Abstract
Background
Access for endovascular repair of abdominal aortic aneurysms (EVAR) is obtained through surgical cutdown or percutaneously. The only devices suitable for percutaneous closure of the 20 French arteriotomies of the common femoral artery (CFA) are the Prostar™ and Proglide™ devices (Abbott Vascular). Positive effects of these devices seem to consist of a lower infection rate, and shorter operation time and hospital stay. This conclusion was published in previous reports comparing techniques in patients in two different groups (cohort or randomized). Access techniques were never compared in one and the same patient; this research simplifies comparison because patient characteristics will be similar in both groups.
Methods/Design
Percutaneous access of the CFA is compared to surgical cutdown in a single patient; in EVAR surgery, access is necessary in both groins in each patient. Randomization is performed on the introduction site of the larger main device of the endoprosthesis. The contralateral device of the endoprosthesis is smaller. When we use this type of randomization, both groups will contain a similar number of main and contralateral devices. Preoperative nose cultures and perineal cultures are obtained, to compare colonization with postoperative wound cultures (in case of a surgical site infection). Furthermore, patient comfort will be considered, using VAS-scores (Visual analog scale). Punch biopsies of the groin will be harvested to retrospectively compare skin of patients who suffered a surgical site infection (SSI) to patients who did not have an SSI.
Discussion
The PiERO trial is a multicenter randomized controlled clinical trial designed to show the consequences of using percutaneous access in EVAR surgery and focuses on the occurrence of surgical site infections.
Trial registration
NTR4257 10 November 2013, NL44578.042.13.
Similar content being viewed by others
Background
Percutaneous endovascular abdominal aortic aneurysm repair (pEVAR) has been stated to be safe and feasible [1], even though several publications report a substantial number of complications [2–4]. With evolving experience, various risk factors have been identified, including obesity, groin scarring, common femoral artery (CFA) morphology and tortuous iliac arteries [1, 5].
Many current devices successfully close percutaneous punctures of the CFA up to 8 Fr.: such as the Angio-Seal™ (St. Jude Medical, Minnetonka, MN, USA), Mynx™ (AccessClosure, Mountain View, CA, USA), and the Starclose™ device (Abbott Vascular, Redwood City, CA, USA). The Prostar XL™ device (Abbott Vascular) has been used in femoral arteries, after sheaths of 18 to 24 Fr., with high rates of procedural success [1]. Wound infections appear to be absent [3, 6, 7] or few (0.2 %) [8]. In contrast, open femoral access has wound infection rates varying from 6.4 % [9] to 7.3 % [7]. Also, a longer surgery and hospital stay have been reported [10–12]. In percutaneous access, secondary interventions were more commonly seen, compared to surgical cutdown [10, 11]. Still, in suitable patients, this seems to be the only device capable of closing a 20 Fr. percutaneous arterial access site.
Although research has been performed, comparing both techniques, a comparison of both techniques in one patient has never been performed prior to now. Risk factors (obesity, CFA morphology and tortuosity of the iliac arteries) will be equally divided in this study design. Therefore, postoperative complications will mainly depend on the technique used and on the diameter of the device implanted. Also, each patient will be able to compare the result of both techniques by subjective pain sensation or discomfort.
Methods/Design
Study design
In the current study, percutaneous femoral access is compared to open femoral access. Bilateral femoral access is required in each patient treated with a bifurcated EVAR. Therefore, each patient can serve as his/her own control. Randomization is performed for the caliber of the endovascular device (main device versus contralateral extension) that is introduced within the aorta.
The PiERO trial is designed as a randomized, controlled, nonblinded, multicenter superiority trial with two parallel groups and a primary endpoint of wound infection during the 30 days after surgery. Simple randomization will be performed concerning the diameter of the device component introduced in the artery, with a 1:1 allocation.
