Abstract
Background
Historically, the molecular classification of colorectal cancer (CRC) was based on the global genomic status, which identified microsatellite instability in mismatch repair (MMR) deficient CRC, and chromosomal instability in MMR proficient CRC. With the introduction of immune checkpoint inhibitors, the microsatellite and chromosomal instability classification regained momentum as the microsatellite instability condition predicted sensitivity to immune checkpoint inhibitors, possibly due to both high tumor mutation burden (TMB) and high levels of infiltrating lymphocytes. Conversely, proficient MMR CRC are mostly resistant to immunotherapy. To better understand the relationship between the microsatellite and chromosomal instability classification, and eventually discover additional CRC subgroups relevant for therapeutic decisions, we developed a computational pipeline that include molecular integrative analysis of genomic, epigenomic and transcriptomic data.
Results
The first step of the pipeline was based on unsupervised hierarchical clustering analysis of copy number variations (CNVs) versus hypermutation status that identified a first CRC cluster with few CNVs enriched in Hypermutated and microsatellite instability samples, a second CRC cluster with a high number of CNVs mostly including non-HM and microsatellite stable samples, and a third cluster (7.8% of the entire dataset) with low CNVs and low TMB, which shared clinical-pathological features with Hypermutated CRCs and thus defined Hypermutated-like CRCs. The mutational features, DNA methylation profile and base substitution fingerprints of these tumors revealed that Hypermutated-like patients are molecularly distinct from Hypermutated and non-Hypermutated tumors and are likely to develop and progress through different genetic events. Transcriptomic analysis highlighted further differences amongst the three groups and revealed an inflamed tumor microenvironment and modulation Immune Checkpoint Genes in Hypermutated-like CRCs.
Conclusion
Therefore, our work highlights Hypermutated-like tumors as a distinct and previously unidentified CRC subgroup possibly responsive to immune checkpoint inhibitors. If further validated, these findings can lead to expanding the fraction of patients eligible to immunotherapy.
Similar content being viewed by others
Introduction
Colorectal Cancer (CRC) is a major cause of cancer-related death worldwide, accounting for approximately 8% of all annually diagnosed cancers [1]. Historically, the molecular classification of CRC was based on the global genomic status, which identified three major groups: tumors with microsatellite instability (MSI; ~ 15% of all CRCs), tumors with chromosomal instability (CIN; ~ 85% of all CRCs) and tumors with a CpG island methylator phenotype (CIMP; ~ 20% of all CRCs) [2].
In MSI tumors, defects of the mismatch repair (MMR) pathway are the leading cause of genetic instability. It can be due to inactivating mutations or to epigenetic silencing by promoter hypermethylation of DNA MMR genes [2], a condition frequently associated to high levels of CpG island methylation and referred to as CIMP-High (CIMP-H, ~ 70–85% of MSI CRCs). Defective DNA MMR (dMMR) leads to reduced restoration of replication errors resulting in the introduction of a high rate of mismatches in microsatellites. The consequent changes in microsatellite lengths may be monitored to classify different phenotypes as microsatellite stable (MSS) or unstable (MSI), which can be further subdivided MSI-High (MSI-H) or MSI-Low (MSI-L) [2, 3]. Tumors with MSI-H typically display a high rate of point mutations [4, 5], a state referred to as hypermutation (HM). Besides dMMR, the HM phenotype is also related to somatic or germline mutations of POLE and POLD1 genes encoding DNA polymerase epsilon and delta, respectively [3].
CIN tumors instead bear high frequency of copy number variations (CNVs). In almost all cases they are MSS or MSI-L, usually share low mutation rate, and null or low level of CIMP (non-CIMP or CIMP-L) [2, 6].
Over the years, additional molecular classifications beyond CIN, MSI and CIMP have been proposed with the aim to dissect the heterogeneity of CRC for prognostic and predictive intents [7,8,9,10,11]. In example, the Consensus Molecular Subtypes (CMS) Consortium, analyzing CRC expression profiling data from multiple studies, converged on the definition of four main CMSs [10]. Although CMSs have prognostic and therapeutic implications, they have not been translated into clinical routine, yet.
With the introduction of immune checkpoint inhibitors (ICIs) for the treatment of metastatic CRC (mCRC), MSI/CIN classification regained momentum as the dMMR/MSI-H condition (~ 2–4% of mCRCs) predicted sensitivity to ICIs in clinical trials, possibly due to both high rate of tumor mutational burden (TMB-H) and high levels of infiltrating lymphocytes typically present in these tumors [3, 12, 13]. Conversely, pMMR-MSS/MSI-L a group, as a whole appears resistant to ICIs therapies.
To better understand the differences between MSI/CIN status and eventually discover additional CRC subgroups relevant for therapeutic decisions, we developed a computational pipeline that include molecular integrative analysis of genomic, epigenomic and transcriptomic data of 520 CRC samples downloaded from The Cancer Genome Atlas (TCGA) data portal. The results highlighted a novel non-CIN, non-MSI and CIMP-L CRC subgroup, characterized by KRAS-high/TP53-low mutation rate, distinct mutational signatures and an inflamed tumor microenvironment.
Materials and methods
Data collection and processing
We downloaded genomic, transcriptomic and epigenomic data from TCGA-COAD and READ projects stored on TCGA data portal (https://portal.gdc.cancer.gov/), accessed in November 2020. We performed meta-analysis on 520 TCGA-COAD and READ patients of which copy number variations (CNVs), whole exome sequencing (WES), transcriptomic (RNA-seq), DNA methylation and MSI status data were available.
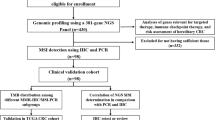
We developed a computational pipeline that includes molecular integrative analysis at genomic, epigenomic and transcriptomic level to better classify patients affected by CRC. The pipeline is subdivided in steps, described in Fig. 1.
Step1: molecular-based CRC subgroups stratification
Tumor mutational burden (TMB) Analysis
Tumor mutational burden (TMB) was calculated dividing the total number of nonsynonymous mutations of every patient per 30 Megabase, which is the average size of the exome. Numbers of nonsynonymous mutations are derived from MAF files retrieved from TCGA resulting from variant analysis of WES experiments on 520 TCGA-COAD and READ patients. According to [5] patients with a TMB higher and lower than 20 per Megabase were classified as HM or non-HM, respectively.
