Abstract
Study goal
We compared the survival rates of women with breast cancer (BC) detected within versus outside the mammography screening program (MSP) “donna”.
Methods
We merged data from the MSP with the data from corresponding cancer registries to categorize BC cases as within MSP (screen-detected and interval carcinomas) and outside the MSP. We analyzed the tumor stage distribution, tumor characteristics and the survival of the women. We further estimated hazard ratios using Cox-regressions to account for different characteristics between groups and corrected the survival rates for lead-time bias.
Results
We identified 1057 invasive (ICD-10: C50) and in-situ (D05) BC cases within the MSP and 1501 outside the MSP between 2010 and 2019 in the Swiss cantons of St. Gallen and Grisons. BC within the MSP had a higher share of stage I carcinoma (46.5% vs. 33.0%; p < 0.01), a smaller (mean) tumor size (19.1 mm vs. 24.9 mm, p < 0.01), and fewer recurrences and metastases in the follow-up period (6.7% vs. 15.6%, p < 0.01). The 10-year survival rates were 91.4% for women within and 72.1% for women outside the MSP (p < 0.05). Survival difference persisted but decreased when women within the same tumor stage were compared. Lead-time corrected hazard ratios for the MSP accounted for age, tumor size and Ki-67 proliferation index were 0.550 (95% CI 0.389, 0.778; p < 0.01) for overall survival and 0.469 (95% CI 0.294, 0.749; p < 0.01) for BC related survival.
Conclusion
Women participating in the “donna” MSP had a significantly higher overall and BC related survival rate than women outside the program. Detection of BC at an earlier tumor stage only partially explains the observed differences.
Similar content being viewed by others
Introduction
The goal of a mammography screening program (MSP) is to detect breast cancer (BC) at a prognostically favorable early stage, thus reducing the burden of disease by less aggressive treatment as well as increasing survival rates [1]. Randomized controlled trials (RCT) from the 1970’s and 1980’s demonstrated a reduction of BC related mortality rates by 15–20% through MSPs [2]. Consequently, national screening programs were introduced in an increasing number of countries. However, following a review by Gøtzsche et al. [3, 4] which concluded that MSPs were not cost-effective, in 2013, the Swiss Medical Board [5] officially advised against the introduction of new MSPs and recommended fading out existing ones. This recommendation was controversially discussed due to contradicting evidence from other studies [6].
While the effectiveness of MSPs is often evaluated based on studies from the past, the underlying decades-old data are only partially applicable to today’s situation. Mortality of BC has about halved in Switzerland [7], the USA [8], and many other Western countries [9]. More advanced treatment options, better technology for digital mammographies, the use of magnetic resonance imaging (MRI), vacuum assisted biopsies and wider use of screening programs as well as a higher awareness of women and the availability of specialized breast centers have all contributed to this favorable change.
To account for these improvements in diagnosis and treatment, updated studies are required using different methodologies, as conducting RCTs for the evaluation of MSPs is ethically not acceptable. Employing various methodological designs, a series of more recent international studies has shown decreased mortality and a reduction in disability-adjusted life years for women with BC diagnosed via MSPs [10,11,12]. For Switzerland, Herrmann [7] found a strong decline of overall BC mortality from 1992 to 2012, but, by comparing cantons with and without MSP, he did not detect significant regional differences as an effect of organized MSPs. Reports of several Swiss MSPs do not comment on mortality reduction due to screening. To the best of our knowledge a scientific evaluation on patient level of the effect on survival rates of MSPs compared to opportunistic screening was not performed in Switzerland, yet.
Therefore, we merged data from the MSP “donna” with a comprehensive dataset from the Cancer Registry of Eastern Switzerland and Grisons-Glarus to evaluate the impact of the MSP “donna” on the tumor stage distribution of detected BC, on the survival of the affected women and the applied cancer treatment. While other studies focused on effect differences between screen-detected versus non-screen-detected BC cases [13, 14], we deliberately investigated the effect that participation in an MSP had on women diagnosed with BC.
Patients and methods
Study population
The study included all 50- to 69-year-old women diagnosed with invasive and in-situ BC (ICD-10: C50 and D05) between 2010 and 2019 in the Swiss cantons of St. Gallen and Grisons. BC was either diagnosed within or outside the “donna” MSP. Cancer data was retrieved from the databases of the Cancer Registries of Eastern Switzerland and Grisons-Glarus [15], which document all cancer cases diagnosed in the two cantons and follow-up the vital status of each patient via the cantonal administrations and record the date of death or the date of last contact.
