Abstract
Background
Gremlin-1 (GREM1) and Gremlin-2 (GREM2) are bone morphogenetic protein antagonists that play important roles in organogenesis, tissue differentiation, and tissue homeostasis. Although GREM1 has been reported to be involved in promoting various cancers, little has been reported about effects of GREM2 on cancer. Recently, it has been reported that GREM2 can inhibit adipogenesis in adipose-derived stromal/stem cells. However, as an inhibitor of adipogenesis, the role of GREM2 in cancer progression is not well understood yet.
Methods
Pre-adipocyte 3T3-L1 cells overexpressing mock or Grem2 were established using a lentiviral transduction system and differentiated into adipocytes-mock and adipocytes-Grem2, respectively. To investigate the effect of adipocyte-Grem2 on breast cancer cells, we analyzed the proliferative and invasion abilities of spheroids using a 3D co-culture system of breast cancer cells and adipocytes or conditioned medium (CM) of adipocytes. An orthotopic breast cancer mouse model was used to examine the role of adipocytes-Grem2 in breast cancer progression.
Results
Grem2 overexpression suppressed adipogenesis of 3T3-L1 cells. Proliferative and invasion abilities of spheroids formed by co-culturing MTV/TM-011 breast cancer cells and adipocytes-Grem2 were significantly reduced compared to those of spheroids formed by co-culturing MTV/TM-011 cells and adipocytes-mock. Compared to adipocytes-mock, adipocytes-Grem2 showed decreased mRNA expression of several adipokines, notably IL-6. The concentration of IL-6 in the CM of these cells was also decreased. Proliferative and invasive abilities of breast cancer cells reduced by adipocytes-Grem2 were restored by IL-6 treatment. Expression levels of vimentin, slug, and twist1 in breast cancer cells were decreased by treatment with CM of adipocytes-Grem2 but increased by IL-6 treatment. In orthotopic breast cancer mouse model, mice injected with both MTV/TM-011 cells and adipocytes-Grem2 showed smaller primary tumors and lower lung metastasis than controls. However, IL-6 administration increased both the size of primary tumor and the number of metastatic lung lesions, which were reduced by adipocytes-Grem2.
Conclusions
Our study suggests that GREM2 overexpression in adipocytes can inhibit adipogenesis, reduce the expression and secretion of several adipokines, including IL-6, and ultimately inhibit breast cancer progression.
Similar content being viewed by others
Background
Cysteine knot-secreting proteins Gremlin-1 (GREM1) and Gremlin-2 (GREM2) are bone morphogenetic protein (BMP) antagonists. These gremlins play important roles in embryogenesis, organ development, and tissue differentiation through antagonistic regulation of BMPs [1, 2]. GREM1 is implicated in various pathological conditions such as pulmonary or renal fibrosis [3,4,5] and diabetic kidney disease [6]. In addition, GREM1 is overexpressed in various cancers. It has been reported to be involved in cancer proliferation and metastasis [7, 8]. Unlike GREM1, GREM2 has few reports in these pathological conditions. GREM2 can inhibit the differentiation of bone marrow-derived mesenchymal stem cells into osteoblasts [9]. GREM2 can regulate cardiac differentiation of cardiac progenitor cells and enhance cardioprotective effect [10]. GREM2 plays a role in suppressing side effects of excessive inflammation after myocardial infarction by inhibiting BMP signaling [11]. More interestingly, GREM2 not only inhibits adipogenesis in 3T3-L1 pre-adipocytes [12], but also functions as an inhibitor of adipogenesis in adipose-derived stromal/stem cells [13] through activation of Wnt/β-catenin signaling. However, the role of GREM2 in cancer progression is not well understood yet.
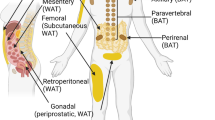
Adipocytes are derived from pluripotent mesenchymal stem cells, converted into pre-adipocytes, and then differentiated into mature adipocytes. This process of differentiation of adipocytes is called adipogenesis. Various proteins such as peroxisome proliferator-activated receptor γ (PPARγ), CCAAT/enhancer binding protein α (C/EBPα), and fatty acid binding protein 4 (FABP4) are involved in adipogenesis [14,15,16]. Adipocytes are one of the major stromal cells of many tissues. They are considered to play an important role in promoting cancer growth in the tumor microenvironment [17]. In particular, since adipocytes are main stromal cells of breast tissues, interactions between adipocytes and breast cancer cells are highly correlated with breast cancer progression [18].
Cancer-associated adipocytes (CAAs) are involved in breast tumorigenesis [19]. CAAs secrete a variety of inflammatory and cancer-related adipokines such as tumor necrosis factor-α, interleukin-6 (IL-6), and plasminogen activator inhibitor-1 that can increase breast cancer cell proliferation, invasion, metastasis, and therapeutic resistance [20,21,22,23]. In particular, IL-6 and its associated signaling can promote breast cancer progression and metastasis [24,25,26,27]. IL-6 secreted from adipose stromal cells (ASCs) can promote the migration and invasion of estrogen receptor-negative breast cancer cells both in vitro and in vivo, while depletion of IL-6 in conditioned medium (CM) of ASCs can suppress the stimulatory effect of ASCs on breast cancer cell migration and invasion [28]. Adipocyte-derived IL-6 and leptin can promote breast cancer metastasis by promoting the expression of lysyl hydroxylase [24]. Serum IL-6 levels are positively correlated with serum VEGF levels in breast cancer patients, which can promote angiogenesis and metastasis [29]. IL-6 can increase resistance of breast cancer cells to drug treatment by inducing Mdr1 gene expression [30], and downregulation of IL-6 is associated with better response to breast cancer treatment [31].
Inhibiting adipocyte differentiation or blocking adipokine secretion through modulation of adipocytes could be a new treatment paradigm for breast cancer. TAZ knockdown or deficiency in mouse adipocytes inhibits breast tumorigenesis through impaired expression and secretion of the adipocytes-derived hormone Resistin [32]. More recently, BZ26, a derivative of the PPARγ antagonist GW9662, attenuated breast cancer progression by inhibiting the progression of mature adipocytes into CAA-like cells [33]. Although many studies have reported that adipogenesis can promote breast cancer, studies on new adipogenesis inhibitors that can inhibit breast cancer growth and their mechanisms are not yet well known. In this study, we found that GREM2 suppressed adipocyte differentiation and that adipocytes overexpressing Grem2 reduced the production of several adipokines, including IL-6, contributing to the inhibition of breast cancer cell growth and lung metastasis. These results suggest that overexpressing GREM2 in adipocytes can be a new therapeutic approach to effectively inhibit breast cancer proliferation and metastasis.