CNV calling and analysis
We performed CNVs calling from segmented mean data employing GISTIC 2.0 which identifies genomic regions that are significantly gained or lost across the 520 TCGA-COAD and READ tumors [14]. For details on how GISTIC calculates focal and broad amplification/deletion in chromosome regions and how the algorithm was set to our data, refer to Additional file 1. The R package copynumber [15] was used to visualize the frequency of gain/loss in the chromosome regions among the CRC’s subgroups identified. The association between frequency of CNVs events in the chromosome regions and the CRC’s subgroups identified was evaluated using Fisher’s exact test.
Step 2: molecular characterization of the subgroups identified
Mutational data analysis
The R package maftools [16], which contains functions to perform most used analyses in cancer genomics and to create feature rich customizable visualizations, have been used to analyze MAF files of the 520 TCGA-COAD and READ tumors and to address the mutational signatures. We studied top frequently mutated genes discovered in our cohort plus recurrently mutated genes defined in the COSMIC database [17]. The association between different mutational rates in the genes analyzed and HM, HM-like and non-HM groups was evaluated using Fisher’s exact test. Further, we performed the analysis of the non-silent mutations existing in POLE exonuclease domain from exon 9–14 in the three subgroups.
Other algorithms implemented in the maftools package allowed the extraction of mutational signatures from MAF files and to compare them with the validated signature present in the COSMIC curated database. For details on the evaluation of mutational signatures, refer to Additional file 1.
DNA methylation analysis
Data containing β-values from the Illumina Infinium HumanMethylation450 Array were available for 382/520 of the patients enrolled in the study. In pre-processing steps, we filtered out probes containing Single Nucleotide Polymorphisms (SNPs) and designed on X and Y chromosomes. To determine CpG Island Methylator Phenotype (CIMP) status, we first identified the 1000 differentially methylated CpGs between the three groups (ANOVA-like test using limma package) [18]. Afterwards, we computed an unsupervised hierarchical clustering that identified 3 clusters and considered the methylome patterns of the clusters we could assign to cluster 1 to CIMP-Low (CIMP-L), cluster 2 to CIMP-High (CIMP-H) and cluster 3 to non-CIMP (Fig. 3). The hierarchical clustering analysis was performed by using “maximum” as clustering distance and “ward.D2” as clustering method.
Step 3: tumor microenvironment inflammation assessment
Weighted gene co-expression network analysis (WGCNA) of the transcriptomic data of 520 TCGA-COAD and TCGA-READ tumors was leveraged by using the R package WGCNA [19, 20]. For details on how the WGCNA algorithm was implemented, refer to Additional file 1.
RNA-seq data of the 520 TCGA-COAD and TCGA-READ patients was leveraged to evaluate the quality and quantity of immune infiltrate in the tumoral environment. Analysis was conducted using ImSig, which is a R library that provides functions to study the expression and abundance of immune cells in cancer tissue transcriptomics [21]. This approach incorporates immune/inflammatory cells in 7 major classes (B cells, Interferon, Macrophages, Monocytes, Neutrophils, NK cells, T cells) plus 3 additional signatures (Plasma cells, Proliferation and Translation). A correlation cut-off of 0.8 was used, to remove genes that did not exhibit a strong correlation with the ImSig signatures. Furthermore, to assess the statistical significance of the difference of the mean expression of each immune signature in the multiple comparison of the three groups the Tuckey’s test was used, which is a post-hoc test after ANOVA analysis.
In addition, we studied the expression of 79 Immune Checkpoint Genes (ICGs) curated by [22], in our cohort. A differentially expression analysis was performed using the multiple comparison of the three subgroups using Wald test (Additional file 4: Table S6) and p-value was adjusted according to the Benjamini–Hochberg method. Thresholds for FDR < 0.1 and Log2 Fold Change > 0.4 were used to select significant differentially expressed genes.
Results
Classification of the CRC samples according to TMB and CNVs
We subjected 520 CRC tumor samples of COAD/READ projects to TMB analysis. 78/520 (15%) samples were classified as hypermutated (HM: TMB > 20 per 106 bases) with a median value of 44.9 mutations per 106 bases (range: 26–347 per 106 bases), while 442/520 (85%) samples were classified as non-HM with a median value of 3.5 mutations per 106 bases (range: 0.1–24 per 106 bases).
The CNV calling analysis resulted in 29 amplified and 41 deleted focal regions significantly altered through all sets of tumor samples. We then subjected the 520 tumor samples to an unsupervised hierarchical clustering analysis of the CNVs which identified two main clusters (Fig. 2): Cluster A (ClA) characterized by few CNV events and Cluster B (ClB) with a high number of CNVs events. ClA was enriched in HM samples (n = 76/117; 65%; Fig. 2, yellow bars), while ClB mostly contained non-HM samples (n = 401/403; 99.5%; Fig. 2, blue bars). Within ClA, we noted a group of 41 samples with low CNV profile and very low TMB (median value of 3.9 mutations per 106 bases, range: 0.1–23 mutations per 106 bases). Based on their clinical-pathological similarities with HM CRCs (as described below) this subset will be referred to as HM-like (Fig. 2) and accounted for 7.8% of the entire dataset.
Unsupervised hierarchical clustering analysis based on CNVs data of the 520 CRC patients selected from TCGA-COAD and READ projects. The lines in the heatmap represent significant focal alteration. The columns correspond to the 520 patients. HM and non-HM samples are indicated in yellow and blue colors, respectively. This analysis identified two main clusters: cluster a (ClA) and cluster b (ClB). ClA (117/520; 22.5%) is characterized by a few events of CNVs along the chromosome regions and was enriched in HM samples (n = 76/117; 63.9%). ClB contains samples with a high number of CNVs events and it mostly consists of non-HM samples (n = 401/403; 99%). Among ClA, we identified a sub-group of tumors (called HM-like; n = 41/520; 7.8%) with a similar CNV profile of ClA, also characterized by a low TMB. To the right-hand side of the figure, a scale indicates the color code relative to the log2 segment mean value of CNVs (ranging from − 1 up to 3)
The profiles of CNVs amount and distribution among chromosomes was clearly distinct between the three subgroups. Overall, the HM-like group was characterized by a CNV profile more similar to the HM group than to the non-HM group (Fig. 3). However, these tumors also showed recurrence of gains (chromosomes 7, 9p and 19q) and losses (chromosome 8p, 10, 11, 15q, 17p and 18) more typical of non-HM samples (Fig. 3, Additional file 1: Tables S1, S2).