The MSP “donna” in the Swiss cantons of St. Gallen and Grisons
Each woman between 50 and 69 years of age in the cantons of St. Gallen (since 2010) and Grisons (since 2011) is invited bi-annually to voluntarily participate in the MSP “donna”, free of charge except for a small deductible. Each year around 18,500 mammographies are done within the MSP, with a participation rate oscillating around 50%.
Sample generation and data cleansing
Figure 1 shows the derivation of the final data sample for our analyses. The data from the Cancer Registries and from the MSP were merged using a unique screening-ID. A recorded tumor from the Cancer Registries was classified as a BC within MSP if the woman took part in the MSP “donna” and the carcinoma was either screen-detected or symptomatically detected within 2 years after the last mammography (see definition for interval carcinoma [16]). The remaining women with BC were labelled as outside the MSP. A total of 35 lobular carcinoma in situ (LCIS) cases were excluded from the analyses. Further, six cases were excluded due to insufficient information regarding their UICC-TNM tumor stage. 100 women had two primary BCs within the study period. Only the first tumor was included in the sample. If two primary tumors were diagnosed on the same day, the tumor with the highest stage was considered. Hence, the final data set comprised 1057 BC cases within and 1501 BC cases outside the MSP. The carcinomas within the MSP were either screen-detected carcinomas following a positive mammography (n = 840) or interval cancer cases (n = 217). Furthermore, we excluded in-situ carcinomas (n = 316) from the survival analyses to partially account for length bias and overdiagnosis from screening [17].
Derivation of the final data set for the analyses. Notes: Second primary BC were either excluded if diagnosed after the first primary BC or if two BCs had the same diagnosis date, the one with the more favorable tumor characteristics, based on UICC-TNM stage, T-Stage, histologic grading, tumor size, estrogen or progesterone receptor status, was excluded
Variables of interest
The final sample includes variables on patient and tumor characteristics, treatments, and survival. Patient characteristics include the age at diagnosis, canton of living and birthplace. Tumor characteristics include information about the biology of the tumor, i.e., tumor stage, tumor size, hormone receptor status, histologic grading, the human epidermal growth factor receptor 2 (HER2) status, and the Ki-67 proliferation index (Ki-67). Data for the patient’s primary treatments include information about adjuvant chemotherapies, surgical interventions, radiation therapy and whether the treatment was done in a certified breast center. Finally, follow-up data includes information about any occurred metastasis or recurrence, and the date of the last updated vital status. Patients from the canton of St. Gallen were followed up until mid-November 2022, from the canton of Grisons until the end of August 2023.
Methods and statistical analyses
Carcinomas within the MSP were compared to those outside the MSP with respect to their patient and tumor characteristics, primary treatments, and their survival. Wilcoxon-Mann Whitney rank sum tests or student’s t-tests, as appropriate, were used to test for significance in differences. The survival of the two groups was compared using Kaplan–Meier curves. Greenwood Point estimators for the Kaplan–Meier estimates were used to test for significance of the results.
Furthermore, to account for confounders, Cox proportional hazards regression models were calculated to estimate hazard ratios (HR). We estimated models controlling for age at diagnosis, tumor stages, Ki-67, tumor size, HER2, and treatment in certified breast centers to investigate potential survival differences. Moreover, we corrected results from Kaplan–Meier estimates and Cox proportional hazards regressions for lead-time bias, by adjusting survival time of women whose BC was screen-detected. Corrections are based on the methodological approach of Duffy et al. [13], using mean sojourn times from Tabar et al. [18]. We further included the year of diagnosis as dummy to account for treatment advancement over time (incidence period correction). All statistical analyses were done in Stata 18.
Ethics approval
This retrospective cohort study was submitted to the Ethics Commission of Eastern Switzerland (EKOS-23/061). It was ruled to be a quality control covered by the informed patient consent of the MSP. All data was pseudonymized by the Cancer Registry of Eastern Switzerland prior to analyses.
Results
Descriptives and comparative analyses
The study included 2558 women aged 50–69 with a BC diagnosis between 2010 and 2019. The average age at diagnosis was 59.3 years for women within and 60.7 years outside the MSP (see Table 1). Geographically, more BC cases are within the MSP in the canton of St. Gallen, compared to the more rural canton of Grisons (p < 0.05).