Methods
Cell culture and reagents
3T3-L1 cells were purchased from the American Type Culture Collection (USA). 3T3-L1 cells were maintained in DMEM (Thermo Fisher Scientific, USA), bovine calf serum (BCS, HyClone, USA) and 1% penicillin/streptomycin (Corning Inc., USA). MDA-MB-231 and MTV/TM-011 cells were obtained from Korean Cell Line Bank (Republic of Korea). MDA-MB-231 and MTV/TM-011 cells were cultured in RPMI (Corning Inc.) containing 10% fetal bovine serum (Thermo Fisher Scientific) and 1% penicillin/streptomycin (Corning Inc.). Cells were maintained at 37 °C in a humidified atmosphere with 5% CO2/95% air. Recombinant mouse GREM2 protein was obtained from R&D Systems (USA). Recombinant mouse IL-6 protein was purchased from Sino Biological Inc. (China). Rabbit polyclonal GREM2 antibody was purchased from Abcam (UK). Anti-PPARγ, anti-C/EBPα, anti-FABP4, anti-vimentin, anti-slug, anti-twist1, and anti-β-actin were obtained from Cell Signaling Technology (USA). Epigallocatechin gallate (EGCG), metformin, and PKH26/PKH67 fluorescent cell linker kits were purchased from Sigma-Aldrich (USA).
Establishment of stable cell line
3T3-L1 cell lines stably expressing either mock or Grem2 were established using a lentiviral transduction system. Briefly, mouse Grem2 lentiviral vector (EX-Mm06243-Lv122) was obtained from GeneCopoeia (USA). The lentiviruses were packaged in 293T cells using Lenti-Pac™ HIV expression packaging kit (GeneCopoeia). After 72 h transfection, the viral supernatant was collected, filtered and used for the transduction of 3T3-L1 cells in the presence of 8 μg/ml polybrene (Merck Millipore, USA). Stable cell lines were selected by 1 μg/ml puromycin (InvivoGen, USA).
Differentiation of 3T3-L1 pre-adipocytes
3T3-L1 cells were cultured to reach 100% confluence in DMEM containing 10% BCS and then cultured for an additional 48 h. To initiate differentiation, the growth medium was removed and DMEM differentiation medium containing 10% FBS, 0.5 mM methylisobutylxanthine (Sigma-Aldrich, USA), 1 μM dexamethasone (Sigma-Aldrich), and 10 μg/ml insulin (Sigma-Aldrich) was added. After 48 h, the differentiation medium was replaced with DMEM adipocyte maintenance medium containing 10 μg/ml insulin, and the medium was changed every 48–72 h. When adipogenesis was observed in 3T3-L1 cells, the medium was replaced with fresh DMEM medium containing 10% FBS once every 2–3 days.
Oil red O staining
3T3-L1 cells were differentiated and cultured for 9 days, and fat droplets were stain with Oil red O solution (Sigma-Aldrich). The dye was decolorized with 100% isopropyl alcohol and quantified at 500 nm absorbance.
Western blot analysis
Standard sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) and western blotting were used to analyze the expression of various proteins. Cells were lysed in the lysis buffer (Cell Signaling Technology) containing protease inhibitors and phosphatase inhibitors (Roche, Basel, Switzerland). The quantitative protein concentration was determined by BCA Protein Assay Kit (Thermo Fisher Scientific) and equal amounts of protein were loaded on 8–12% SDS-PAGE. Proteins were transferred to polyvinylidene difluoride membrane (Merck Millipore) and subjected to immunoblotting using various antibodies overnight at 4 °C, followed by further incubation with the secondary antibody (AbFrontier, Republic of Korea) at room temperature for 1 h. Visualization of protein bands was detected with Westsave Gold detection reagents (AbFrontier).
3D spheroid formation
3T3-L1 and MTV/TM-011 cells were labeled with green or red fluorescent cell linker (Sigma-Aldrich), respectively. The cells were mixed with each other in a 1:1 ratio [34] and seeded in 96-well low-adhesion plates (Cornning). To check the cell proliferation of the spheroids, the cell viability was analyzed using CellTiter-Glo® 3D cell viability assay (Promega, USA). For 3D spheroid invasion assays, 3T3-L1 and MTV/TM-011 cells were mixed with extracellular matrix and seeded in the 3D culture qualified 96 well spheroid formation plate (CULTREX). After 3-days incubation, the invasion matrix was added. The plate was incubated for additional 5–9 days and the invasion of spheroids was observed under the microscope. The obtained images were analyzed using software ImageJ described by the manufacturer.
Reverse transcription-quantitative polymerase chain reaction (RT-qPCR)
Total RNA was isolated from cells using TRIzol® (Thermo Fisher Scientific). Reverse transcription of total RNA was performed using M-MLV reverse transcriptase (Enzynomics, Republic of Korea) according to the manufacturer’s protocol. Quantitative PCR (qPCR) was performed using TOP real™ qPCR 2X Pre-MIX (Enzynomics) and StepOnePlus Real-Time PCR (Thermo Fisher Scientific). Actb was used as internal references. Primer sequences are listed in the Additional file 1: Table S1.
IL-6 enzyme-linked immunosorbent assay (ELISA) assay
After differentiation of 3T3-L1-mock or 3T3-L1-Grem2 cells for 9 days, conditioned medium was obtained from each cell line. Each conditioned medium was placed on an IL-6 ELISA microplate (Thermo Fisher Scientific) and incubated for 2 h. All procedures were performed according to the manufacturer's instructions.
In vivo mouse model
Female BALB/c mice, 5 weeks of age (weight 18–20 ± 1–2 g) were purchased from Orient Bio Inc. (Republic of Korea). Mice were controlled in specific pathogen free conditions: 20–24 °C, 12/12 h of dark/light cycle, 60 ± 5% humidity, and plastic cage (4 mice/cage). For the orthotopic breast cancer mouse model, differentiated 3T3-L1-mock or 3T3-L1-Grem2 cells were mixed with MTV/TM-011 cells and inoculated into the fourth mammary fat pad of anesthetized mice by isoflurane inhalation. Both the volume of the primary tumors and the body weight of mice were measured twice a week. At the end of the experiment, mice were euthanized by CO inhalation and each tumor was removed.