As expected, most HM tumors were classified as MSI-H (n = 61/78; 78.2%), while non-HM and HM-like patients were much more frequently MSS stable (n = 377/401; 94.0% and n = 34/41; 82.9%, respectively; Table 1). Consistent with the results of population studies [23], POLE exonuclease domain mutation rate was 2.9% (15/520) in our cohort, and all mutations fell in HM-group (15/78; 19.2%), while non-HM and HM-like patients showed no POLE alteration (Table 1).
Overall, this analysis suggests that non-HM and HM subsets largely comprise CRCs associated with typical CIN and MSI/hypermutated phenotypes, respectively, while HM-like tumors appear as a distinct entity, with rather low CNVs and mutation rates.
Clinical-pathological features and gene mutation rates in HM, HM-like and non-HM samples
Clinical-pathological features of HM, HM-like and non-HM samples are reported in Table 1. No significant associations were found with age or gender. As expected, HM patients were significantly enriched in early stages and in ascending colon localization compared to non-HM patients, which were more associated with stage 4 and in descending colon localization [11, 24]. Intriguingly, HM-like patients shared with HM subset a similar enrichment in early stages, with only 2.4% (1/41) and 3.8% (3/78) of the patients with HM-like and HM profiles in stage 4, against a rate of 18.0% (72/401) for non-HM patients (P < 0.0001, Fisher’s exact test). Moreover, HM-like tumors were more frequently associated with ascending colon location (21/41; 51.2%) similar to HM (50/78; 64.1%), in contrast to non-HM tumors which were associated with descending colon location (253/401; 63.1%) (P < 0.0001, Fisher’s exact test).
To further compare the overall molecular features of HM-like versus HM and non-HM subsets we examined SNV data. As expected from the literature and according to their CIN profile [25] non-HM tumors had higher mutation rate in APC (84%), TP53 (69%) and KRAS (41%) compared to HM tumors (Table 2). In contrast, HM tumors had high mutation rates in genes of the WNT signaling, TGF-β, PI3K-AKT and MAPK/ERK pathways as well as in ATM, KMT2D and LRP1D [26]. Interestingly, HM-like tumors had the highest frequency in KRAS (59%) and SOX9 (27%) gene mutations compared to the other groups. Also, they showed the lowest TP53 mutation rate (15%) and a rate of APC mutations similar to HM samples and significantly lower than non-HM samples (Table 2).
The pattern of mutational targets and rates support the hypothesis that HM-like tumors may represent a distinct subgroup of CRCs, which may develop and progress through a different sequence of genetic events compared to the well-known MSI/hypermutated and MSS/CIN subsets, while sharing prevalence of early stages and ascending colon localization with the HM subset.
Fingerprints of base substitutions in HM, HM-like and non-HM groups reveals unique mutational signature for each group
To further question whether HM-like CRCs are distinct from MSI/hypermutated and MSS/CIN subsets, we searched for the emergence of specific mutational signatures in the three subgroups. Indeed, different mutational processes generate unique combinations of base changes, termed “Mutational Signatures” which can be used as a readout of the biological history of a cancer [27]. To define the mutational signatures associated with HM, HM-like and non-HM groups we performed a classification of base substitutions to include the 3′ and 5′ flanking bases at the mutated site [16]. Thus, we extracted 3 mutational signatures from each group and compared them to COSMIC Single Base Substitution (SBS) Signatures database, a catalog of known mutational signatures identified from > 12,000 samples derived from 40 types of human cancer in which additional information for each signature were also provided.
The top three signatures extracted from the HM group were the most similar to COSMIC SBS6, SBS10b and SBS44 signatures (Table 3) and that is consistent with the “hypermutated” phenotype defining the HM group, since SBS10b signature is associated with POLE mutations, which outbreaks in a high mutational rate, and COSMIC SBS6 and SBS44 are typically associated with dMMR.
The three signatures extracted from non-HM samples had the highest similarity with COSMIC SBS1, SBS6 and SBS40 signatures (Table 3). SBS1, which was also noted in the other subgroups, is related to the spontaneous or enzymatic deamination of 5-methylcytosine to thymine and is widespread in many tumors. SBS40 signature is not clearly associated with a specific etiology, but like SBS1 it is widespread in most cancers and shows some relationships with the age of patients [28].
The three signatures extracted from HM-like samples showed high similarities with SBS1, SBS6 and SBS30. In particular, similarity to SBS30 represents a feature unique to HM-like samples (Table 3). This signature has been recently associated with deficiency in the base excision repair and in particular with inactivation of the NTHL1 gene [29]. Despite some similarities in the mutational signatures were shared by two or even all three subgroups (i.e. SBS1, SBS6 and SBS15), this analysis further evidenced distinct mutational profiles between the HM, HM-like and non-HM subgroups.
Different CpG methylation patterns occur in the three CRC subgroups
Next, we performed an unsupervised hierarchical clustering analysis for 382 of the TCGA-COAD/READ samples for which CpGs methylation data were available. The hierarchical clustering dendrogram defined three distinct tumor groups: CIMP-H (n = 57/382; 14.9%) with a high rate of CpGs probes methylated; CIMP-L (n = 107/382; 28.0%) with low rate of CpGs probes methylated and non-CIMP (n = 218/382; 57.1%) characterized by the absence of CpGs methylated probes (Fig. 4 and Additional file 1: Fig. S1). As expected, most of the HM patients belong to the CIMP-H cluster (41/57; 71.9%) and most non-HM tumors belong to the non-CIMP cluster (214/294; 72.8%), while a small number of HM and non-HM tumors clustered in the CIMP-L group. Interestingly, we revealed that the HM-like samples are mainly associated with CIMP-L phenotype (24/31; 77.4%) (Fig. 4; Additional file 1: Fig. S2). These results highlighted a different methylome pattern of HM-like tumors compared HM and non-HM.