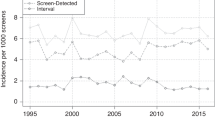
While ~ 40% of BC cases in our sample were detected within the MSP, the share of detection varied considerably across the years, from 7% in the inauguration year of the program (2010) to 45–53% in the last two rounds from 2015 to 2019 (see Fig. 5). Tumor stage distribution of women within the MSP was significantly different from women outside the MSP (p < 0.05). Figure 2 displays the corresponding distributions and shows that BC within the MSP were diagnosed at earlier stages with fewer locally advanced and metastatic characteristics. In particular, within the MSP 17.5% of BC were in the in-situ stage (vs. 8.7% outside the MSP) and further 46.5% were detected in stage I (vs. 33.0%). Finally, only 6.2 and 2.4% of BC cases within the MSP had stages III and IV (vs. 11.0 and 11.9%). Moreover, lymph node involvement (26.1 vs. 42.4%) and tumor sizes (19.3 vs. 25.3 mm) were significantly different. Other significant differences between the two groups could be found for positivity of progesterone receptors (78.6% vs. 75.0%), Ki-67 (34.4% vs. 41.5%) and the distribution of the histologic grading—with a more favorable grading for BC within compared to outside the MSP.
Comparative treatment and survival analyses
As can be seen in Table 2, treatments of women with invasive BC (stages I–IV) within the MSP were less aggressive and less burdensome than for women outside the MSP, which is reflected by half the rate of radical mastectomies (8.8% vs. 18.4%; p < 0.05) and a significantly lower proportion of patients undergoing adjuvant chemotherapy (33.7% vs. 44.1%; p < 0.05). Treatment was significantly more often performed within certified breast centers for women within the MSP. Noteworthy, the share of treated women in certified breast centers has changed over time. For instance, the first breast centers were certified in 2012 and the overall fraction of patients treated in breast centers has increased from 2% in 2012 to 74% in 2019.
Furthermore, Table 2 shows that the survival rates were significantly higher for women within the MSP. The difference in the survival rates increased over time, where 1-year survival rates differed by 2.9 percentage points (pp) (99.7% vs. 96.8%), the 5-year survival rate already differed by 11.6pp (96.7% vs. 85.1%) and the 10-year survival rate by 19.3pp (91.4% vs. 72.1%). Similar differences were also observed for the subgroups of tumor stage I and II. Other stages have a fairly low number of cases but show similar, albeit insignificant patterns.
Kaplan–Meier curves
Figure 3 depicts the survival probabilities over time. While the difference in survival increases over time, the differences are at almost all points in time significant. The overall Kaplan–Meier HR of within versus outside the MSP is 0.271 for all BC cases (Table 3). These significant better outcomes for women within the MSP persist, albeit at a lower magnitude, for the subgroups of stage I and II, that account for 71% of diagnosed BC cases. Moreover, Fig. 3b shows the lead-time corrected Kaplan–Meier curve for all tumor groups. The lead-time correction lowered the survival curve for women within the MSP, but survival was still significantly better for women within the MSP (84.7% survival rate after 10 years). Confidence intervals become large over time as sample size within MSP shrinks due to the lead-time correction.
Kaplan–Meier Curves of overall survival of women within versus outside the MSP—for all tumor stages, lead-time corrected, stage I, and stage II. Note: Shaded areas represent the confidence interval; within MSP consists of screen-detected and interval carcinomas; outside MSP comprise all women with BC that were not participating in any MSP; within MSP (adjusted) corrects the survival time for lead time [13, 18]
Furthermore, Fig. 4 shows, that the within MSP survival curve of BC specific survival is higher than for overall survival. For instance, 10-year BC survival lies at 96.5% for women within the MSP vs. at 92.5% for overall survival (82.5% vs. 74.0% for BC outside MSP). The Kaplan–Meier HR of BC related mortality of within MSP vs. outside MSP is 0.231 (see Table 3). This pattern is also true for the lead-time corrected Kaplan–Meier curve—which shows a survival rate at year 10 of 89.5%.