Immunofluorescence staining
Before staining of fixed paraffin-embedded tissues, we followed the standard protocol including the steps of deparaffinization, antigen retrieval, and permeabilization. For immunofluorescence, detection of primary antibodies was done using fluorescent conjugates of Alexa Fluor® 488 antibody (Thermo Fisher Scientific) along with ProLong® Gold Antifade Reagent with DAPI (Thermo Fisher Scientific).
Statistical analysis
Data were expressed as the mean ± SD of results obtained from at least three independent experiments. Significant differences were determined by a Student’s t-test or one/two-way ANOVA. A p value of less than 0.05 was considered to be statistically significant.
Results
GREM2 inhibits adipogenesis in pre-adipocytes
It has been reported that GREM2 can inhibit adipogenesis in pre-adipocytes [12]. To confirm the function of GREM2 as an adipogenic inhibitor, GREM2 expression levels in differentiated adipocytes with or without treatment with well-known adipogenic inhibitors such as epigallocatechin-gallate (EGCG) and metformin were compared. 3T3-L1 pre-adipocytes were cultured to confluence and differentiated using the standard induction cocktail with EGCG or metformin for 9 days. EGCG and metformin reduced the adipogenesis of 3T3-L1 cells, which was confirmed by Oil red O staining (Fig. 1a, b). Interestingly, expression levels of adipocyte differentiation regulators such as PPARγ, C/EBPα, and FABP4 were decreased, whereas the expression of GREM2 was increased in adipocytes treated with high concentrations of EGCG and metformin (Fig. 1c, d). Conflicting expression of these adipogenic regulators and GREM2 was more pronounced in metformin-treated cells, which showed significantly inhibited adipogenesis, than in EGCG-treated cells. To investigate correlations between GREM2 and adipogenic regulators such as PPARγ, C/EBPα, and FABP4, GTEx datasets from human breast tissues were obtained using the web server GEPIA [35]. As shown in Fig. 1e, correlation analysis revealed negative correlations of GREM2 with PPARγ (Spearman r = − 0.66, p = 5.2 × 10−24), C/EBPα (Spearman r = − 0.54, p = 6.1 × 10−15), and FABP4 (Spearman r = − 0.62, p = 1 × 10−20).
GREM2 expression is increased in adipocytes in which adipogenesis is inhibited by adipogenic inhibitors. A–C 3T3-L1 cells were cultured to confluence and differentiated using the standard induction cocktail with EGCG (10 or 50 μM) or metformin (5 or 10 mM) for 9 days. The effect of EGCG or metformin on lipid accumulation was measured by Oil red O staining (A). The bar graph represents relative lipid accumulation. Two-sided t-test. ***, p < 0.001, ns, not significant (B). On the 9th day of differentiation, proteins were isolated from adipocytes and the lysates were immunoblotted with the indicated antibodies (C). D The bar graphs represent relative band intensity. V: vehicle, E: EGCG, M: metformin. Two-sided t-test. *, p < 0.05; **, p < 0.01; ***, p < 0.001. E The correlation between GREM2 and adipogenic regulators in GTEx human breast tissues was investigated by using the web GEPIA. Correlation analysis was conducted using Spearman rank test
To determine whether GREM2 could directly inhibit 3T3-L1 adipogenesis, mouse recombinant GREM2 protein was used to treat 3T3-L1 cells for 9 days to induce differentiation. Cell morphology and Oil red O staining results indicated that cells differentiated by treatment with GREM2 protein accumulated significantly less lipids than vehicle-treated cells (Fig. 2a, b). In addition, expression levels of adipogenic regulators such as PPARγ, C/EBPα, and FABP4 were reduced in differentiated 3T3-L1 cells treated with GREM2 protein (Fig. 2c, d). Next, 3T3-L1 cell lines stably overexpressing mock or Grem2 were established using a lentiviral transduction system. 3T3-L1-mock or 3T3-L1-Grem2 cells were cultured to confluence and differentiated into adipocytes (adipocytes-mock and adipocytes-Grem2) using the standard induction cocktail for 9 days. As shown in Fig. 2e and f, lipid accumulation was significantly inhibited in adipocytes-Grem2 cells compared to that in control cells. Expression levels of adipogenic regulators were also reduced in adipocytes-Grem2 cells (Fig. 2g, h). Together, these results indicate that GREM2 is an important regulator of adipogenesis by suppressing it.
GREM2 inhibits adipogenesis in 3T3-L1 pre-adipocytes. A and B 3T3-L1 cells were cultured to confluence and differentiated using the standard induction cocktail with vehicle or GREM2 recombinant protein (50 ng/ml) for 9 days. The effect of vehicle or GREM2 protein on lipid accumulation was measured by Oil red O staining (A) and the bar graph represents relative lipid accumulation (B). E and F 3T3-L1-mock or 3T3-L1-Grem2 pre-adipocytes were cultured to confluence and differentiated using the standard induction cocktail for 9 days. The effect of mock or Grem2 overexpression in pre-adipocytes on lipid accumulation was measured by Oil red O staining (E) and the bar graph represents relative lipid accumulation (F). C and G On the 9th day of differentiation, proteins were isolated from adipocytes and the lysates were immunoblotted with the indicated antibodies. D and H The bar graphs represent relative band intensity. Two-sided t-test. ***, p < 0.001
Grem2-overexpressing adipocytes inhibit proliferation and invasion of breast cancer cells
Adipogenesis is associated with obesity, which in turn may increase the risk and aggressiveness of breast cancer [36]. We used a 3D co-culture system of adipocytes and breast cancer cells to investigate the effect of GREM2-suppressed adipogenesis on breast cancer cells. 3T3-L1-mock and 3T3-L1-Grem2 cells were differentiated into adipocytes (adipocytes-mock and adipocytes-Grem2) for 9 days and then mixed with breast cancer MTV/TM-011 cells at the same ratio to form 3D spheroids in ultra-low attachment plates (Fig. 3a). Cell membranes of adipocytes and breast cancer cells were stained with fluorescent dyes of different colors (red: breast cancer cells, green: adipocytes) to confirm that these cells were well mixed within the spheroid. As shown in Fig. 3b, sizes of spheroids formed by co-culture of MTV/TM-011 cells and adipocytes-Grem2 were smaller than those of spheroids formed by co-culture of MTV/TM-011 cells and adipocytes-mock. CellTiter-Glo® 3D Cell Viability Assay results also showed that the proliferation of spheroids formed by co-culture of MTV/TM-011 cells and adipocytes-Grem2 was significantly reduced compared to that of the control group (Fig. 3c).