Unsupervised hierarchical clustering analysis based on CpGs methylation data of the 382 patients selected from TCGA-COAD and READ projects. The lines on the heatmap represent the 1000 most differentially methylated CpGs probes between HM, HM-like and non-HM groups. The columns correspond to the 382 patients. Inside the cells of the heatmap are reported the β-values which represent the methylation rate of the probes. The HM patients are reported in yellow; the HM-like patients in red while the non-HM patients in blue. The hierarchical clustering dendrogram supported three distinct tumour groups: CIMP-H (n = 57) defined by an high rate of CpGs probes methylated; CIMP-L (n = 107) with low rate of CpGs probes methylated and non-CIMP (n = 218) characterized by the absence of CpGs probes methylated
WGCNA analysis supports HM, HM-like and non-HM tumors as three distinct CRC subgroups
We performed the WGCNA network-based methodology on the transcriptomic data of 520 TCGA-COAD/READ patients. This analysis revealed 12 highly correlated modules within the gene correlation network, which encompassed genes that were more correlated among each other than with other nodes in the network. For each module, through the WGCNA analysis, we computed the module eigengene defined as the first principal component of that module. By considering as external clinical traits the HM, HM-like, and non-HM status, we then computed the Pearson correlation coefficient between the module eigengene of each module and these external traits (Fig. 5a). We found (1) three modules with statistically significant positive correlations with the HM status, meaning that genes belonging to these three modules were highly expressed in HM patients; (2) two modules with statistically significant positive correlations with the HM-like status, whose genes were highly expressed in HM-like patients; (3) one module with a statistically significant positive correlation with the non-HM status, whose genes were highly expressed in non-HM patients. All these modules did not overlap among the patient status (i.e., HM, HM-like, non-HM), suggesting that these three classes of CRC patients are different also with respect to the gene expression data. In order to identify specific gene signatures of the three subgroups, for each gene we computed the module membership (MM) as the correlation between its gene expression profile and the module eigengene and sorted genes within their own modules according to the MM (Additional file 2: Table S3). Yet, we considered as representative genes of a given module the ones whose MM is greater than 0.7.
WGCNA analysis. a Heatmap of module-trait associations. In the heatmap, each row corresponds to a module eigengene and each column to a trait. Each cell contains the corresponding correlation and P value. The table is color-coded by correlation according to the color legend. The traits along the columns have been numerically encoded as follows: HM status (no = 1, yes = 2); HM like status (no = 1, yes = 2); non-HM status (no = 1, yes = 2). The colour labels of modules with at least one statistically significant correlation were highlighted. b, c KEGG pathways. Results of KEGG pathways enrichment analysis for the most representative genes (module membership > 0.9) falling within the modules statistically significant correlated with the HM status (b), HM like status (c), and non-HM status (d). The names of genes annotated for the enriched KEGG pathways were reported
Then, for each patient status, we grouped together the representative genes of the modules with the highest correlation and performed a functional enrichment analysis. Via this process, we associated putative biomarkers and functional pathways to each status (i.e., HM, HM-like, non-HM). Also, this analysis confirmed relevant differences among the three subgroups. In detail, the HM status was characterized by high expression of genes mainly involved in the inflammatory bowel disease, Toll-like receptor signaling pathway, PI3K-Akt signaling pathway and JAK-STAT signaling pathways (Fig. 5b, Additional file 3: Table S4). The HM-like status was characterized by high expression of genes mainly involved in estrogen signaling and pathways related to the immune/inflammatory response (Fig. 5c, Additional file 3: Table S4). The non-HM status was characterized by high expression of genes mainly involved in RNA processing, DNA repair and VEGF signaling pathway (Fig. 5d, Additional file 3: Table S4).
Rate of immune infiltrate in tumoral microenvironment of the three CRC subgroups
dMMR CRC, largely clustering in the HM subgroups, are typically associated with immune infiltration and good response to ICB therapy [3]. WCGNA analysis indicated activation of inflammatory/immune response genes in HM and HM-like tumors. Therefore, we set out to determine the rate of immune/inflammatory infiltration more specifically in the three subsets by a computational analysis of tumor transcriptomic data, using the R package ImSig [21]. By this mean, 10 signatures describing the relative abundance and statistical analysis of 7 inflammatory/immune cells plus 3 additional signatures were analyzed. Concerning T and NK lymphocytes, as expected, we observed the highest signature representation in the HM group, while non-HM have a significantly lower degree of immune cell infiltration (P < 0.01) (Fig. 6 and Additional file 1: Fig. S3). Interestingly, HM-like tumors showed T and NK cell signatures similar to HM samples and significantly different than non-HM group (P < 0.01). On the other side, HM-like tumors had proliferation, macrophage and interferon signatures more similar to non-HM than HM tumors. However, some genes belonging to interferon signatures and involved in inflammatory/immune responses shared a similar expression between HM-like and HM tumors, while being different from non-HM tumors (Additional file 1: Table S5).