Sample size calculation
The assumption has been made that a pEVAR is less likely to cause a surgical site infection (SSI) than an EVAR with surgical cutdown to the femoral artery. We estimated the number of patients needed in a superiority trial with an effect size of 90 % and a margin of 10 (alpha 5 %, power 80 %). Assuming an SSI incidence of 6.8 % (Table 1) in an open surgical femoral cutdown and of 0.1 % in pEVAR, where p1 = 0.068 and p2 = 0.001 and using the equation n = 8 × (p1(1 − p1) + p2(1 − p2))/(p1 − p2)2 [13], 120 patients are required to reach sufficient evidence and avoid a type 2 error (including a fall-out percentage of 5 %).
Setting
The trial is a multicenter trial, including one academic hospital and four general hospitals in the northern part of the Netherlands. In each center, all vascular surgeons perform surgeries for this study (Table 2). Participating hospitals are outlined on www.pierotrial.nl. In participating centers, each surgeon or interventionalist performing the procedure must have had the experience of 20 Prostar™procedures or 10 Proglide™ procedures prior to including patients in the PiERO trial, to prevent a performance bias. The Proglide™ procedure is a procedure easier to master. A minimum experience of 20 surgical cut downs to the common femoral artery (CFA) is also required. All punctures of the CFA should be performed with ultrasound guidance.
Primary endpoints
The primary endpoints include the number of SSI’s in the groin within 30 days postoperatively and at final evaluation 1 year after the operation. Wounds will be evaluated by means of the Southampton Wound Assessment score [14]. This score lowers the variability in wound assessment by various researchers. When an SSI is diagnosed, both clinically and through the SWA score (Grade III or more), a wound culture should confirm the diagnosis, as described in the CDC definition (Centers for Disease Control and Prevention) [15].
Secondary endpoints
Wound complications in both groups are assessed during the first 30 days postoperatively. Close attention will be paid to hematoma, femoral neuropathy, dehiscence, fluid discharge, stenotic/occlusive complications in the CFA and signs of infection.
When a Staphylococcus aureus SSI occurs (as the major contributor to all in the groin), preoperative isolates will be compared to postoperative SSI involved strains.
All patients will score their wound comfort or pain in a validated VAS score 1 day, and 2 weeks after surgery. Outcomes for open femoral versus percutaneous access will be compared.
Percutaneous access of the CFA is expected to inflict less surgical site infections in the groin compared to open surgical cutdown of the CFA. A lower incidence of infections and localized postoperative problems is expected to offset the additional costs of the percutaneous device. Still, the reduction in complaints needs to be quantified.
Follow-up will be performed until 1 year after the operation, according to the definition of a surgical site infection: “if implant (the endoprosthesis) is in place and the infection appears to be related to the operation” [15].
Recent studies suggest that certain patients may be colonized by multiple different S. aureus clones [16]. Also, these bacteria may hide intracellularly [17]. In case of a SSI, we hope to identify the initial localization of the causative microorganism. Therefore, preoperative cultures and punch biopsies will be used, respectively, to study the clonality of isolates by genotyping and to identify intracellular bacteria by fluorescence in situ hybridization (FISH) and fluorescence microscopy [18].
Ethical considerations
Patients who meet the entry criteria will be fully informed about the trial and provided with a patient information and consent form. Patients willing to participate in the study will be included after signing the informed consent form. This study is being conducted in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice guidelines. The protocol, site-specific informed consent forms, participant education and recruitment materials, and other requested documents were reviewed and approved by the Medical Ethics committee of Groningen (CMO 2013-365) and the local institutional board of each participating center (Table 2).
Safety and quality control
Adverse events (AE) are defined as any undesirable experience occurring to a participant during the study, whether or not considered related to the investigational device. This definition includes events occurring during the hospital stay and up to 30 days of follow-up. Underlying disease that was present at the time of enrollment is not reported as an AE, but any increase in the severity of the underlying disease will be reported as an AE. All AEs will be monitored from the time of enrollment through the 30-day follow-up. AE’s will be recorded on the case record forms (CRFs). A description of the event, including the start date, end date, action taken and the outcome will be reported.
A severe adverse event (SAE) is any event leading to death, major amputation, prolonged hospitalization or renewed hospitalization due to complications and will be communicated to the Medical Ethical committee through “Toetsingonline.”
Inclusion criteria
In order to be eligible to participate in this study, a subject must meet all of the following criteria:
-
1.
