can improve quality of life or psychosocial factors of individuals with knee osteoarthritis? A systematic review with meta-analysis of primary outcomes from randomised controlled trials. Br J Sports Med. 2018;52(16):1031.
McAlindon TE, Bannuru RR, Sullivan MC, Arden NK, Berenbaum F, Bierma-Zeinstra SM, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage. 2014;22(3):363–88. https://doi.org/10.1016/j.joca.2014.01.003.
Kolasinski SL, Neogi T, Hochberg MC, Oatis C, Guyatt G, Block J, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Rheum. 2020;72(2):220–33. https://doi.org/10.1002/art.41142.
Brosseau L, Taki J, Desjardins B, Thevenot O, Fransen M, Wells GA, et al. The Ottawa panel clinical practice guidelines for the management of knee osteoarthritis. Part two: strengthening exercise programs. Clin Rehabil. 2017;31(5):596–611. https://doi.org/10.1177/0269215517691084.
Brosseau L, Taki J, Desjardins B, Thevenot O, Fransen M, Wells GA, et al. The Ottawa panel clinical practice guidelines for the management of knee osteoarthritis. Part three: aerobic exercise programs. Clin Rehabil. 2017;31(5):612–24. https://doi.org/10.1177/0269215517691085.
Brosseau L, Taki J, Desjardins B, Thevenot O, Fransen M, Wells GA, et al. The Ottawa panel clinical practice guidelines for the management of knee osteoarthritis. Part one: introduction, and mind-body exercise programs. Clin Rehabil. 2017;31(5):582–95. https://doi.org/10.1177/0269215517691083.
Goh S-L, Persson MSM, Bhattacharya A, Hall M, Doherty M, Zhang W. Relative efficacy of different types of exercise for treatment of knee and hip osteoarthritis: protocol for network meta-analysis of randomised controlled trials. Syst Rev. 2016;5(1):147. https://doi.org/10.1186/s13643-016-0321-6.
Smith TO, King JJ, Hing CB. The effectiveness of proprioceptive-based exercise for osteoarthritis of the knee: a systematic review and meta-analysis. Rheumatol Int. 2012;32(11):3339–51. https://doi.org/10.1007/s00296-012-2480-7.
Lephart SM, Fu FH. Proprioception and neuromuscular control in joint stability. Champaign, IL: Human Kinetics Inc; 2000.
Sharma L. Proprioceptive impairment in knee osteoarthritis. Rheum Dis Clin North Am. 1999;25(2):299–314. https://doi.org/10.1016/S0889-857X(05)70069-7.
Felson DT, Gross KD, Nevitt MC, Yang M, Lane NE, Torner JC, et al. The effects of impaired joint position sense on the development and progression of pain and structural damage in knee osteoarthritis. Arthritis Rheum. 2009;61(8):1070–6. https://doi.org/10.1002/art.24606.
Lund H, Juul-Kristensen B, Hansen K, Christensen R, Christensen H, Danneskiold-Samsoe B, et al. Movement detection impaired in patients with knee osteoarthritis compared to healthy controls: a cross-sectional case-control study. J Musculoskelet Neuronal Interact. 2008;8(4):391–400.
Jeong HS, Lee SC, Jee H, Song JB, Chang HS, Lee SY. Proprioceptive training and outcomes of patients with knee osteoarthritis: a meta-analysis of randomized controlled trials. J Athl Train. 2019;54(4):418–28. https://doi.org/10.4085/1062-6050-329-17.
Anwer S, Alghadir A, Brismée JM. Effect of home exercise program in patients with knee osteoarthritis: a systematic review and meta-analysis. J Geriatr Phys Ther. 2016;39(1):38–48. https://doi.org/10.1519/JPT.0000000000000045.
Rogers MW, Tamulevicius N, Coetsee MF, Curry BF, Semple SJ. Knee osteoarthritis and the efficacy of kinesthesia, balance & agility exercise training: a pilot study. Int J Exerc Sci. 2011;4(2):124–32.
Fitzgerald GK, Axe MJ, Snyder-Mackler L. The efficacy of perturbation training in nonoperative anterior cruciate ligament rehabilitation programs for physically active individuals. Phys Ther. 2000;80(2):128–14. https://doi.org/10.1093/ptj/80.2.128.
Liu-Ambrose T, Taunton JE, MacIntyre D, McConkey P, Khan KM. The effects of proprioceptive or strength training on the neuromuscular function of the ACL reconstructed knee: a randomized clinical trial. Scan J Med Sci Sports. 2003;13(2):115–23. https://doi.org/10.1034/j.1600-0838.2003.02113.x.
