Abstract
Background
Cardiac arrest causes ischaemic brain injury. Arterial carbon dioxide tension (PaCO2) is a major determinant of cerebral blood flow. Thus, mild hypercapnia in the 24 h following cardiac arrest may increase cerebral blood flow and attenuate such injury. We describe the Carbon Control and Cardiac Arrest (CCC) trial.
Methods/Design
The CCC trial is a pilot multicentre feasibility, safety and biological efficacy randomized controlled trial recruiting adult cardiac arrest patients admitted to the intensive care unit after return of spontaneous circulation. At admission, using concealed allocation, participants are randomized to 24 h of either normocapnia (PaCO2 35 to 45 mmHg) or mild hypercapnia (PaCO2 50 to 55 mmHg). Key feasibility outcomes are recruitment rate and protocol compliance rate. The primary biological efficacy and biological safety measures are the between-groups difference in serum neuron-specific enolase and S100b protein levels at 24 h, 48 h and 72 h. Secondary outcome measure include adverse events, in-hospital mortality, and neurological assessment at 6 months.
Discussion
The trial commenced in December 2012 and, when completed, will provide clinical evidence as to whether targeting mild hypercapnia for 24 h following intensive care unit admission for cardiac arrest patients is feasible and safe and whether it results in decreased concentrations of neurological injury biomarkers compared with normocapnia. Trial results will also be used to determine whether a phase IIb study powered for survival at 90 days is feasible and justified.
Trial registration
Australian New Zealand Clinical Trials Registry ACTRN12612000690853.
Similar content being viewed by others
Background
Cardiac arrest results in the immediate cessation of blood flow, sudden unconsciousness and, without prompt return of spontaneous circulation, irreversible brain injury within minutes [1,2]. Blood flow following return of spontaneous circulation, while vital to survival, also heralds the onset of cerebral reperfusion injury [3]. For cardiac arrest survivors, acute neurological injury exerts a profound effect on immediate, short-term and long-term quality of life outcomes [4,5]. Recent level I evidence has shown that the application of therapeutic hypothermia does not afford the previously accepted benefits of neurological protection or reduction in mortality [6]. Despite best efforts, the mortality outcomes for resuscitated cardiac arrest patients admitted to the intensive care unit remain high [7] and, in Australia and New Zealand, over the past decade intensive care unit mortality has essentially remained unchanged at 46% in 2003 and 48% in 2012 [8]. Thus, identifying modifiable aspects of post-resuscitation care to provide cerebral protection remains of extreme importance.
Arterial carbon dioxide tension (PaCO2) may be a modifiable component of patient care that might deliver improved neurological outcomes. Mild hypercapnia increases cerebral perfusion [9,10] is known to have anticonvulsant properties [11,12] as well as anti-inflammatory and anti-oxidant effects [13]. However, optimal PaCO2 levels during the early post-resuscitation period are currently poorly defined. Nonetheless, retrospective cohort studies have identified hypocapnia, both before admittance to [13,14] and within the intensive care unit [15-19], as being independently associated with worse neurological and mortality outcomes in cardiac arrest patients. Recently, a retrospective observational study of 16,542 patients enrolled at 125 participating intensive care units in Australia and New Zealand between 2000 and 2011 [18] found that, while hypercapnic patients had a similar mortality rate to normocapnic patients, they had a greater likelihood of being discharged home. Such findings were independently confirmed in a study of 409 out-of-hospital cardiac arrest patients from 21 Finnish intensive care units between March 2010 and February 2011 [11], and supported by observations on cardiac arrest in children [20] and experimental studies [21,22].
Therefore, mild hypercapnia during the 24 hours after cardiac arrest might contribute to positive neurological outcomes. Moreover, given that resuscitated cardiac arrest patients admitted to the intensive care unit typically receive mechanical ventilation, it should be feasible to target specific PaCO2 levels. This article describes a protocol for a pilot feasibility, safety and biological efficacy multicentre randomized controlled trial of therapeutic hypercapnia after cardiac arrest: the Carbon Control after Cardiac Arrest (CCC) trial.
Methods/Design
The CCC trial is a prospective pilot, feasibility, safety and biological efficacy multicentre, randomized controlled trial.