Adipocytes overexpressing Grem2 inhibit the proliferation and invasion of breast cancer cells. A–C After differentiation of 3T3-L1-mock or 3T3-L1-Grem2 pre-adipocytes for 9 days, each cell line was mixed with MTV/TM-011 cells and seeded into ultra-low attachment 96 wells. Before mixing the cells, adipocytes were fluorescently stained green and breast cancer cells red (A). The growth of spheroids by 3D co-culture was observed under a fluorescence microscope (B) and their proliferation level was measured using the CellTiter-Glo® 3D Cell Viability Assay (C). Scale bar = 100 µm. Two-sided t-test. ***, p < 0.001. D–F After differentiation of 3T3-L1-mock or 3T3-L1-Grem2 pre-adipocytes for 9 days, each cell line was mixed with MTV/TM-011 cells and performed 3D invasion assay (D, E). The invasion area was measured using the Image J (F). Scale bar = 100 µm. Two-way ANOVA. *, p < 0.05; **, p < 0.01; ***, p < 0.001; ns, not significant
Next, we performed a co-spheroid invasion assay to determine the effect of Grem2-overexpressing adipocytes on invasion ability of breast cancer cells (Fig. 3d). After culturing spheroids with invasion matrix, the invasion area of each spheroid was measured on the 3rd, 7th, and 9th days. As a result, it was confirmed that the invasion area of spheroids formed with MTV/TM-011 cells and adipocytes-Grem2 was significantly suppressed compared to that of spheroids formed with MTV/TM-011 cells and adipocytes-mock (Fig. 3e, f). These results suggest that Grem2-overexpressing adipocytes can inhibit the proliferation and invasiveness of breast cancer cells.
Expression of adipokines is lower in Grem2-overexpressing adipocytes than in control cells
Various adipokines secreted from adipocytes are known to promote cancers including breast cancer [37,38,39]. We hypothesized that adipocytes overexpressing Grem2 could inhibit breast cancer cell proliferation and invasion by suppressing certain adipokines. First, breast cancer cells were directly treated with conditioned medium (CM) obtained from differentiated pre-adipocytes. Its effect on proliferation of breast cancer cells was investigated. As a result, it was confirmed that the proliferation of breast cancer cells (MTV/TM-011 or MDA-MB-231) treated with the CM obtained from adipocytes-Grem2 was significantly reduced compared to that of cells treated with CM obtained from adipocytes-mock (Fig. 4a). Next, we investigated mRNA levels of several adipokines using qRT-PCR to determine which adipokines were suppressed in Grem2-overexpressing adipocytes. After differentiation of 3T3-L1 cells by treatment with vehicle or mouse recombinant GREM2 protein, RNA was isolated from each adipocyte and mRNA expression levels of Il6, Serpine1, Igf1, Tnf, and Ccl2 were determined. As shown in Fig. 4b, the expression levels of all adipokines except Tnf were significantly decreased in adipocytes differentiated by GREM2 protein treatment. Consistent with these results, the expression of several adipokines, including Il6, in adipocytes differentiated from 3T3-L1-Grem2 cells was significantly decreased compared to that in the control group (Fig. 4c). In addition, IL-6 ELISA analysis revealed that the concentration of IL-6 present in the culture medium of Grem2-overexpressing adipocytes was significantly reduced compared to that in the control group (Fig. 4d). Based on previous studies showing that overexpression of Grem2 in adipocytes increases Wnt/β-catenin signaling, we further tested whether GREM2 suppresses IL-6 expression by increasing Wnt/β-catenin activity in adipocytes. As shown in the Fig. 4e, IL-6 expression was decreased in adipocytes-Grem2 compared to adipocytes-mock and again significantly increased when co-treated with MSAB, a Wnt/β-catenin inhibitor.
IL-6 expression is reduced in adipocytes overexpressing Grem2. A 3T3-L1-mock or 3T3-L1-Grem2 cells were differentiated into adipocytes, and each CM was obtained from day 7 to day 9 when adipogenesis was observed. MTV/TM-011 or MDA-MB-231 cells were seeded in 96 well plates and incubated with each CM for 72 h, followed by MTS assay. B 3T3-L1 cells were differentiated using the standard induction cocktail with vehicle or GREM2 recombinant protein (50 ng/ml) for 9 days. RNA was isolated from each cell line and the expression of the indicated genes was analyzed by qPCR. C 3T3-L1-mock or 3T3-L1-Grem2 cells were differentiated using the standard induction cocktail for 9 days. RNA was isolated from each cell line and the expression of the indicated genes was analyzed by qPCR. D 3T3-L1-mock or 3T3-L1-Grem2 cells were differentiated into adipocytes, and IL-6 content was examined in each adipocyte CM obtained on the 9th day of differentiation. Two-sided t-test. *, p < 0.05; **, p < 0.01; ***, p < 0.001; ns, not significant. E Adipocytes-mock or adipocytes-Grem2 cells were treated with or without MSAB (10 μM) for 24 h. RNA was isolated from each cell line and the expression of the indicated genes was analyzed by qPCR. Two-way ANOVA. ***, p < 0.001; ns, not significant
Various studies have reported that cytokines, including IL-6, are expressed in cancer cells themselves [40,41,42,43,44]. Recently, it was confirmed that breast cancer cells are secretory cells capable of producing various cytokines using the 41 cytokine MILLIPLEX assay [45]. Therefore, we checked whether Grem2 overexpression in adipocytes also affected the reduction of IL-6 expression in breast cancer cells. After culturing adipocytes-mock or adipocytes-Grem2 on the transwells and MTV/TM-011 breast cancer cells on the bottom for 48 h, changes in IL-6 mRNA expression in breast cancer cells were examined. Interestingly, the expression of IL-6 in breast cancer cells was significantly reduced by co-culture of adipocytes-Grem2 (Additional file 2: Fig. S1). Taken together, these results suggest that Grem2-overexpressing adipocytes have the potential to suppress the expression of cytokines, including IL-6, in adipocytes or breast cancer cells, which may contribute to the inhibition of breast cancer progression.