Mandelbaum BR, Silvers HJ, Watanabe DS, Knarr JF, Thomas SD, Griffin LY, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33(7):1003–10. https://doi.org/10.1177/0363546504272261.
Hurd WJ, Chmielewski TL, Snyer-Mackler L. Perturbation-enhanced neuromuscular training alters muscle activity in female athletes. Knee Surg Sports Traumatol Arthrosc. 2006;14(1):60–9. https://doi.org/10.1007/s00167-005-0624-y.
Eils E, Rosenbaum D. A multi-station proprioceptive exercise program in patients with ankle instability. Med Sci Sports Exerc. 2001;33(12):1991–8. https://doi.org/10.1097/00005768-200112000-00003.
McGuine TA, Keen JS. The effect of a balance training program on the risk of ankle sprains in high school athletes. Am J Sports Med. 2001;34:1103–11.
Fitzgerald GK, Childs JD, Ridge TM, Irrgang JJ. Agility and perturpation training for a physically active individual with knee osteoarthritis. Phys Ther. 2002;82(4):372–82. https://doi.org/10.1093/ptj/82.4.372.
Rogers MW, Tamulevicius N, Semple SJ, Krkeljas Z. Efficacy of home-based kinesthesia, balance & agility exercise training among persons with symptomatic knee osteoarthritis. J Sports Sci Med. 2012;11(4):751–8.
Fitzgerald GK, Piva SR, Gil AB, Wisniewski SR, Oddis CV, Irrgang JJ. Agility and perturbation training techniques in exercise therapy for reducing pain and improving function in people with knee osteoarthritis: a randomized clinical trial. Phys Ther. 2011;91(4):452–69. https://doi.org/10.2522/ptj.20100188.
Diracoglu D, Aydin R, Baskent A, Celik A. Effects of kinesthesia and balance exercises in knee osteoarthritis. J Clin Rheumatol. 2005;11(6):303–10. https://doi.org/10.1097/01.rhu.0000191213.37853.3d.
Sekir U, Gür H. A multi-station proprioceptive exercise program in patients with bilateral knee osteoarthrosis: functional capacity, pain and sensoriomotor function. A randomized controlled trial. J Sports Sci Med. 2005;4(4):590–603.
Chaipinyo K, Karoonsupcharoen O. No difference between home-based strength training and home-based balance training on pain in patients with knee osteoarthritis: a randomised trial. Aust J Physiother. 2009;55(1):25–30. https://doi.org/10.1016/S0004-9514(09)70057-1.
Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986;29(8):1039–49. https://doi.org/10.1002/art.1780290816.
Odole AC, Akinpelu AO. Validity and internal consistency of a Hausa version of the Ibadan Knee/Hip Osteoarthritis Outcome Measure. Health Qual Life Outcomes. 2008;6(1):86. https://doi.org/10.1186/1477-7525-6-86.
Odole AC, Odunaiya NA, Akinpelu AO. Ibadan knee/hip osteoarthritis outcome measure: process of development. Ann Ib Postgrad Med. 2013;11(2):71–6.
Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW, Loge JH, et al. Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage. 2011;41(6):1073–93. https://doi.org/10.1016/j.jpainsymman.2010.08.016.
Odole AC, Akinpelu AO. Translation and alternate forms reliability of the Visual Analogue Scale in the three major Nigerian languages. Internet J Allied Health Sci Pract. 2009;7(3):13.
Ibrahim AA, Akindele MO, Bello B, Kaka B. Translation, cross-cultural adaptation, and psychometric properties of the Hausa versions of the Numerical Pain Rating Scale and Global Rating of Change Scale in a low-literate population with chronic low back pain. Spine. 2020;45(8):E439–47. https://doi.org/10.1097/BRS.0000000000003306.
Irrgang JJ, Snyder-Mackler L, Wainner RS, Fu FH, Harner CD. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998;80(8):1132–45. https://doi.org/10.2106/00004623-199808000-00006.
Roy JS, Esculier JF, Maltais DB. Translation, cross-cultural adaptation and validation of the French version of the Knee Outcome Survey-Activities of Daily Living Scale. Clin Rehabil. 2014;28(6):614–23. https://doi.org/10.1177/0269215513511342.