More than 18 years of age.
-
2.
Informed consent.
-
3.
Physically and mentally capable of giving consent for participation and data storage.
-
4.
diagnosed with an aneurysm of the abdominal aorta with a diameter of at least 55 mm (or growth of 5 mm or more in 6 months) suitable for bifurcated endovascular repair through two femoral access sites, without additional access needed.
Exclusion criteria
Exclusion criteria are indicated as follows:
-
1.
Patients with severe atherosclerosis at the access site (more than 50 % of the circumference of the common femoral artery).
-
2.
Patients with previous common femoral artery surgery.
-
3.
Patients with a documented infection at the time of operation.
-
4.
Patients treated with an aorto-monoiliacal device implanted, followed by a femoro-femoral crossover.
-
5.
Patients with an aneurysm necessitating more than two accesses (brachial or carotid) for repair.
Recruitment
Patients more than 18 years of age and presenting at the outpatient clinic of participating hospitals, with an indication for bifurcated EVAR will be asked to participate. Patients will be informed about the purpose, and intervention of the study, its duration and the risks. Consent will be obtained with explanation and a signature on the Informed Consent Form. Patients have 1 week to consider their decision.
Withdrawal from the study is possible at any time for any reason and is without further consequences.
Randomization
Randomization will be performed prior to operation. The operating physician or his/her assistant must draw a blinded envelop to allocate the patient to one of the two groups.
In the first group (group A), surgical access is achieved for the main body of the endoprosthesis. In the second group (group B), the Prostar XL™/Proglide™ device gives passage to the main device.
The allocation will be noted at the case report form (CRF) present in the envelope, which also contains a circular blade of 3 mm diameter, and 3 culture mediums (Thioglycollate medium USP, Mediaproducts, Groningen, Germany). Two cultures are taken after completion of the preoperative checklist and after administration of prophylactic antibiotics (1 g cefazolin, intravenously 15 to 60 min before surgery): one nose culture and one perineal culture is performed with a swab, rotated at the nasal and perineal site. The punch biopsy is collected from the right groin after disinfection, a circular blade of 3 mm is rotated and 2 skin biopsies are harvested. One punch biopsy is stored in formaldehyde; the second punch biopsy is stored in the third culture medium.
The culture media and formaldehyde storages have been coded in advance by the investigator, who prepared the content of the blinded envelop, and these samples will be sent to the laboratory of CERTE in an enclosed addressed envelope.
Blinding
The operating team cannot be blinded for the allocation. Medical staff responsible for control visits and wound evaluation will be blinded for the passage of the main device or the contralateral leg. The scar of the Prostar XL™/Proglide™ device will, however, be smaller. This is an investigator-blinded study.
Emergency unblinding
To maintain the overall quality and legitimacy of the clinical trial, code breaks should occur only in exceptional circumstances when knowledge of the actual treatment is absolutely essential for further management of the patient. If unblinding is deemed necessary, the investigator should use the system for emergency unblinding through contacting the supervising investigator in writing. The objective database manager, who supervises the codes, is not allowed to give access to the coded patients, unless the supervising investigator (C.J. Zeebregts), in a written memo, gives approval.
Treatment details
Participant timelines
Participants are enrolled in the PiERO trial during their preoperative evaluation. Postoperative assessment is performed during the regular outpatient follow up.
Concomitant care
In case of an SSI, the wound must be opened, cultured and rinsed with clean water, as considered appropriate according to the treating physician. When infection persists or escalates, oral or intravenous antibiotics are administered. If a second operation is necessary to restrain an infection, this will be registered as an AE.
This trial has no prohibited concomitant medication.
Follow-up
Wound control is performed at 1 day, 2 weeks and 6 weeks after operation. Final evaluation will take place at 1 year after the procedure. This evaluation will be carried out for infection of the endoprosthesis, according to the definition [15]. The wound evaluation is carried out using the Southampton Wound Assessment score. Wound complications emerging in between measuring points (1 day, 2 weeks and 6 weeks) will also be recorded.