Feasibility outcome measures include screened:recruited patient ratio, weekly recruitment rate, protocol adherence, time from cardiac arrest to first intensive care unit arterial blood gas analysis, separation in PaCO2 levels between groups, and ability to obtain Glasgow Outcome Scale (Extended) assessments at 6 months from the date of randomization for survivors. Safety outcome measures include adverse changes in serum concentrations of neuron-specific enolase and S100b protein (at 24 h, 48 h and 72 h), incidence and types of cardiac arrhythmia, adverse changes in acid-base values, oxygenation (mean arterial oxygen tension, fraction of inspired oxygen requirement, alveolar-arterial gradient, positive end expiratory pressure requirements) or in the findings of cardiac echocardiography or cerebral computed tomography during the first 24 h after admission to the intensive care unit, occurrence of cerebral edema or right ventricular failure, incidence of acute kidney injury as estimated using ‘risk, injury, failure, loss, end-stage’ renal disease (RIFLE) criteria, need for continuous renal replacement therapy, and liver failure.
The primary biological efficacy outcome measure is the difference in serum concentrations of neuron-specific enolase and S100b protein at 24 h, 48 h and 72 h after randomization between the hypercapnia and the control groups. Neuron-specific enolase (a cytoplasmic glycolytic enzyme) and S100b (a calcium binding protein) are biomarkers specific to the central nervous system [23,24]. Serum concentrations of neuron-specific enolase and S100b increase in both the cerebrospinal fluid and blood following a cardiac arrest. Both biomarkers are predictive of neurological outcome rather than survival outcome for resuscitated cardiac arrest patients [23,24]. Sustained elevated concentrations of neuron-specific enolase and S100b protein in the first 24 h to 72 h following cardiac arrest are associated with poor neurological outcome [24,25]. Secondary efficacy outcome measures include date, time and vital status at intensive care unit and hospital discharge and hospital discharge destination as clinical outcomes. A summary of the feasibility, safety and primary and secondary outcomes is provided in Table 1.
Study setting and participants
The intensive care units of four tertiary hospitals in Australia and New Zealand will participate in this trial. The CCC trial participants have to satisfy the protocol-defined inclusion and exclusion criteria.
Inclusion criteria
-
Resuscitated non-traumatic in-hospital or out-of-hospital cardiac arrest;
-
Receiving mechanical ventilation;
-
Admitted to intensive care unit.
Exclusion criteria
-
Spontaneous ventilation;
-
Death considered imminent;
-
Clinical or radiological suspicion of raised intracranial pressure or intracranial bleeding;
-
Pregnant;
-
Younger than 18 years;
-
Severe chronic airflow limitation;
-
Severe metabolic acidosis (pH < 7.1 and base excess < −6 mmol/l) uncorrected within the first 2 h of admission to intensive care unit;
-
Transferred from another healthcare facility;
-
Participation declined by the treating clinician.
Randomization, allocation concealment and interventions
Randomization to either group will be performed using sealed opaque envelopes with permuted blocks of random sizes (block sizes 2 to 6) in a 1:1 ratio. Clinicians will be directed to target normocapnia (PaCO2 35 to 45 mmHg) or mild hypercapnia (PaCO2 50 to 55 mmHg) for 24 h during mechanical ventilation for each participant from the time of randomization. At all four sites, ventilation management, to adjust PaCO2 levels, will be achieved using intensive care unit-performed arterial blood gas analysis data assessed after adjustment to 37°C (alpha-stat) and guided on a minute-by-minute basis by end-tidal CO2 levels. After the 24 h intervention period, the treating clinician will determine the target PaCO2 level for each participant as per usual care. All remaining patient care decisions will be at the treating clinicians’ discretion. Blood samples will be centrifuged and isolated serum will immediately be frozen to −80°C at each participating site. Stored serum samples will then be shipped to the coordinating hospital and sent for batch analysis at a central laboratory in Melbourne, Victoria.
Data collection and management
Trained research staff at each trial site will collect trial related data using a paper-based case report form. Information to be collected using the case report form is outlined in Table 2. Completed case report forms will be sent to the principal investigator at the Austin Hospital, and data will be collated and entered into a central trial database. The trial investigators at the Austin Hospital, Melbourne will develop and manage the trial database, coordinate sample shipment and batch analysis and will perform the data analysis.