Kaplan–Meier Curves of BC related survival of women diagnosed within vs. outside the MSP. Notes: Shaded areas represent the confidence interval; within MSP consists of screen-detected and interval carcinomas; outside MSP comprise all women with BC that were not participating in any MSP; within MSP (adjusted) corrects the survival time for lead time [13, 18]
Cox proportional hazards regressions
Table 3 displays HR for overall mortality from six specifications of the Cox proportional hazards regression model, from a simple specification (1&2) only including whether the woman participated in the MSP or not, to controlling for different variables (3–6). Specifications (2–6) show results for lead-time corrected survival times. Specification (1) shows that women within the MSP had a 72.9% lower hazard of mortality (HR: 0.271; p < 0.01). When only looking at BC-related mortality, the HR was 0.231 (p < 0.01) (see Table 4). The lead-time adjusted results (2) show a change of the HR to 0.377 (p < 0.01). The HR of the program remained similar when accounted for age (3). When controlled for tumor size and Ki-67 (4), control variables for length bias, the HR increases to 0.550 (p < 0.01) with significant negative effects of Ki-67 and tumor size on survival. The similar specification for BC-related survival showed an HR of 0.469 (p < 0.01).
The effect of the MSP decreased when additionally accounted for tumor stages (HR: 0.691; p < 0.05). The higher the tumor stage, the higher was the hazard of mortality. Women diagnosed with stage IV had a ~ 16-times higher hazard of mortality than women with stage I carcinomas. When further controlled for HER2 and treatment in certified breast centers (6), the effect of the MSP changed slightly (HR: 0.699; p < 0.05), where HER2 had a significant effect on survival (HR: 1.880; p < 0.01), and certified breast center had no significant effect on the HR. HRs for BC-related mortality are shown in Table 4, and show insignificant HRs for the MSP as soon as tumor stages are included in the model.
Discussion
The results demonstrate a statistically more favorable tumor stage distribution within compared to outside the MSP. Tumor stage is predictive for survival and women with lower stages had less aggressive treatment options available. We found, furthermore, that the proportion of Ki-67 levels is significantly higher for BC diagnosed outside the MSP. High Ki-67 levels are associated with higher grading, larger tumor size [19] and correlate to late endocrine resistance [20]. Consequently, we found that the number of mastectomies for cases within the MSP was about half compared to outside the MSP (8.9% vs. 17.7%). These results are in line with Hermann et al. [21] in a partially overlapping population covering a different time period. Less invasive and aggressive treatments directly translate into an improved quality of life for patients, as reported by Jay et al. [22] who showed better patient reported outcomes with respect to breast, psychosocial and sexual well-being of breast conserving therapy compared to mastectomy. Moreover, less lymph node infiltrations lead to fewer axillary dissections, potentially preventing possible burdensome side effects, such as lymphedema.
Most importantly, we found a significant survival difference for women within the MSP compared to women outside the MSP, starting in the first year after diagnosis with a continuously widening survival difference in absolute terms. At ten years after diagnosis the uncorrected survival difference amounted to 18.2pp (92.2% vs. 74.0%). However, estimations for survival effects of MSPs in observational studies are prone to lead-time bias [23]. Lead-time bias happens when screening increases the perceived survival time without affecting the course of the disease [24]. When correcting the survival of women with screen-detected BC for lead-time [13] the positive effect of MSPs on survival was still highly significant (HR: 0.377; p < 0.01). HR of the MSP, uncorrected and corrected for lead-time were in line with other studies [13, 25]. For instance, Schumann et al. [25] found an unadjusted HR of a German MSP of 0.23, and when adjusted for lead-time bias via several methods HRs between 0.32 and 0.39. Duffy et al. [13] estimated lead-time corrected HR for a Swedish MSP of 0.40. Nevertheless, other studies such as Munck et al. [14] reported lower effects of MSPs (HR: 0.76) in the Netherlands on disease-free survival when corrected for lead-time bias. This difference might be explained by a shorter follow-up time, investigating disease-free survival instead of overall survival, and by different patient characteristics in their sample (e.g., tumor stage distribution).
Furthermore, a different age distribution between the groups could affect overall survival, due to non-BC related mortality. Accounting for age only marginally affected survival. Further, differences in other characteristics such as Ki-67 and tumor size—potential determinants for a length bias (screening detects disproportionately more slowly growing tumors) [26]—could lead to an overestimation of the effectiveness of MSPs. However, lead-time corrected HR controlled for age, Ki-67 and tumor size still showed significantly positive effects of the MSP (HR: 0.550; p < 0.01).