Olsson L, Lund H, Henriksen M, Rogind H, Bliddal H, Danneskiold-Samsøe B. Test–retest reliability of a knee joint position sense measurement method in sitting and prone position. Adv Physiother. 2004;6(1):37–47. https://doi.org/10.1080/14038190310009894.
Piriyaprasarth P, Morris ME, Winter A, Bialocerkowski AE. The reliability of knee joint position testing using electrogoniometry. BMC Musculoskelet Disord. 2008;9(1):6. https://doi.org/10.1186/1471-2474-9-6.
Larsen R, Lund H, Christensen R, Røgind H, Danneskiold-Samsøe B, Bliddal H. Effect of static stretching of quadriceps and hamstring muscles on knee joint position sense. Br J Sports Med. 2005;39(1):43–6. https://doi.org/10.1136/bjsm.2003.011056.
Gerhardt JJ. Documentation of Joint Motion: International Standard Neutral-zero Measuring, SFTR Recording and Application of Goniometers, Inclinometers, and Calipers. Portland: Isomed Inc; 1996.
Pradeep T, Solomen S, Aaron P. The influence of dynamic stretch of quadriceps, hamstrings and its combined stretch effect on knee joint position sense (JPS) in healthy adults. Int J Multidiscip Res Dev. 2016;3(7):50–4.
Han J, Waddington G, Adams R, Anson J, Liu Y. Assessing proprioception: a critical review of methods. J Sport Health Sci. 2016;5(1):80–90. https://doi.org/10.1016/j.jshs.2014.10.004.
Guillemin F, Rat AC, Goetz C, Spitz E, Pouchot J, Coste J. The Mini-OAKHQOL for knee and hip osteoarthritis quality of life was obtained following recent shortening guidelines. J Clin Epidemiol. 2016;69:70–8. https://doi.org/10.1016/j.jclinepi.2015.06.010.
Rat AC, Pouchot J, Coste J, Baumann C, Spitz E, Retel-Rude N, et al. Development and testing of a specific quality-of-life questionnaire for knee and hip osteoarthritis: OAKHQOL (OsteoArthritis of Knee Hip Quality Of Life). Joint Bone Spine. 2016;73(6):697–704.
Gonzalez Saenz de Tejada M, Bilbao A, Herrera C, Garcia L, Sarasqueta C, Escobar A. Validation of the Mini-OAKHQOL for use in patients with osteoarthritis in Spain. Clin Rheumatol. 2017;36(8):1855–64. https://doi.org/10.1007/s10067-017-3611-z.
Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25(24):3186–91. https://doi.org/10.1097/00007632-200012150-00014.
Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–91. https://doi.org/10.3758/BF03193146.
Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res. 2011;20(1):40–9. https://doi.org/10.1002/mpr.329.
Acknowledgements
We would like to thank the entire physiotherapists who will be assisting in the recruitment, assessment, and treatment of patients in this study. We also acknowledge the head of the Physiotherapy Department of Muhammad Abdullahi Wase Teaching Hospital, Murtala Muhammad Specialist Hospital, Aminu Kano Teaching Hospital, and National Orthopaedic Hospital Dala for their valuable support.
Funding
This research received no grant from any funding agency.
Author information
Authors and Affiliations
Contributions
AIA is the Principal Investigator. AIA conceived the study. AIA and AAI developed the first draft of the protocol. AAI reviewed and edited the protocol. MOA supervised the protocol. AAI proposed the statistical analyses. All authors contributed to the trial design. The authors have read, contributed to, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study got ethical approval from the Health Research Ethics Committee of Ministry of Health, Kano State (MOH/Off/797/T.I./600); Aminu Kano Teaching Hospital (AKTH), Kano State (MAC/SUB/12A/P-3/VI/2279); and National Orthopaedic Hospital Dala (NOHD), Kano State (NOHDK/RET/ETHIC/6O). Written informed consent was obtained from all participants prior to participating in the study. Any justifiable modifications to this protocol will be communicated to the aforementioned Health Research Ethics Committee as well as updated in the Pan African Clinical Trials Registry (PACTR201810713260138).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
SPIRIT 2013 Checklist: Recommended items to address in a clinical trial protocol and related documents*.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Adhama, A.I., Akindele, M.O. & Ibrahim, A.A. Effects of variable frequencies of kinesthesia, balance and agility exercise program in adults with knee osteoarthritis: study protocol for a randomized controlled trial. Trials 22, 470 (2021). https://doi.org/10.1186/s13063-021-05386-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-021-05386-3