Ethical issues and trial registration
The Austin Hospital Human Research Ethics Committee is the lead ethics committee (approval: HREC/13/Austin/166; previously H2012/04737) and has provided approval for the Australian sites. Jurisdictional ethics committee approval has been obtained from the Health and Disability Ethics Committees, Ministry of Health, NZ (12/NTA/54) for the New Zealand site. Because of the specific nature of the trial, and the need to apply the intervention in a timely fashion, the need for prior informed consent was waived by the human research ethics committee. At the earliest appropriate time, the participant or their legal surrogate were asked for delayed consent. The trial was prospectively registered with the Australian New Zealand Clinical Trials Registry (ACTRN12612000690853).
Statistical analysis
Trial profile
Flow of patients through the trial will be displayed in a Consolidated Standards of Reporting Trials (CONSORT) diagram. We will report the number of screened patients who met study inclusion criteria and the number of patients included in the study. We will report the reasons for exclusion of ineligible patients according to the predefined inclusion and exclusion criteria, as listed. In addition, we will report the number of patients enrolled into the trial and the number of participants from whom a full set of serum biomarker samples were obtained.
Statistical analysis procedures
The efficacy and safety of the intervention will be evaluated on an intention-to-treat analysis of all eligible participants randomized to the trial. A sample size of 50 participants with full serum biomarker samples (baseline, 24 h, 48 h and 72 h) was deemed sufficient to allow for a meaningful assessment of neurological biomarker difference between groups and for safety and feasibility outcomes. No imputation or assumptions will be made for missing data. Normally distributed continuous data will be reported as mean with standard deviation and compared using Student’s t test or analysis of variance (ANOVA). Non-normally distributed continuous data will be reported as median with interquartile range and compared using the Mann-Whitney U test or the Kruskal-Wallis one way ANOVA. Where sufficient symmetry exists, biomarker sample data for each participant for each time-point will be compared with repeated measures ANOVA; alternatively, non-parametric techniques will be employed. Categorical data will be reported as number and percentage and compared using chi-square or Fisher exact tests where indicated. Unless otherwise stated, a two-sided P value of 0.05 will be used to indicate statistical significance. We will also perform an adjusted analysis for key cardiac arrest or baseline characteristics or intensive care unit management imbalances. All analyses will be performed using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).
Tables and figures
Planned tables are:
-
Baseline characteristics, cardiac arrest characteristics and intensive care unit procedures for the trial participants overall and according to study group.
-
Primary and secondary outcome measures.
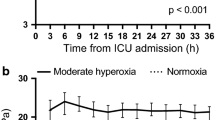
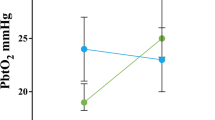
Planned figures are:
-
CONSORT-style diagram illustrating the flow of patients through the trial.
-
PaCO2 levels for normocapnia and mild hypercapnia group participants over the first 36 h following enrolment.
-
Serum neuron-specific enolase concentrations for normocapnia and mild hypercapnia group participants with a complete set of neurological injury biomarkers (baseline, 24 h, 48 h, and 72 h).
-
Serum S100b protein concentrations for normocapnia and mild hypercapnia group participants with a complete set of neurological injury biomarkers (baseline, 24 h, 48 h, and 72 h).
Data and safety monitoring
No data monitoring committee was established for this investigator-initiated clinical trial. The principal investigator at each site will review safety data for the duration of the trial. All adverse events and serious adverse events linked with the study intervention will be reported to the Austin Health Human Research Ethics Committee within 24 h of study staff becoming aware of the event and in accordance with institutional and jurisdictional human research ethics committee requirements.
Funding and support
The CCC trial is supported by the Australian and New Zealand Intensive Care Society Clinical Trials Group. Funding support has been received from the Anaesthesia Intensive Care Trust Fund (Austin Hospital, Melbourne), Intensive Care Foundation, Ambulance Victoria and the Austin Medical Research Foundation. Funding bodies have no input into the design, management or reporting of the trial.