This sustained difference in survival can have multiple reasons. Firstly, we observed different tumor characteristics of women depending on MSP participation. For instance, a more favorable tumor stage distribution is a well-recognized prognostic factor [27] and an acknowledged advantage of screening [28], and might explain the survival differences. While we showed that the detection of BC at an earlier stage had a significant effect on survival, it only partially explained the observed effects. Significant overall survival differences lowered but persisted when women of the same tumor stages were compared (e.g., for stage 1 at 10 years: 96.3% vs. 85.8%; p < 0.05), and when HR were controlled for tumor stage distribution (HR: 0.691; p < 0.05).
Secondly, outcome differences might occur if groups are treated in different medical settings. We found that women within the MSP were more often treated in certified breast centers, where treatment was different with less mastectomies and fewer chemotherapy. These differences are supported by evidence from other studies. For example, a Dutch study found that non-screeners more often stopped taking adjuvant antihormonal treatments [29]. Moreover, if a suspicious finding appears in a screening mammography, the warranted sequence of further examinations, biopsy, and interdisciplinary tumor boards is still part of the organized MSP. Most of the time surgery and adjuvant treatment are given in one of the certified breast centers according to strict quality-controlled guidelines. The fact that women, whose BC was diagnosed outside the program, were more often treated outside of a certified breast center, could contribute to the different treatment outcomes and is a possible explanation for the finding that survival differences persisted in favor of the MSP even if corrected for stage distribution. Surprisingly, we did not find significant effects from treatments in certified breast centers for our sample. This result needs to be taken with care as certification only started in 2010 in Switzerland and their share varied considerably from 2010 to 2019. Furthermore, lower shares of detected BC cases within the program in earlier years (see Fig. 5) coupled with treatment advancements over time potentially bias our results. Therefore, we included an incidence year dummy in our regressions to account for period effects.
Lastly, as this was an observational study, there might have been unobserved differences in the characteristics of women participating in MSPs compared to those not participating. For instance, the screened population might differ in socioeconomic status (SES) and simultaneously in health-related factors as shown in several studies [30, 31], which can affect survival. A study from the Netherlands [30] showed that women of low SES were less likely to participate in MSPs than women with high SES (odds ratio of 1.8), and further had less favorable tumor stages—and thus were more likely to die from BC. Similar studies from Switzerland demonstrated significant differences of the tumor stage distribution of BC diagnosed in patients of lower compared to higher SES [32] as well as higher screening uptake of women with higher SES [33, 34]. While we controlled for tumor stage distribution in our analyses, other unobserved differences in survival relevant factors between the groups might have affected the differences in survival, and would, if systematic, lead to an overestimation of the survival effect from participating in MSPs.
Comparing our results to other studies shows that various incidence based mortality studies could find a 26% reduction of deaths of BC comparing to historical controls or areas without screening [11]. A more current survey of European screening programs showed a wide variation but significant reductions of BC mortality when comparing screened to non-screened women [12]. Duffy et al. [35] found that in the population of women regularly undergoing mammography screening the proportion of BC fatal after 10 years was reduced by 50%, somewhat less so in intermittent participants (− 36%). For women participating at five consecutive screening rounds the risk of dying from BC was reduced by 74%, and after statistical adjustments for self-selection to 66% (HR: 0.34) [36]. These HR are in the range of our findings.