Three VAS scores (Visual Analog Scale) will be obtained before the operation, 1 day after the operation, and 2 weeks after the operation.
Scores are registered in the CRF (case report form) and collected by the objective database manager (Table 3).
Data management
All forms, diskettes and tapes related to study data will be kept by the database manager. Access to the study data will be restricted. Values will be stored in an Excel sheet. Each additional value added to the database will be stored in consecutively numbered Excel documents, in a security-coded computer. A complete back up of the primary DCC database will be performed weekly and will be stored in locked files (data cannot be altered).
Statistical analyses
Primary study parameter(s)
The occurrence of SSIs in both groups will be compared with a McNemar’s test and proportional hazards regression. Only two measuring points will be defined, but wound complications are expected to emerge also between these measuring points. A Kaplan Meier curve may be used to log incidences according to time. Both groups will be compared using the log rank test.
Secondary study parameter(s)
The number of wound complications in both groups will be compared as mentioned previously.
Patient characteristics will be controlled by multivariate analysis with respect to the duration of operation, left/right differences, preoperative bacterial colonization of the nose and the perineum, diabetes mellitus, body mass index, medication, smoking habits and device failure. Although identical groups are examined, we will be able to identify outliers.
Correlations between factors will be estimated using the Pearson correlation coefficient. Proportions of categorical variables are compared using Chi square and Fisher Exact tests, and means of continuous variables are compared using t tests.
The analysis of the primary endpoint (surgical site infection) will be based on an intention-to-treat principle by proportional hazards regression (visualized by Kaplan-Meier survival curves). Intention-to-treat implies that open access because of failed percutaneous access is not excluded from analysis but remains in the percutaneous group. Reasons why percutaneous access may not be successful are inability to obtain access to the arterial lumen with a needle, rupture of the threads of the Prostar XL™ device/2 Proglide™ devices, necessitating open repair and persistent bleeding despite successful use of the Prostar XL™ device/2 Proglide™ devices. The survival analysis is not affected by patient withdrawals (as they will be censored) provided that dropping out is unrelated to prognosis (Table 4). Other outcomes, such as VAS scores 2 weeks post-randomization, may be missing for patients who withdraw from the trial. We will actively seek out reasons for withdrawal and compare the reasons qualitatively.
Publication of data
The scientific integrity of the project requires that the data from all sites be analyzed study-wide and reported as such. Thus, an individual center is not expected to report the data collected from its center alone. All presentations and publications are expected to protect the integrity of the major objectives of the study.
Recommendations will be given by Abbott, and Abbott will be granted the nonexclusive right to use any publication or presentation resulting from the research.
Publications will be prepared under the responsibility of the principle investigator and the contributions of all authors will be specified. A copy of such publication will be provided to Abbott for its review and comment. The principle investigator will give due consideration to any comments made by Abbott. Changes will be incorporated only when Abbott will require protection of Abbott’s proprietary rights and interests. This will not interfere with the ethical responsibility to disseminate the trial results in an unbiased and timely manner; consequently, Abbott cannot prohibit publication.
Discussion
Comparison of the incidence of SSIs in one patient may answer (an important part of) the question whether percutaneous closure devices deserve a role in the prevention of SSIs after EVAR. The cost of an SSI is estimated to be between US $10.000, and $20.000 per infection [19]. In pEVAR, a trend was noticed to reduce procedure and hospitalization times [10–12, 20]. The aim of this study is to contribute to the rationale of using percutaneous devices for femoral access in EVAR.
Analysis will be performed on an intention-to-treat basis. When a percutaneous access, for some reason, is not successful, open access will be obtained. Reasons why percutaneous access may not be successful are described in the Statistical Analysis section.
For all participants, cultures of the nose and the perineum will be taken preoperatively. In addition, two punch biopsies from the right groin will be obtained to evaluate the presence of microorganisms in deeper layers of the skin or intracellularly (by culture/molecular methods and PA research). The intention is to compare cultures and SSIs as it becomes more apparent that differences in hostility between bacterial species and/or clones exists [16, 17]. Therefore, the assumption was made, that a SSI does not only develop due to flaws in sterility [21], but also because some bacteria might be able to conceal themselves better in or on their host, than other bacteria. We know that bacteria can hide intracellularly [17, 22], and take over resistance genes from each other. Therefore, it might be interesting to compare S. aureus strains not causing SSIs, to those that do cause an SSI.