IL-6 affects the restoration of the proliferative and invasion abilities of breast cancer cells reduced by Grem2-overexpressing adipocytes
Next, whether reduced expression and secretion of IL-6 in Grem2-overexpressing adipocytes had a direct effect on the proliferation of breast cancer cells was determined. MTV/TM-011 breast cancer cells were treated with CM from mock- or Grem2-overexpressing adipocytes. CM obtained from Grem2-overexpressing adipocytes decreased the proliferation of breast cancer cells compared to the control. Such decrease was significantly restored by IL-6 recombinant protein treatment (Fig. 5a). To examine effects of Grem2-overexpressing adipocytes and IL-6 protein on invasive capacity of breast cancer cells, we performed a 3D invasion assay. As shown in Fig. 5b and c, the invasive capacity of MTV/TM-011 cells was decreased by CM obtained from Grem2-overexpressing adipocytes compared to the control. Such decrease was again significantly rescued by IL-6 treatment. These results were consistent with results of the invasion assay by 3D co-culture of breast cancer cells and adipocytes overexpressing Grem2. Co-spheroids of MTV/TM-011 cells and Grem2-overexpressing adipocytes showed decreased invasive ability compared to the control. Such decrease was significantly restored by further treatment with IL-6 protein (Fig. 5d, e). The invasion ability of breast cancer cells, which was reduced by adipocyte-Grem2, was greatly restored by IL-6 treatment alone, but additional administration of Serpine1, another cytokine reduced by adipocyte-Grem2, had a greater effect on recovering cancer cell invasion (Additional file 3: Fig. S2).
IL-6 restores the ability of breast cancer cells to proliferate and invade, which was inhibited by adipocytes overexpressing Grem2. A MTV/TM-011 cells were seeded in a 96-well plate and treated with each adipocyte CM or IL-6 recombinant protein (25 ng/ml) for 72 h, followed by MTS assay. B MTV/TM-011 cells were treated with each adipocyte CM or IL-6 recombinant protein (25 ng/ml), and then 3D invasion analysis was performed. Scale bar = 100 µm. D After differentiation of 3T3-L1-mock or 3T3-L1-Grem2 into adipocytes for 9 days, 3D invasion assay was performed by mixing adipocytes-mock or adipocytes-Grem2 with MTV/TM-011 cells. Scale bar = 100 µm. C and E The relative invasion area was measured using the Image J. F MTV/TM-011 or MDA-MB-231 cells were treated with each adipocyte CM or IL-6 recombinant protein (25 ng/ml) for 72 h. The lysates were immunoblotted with the indicated antibodies. H Each adipocyte and MTV/TM-011 cells were co-cultured for 72 h in a transwell system (upper chamber: adipocytes, bottom: MTV/TM-011) with or without IL-6 recombinant protein (25 ng/ml). The lysates of MTV/TM-011 cells were immunoblotted with the indicated antibodies. G and I The bar graphs represent relative band intensity. Two-way ANOVA. *, p < 0.05; **, p < 0.01; ***, p < 0.001; ns, not significant
To further confirm the effects of Grem2-overexpressing adipocytes and IL-6 on the invasion ability of breast cancer cells, expression levels of key proteins related to epithelial-mesenchymal transition (EMT) and cancer cell invasion were examined. Two breast cancer cell lines MTV/TM-011 and MDA-MB-231 were treated with CM obtained from adipocytes-mock or adipocytes-Grem2. As a result, expressions levels of vimentin, slug, and twist1 were all decreased in breast cancer cells by the CM obtained from adipocytes-Grem2. However, expression levels of these proteins were increased again by combined treatment with adipocytes-Grem2 CM and IL-6 (Fig. 5f, g). Next, adipocytes and breast cancer cells were indirectly co-cultured through a transwell system. As a result of co-culture of MTV/TM-011 cells and adipocytes-Grem2, protein expression levels of vimentin, slug, and twist1 in MTV/TM-011 cells were significantly decreased compared to those of co-culture with adipocytes-mock. Incubation with IL-6 and adipocytes-Grem2 also increased expression levels of these proteins in MTV/TM-011 cells (Fig. 5h, i). These results suggest that adipokines, especially IL-6, are reduced in adipocytes overexpressing Grem2, which has the effect of suppressing the proliferation and invasion of breast cancer cells.
Proliferative and lung metastatic abilities of breast cancer cells in vivo are decreased by Grem2-overexpressing adipocytes but increased by IL-6 treatment
To investigate the role of GREM2 in breast cancer proliferation and metastasis, 3T3-L1-mock or 3T3-L1-Grem2 cells were differentiated into adipocytes, mixed with MTV/TM-011 cells, and orthotopically implanted into mammary fat pads of mice. Mice injected with MTV/TM-011 cells and adipocytes-Grem2 developed smaller primary tumors than mice injected with MTV/TM-011 cells and adipocytes-mock, resulting in a dramatic reduction in tumor volume [mean ± SD (mm3): 333.07 ± 103.87 (MTV/TM-011 + adipocytes-mock_vehicle) vs. 148.78 ± 34.16 (MTV/TM-011 + adipocytes-Grem2_vehicle), six mice/each group]. Interestingly, intraperitoneal administration of recombinant IL-6 protein in mice injected with MTV/TM-011 cells and adipocytes-Grem2 accelerated primary tumor growth compared to vehicle-treated group [mean ± SD (mm3): 148.78 ± 34.16 (MTV/TM-011 + adipocytes-Grem2_vehicle) vs. 249.55 ± 97.8 (MTV/TM-011 + adipocytes-Grem2_IL-6], six mice in MTV/TM-011 + adipocytes-Grem2_vehicle; five mice in MTV/TM-011 + adipocytes-Grem2_IL-6) (Fig. 6a, b). Consistent with the growth outcome of the primary tumor, mice injected with MTV/TM-011 cells and adipocytes-Grem2 had less lung metastases than mice injected with MTV/TM-011 cells and adipocytes-mock. Additionally, intraperitoneal administration of recombinant IL-6 protein in mice injected with MTV/TM-011 cells and adipocytes-Grem2 increased the number of metastatic lung lesions compared to the vehicle-treated group (Fig. 6c and Additional file 4: Fig. S3). To further confirm effects of Grem2-overexpressing adipocytes and IL-6 on breast cancer progression in vivo, levels of vimentin, slug, and twist1 in primary tumors from each group were analyzed by immunofluorescence staining. As shown in Fig. 6d and Additional file 5: Fig. S4, expression levels of these proteins were significantly decreased in mice injected with MTV/TM-011 cells and adipocytes-Grem2 compared to those in mice injected with MTV/TM-011 cells and adipocytes-mock. In addition, when IL-6 was administered to mice injected with MTV/TM-011 cells and adipocytes-Grem2, expression levels of these proteins were increased again. Taken together, these results indicate that overexpressing Grem2 in adipocytes can reduce breast cancer cell proliferation and lung metastasis in vivo and IL-6 can reverse these effects. These results suggest that decreased IL-6 secretion due to overexpression of Grem2 in adipocytes contributes to suppressing breast cancer progression.