Results of immune signatures analysis performed by ImSig. The boxplots (A and B) show the gene expression of T and NK signature genes (estimated relative abundance) across the HM, non-HM and HM-like groups. Statistical analysis of data was performed using analysis of variance (ANOVA) followed by multiple comparison Tukey’s test. **P < .01, *P < .05
Next, we performed a differential expression analysis of the 79 ICGs described by [22] expressed in the series (Additional file 4: Table S6). The comparison between HM and non-HM samples revealed that 46 ICGs were differentially expressed and as expected, most of these (29/46; 63.0%) were more expressed in HM group than non-HM. These included KIR and HLA genes, possibly suggestive of NK and antigen presenting cells infiltration, as well as multiple genes directly involved in immune checkpoint regulation, including the well-known PD-L1, PD1, CTLA4, LAG3, TIM3 and TIGIT (Additional file 4: Table S6 and Fig. 7). Interestingly, 17 genes were significantly less expressed in HM compared to non-HM samples (Additional file 4: Table S6). HM-like tumors profoundly differed from HM and non-HM samples. They showed 13 ICGs significantly more expressed compared to non-HM tumors. KIR genes, TIGIT, PD1 and CTLA4 show a similar trend compared to HM samples. Differences in the expression of HLA genes did not reach statistical significance, while CD96 appears even more differentially expressed in this subgroup than in HM tumors, comparing with non-HM subset. Remarkably, we noticed that 4 genes whose role in immune checkpoint regulation is emerging (VTCN1, BTNL9, BTLA and CD28) are specifically more expressed in HM-like group compared to non-HM samples (Additional file 4: Table S6 and Fig. 7). Also, in this comparison we found repressed genes (i.e. SIRPA, BTN2A1 and PVR), some of which followed the same trend of HM tumors, while others where rather specific for this subset (i.e. CD70, CD40). Conversely, IDO1, TDO2 and CD40LG expression trend was completely opposite in HM versus HM-like subgroups.
Example of ICGs differentially expressed in HM, non-HM and HM-like groups. The Box Plots show A ICGs more expressed in HM group versus non-HM, which may (KIR genes) or may not (HLA genes) be significantly more expressed in HM-like vs non-HM tumors; B gene sharing a similar trend of expression between HM and HM-like; C gene specifically more expressed in HM-like group (VTCN1 and BTNL9) or with an opposite trend of expression in HM versus HM-like (CD40LG). The analysis was performed using the multiple comparison of the three subgroups using Wald test and P value was adjusted according to the Benjamini–Hochberg method. Thresholds for FDR < 0.1 and Log2 Fold Change > 0.4 were used to select significant differentially expressed genes
Discussion
The comprehension of the biological processes underlying cancer evolution and the molecular stratification of tumors is extremely relevant for prognostic and therapeutic purposes. To this end, the broad inter/intra-tumor molecular heterogeneity of CRC has been widely explored by NGS-based genomic and transcriptomic profiling. Reflecting the different biology of CRCs and their major molecular differences, several molecular classifications with prognostic and predictive value have been proposed [7,8,9,10,11].
One major distinction remains between CIN, MSI and CIMP-H CRCs, with CIN and MSI being mostly mutually exclusive, while CIMP-H largely but incompletely overlaps with MSI CRCs. Despite extensive investigations, this classification remained of poor clinical value until the introduction of ICIs therapies for the treatment of mCRC. In this frame, MSI/CIN classification gained clinical relevance since dMMR/MSI-H CRCs are often responsive to ICIs, probably due to both high TMB (hypermutation status) and high levels of TILs, which are typical hallmarks of these tumors [12, 13]. Indeed, the high mutation load of these tumors might lead to generation of a high number of immunogenic neoantigens [23], which in turn could facilitate immune responses against cancer cells. Conversely, CIN CRCs usually bear low TMB and are mostly resistant to ICIs.
By performing hierarchical clustering analysis of CNVs versus hypermutation status exploiting TCGA CRC datasets, we identified a third cluster of CRCs (7.8%) characterized by low CNVs and low TMB, distinct from the HM and non-HM subsets, which largely match the MSI and CIN groups, respectively. Since this new cluster shares clinical-pathological features with HM CRCs, it was named HM-like subset.
Interestingly, HM-like tumors also showed a distinct mutational profile compared with HM and non-HM tumors, for which we highlighted profiles essentially in line with the literature [11, 30]. In example, the rate of APC mutations in HM-like tumors was similar to HM samples and significantly lower than non-HM samples, while mutations in alternative targets of the WNT and TGF-beta pathways were much lower than those occurring in HM samples, suggesting that this tumor subset is probably less dependent from WNT activation than the other groups. Most importantly, HM-like tumors are characterized by the highest rate of KRAS mutation, a feature that has been previously noted in CIMP-L CRCs [31]. This is a CRC subset with a yet poorly defined clinical relevance, often grouped with the non-CIMP tumors in various studies [32] and sharing the majority of methylation targets with CIMP-H tumors [33]. By methylation analysis, we found that HM-like tumors had mainly a CIMP-L phenotype, at variance with HM and non-HM tumors, which were mostly associated with CIMP-H and non-CIMP phenotype, respectively [11]. Therefore, our data confirm a particularly high recurrence of KRAS mutations in a specific subset of CRCs, associated with CIMP-L phenotype. While the molecular background for this association is not understood yet, recent studies seem to indicate that the strong association between BRAF mutations and CIMP-H phenotype might be due to the need to suppress a senescence-inducing gene expression program promoted by mutant BRAF [34]. Oncogenic RAS molecules are also known to activate senescence in untransformed cells [35, 36]. It is tempting to speculate that also the relevant overlap between KRAS mutation and the CIMP-L phenotype in the HM-like subgroup could be related to the repression of a similar senescence-inducing gene expression program. Further efforts will be required to formally prove this hypothesis.
HM-like CRCs also showed the highest frequency of SOX9 gene mutations and the lowest rate of TP53 mutations. This association has been previously recognized, but its functional significance remains ununderstood [37].
Overall, the genetic marks of HM-like supports the hypothesis that may represent a distinct subgroup of CRCs, which may arise and progress through a different sequence of genetic events compared to the well-known MSI/hypermutated and MSS/CIN subsets. This is further supported by the analysis of mutational signatures, which indicate their unique similarity to the SBS30 pattern. This was recently associated with deficiency in the base excision repair and with inactivation of the NTHL1 gene [29]. Biallelic NTHL1 mutations are responsible for the NTHL1-tumor syndrome, a cancer-predisposing disease characterized by the occurrence of adenomatous polyposis and cancer at different sites, in addition to CRC [38]. This specific genetic fingerprint indicates that also the pathogenic mechanisms and the etiology underlying HM-like CRCs might be distinct from those leading to HM and non-HM CRCs. So far, we were unable to pull out genomic or transcriptomic alterations in the NTHL1 gene specifically occurring in the HM-like group, suggesting that functional inactivation of its pathway perhaps associated to the specific CIMP-L pattern might be involved in this respect. Additional studies should be implemented to highlight possible genetic/epigenetic hits or alternative/parallel pathways to NTHL1 inactivation, which might end up in eliciting the same molecular fingerprints.