Discussion
The study commenced recruitment on 6 December 2012 at the Austin Hospital, Melbourne, Australia as single-centre trial. In October, 2013 the additional three participating sites joined the CCC trial, following the receipt of streamlined ethical approval, making this a multicentre trial. It is estimated that participant recruitment will be completed by November 2014 and final 6-month neurological assessment completed in May, 2015.
The results of the CCC trial will provide preliminary clinical evidence regarding the feasibility and safety of targeting mild hypercapnia for 24 h following intensive care unit admission for cardiac arrest patients. It will also provide preliminary information on whether such treatment leads to lower levels of neurological injury biomarkers concentrations, compared with normocapnia. Such trial results will be used to determine whether a phase IIb study is feasible, safe and justified.
Trial status
Recruitment is active.
Abbreviations
- ANOVA:
-
analysis of variance
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- CCC:
-
Carbon Control and Cardiac Arrest
- CONSORT:
-
Consolidated Standards of Reporting Trials
- PaCO2:
-
arterial carbon dioxide tension
- RIFLE criteria:
-
‘risk, injury, failure, loss, end-stage’
References
Wiklund LM, Miclescu A, Semenas E, Rubertsson S, Sharma HS. Central nervous tissue damage after hypoxia and reperfusion in conjunction with cardiac arrest and cardiopulmonary resuscitation: mechanisms of action and possibilities for mitigation. Int Rev Neurobiol. 2012;102:173–87.
Eastwood GM, Young PJ, Bellomo R. The impact of oxygen and carbon dioxide management on outcome after cardiac arrest. Curr Opin Crit Care. 2014;20:266–72.
Neumar RW, Nolan JP, Adrie C, Aibiki M, Berg RA, Böttiger BW, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication: a consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anaesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care, the Council on Clinical Cardiology; and the Stroke Council. Circulation. 2008;118:2452–83.
Lemiale V, Dumas F, Mongardon N, Giovanetti O, Charpentier J, Chiche JD, et al. Intensive care unit mortality after cardiac arrest: the relative contribution of shock and brain injury in a large cohort. Intensive Care Med. 2013;39:1972–80.
Polanowska KE, Sarzyńska-Długosz IM, Paprot AE, Sikorska S, Seniów JB, Karpiński G, et al. Neuropsychological and neurological sequelae of out-of-hospital cardiac arrest and estimated need for neurorehabilitation: a prospective pilot study. Kardiol Pol. 2014;72:814–22.
Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C, et al. Targeted temperature management at 33°C versus 36°C after cardiac arrest. N Engl J Med. 2013;369:2197–206.
Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–31.
Eastwood GM, Bailey M, Bellomo R. Letter in response to the editorial on the Targeted Temperature Management after Cardiac Arrest trial. N Eng J Med. 2014;370:1356–61.
Curley G, Laffey JG, Kavanagh BP. Bench-to-bedside review: carbon dioxide. Crit Care. 2010;14:220.
Yokoyama I, Inoue Y, Kinoshita T, Itoh H, Kanno I, Iida H. Heart and brain circulation and CO2 in healthy men. Acta Physiol. 2008;193:303–8.
Pollock GH, Stein SN, Gyarfus K. Central inhibitory effects of carbon dioxide: man. Proc Soc Exp Biol Med. 1949;70:291.
Tolner EA, Hochman DW, Hassinen P, Otáhal J, Gaily E, Haglund MM, et al. Five percent CO2 is a potent, fast-acting inhalation anticonvulsant. Epilepsia. 2011;52:104–14.
Shoja MM, Tubbs RS, Shokouhi G, Loukas M, Ghabili K, Ansarin K. The potential role of carbon dioxide in the neuroimmunoendocrine changes following cerebral ischemia. Life Sci. 2008;83:381–7.
Aufderheide TP, Lurie KG. Death by hyperventilation: a common and life-threatening problem during cardiopulmonary resuscitation. Crit Care Med. 2004;32:S345–51.
Touma O, Davies M. The prognostic value of end tidal carbon dioxide during cardiac arrest: a systematic review. Resuscitation. 2013;84:1470–9.
Roberts BW, Kilgannon JH, Chansky ME, Mittal N, Wooden J, Trzeciak S. Association between postresuscitation partial pressure of arterial carbon dioxide and neurological outcome in patients with post-cardiac arrest syndrome. Circulation. 2013;127:2107–13.