IL-6 restores breast cancer proliferation and lung metastasis inhibited by adipocytes overexpressing Grem2. A–C After differentiation of 3T3-L1-mock or 3T3-L1-Grem2 into adipocytes for 9 days, adipocytes-mock or adipocytes-Grem2 were mixed with MTV/TM-011 cells and injected into mammary fat pads of mice. Representative images of primary tumors (A), tumor volume (B), and lung metastatic foci (C). Black arrowheads indicate prominent lung metastatic foci. D Representative immunofluorescence images of vimentin, slug, and twist1 in tumors. Scale bar = 100 μm. Two-way ANOVA. *, p < 0.05; **, p < 0.01; ns, not significant
Discussion
Since adipogenesis causes various diseases such as obesity and cancer, various compounds capable of suppressing it have been reported. In particular, EGCG, a green tea extract, and metformin, a hypoglycaemic drug, can inhibit adipogenesis and lipid accumulation of pre-adipocytes [46,47,48,49]. In this study, it was confirmed that when pre-adipocytes were treated with metformin, adipocyte differentiation was inhibited, while GREM2 expression was significantly increased. Together with these results, the inhibition of adipogenesis by GREM2 itself clearly showed that GREM2 could act as an adipogenic inhibitor. The present study demonstrates that GREM2 can inhibit adipogenesis and that adipocytes overexpressing Grem2 play an important role in inhibiting breast cancer cell growth, migration, and metastasis.
The tumor microenvironment composed of various cell types and extracellular matrix proteins provides favorable conditions for the growth and survival of cancer cells. Therefore, it is important to consider the tumor microenvironment in order to effectively inhibit tumor proliferation and metastasis [50, 51]. Adipose tissue is a representative stromal tissue of the breast. Cancer-related adipocytes have been reported to play a role in promoting breast cancer in the breast cancer microenvironment. Our results suggest that inhibition of adipogenesis in adipocytes might affect the breast cancer microenvironment and inhibit the progression of breast cancer. In this study, the expression of several adipokines was significantly suppressed in adipocytes overexpressing GREM2 compared to those in control cells. In particular, inhibition of the adipokine IL-6 by GREM2 had an effect in suppressing proliferation, migration, and metastasis of breast cancer cells in the breast cancer microenvironment. In addition to adipocytes, fibroblasts are also one of the major stromal cells constituting the breast [52,53,54]. Although the effect of GREM2 on cancer-associated fibroblasts in the breast cancer microenvironment is still unknown, exosomal miR-423-5p secreted by cancer-associated fibroblasts in prostate cancer is known to be able to promote chemotherapy resistance by inhibiting GREM2 [55]. Thus, further studies are needed to examine the relationship between GREM2 and cancer-associated fibroblasts in breast cancer.
This study showed that the expression and production of several adipokines were suppressed in Grem2-overexpressing adipocytes. One of the transcription factors that regulates the expression of the representative adipokine IL-6 is NF-κB [56, 57]. Wnt/β-catenin is known to negatively regulate the NF-κB signaling pathway [58, 59]. In human chondrocytes, Wnt-3A stimulation can suppress mRNA expression of IL-6 induced by NF-κB/IL-1β [60]. Activation of β-catenin also reduced NF-κB activity and the expression of its target gene IL-6 [61]. It has been reported that β-catenin can inhibit IL-6 transcription and expression in human astrocytes [62, 63]. C/EBP family members are also transcription factors involved in the expression of several adipokines, including IL-6, and are known to be negatively regulated by Wnt/β-catenin. C/EBPα, C/EBPβ and C/EBPδ are all involved in adipogenesis, and the Wnt/β-catenin pathway eventually inhibits them to suppress adipogenesis [64]. In addition, Wnt signaling suppressed C/EBPα and PPARγ to stimulate osteoblastogenesis of mesenchymal precursors [65]. Interestingly, GREM2 is known to inhibit adipogenesis of pre-adipocytes and adipose-derived stromal/stem cells by activating Wnt/β-catenin signaling [12, 13]. We confirmed that reduced IL-6 expression in Grem2-overexpressing adipocytes was restored when treated with a Wnt/β-catenin inhibitor. This shows that the increase in Wnt/β-catenin signaling by GREM2 is involved in the decrease in IL-6 expression. Although a direct relationship between GREM2 and IL-6 has not been reported yet, our results suggest that overexpression of GREM2 in adipocytes might inhibit IL-6 expression through activation of Wnt/β-catenin signaling. This phenomenon may be related to decreased activity of NF-κB or C/EBP transcription factors due to increased Wnt/β-catenin signaling.
As an adipogenic inhibitor, GREM2 could be developed as a target for obesity or a therapeutic means to inhibit breast cancer progression. This study suggests that reduced expression of several adipokines in adipocytes overexpressing GREM2 may contribute to breast cancer suppression. Additionally, our study suggests that GREM2, a type of cytokine, can be secreted when overexpressed in adipocytes and may directly contribute to the suppression of breast cancer independently of adipokines. The mechanism by which GREM2 directly affects breast cancer cells requires further detailed studies. Recently, research on gene therapy for various diseases has been actively conducted. One of the most frequently used techniques is inserting a gene of interest or healthy gene into a vector such as a plasmid, nanostructure, or virus [66, 67]. TP53 is a representative tumor suppressor involved in cell cycle arrest, apoptosis, and DNA damage repair. Gene therapy using adenoviral p53 has shown anti-tumor effects in pre-clinical and clinical studies [68, 69]. In this context, further studies are needed to utilize GREM2 for gene therapy or to discover small molecules that can increase GREM2 expression in adipocytes to effectively treat breast cancer.
Conclusion
In conclusion, we, for the first time, report that GREM2 overexpression in adipocytes can inhibit breast cancer proliferation and metastasis. GREM2 inhibited adipogenesis and the production of the adipokines, including IL-6, in adipocytes, which likely makes an important contribution to the inhibition of breast cancer progression. In addition, it is possible that GREM2 itself, secreted from GREM2-overexpressing adipocytes, has an effect on breast cancer suppression independently of adipokines. GREM2 can be an effective therapeutic target for treating various adipocyte-associated carcinomas. Our findings suggest that overexpressing GREM2 in adipocytes is a novel therapeutic approach to effectively inhibit breast cancer proliferation and metastasis.