Limitations
Our study comes with limitations. Firstly, the overall mortality rate of age-standardized BC has significantly shrunk over the last 30 years not only internationally, but also in our local data from 34.3 to 18.7 per 100,000/year, whereas the age-standardized incidence has increased from 87.0 to 103.5 cases per 100,000/year [37]. Improvements in treatment had an important and beneficial effect on BC mortality and might be more relevant for decreasing overall mortality than screening [38]. In our study we do not compare with historical controls before the introduction of screening. Using incidence-based mortality data of the two groups diagnosed and treated at the same time in the same area eliminates a bias caused by considerably better treatment regimens over time. We controlled for period effects by including the year of the incidence as dummy variable to account for improvements in treatment over time. Secondly, the correction of lead-time bias can only approximate the effect of sojourn time and is based on a multi-state Markov model [13]. Abrahamsson et al. [39] in their simulation based on a tumor growth model showed that lead times can be shorter when conditional to tumor characteristics. This could potentially result in an underestimation of lead-time corrected survival effects from MSPs. Thirdly, adjustment of length bias is usually based on many assumptions [39]. By estimating models controlling for Ki-67 and tumor size, potential indicators for length bias, we showed that survival differences persisted. At the same time, differences in tumor size and Ki-67 are also direct advantages of MSPs—and controlled results do not fully reflect length bias. Lastly, bias might arise due to an overdiagnosis of tumors within the MSP [40]. By estimating our models excluding in-situ carcinoma we partially address the overdiagnosis bias [41]. Lastly, a certain share of BC cases outside the MSP are detected via opportunistic screening (see Fig. 5), which might affect the survival likelihood of the outside MSP cases positively. As we want to evaluate the effectiveness of an organized MSP, the “donna” program, compared to any outside detected BC, the key takeaways from our study are unaffected.
Conclusion
To summarize, our results strongly support findings from other countries that participation in MSPs significantly increases survival of women with BC. Not correcting HR for lead-time and length bias leads to an overestimation of the effects from MSPs on survival. Moreover, diagnosis of BC in earlier tumor stages within MSPs allows for significantly less aggressive treatments contributing to a better quality of life. Given the presented results on the effectiveness of the MSP “donna” an evaluation of the cost-effectiveness is desirable. This might lead to a broader adoption of MSPs in Switzerland.
Availability of data and materials
Raw data for the mammography screening program “donna” and the Cancer Registry of Eastern Switzerland are not publicly available to preserve individuals’/patients´ privacy.
References
Bulliard JL, Braendle K, Fracheboud J, Zwahlen M. Breast cancer screening programmes in Switzerland, 2010–2018; 2021.
Marmot MG, Altman DG, Cameron DA, Dewar JA, Thompson SG, Wilcox M. The benefits and harms of breast cancer screening: an independent review. Br J Cancer. 2013;108:2205–40.
Gøtzsche PC, Olsen O. Is screening for breast cancer with mammography justifiable? Lancet. 2000;355:129–34.
Gøtzsche PC. Relation between breast cancer mortality and screening effectiveness: systematic review of the mammography trials. Dan Med Bull. 2011;58:A4246.
Swiss Medical Board: Systematisches Mammographie-Screening; 2013.
Duffy SW, Chen THH, Smith RA, Yen AMF, Tabar L. Real and artificial controversies in breast cancer screening. Breast Cancer Management. 2013;2:519–28.
Herrmann C, Vounatsou P, Thürlimann B, Probst-Hensch N, Rothermundt C, Ess S. Impact of mammography screening programmes on breast cancer mortality in Switzerland, a country with different regional screening policies. BMJ Open. 2018;8:e017806.
Giaquinto AN, Sung H, Miller KD, Kramer JL, Newman LA, Minihan A, Jemal A, Siegel RL. Breast Cancer Statistics, 2022. CA Cancer J Clin. 2022;72:524–41.
Lei S, Zheng R, Zhang S, Wang S, Chen R, Sun K, Zeng H, Zhou J, Wei W. Global patterns of breast cancer incidence and mortality: a population-based cancer registry data analysis from 2000 to 2020. Cancer Commun (London, England). 2021;41:1183–94.
Lim ZL, Ho PJ, Khng AJ, Yeoh YS, Ong ATW, Tan BKT, Tan EY, Tan S-M, Lim GH, Lee JA, Tan VKM, Hu J, Li J, Hartman M. Mammography screening is associated with more favourable breast cancer tumour characteristics and better overall survival: case-only analysis of 3739 Asian breast cancer patients. BMC Med. 2022;20:239.
Njor S, Nyström L, Moss S, Paci E, Broeders M, Segnan N, Lynge E. Breast cancer mortality in mammographic screening in Europe: a review of incidence-based mortality studies. J Med Screen. 2012;19(Suppl 1):33–41.
Molassiotis A, Tyrovolas S, Giné-Vázquez I, Yeo W, Aapro M, Herrstedt J. Organized breast cancer screening not only reduces mortality from breast cancer but also significantly decreases disability-adjusted life years: analysis of the Global Burden of Disease Study and screening programme availability in 130 countries. ESMO open. 2021;6:100111.