Pynnonen L, Falkenback P, Kamarainen A, Lonnrot K, Yli-Hankala A, Tenhunen J. Therapeutic hypothermia after cardiac arrest - cerebral perfusion and metabolism during upper and lower threshold normocapnia. Resuscitation. 2011;82:1174–9.
Schneider AG, Eastwood GM, Bellomo R, Bailey M, Lipcsey M, Pilcher D, et al. Arterial carbon dioxide tension and outcome in patients admitted to the intensive care unit after cardiac arrest. Resuscitation. 2013;84:927–34.
Vaahersalo J, Bendel S, Reinikainen M, Kurola J, Tiainen M, Raj R, et al. Arterial blood gas tensions after resuscitation from out-of-hospital cardiac arrest: associations with long-term neurological outcome. Crit Care Med. 2014;42:1463–70.
Del Castillo J, López-Herce J, Matamoros M, Cañadas S, Rodriguez-Calvo A, Cechetti C, et al. Hyperoxia, hypocapnia and hypercapnia as outcome factors after cardiac arrest in children. Resuscitation. 2012;83:1456–61.
Falkenbach P, Kämäräinen A, Mäkelä A, Kurola J, Varpula T, Ala-Kokko T, et al. Incidence of iatrogenic dyscarbia during mild therapeutic hypothermia after successful resuscitation from out-of-hospital cardiac arrest. Resuscitation. 2009;80:990–3.
Vannucci RC, Towfighi J, Heitjan DF, Brucklacher RM. Carbon dioxide protects the perinatal brain from hypoxic-ischemic damage: an experimental study in the immature rat. Pediatrics. 1995;95:868–74.
Shinozaki K, Oda S, Sadahiro T, Nakamura M, Hirayama Y, Abe R, et al. S-100B and neuron-specific enolase as predictors of neurological outcome in patients after cardiac arrest and return of spontaneous circulation: a systematic review. Crit Care. 2009;13:R121.
Calderon LM, Guyette FZ, Ankur AD, Callaway CW, Rittenberger JC, Service PCA. Combining NSE and S100B with clinical examination findings to predict survival after resuscitation from cardiac arrest. Resuscitation. 2014;85:1025–9.
Shinozaki K, Oda S, Sadahiro T, Nakamura M, Abe R, Nakada TA, et al. Serum S-100B is superior to neuron-specific enolase as an early prognostic biomarker for neurological outcome following cardiopulmonary resuscitation. Resuscitation. 2009;80:870–5.
Acknowledgements
Thanks to the site principal investigators: Associate Professor Nerina Harley (Royal Melbourne Hospital, Australia), Dr Shay McGuiness (Auckland City Hospital, New Zealand) and Dr Gopal Taori (Monash Medical Centre, Australia); research coordinators: Ms Leah Peck, Ms Helen Young (Austin Hospital, Australia), Ms Deborah Barge, Ms Andrea Jordan (Royal Melbourne Hospital, Australia), Ms Pauline Galt, Ms Tammy Lamac (Monash Medical Centre, Australia); and clinical staff who facilitated the conduct of this study. We acknowledge the following funding bodies: Anaesthesia Intensive Care Trust Fund (Austin Hospital, Melbourne); the Australia and New Zealand Intensive Care Foundation; Ambulance Victoria; and the Austin Medical Research Foundation.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Competing interests
All authors state that they have no competing interests to declare.
Authors’ contributions
GME conceived the study, contributed to the study design, obtained grant funding and was responsible for preparing the manuscript. RB conceived the study, contributed to the study design, obtained grant function and is the principal investigator. AGS conceived the study, contributed to the study design, obtained grant funding and revised the manuscript. SS contributed to the study design and revised the manuscript. MB contributed to the study, provided statistical input and revised the manuscript. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Eastwood, G.M., Schneider, A.G., Suzuki, S. et al. A pilot feasibility, safety and biological efficacy multicentre trial of therapeutic hypercapnia after cardiac arrest: study protocol for a randomized controlled trial. Trials 16, 135 (2015). https://doi.org/10.1186/s13063-015-0676-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-015-0676-3