In conclusion, the PiERO trial is a multicenter randomized controlled clinical trial designed to show the consequences of using percutaneous access in EVAR surgery, when considering surgical site infections. In addition, patient comfort, estimated hospital stay and other wound complications are taken under consideration.
Trial status
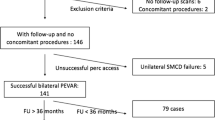
Patients have been included as follows in the various participating centers:
Abbreviations
- AE:
-
adverse event
- CERTE:
-
the name of the infectious laboratory
- CFA:
-
common femoral artery
- CMO:
-
Commissie Mensgebonden Onderzoek = Commission Research on Humans
- CRF:
-
case report form
- EVAR:
-
endo-vascular aneurysm repair
- FISH:
-
fluorescence in situ hybridization
- Fr.:
-
French
- Nm:
-
Not mentioned
- pEVAR:
-
percutaneous endovascular aneurysm repair
- PiERO:
-
Percutaneous access in Endovascular Repair versus Open access
- SAE:
-
serious adverse event
- SSI:
-
surgical site infection
- SWA-score:
-
Southampton Wound Assessment score
- VAS:
-
Visual Analog Scale
References
Jean-Baptiste E, Hassen-Khodja R, Haudebourg P, Bouillanne P-J, Declemy S, Batt M. Percutaneous closure devices for endovascular repair of infrarenal abdominal aortic aneurysms: a prospective, non-randomized comparative study. Eur J Vasc Endovasc Surg. 2008;35:422–8.
Wilson JS, Johnson BL, Parker JL, Back MR, Bandyk DF. Management of vascular complications following femoral artery catheterization with and without percutaneous arterial closure devices. Ann Vasc Surg. 2002;16:597–600.
Nehler MR, Lawrence WA, Whitehill TA, Charette SD, Jones DN, Krupski WC. Iatrogenic vascular injuries from percutaneous vascular suturing devices. J Vasc Surg. 2001;33:943–7.
Piffaretti G, Mariscalco G, Tozzi M, Rivolta N, Castelli P, Sala A. Predictive factors of complications after surgical repair of iatrogenic femoral pseudoaneurysms. World J Surg. 2011;35:911–6.
Torsello GBKB, Klenk E, Tessarek J, Osada N, Torsello GF. Endovascular suture versus cutdown for endovascular aneurysm repair: a prospective randomized pilot study. J Vasc Surg. 2003;38:78–82.
Eisenack M, Umscheid T, Tessarek J, Torsello GF, Torsello GB. Percutaneous endovascular aortic aneurysm repair: a prospective evaluation of safety, efficienty, and risk factors. J Endovasc Ther. 2009;16:708–13.
Zhong-han NI, Jian-fang LUO, Wen-hui HUANG, Yuan LIU, Ling XUE, Rui-xin FAN, et al. Totally percutaneous thoracic endovascular aortic repair with the preclosing technique: a case–control study. Chin Med J. 2011;124:851–5.
Johanning JM, Franklin DP, Elmore JR, Han DC. Femoral artery infections associated with percutaneous arterial closure devices. J Vasc Surg. 2001;34:983–5.
Postoperative Wound Infections. 2012. http://www.rivm.nl/dsresource?type=pdf&disposition=inline&objectid=rivmp:232885&versionid=&subobjectname. Accessed January 2014.
Torsello GB, Kasprzak B, Klenk E, Tessarek J, Osada N, Torsello GF. Endovascular suture versus cutdown for endovascular aneurysm repair: a prospective randomized pilot study. J Vasc Surg. 2003;38:78–82.
Morasch MD, Kibbe MR, Evans ME, Meadows WS, Eskandari K, Matsumura JS, et al. Percutaneous repair of abdominal aortic aneurysm. J Vasc Surg. 2004;40:12–6.