Availability of data and materials
Available upon request to corresponding author (sappark@sch.ac.kr).
References
Ali IH, Brazil DP. Bone morphogenetic proteins and their antagonists: current and emerging clinical uses. Br J Pharmacol. 2014;171(15):3620–32.
Yanagita M. BMP antagonists: their roles in development and involvement in pathophysiology. Cytokine Growth Factor Rev. 2005;16(3):309–17.
Church RH, Ali I, Tate M, Lavin D, Krishnakumar A, Kok HM, et al. Gremlin1 plays a key role in kidney development and renal fibrosis. Am J Physiol Renal Physiol. 2017;312(6):F1141–57.
Farkas L, Farkas D, Gauldie J, Warburton D, Shi W, Kolb M. Transient overexpression of Gremlin results in epithelial activation and reversible fibrosis in rat lungs. Am J Respir Cell Mol Biol. 2011;44(6):870–8.
Myllarniemi M, Lindholm P, Ryynanen MJ, Kliment CR, Salmenkivi K, Keski-Oja J, et al. Gremlin-mediated decrease in bone morphogenetic protein signaling promotes pulmonary fibrosis. Am J Respir Crit Care Med. 2008;177(3):321–9.
Roxburgh SA, Kattla JJ, Curran SP, O’Meara YM, Pollock CA, Goldschmeding R, et al. Allelic depletion of grem1 attenuates diabetic kidney disease. Diabetes. 2009;58(7):1641–50.
Sung NJ, Kim NH, Surh YJ, Park SA. Gremlin-1 promotes metastasis of breast cancer cells by activating STAT3-MMP13 signaling pathway. Int J Mol Sci. 2020;21(23):9227.
Park SA, Sung NJ, Choi BJ, Kim W, Kim SH, Surh YJ. Gremlin-1 augments the oestrogen-related receptor alpha signalling through EGFR activation: implications for the progression of breast cancer. Br J Cancer. 2020;123(6):988–99.
Wang CL, Xiao F, Wang CD, Zhu JF, Shen C, Zuo B, et al. Gremlin2 suppression increases the BMP-2-induced osteogenesis of human bone marrow-derived mesenchymal stem cells via the BMP-2/Smad/Runx2 signaling pathway. J Cell Biochem. 2017;118(2):286–97.
Li W, Lu Y, Han R, Yue Q, Song X, Wang F, et al. Gremlin2 regulates the differentiation and function of cardiac progenitor cells via the notch signaling pathway. Cell Physiol Biochem. 2018;47(2):579–89.
Sanders LN, Schoenhard JA, Saleh MA, Mukherjee A, Ryzhov S, McMaster WG Jr, et al. BMP antagonist gremlin 2 limits inflammation after myocardial infarction. Circ Res. 2016;119(3):434–49.
Wu Q, Tang SG, Yuan ZM. Gremlin 2 inhibits adipocyte differentiation through activation of Wnt/beta-catenin signaling. Mol Med Rep. 2015;12(4):5891–6.
Kawagishi-Hotta M, Hasegawa S, Igarashi T, Date Y, Ishii Y, Inoue Y, et al. Increase of gremlin 2 with age in human adipose-derived stromal/stem cells and its inhibitory effect on adipogenesis. Regen Ther. 2019;11:324–30.
Ahmad B, Serpell CJ, Fong IL, Wong EH. Molecular mechanisms of adipogenesis: the anti-adipogenic role of AMP-activated protein kinase. Front Mol Biosci. 2020;7:76.
Ali AT, Hochfeld WE, Myburgh R, Pepper MS. Adipocyte and adipogenesis. Eur J Cell Biol. 2013;92(6–7):229–36.
Tang QQ, Lane MD. Adipogenesis: from stem cell to adipocyte. Annu Rev Biochem. 2012;81:715–36.
Yao H, He S. Multi-faceted role of cancer-associated adipocytes in the tumor microenvironment. Mol Med Rep. 2021;24(6):1–14.
Wu Q, Li B, Li Z, Li J, Sun S, Sun S. Cancer-associated adipocytes: key players in breast cancer progression. J Hematol Oncol. 2019;12(1):95.
Rybinska I, Mangano N, Tagliabue E, Triulzi T. Cancer-associated adipocytes in breast cancer: causes and consequences. Int J Mol Sci. 2021;22(7):3775.
Chu DT, Phuong TNT, Tien NLB, Tran DK, Nguyen TT, Thanh VV, et al. The effects of adipocytes on the regulation of breast cancer in the tumor microenvironment: an update. Cells. 2019;8(8):857.
Booth A, Magnuson A, Fouts J, Foster M. Adipose tissue, obesity and adipokines: role in cancer promotion. Horm Mol Biol Clin Investig. 2015;21(1):57–74.
Divella R, De Luca R, Abbate I, Naglieri E, Daniele A. Obesity and cancer: the role of adipose tissue and adipo-cytokines-induced chronic inflammation. J Cancer. 2016;7(15):2346–59.
Balistreri CR, Caruso C, Candore G. The role of adipose tissue and adipokines in obesity-related inflammatory diseases. Mediat Inflamm. 2010;2010:802078.
He JY, Wei XH, Li SJ, Liu Y, Hu HL, Li ZZ, et al. Adipocyte-derived IL-6 and leptin promote breast cancer metastasis via upregulation of Lysyl Hydroxylase-2 expression. Cell Commun Signal. 2018;16(1):100.
Manore SG, Doheny DL, Wong GL, Lo HW. IL-6/JAK/STAT3 signaling in breast cancer metastasis: biology and treatment. Front Oncol. 2022;12:866014.
Masjedi A, Hashemi V, Hojjat-Farsangi M, Ghalamfarsa G, Azizi G, Yousefi M, et al. The significant role of interleukin-6 and its signaling pathway in the immunopathogenesis and treatment of breast cancer. Biomed Pharmacother. 2018;108:1415–24.
Gyamfi J, Eom M, Koo JS, Choi J. Multifaceted roles of interleukin-6 in adipocyte-breast cancer cell interaction. Transl Oncol. 2018;11(2):275–85.
Walter M, Liang S, Ghosh S, Hornsby PJ, Li R. Interleukin 6 secreted from adipose stromal cells promotes migration and invasion of breast cancer cells. Oncogene. 2009;28(30):2745–55.