The existence of a small group of pMMR/MSS CRCs (~ 10%) responsive to ICIs therapies has been inferred in several clinical studies [39,40,41]. Pagès and collaborators observed a high immunoscore in 21% of MSS compared to 45% of MSI [42]. Similar findings were reported by Kikuchi et al. which identified a subset of MSI‐L/MSS CRCs within the TCGA COAD/READ dataset showing upregulation of the IFN‐γ and CD8 T effector gene signatures [43]. They also confirmed the presence of a small fraction (~ 12%) of pMMR CRCs positive for PD‐L1 and p‐STAT1 showing increasing grades of infiltrating CD4(+) or CD8(+) TILs on a population of 219 CRC samples.
Our work raised the question whether the HM-like group identifies the same CRC subset. Indeed, not only WCGNA analysis of the transcriptome evidenced relevant differences among the three groups, but also indicated that the HM-like tumors bore high expression of genes associated with immune/inflammatory response. To better investigate this latter aspect, we defined the immune/inflammatory infiltration signature in the three subsets, according to [21]. Intriguingly, we confirmed that HM-like tumors showed T and NK cells signatures similar to HM samples which, as widely known, are inflamed tumors well responsive to ICI therapies. In contrast, proliferation, macrophage and interferon signatures in HM-like tumors were on average more similar to the non-HM than to HM group.
Data on the differential expressions of the ICGs curated by [22] further confirmed the outstanding differences among the three groups. Coherently with the immune infiltration analysis, HM samples showed a high expression of multiple ICGs, confirming the presence of an immune/inflammatory infiltrate (KIR and HLA genes) and differential expression of immune response modulators, including those targeted by established ICI therapies. KIR genes and ICGs (i.e., PD1, CTLA4, CD96 and TIGIT) for which specific targeting therapies have been introduced in the clinical practice [3, 44] also showed a higher expression in HM-like tumors compared to non-HM samples, supporting their immune/inflammatory infiltration. Moreover, our analysis highlighted ICGs exclusively expressed in HM-like, e.g. VTCN1, PCDCD1, CD96, BTNL9 and BTLA, encoding for important immune regulators of both stimulatory and inhibitory pathways, some of which are emerging as new promising targets for immunotherapy [45, 46]. While these data confirm the presence of an immune/inflammatory infiltrate in HM-like tumors showing modulation of established and potentially new immune checkpoint targets to consider for ICI therapies, remarkable differences emerged between HM-like and HM group. Among them, the relatively lower expression of HLA genes in HM-like samples is in line with the poor macrophage signature observed in this subgroup compared to HM samples. The significance of a potentially lower infiltration by antigen presenting/dendritic cells and the relevant differences in the pattern of immunomodulating molecules expressed in HM and HM-like tumors cannot be easily interpreted at the time being and definitely requires further investigations. These differences, however, do not contrast with our hypothesis that HM-like CRCs might be responsive to ICI. Of relevance, the strong negative regulation of IDO and TDO2 in HM-like compared to both HM and non-HM tumors suggest that the formers are possibly characterized by a less immunosuppressive microenvironment caused by the release of tryptophan metabolites. Perhaps this condition might also be related to the more frequent association of HM-like tumors with early stages CRC and may eventually make them more prone to immune reactivation.
Unfortunately, a major limitation of this study is represented by the lack of a univocal specific molecular biomarker/s facilitating the identification of HM-like CRC, in clinical settings. To this end, the possibility to use CIMP-L phenotype needs to be explored.
Conclusions
Our work indicates the existence of a previously unidentified CRC subgroup with distinctive features and possibly responsive to current or to be defined ICIs. If validated by experimental work, these findings can lead to expanding the fraction of patients eligible to ICIs treatment.
Availability of data and materials
All data generated or analyzed in this study are included in this article (and its supplementary information files), and are available from the corresponding author on request.
References
Cancer Statistics, 2021—PubMed. https://pubmed-ncbi-nlm-nih-gov.ezproxy.uniroma1.it/33433946/. Accessed 13 Dec 2021.
Nguyen HT, Duong H-Q. The molecular characteristics of colorectal cancer: implications for diagnosis and therapy. Oncol Lett. 2018;16(1):9–18. https://doi.org/10.3892/ol.2018.8679.
Ganesh K, Stadler ZK, Cercek A, Mendelsohn RB, Shia J, Segal NH, Diaz LA. Immunotherapy in colorectal cancer: rationale, challenges and potential. Nat Rev Gastroenterol Hepatol. 2019;16(6):361–75. https://doi.org/10.1038/s41575-019-0126-x.
Chalmers ZR, Connelly CF, Fabrizio D, Gay L, Ali SM, Ennis R, Schrock A, et al. Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med. 2017;9:1–14. https://doi.org/10.1186/s13073-017-0424-2.
Goodman AM, Kato S, Bazhenova L, Patel SP, Frampton GM, Miller V, Stephens PJ, Daniels GA, Kurzrock R. Tumor mutational burden as an independent predictor of response to immunotherapy in diverse cancers. Mol Cancer Ther. 2017;16(11):2598–608. https://doi.org/10.1158/1535-7163.MCT-17-0386.
Cheng Y-W, Pincas H, Bacolod M, Schemmann G, Giardina SF, Huang J, Barral S, et al. CpG island methylator phenotype associates with low-degree chromosomal abnormalities in colorectal cancer. Clin Cancer Res. 2008;14(19):6005–13. https://doi.org/10.1158/1078-0432.CCR-08-0216.
Belardinilli F, Capalbo C, Malapelle U, Pisapia P, Raimondo D, Milanetti E, Yasaman M, et al. Clinical multigene panel sequencing identifies distinct mutational association patterns in metastatic colorectal cancer. Front Oncol. 2020;10:560. https://doi.org/10.3389/fonc.2020.00560.
Capalbo C, Belardinilli F, Raimondo D, Milanetti E, Malapelle U, Pisapia P, Magri V, et al. A simplified genomic profiling approach predicts outcome in metastatic colorectal cancer. Cancers. 2019;11(2):147. https://doi.org/10.3390/cancers11020147.