Duffy SW, Nagtegaal ID, Wallis M, Cafferty FH, Houssami N, Warwick J, Allgood PC, Kearins O, Tappenden N, O’Sullivan E, Lawrence G. Correcting for lead time and length bias in estimating the effect of screen detection on cancer survival. Am J Epidemiol. 2008;168:98–104.
de Munck L, Eijkelboom AH, Otten JDM, Broeders MJM, Siesling S. Method of primary breast cancer detection and the disease-free interval, adjusting for lead time. J Natl Cancer Inst. 2023;116:370–8.
Swiss Cancer Regsitries: Description of the legally binding data dictionary for all cancer registries under the new law on cancer registrations; 2019.
Perry N. Guidelines for quality assurance in breast cancer screening and diagnosis. Luxembourg: Office for Official Publications of the European Communities; 2006.
Duffy SW, Lynge E, Jonsson H, Ayyaz S, Olsen AH. Complexities in the estimation of overdiagnosis in breast cancer screening. Br J Cancer. 2008;99:1176–8.
Tabár L, Vitak B, Chen HH, Duffy SW, Yen MF, Chiang CF, Krusemo UB, Tot T, Smith RA. The Swedish Two-County Trial twenty years later Updated mortality results and new insights from long-term follow-up. Radiol Clin North Am. 2000;38:625–51.
Marwah N, Batra A, Marwah S, Gupta V, Shakya S, Sen R. Correlation of proliferative index with various clinicopathologic prognostic parameters in primary breast carcinoma: a study from North India. J Cancer Res Ther. 2018;14:537–42.
Lee J, Lee Y-J, Bae SJ, Baek SH, Kook Y, Cha YJ, Lee JW, Son BH, Ahn SH, Lee HJ, Gong G, Jeong J, Lee SB, Ahn SG. Ki-67, 21-gene recurrence score, endocrine resistance, and survival in patients with breast cancer. JAMA Netw Open. 2023;6:e2330961.
Herrmann C, Morant R, Walser E, Mousavi M, Thürlimann B. Screening is associated with lower mastectomy rates in eastern Switzerland beyond stage effects. BMC Cancer. 2021;21:229.
Jay M, Creelman B, Baliski C. Patient reported outcomes associated with surgical intervention for breast cancer. Am J Surg. 2020;219:816–22.
Shapiro S, Goldberg JD, Hutchison GB. Lead time in breast cancer detection and implications for periodicity of screening. Am J Epidemiol. 1974;100:357–66.
Cox B, Sneyd MJ. Bias in breast cancer research in the screening era. Breast (Edinburgh, Scotland). 2013;22:1041–5.
Schumann L, Hadwiger M, Eisemann N, Katalinic A. Lead-time corrected effect on breast cancer survival in Germany by mode of detection. Cancers. 2024;16:1326.
Marcus PM, Prorok PC, Miller AB, DeVoto EJ, Kramer BS. Conceptualizing overdiagnosis in cancer screening. J Natl Cancer Inst. 2015;107:djv014.
Ellison LF, Saint-Jacques N. Five-year cancer survival by stage at diagnosis in Canada. Health Rep. 2023;34:3–15.
Wilkinson AN, Billette J-M, Ellison LF, Killip MA, Islam N, Seely JM. the impact of organised screening programs on breast cancer stage at diagnosis for Canadian women Aged 40–49 and 50–59. Curr oncol (Toronto, Ont). 2022;29:5627–43.
He W, Eriksson L, Törnberg S, Strand F, Hall P, Czene K. Discontinuation of adjuvant hormone therapy among breast cancer patients not previously attending mammography screening. BMC Med. 2019;17:24.
Aarts MJ, Voogd AC, Duijm LEM, Coebergh JWW, Louwman WJ. Socioeconomic inequalities in attending the mass screening for breast cancer in the south of the Netherlands–associations with stage at diagnosis and survival. Breast Cancer Res Treat. 2011;128:517–25.
Pokora RM, Büttner M, Schulz A, Schuster AK, Merzenich H, Teifke A, Michal M, Lackner K, Münzel T, Zeissig SR, Wild PS, Singer S, Wollschläger D. Determinants of mammography screening participation-a cross-sectional analysis of the German population-based Gutenberg Health Study (GHS). PLoS ONE. 2022;17:e0275525.