Metcalfe MM, Brownrigg JRW, Black SA, Loosemore T, Loftus IM, Thompson MM. Unselected percutaneous access with large vessel closure for endovascular aortic surgery: experience and predictors of technical success. Eur J Vasc Endovasc Surg. 2012;43:378–81.
Campbell MJ, Swinscow TDV. Statistics at square one. 11th ed. West Sussex: Wiley-Blackwell; 2009.
Bailey IS, Karran SE, Toyn K, Brough P, Ranaboldo C, Karran SJ. Community surveillance of complications after hernia surgery. Brit Med J. 1992;304:469–71.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Am J Infec Control. 1999;27:97–132.
van der Kooi-Pol MM, de Vogel CP, Westerhout-Pluister GN, Veenstra-Kyuchukova YK, Duipmans JC, Glasner C, et al. High anti-staphylococcal antibody titers in patients with epidermolysis bullosa relate to long-term colonization with alternating types of Staphylococcus aureus. J Invest Dermatol. 2013;133:847–50.
Kubica M, GUzik K, Koziel J, Zarebski M, Richter W, Gajkowska B, et al. A potential new pathway for Staphylococcus aureus dissemination: the silent survival of S. aureus phagocytosed by human monocyte-derived macrophages. PLoS One. 2008;3:e1409.
Lawson TS, Connally RE, Iredell JR, Vemulpad S, Piper JA. Detection of staphylococcus aureus with a fluorescence In situ hybridization that does not require lysostaphin. J Clin Lab Anal. 2011;25:142–7.
Vogel TR, Dombrovskiy VY, Carson JL, Haser PB, Lowry SF, Graham AM. Infectious complications after elective vascular surgical procedures. J Vasc Surg. 2010;51:122–30.
Bensley RP, Hurks R, Huang Z, Pomposelli F, Hamdan A, Wyers M, et al. Ultrasound-guided percutaneous endovascular aneurysm repair success is predicted by access vessel diameter. J Vasc Surg. 2012;55:1554–61.
Vierhout BP, Reijnen MMPJ, Oskam J, Ott A, van den Dungen JJAM, Zeebregts CJ. Cyanoacrylate skin microsealant for preventing surgical site infection after vascular surgery: a discontinued randomized clinical trial. Surg Inf. 2014;15:425–30.
Voyich JM, Braughton KR, Sturdevant DE, Whitney AR, Said-Salim B, Porcella SF, et al. Insights into mechanisms used by Staphylococcus aureus to avoid destruction by human neutrophils. J Immunol. 2005;175:3907–19.
Acknowledgements
We thank Linda Kuntz for the initiation of the trial at the different locations and the thorough registration of all data in the first year of research. Bart Berger, thank you for the design of the website. Paulien van Twuyver, thank you for revising the manuscript as a native English speaker. None of the researchers received any funding whatsoever.
Declaration of interest
For this research, a grant was provided by a pharmaceutical industry (Abbott Vascular). These funds provided the salary for the independent database manager. The Principal and local investigators did not receive funding. The medical devices were purchased without a discount.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
BV designed the study, drafted the manuscript and is supervising the progression of the trial. BRS reviewed the manuscript and is supervising the inclusion and follow-up of subjects in the trial in the UMCG. AO participated in the design of the study, reviewed the manuscript, and reviewed the statistical analysis. JD participated in the design of the study, reviewed the manuscript, and carries out the bacterial typing and fluorescence microscopy. TK reviewed the manuscript and is supervising the inclusion and follow-up of subjects in the trial in the MCL. MP reviewed the manuscript and is supervising the inclusion and follow-up of subjects in the trial in the Isala hospital. JB supervised the design of the study and reviewed the manuscript. CZ participated in the design of the study, reviewed the manuscript and is supervising the overall inclusion of subjects. All authors approved of the revised manuscript and the final draft.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Vierhout, B.P., Saleem, B.R., Ott, A. et al. A comparison of Percutaneous femoral access in Endovascular Repair versus Open femoral access (PiERO): study protocol for a randomized controlled trial. Trials 16, 408 (2015). https://doi.org/10.1186/s13063-015-0911-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-015-0911-y