Nicola De, Francesca FG, Pallocca M, Sperati F, Pizzuti L, Melucci E, Casini B, et al. Deep sequencing and pathway-focused analysis revealed multigene oncodriver signatures predicting survival outcomes in advanced colorectal cancer. Oncogenesis. 2018;7(7):55. https://doi.org/10.1038/s41389-018-0066-2.
Guinney J, Dienstmann R, Wang X, de Reyniès A, Schlicker A, Soneson C, Marisa L, et al. The consensus molecular subtypes of colorectal cancer. Nat Med. 2015;21(11):1350–6. https://doi.org/10.1038/nm.3967.
Muzny DM, Bainbridge MN, Chang K, Dinh HH, Drummond JA, Fowler G, Kovar CL, et al. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487(7407):330–7. https://doi.org/10.1038/nature11252.
André T, Shiu K-K, Kim TW, Jensen BV, Jensen LH, Punt C, Smith D, et al. Pembrolizumab in microsatellite-instability—high advanced colorectal cancer. N Engl J Med. 2020;383(23):2207–18. https://doi.org/10.1056/NEJMoa2017699.
Le DT, Durham JN, Smith KN, Wang H, Bartlett BR, Aulakh LK, Steve L, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357(6349):409–13. https://doi.org/10.1126/science.aan6733.
Mermel CH, Schumacher SE, Hill B, Meyerson ML, Beroukhim R, Getz G. GISTIC2.0 facilitates sensitive and confident localization of the targets of focal somatic copy-number alteration in human cancers. Genome Biol. 2011;12(4):R41. https://doi.org/10.1186/gb-2011-12-4-r41.
Nilsen G, Liestøl K, Van Loo P, Vollan HKM, Eide MB, Rueda OM, Chin S-F, et al. Copynumber: efficient algorithms for single- and multi-track copy number segmentation. BMC Genomics. 2012;13(November):591. https://doi.org/10.1186/1471-2164-13-591.
Mayakonda A, Lin D-C, Assenov Y, Plass C, Phillip Koeffler H. Maftools: efficient and comprehensive analysis of somatic variants in cancer. Genome Res. 2018;28(11):1747–56. https://doi.org/10.1101/gr.239244.118.
COSMIC|SBS—Mutational Signatures. https://cancer.sanger.ac.uk/signatures/sbs/. Accessed 3 May 2021.
Ritchie ME, Phipson B, Di Wu, Yifang Hu, Law CW, Shi W, Smyth GK. Limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43(7):e47–e47. https://doi.org/10.1093/nar/gkv007.
Langfelder P, Horvath S. WGCNA: an R package for weighted correlation network analysis. BMC Bioinform. 2008;9(1):559. https://doi.org/10.1186/1471-2105-9-559.
Zhang B, Horvath S. A general framework for weighted gene co-expression network analysis. Stat Appl Genet Mol Biol. 2005;4(1):12. https://doi.org/10.2202/1544-6115.1128.
Nirmal AJ, Regan T, Shih BB, Hume DA, Sims AH, Freeman TC. Immune cell gene signatures for profiling the microenvironment of solid tumors. Cancer Immunol Res. 2018;6(11):1388–400. https://doi.org/10.1158/2326-6066.CIR-18-0342.
Hu F-F, Liu C-J, Liu L-L, Zhang Q, Guo A-Y. Expression profile of immune checkpoint genes and their roles in predicting immunotherapy response. Brief Bioinform. 2021;22(3):bbaa176. https://doi.org/10.1093/bib/bbaa176.
Strickler JH, Hanks BA, Khasraw M. Tumor mutational burden as a predictor of immunotherapy response: is more always better? Clin Cancer Res. 2021;27(5):1236–41. https://doi.org/10.1158/1078-0432.CCR-20-3054.
Yaeger R, Chatila WK, Lipsyc MD, Hechtman JF, Cercek A, Sanchez-Vega F, Jayakumaran G, et al. Clinical sequencing defines the genomic landscape of metastatic colorectal cancer. Cancer Cell. 2018;33(1):125-136.e3. https://doi.org/10.1016/j.ccell.2017.12.004.
Pino MS, Chung DC. The chromosomal instability pathway in colon cancer. Gastroenterology. 2010;138(6):2059–72. https://doi.org/10.1053/j.gastro.2009.12.065.
Boland CR, Goel A. Microsatellite instability in colorectal cancer. Gastroenterology. 2010;138(6):2073-2087.e3. https://doi.org/10.1053/j.gastro.2009.12.064.
Helleday T, Eshtad S, Nik-Zainal S. Mechanisms underlying mutational signatures in human cancers. Nat Rev Genet. 2014;15(9):585–98. https://doi.org/10.1038/nrg3729.
Alexandrov LB, Kim J, Haradhvala NJ, Huang MN, Ng AWT, Yang Wu, Boot A, et al. The repertoire of mutational signatures in human cancer. Nature. 2020;578(7793):94–101. https://doi.org/10.1038/s41586-020-1943-3.
Drost J, van Boxtel R, Blokzijl F, Mizutani T, Sasaki N, Sasselli V, de Ligt J, et al. Use of CRISPR-modified human stem cell organoids to study the origin of mutational signatures in cancer. Science. 2017;358(6360):234–8. https://doi.org/10.1126/science.aao3130.
Markowitz SD, Bertagnolli MM. Molecular basis of colorectal cancer. N Engl J Med. 2009;361(25):2449–60. https://doi.org/10.1056/NEJMra0804588.
Ogino S, Kawasaki T, Kirkner GJ, Loda M, Fuchs CS. CpG island methylator phenotype-low (CIMP-Low) in colorectal cancer: possible associations with male sex and KRAS mutations. J Mol Diagn. 2006;8(5):582–8. https://doi.org/10.2353/jmoldx.2006.060082.
Jia M, Gao Xu, Zhang Y, Hoffmeister M, Brenner H. Different definitions of CpG island methylator phenotype and outcomes of colorectal cancer: a systematic review. Clin Epigenetics. 2016;8:25. https://doi.org/10.1186/s13148-016-0191-8.