Feller A, Schmidlin K, Bordoni A, Bouchardy C, Bulliard J-L, Camey B, Konzelmann I, Maspoli M, Wanner M, Clough-Gorr KM. Socioeconomic and demographic disparities in breast cancer stage at presentation and survival: a Swiss population-based study. Int J Cancer. 2017;141:1529–39.
Jolidon V, de Prez V, Bracke P, Bell A, Burton-Jeangros C, Cullati S. Revisiting the effects of organized mammography programs on inequalities in breast screening uptake: a multilevel analysis of nationwide data from 1997 to 2017. Front Public Health. 2022;10:812776.
Sandoval JL, Theler J-M, Cullati S, Bouchardy C, Manor O, Gaspoz J-M, Guessous I. Introduction of an organised programme and social inequalities in mammography screening: a 22-year population-based study in Geneva, Switzerland. Prev Med. 2017;103:49–55.
Duffy SW, Tabár L, Yen AM-F, Dean PB, Smith RA, Jonsson H, Törnberg S, Chen SL-S, Chiu SY-H, Fann JC-Y, Ku MM-S, Wu WY-Y, Hsu C-Y, Chen Y-C, Svane G, Azavedo E, Grundström H, Sundén P, Leifland K, Frodis E, Ramos J, Epstein B, Åkerlund A, Sundbom A, Bordás P, Wallin H, Starck L, Björkgren A, Carlson S, Fredriksson I, et al. Mammography screening reduces rates of advanced and fatal breast cancers: results in 549,091 women. Cancer. 2020;126:2971–9.
Smith RA, Duffy SW, Yen AM-F, Tabár L, Lin AT-Y, Chen SL-S, Hsu C-Y, Dean P, Chen TH-H. Beneficial effect of repeated participation in breast cancer screening upon survival. JCO. 2023;41:552.
Katalinic A, Eisemann N, Kraywinkel K, Noftz MR, Hübner J. Breast cancer incidence and mortality before and after implementation of the German mammography screening program. Int J Cancer. 2020;147:709–18.
Plevritis SK, Munoz D, Kurian AW, Stout NK, Alagoz O, Near AM, Lee SJ, van den Broek JJ, Huang X, Schechter CB, Sprague BL, Song J, de Koning HJ, Trentham-Dietz A, van Ravesteyn NT, Gangnon R, Chandler Y, Li Y, Xu C, Ergun MA, Huang H, Berry DA, Mandelblatt JS. Association of screening and treatment with breast cancer mortality by molecular subtype in US women, 2000–2012. JAMA. 2018;319:154–64.
Abrahamsson L, Isheden G, Czene K, Humphreys K. Continuous tumour growth models, lead time estimation and length bias in breast cancer screening studies. Stat Methods Med Res. 2020;29:374–95.
The benefits and harms of breast cancer screening: an independent review. Lancet (London, England) 2012, 380:1778–1786
Ryser MD, Lange J, Inoue LYT, O’Meara ES, Gard C, Miglioretti DL, Bulliard J-L, Brouwer AF, Hwang ES, Etzioni RB. Estimation of breast cancer overdiagnosis in a U.S. breast screening cohort. Ann Intern Med. 2022;175:471–8.
Funding
This research was funded by the Cancer League of Eastern Switzerland.
Author information
Authors and Affiliations
Contributions
All authors contributed to conceptualization. DK and MB developed the methodology. DK, JS and MB were responsible for data curation and DK and MB performed all analyses. All authors interpreted the results. DK wrote the original draft. All authors reviewed and edited the manuscript. RM supervised.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective cohort study was submitted to the Ethics Commission of Eastern Switzerland (EKOS-23/061). It was ruled to be a quality control covered by the informed patient consent of the MSP. All data was pseudonymized by the Cancer Registry of Eastern Switzerland prior to analyses.
Consent for publication
Not applicable.
Competing interests
RM, MB, and AE work for the Cancer League of Eastern Switzerland, which is responsible for the mammography screening program “donna” and the Cancer Registry of Eastern Switzerland. All other authors do not declare any conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kuklinski, D., Blum, M., Subelack, J. et al. Breast cancer patients enrolled in the Swiss mammography screening program “donna” demonstrate prolonged survival. Breast Cancer Res 26, 84 (2024). https://doi.org/10.1186/s13058-024-01841-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13058-024-01841-6