Hinoue T, Weisenberger DJ, Lange CPE, Shen H, Byun H-M, Van Den Berg D, Malik S, et al. Genome-scale analysis of aberrant DNA methylation in colorectal cancer. Genome Res. 2012;22(2):271–82. https://doi.org/10.1101/gr.117523.110.
Tao Y, Kang B, Petkovich DA, Bhandari YR, In J, Stein-O’Brien G, Kong X, et al. Aging-like spontaneous epigenetic silencing facilitates Wnt activation, stemness, and BrafV600E-induced tumorigenesis. Cancer Cell. 2019;35(2):315-328.e6. https://doi.org/10.1016/j.ccell.2019.01.005.
Micco Di, Raffaella MF, Cicalese A, Piccinin S, Gasparini P, Luise C, Schurra C, et al. Oncogene-induced senescence is a DNA damage response triggered by DNA hyper-replication. Nature. 2006;444(7119):638–42. https://doi.org/10.1038/nature05327.
Serrano M, Lin AW, McCurrach ME, Beach D, Lowe SW. Oncogenic Ras provokes premature cell senescence associated with accumulation of P53 and P16INK4a. Cell. 1997;88(5):593–602. https://doi.org/10.1016/S0092-8674(00)81902-9.
Javier BM, Rona Yaeger Lu, Wang F-V, Zehir A, Middha S, Sadowska J, et al. Recurrent, truncating SOX9 mutations are associated with SOX9 overexpression, KRAS mutation, and TP53 wild type status in colorectal carcinoma. Oncotarget. 2016;7(32):50875–82. https://doi.org/10.18632/oncotarget.9682.
Belhadj S, Quintana I, Mur P, Munoz-Torres PM, Henar Alonso M, Navarro M, Terradas M, et al. NTHL1 biallelic mutations seldom cause colorectal cancer, serrated polyposis or a multi-tumor phenotype, in absence of colorectal adenomas. Sci Rep. 2019;9(1):9020. https://doi.org/10.1038/s41598-019-45281-1.
Chalabi M, Fanchi LF, Dijkstra KK, Van den Berg JG, Aalbers AG, Sikorska K, Lopez-Yurda M, et al. Neoadjuvant immunotherapy leads to pathological responses in MMR-proficient and MMR-deficient early-stage colon cancers. Nat Med. 2020;26(4):566–76. https://doi.org/10.1038/s41591-020-0805-8.
Williams DS, Mouradov D, Jorissen RN, Newman MR, Amini E, Nickless DK, Teague JA, et al. Lymphocytic response to tumour and deficient DNA mismatch repair identify subtypes of stage II/III colorectal cancer associated with patient outcomes. Gut. 2019;68(3):465–74. https://doi.org/10.1136/gutjnl-2017-315664.
Zaborowski AM, Winter DC, Lynch L. The therapeutic and prognostic implications of immunobiology in colorectal cancer: a review. Br J Cancer. 2021;125(10):1341–9. https://doi.org/10.1038/s41416-021-01475-x.
Pagès F, Mlecnik B, Marliot F, Bindea G, Fang-Shu Ou, Bifulco C, Lugli A, et al. International validation of the consensus immunoscore for the classification of colon cancer: a prognostic and accuracy study. Lancet. 2018;391(10135):2128–39. https://doi.org/10.1016/S0140-6736(18)30789-X.
Kikuchi T, Mimura K, Okayama H, Nakayama Y, Saito K, Yamada L, Endo E, et al. A subset of patients with MSS/MSI-low-colorectal cancer showed increased CD8(+) TILs together with up-regulated IFN-γ. Oncol Lett. 2019;18(6):5977–85. https://doi.org/10.3892/ol.2019.10953.
Egen JG, Kuhns MS, Allison JP. CTLA-4: new insights into its biological function and use in tumor immunotherapy. Nat Immunol. 2002;3(7):611–8. https://doi.org/10.1038/ni0702-611.
Chen Y-L, Lin H-W, Chien C-L, Lai Y-L, Sun W-Z, Chen C-A, Cheng W-F. BTLA blockade enhances cancer therapy by inhibiting IL-6/IL-10-induced CD19high B lymphocytes. J Immunother Cancer. 2019;7(1):313. https://doi.org/10.1186/s40425-019-0744-4.
Wang J-Y, Wang W-P. B7-H4, a promising target for immunotherapy. Cell Immunol. 2020;347: 104008. https://doi.org/10.1016/j.cellimm.2019.104008.
Acknowledgements
Francesca Belardinilli was supported by PEZCOLLER Foundation.
Funding
This work was supported by: Italian Ministry of Education, Universities and Research—Dipartimenti di Eccellenza—L. 232/2016; Associazione Italiana per la Ricerca sul Cancro (AIRC) [Grant Number IG24329]; Istituto Pasteur-Fondazione Cenci Bolognetti and fondi Ricerca Ateneo La Sapienza (to G. Giannini).
Author information
Authors and Affiliations
Contributions
PS: Methodology, validation, formal analysis, investigation, data curation, writing—original draft; FB: Conceptualization, validation, investigation, data curation, writing—original draft; VL: Methodology, formal analysis, investigation, data curation; PP: Conceptualization, methodology, supervision, data curation, writing—review and editing; GG: Conceptualization, writing—review and editing, supervision, project administration, funding acquisition. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary methods; Supplementary Table 1, 2, 5 and Supplementary figures 1,2 and 3. Descriptions of the supplementary tables and figures are embedded in the file.
Additional file 2.
Supplementary Table 3. This table reported the results of WGCNA analysis.
Additional file 3.
Supplementary Table 4. This table reported the functional enrichment results of the genes falling in the WGCNA - detected modules.
Additional file 4.
Supplementary Table 6. ICGs differentially expressed in the comparison HM vs non-HM and HM-like vs non-HM groups.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sibilio, P., Belardinilli, F., Licursi, V. et al. An integrative in-silico analysis discloses a novel molecular subset of colorectal cancer possibly eligible for immune checkpoint immunotherapy. Biol Direct 17, 10 (2022). https://doi.org/10.1186/s13062-022-00324-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13062-022-00324-y