Benoy I, Salgado R, Colpaert C, Weytjens R, Vermeulen PB, Dirix LY. Serum interleukin 6, plasma VEGF, serum VEGF, and VEGF platelet load in breast cancer patients. Clin Breast Cancer. 2002;2(4):311–5.
Conze D, Weiss L, Regen PS, Bhushan A, Weaver D, Johnson P, et al. Autocrine production of interleukin 6 causes multidrug resistance in breast cancer cells. Cancer Res. 2001;61(24):8851–8.
Guo Y, Xu F, Lu T, Duan Z, Zhang Z. Interleukin-6 signaling pathway in targeted therapy for cancer. Cancer Treat Rev. 2012;38(7):904–10.
Gao Y, Chen X, He Q, Gimple RC, Liao Y, Wang L, et al. Adipocytes promote breast tumorigenesis through TAZ-dependent secretion of Resistin. Proc Natl Acad Sci USA. 2020;117(52):33295–304.
Li L, Geng J, Yu W, Zhou F, Zheng Z, Fu K, et al. Inhibition of PPARgamma by BZ26, a GW9662 derivate, attenuated obesity-related breast cancer progression by inhibiting the reprogramming of mature adipocytes into to cancer associate adipocyte-like cells. Front Pharmacol. 2023;14:1205030.
Watzling M, Klaus L, Weidemeier T, Horder H, Ebert R, Blunk T, et al. Three-dimensional breast cancer model to investigate CCL5/CCR1 expression mediated by direct contact between breast cancer cells and adipose-derived stromal cells or adipocytes. Cancers (Basel). 2023;15(13):3501.
Tang Z, Li C, Kang B, Gao G, Li C, Zhang Z. GEPIA: a web server for cancer and normal gene expression profiling and interactive analyses. Nucleic Acids Res. 2017;45(W1):W98-102.
Faria SS, Correa LH, Heyn GS, de Sant’Ana LP, Almeida RDN, Magalhaes KG. Obesity and breast cancer: the role of crown-like structures in breast adipose tissue in tumor progression, prognosis, and therapy. J Breast Cancer. 2020;23(3):233–45.
Shin E, Koo JS. The role of adipokines and bone marrow adipocytes in breast cancer bone metastasis. Int J Mol Sci. 2020;21(14):4967.
Choe EK, Yi JW, Chai YJ, Park KJ. Upregulation of the adipokine genes ADIPOR1 and SPP1 is related to poor survival outcomes in colorectal cancer. J Surg Oncol. 2018;117(8):1833–40.
Perego S, Sansoni V, Ziemann E, Lombardi G. Another weapon against cancer and metastasis: physical-activity-dependent effects on adiposity and adipokines. Int J Mol Sci. 2021;22(4):2005.
Setrerrahmane S, Xu H. Tumor-related interleukins: old validated targets for new anti-cancer drug development. Mol Cancer. 2017;16(1):153.
Kartikasari AER, Huertas CS, Mitchell A, Plebanski M. Tumor-induced inflammatory cytokines and the emerging diagnostic devices for cancer detection and prognosis. Front Oncol. 2021;11:692142.
Duan Z, Feller AJ, Penson RT, Chabner BA, Seiden MV. Discovery of differentially expressed genes associated with paclitaxel resistance using cDNA array technology: analysis of interleukin (IL) 6, IL-8, and monocyte chemotactic protein 1 in the paclitaxel-resistant phenotype. Clin Cancer Res. 1999;5(11):3445–53.
Pu YS, Hour TC, Chuang SE, Cheng AL, Lai MK, Kuo ML. Interleukin-6 is responsible for drug resistance and anti-apoptotic effects in prostatic cancer cells. Prostate. 2004;60(2):120–9.
Wang Y, Niu XL, Qu Y, Wu J, Zhu YQ, Sun WJ, et al. Autocrine production of interleukin-6 confers cisplatin and paclitaxel resistance in ovarian cancer cells. Cancer Lett. 2010;295(1):110–23.
Chen K, Satlof L, Stoffels G, Kothapalli U, Ziluck N, Lema M, et al. Cytokine secretion in breast cancer cells—MILLIPLEX assay data. Data Brief. 2020;28:104798.
Lin J, Della-Fera MA, Baile CA. Green tea polyphenol epigallocatechin gallate inhibits adipogenesis and induces apoptosis in 3T3-L1 adipocytes. Obes Res. 2005;13(6):982–90.
Tang W, Song H, Cai W, Shen X. Real time monitoring of inhibition of adipogenesis and angiogenesis by (−)-epigallocatechin-3-gallate in 3T3-L1 adipocytes and human umbilical vein endothelial cells. Nutrients. 2015;7(10):8871–86.
Chen D, Wang Y, Wu K, Wang X. Dual effects of metformin on adipogenic differentiation of 3T3-L1 preadipocyte in AMPK-dependent and independent manners. Int J Mol Sci. 2018;19(6):1547.
Zhao Z, Wang C, Jia J, Wang Z, Li L, Deng X, et al. Regulatory network of metformin on adipogenesis determined by combining high-throughput sequencing and GEO database. Adipocyte. 2022;11(1):56–68.
Anderson NM, Simon MC. The tumor microenvironment. Curr Biol. 2020;30(16):R921–5.
Park SA, Surh YJ. Modulation of tumor microenvironment by chemopreventive natural products. Ann N Y Acad Sci. 2017;1401(1):65–74.
Mao Y, Keller ET, Garfield DH, Shen K, Wang J. Stromal cells in tumor microenvironment and breast cancer. Cancer Metastasis Rev. 2013;32(1–2):303–15.
Orimo A, Gupta PB, Sgroi DC, Arenzana-Seisdedos F, Delaunay T, Naeem R, et al. Stromal fibroblasts present in invasive human breast carcinomas promote tumor growth and angiogenesis through elevated SDF-1/CXCL12 secretion. Cell. 2005;121(3):335–48.
Avagliano A, Fiume G, Ruocco MR, Martucci N, Vecchio E, Insabato L, et al. Influence of fibroblasts on mammary gland development, breast cancer microenvironment remodeling, and cancer cell dissemination. Cancers (Basel). 2020;12(6):1697.
Shan G, Gu J, Zhou D, Li L, Cheng W, Wang Y, et al. Cancer-associated fibroblast-secreted exosomal miR-423-5p promotes chemotherapy resistance in prostate cancer by targeting GREM2 through the TGF-beta signaling pathway. Exp Mol Med. 2020;52(11):1809–22.
Brasier AR. The nuclear factor-kappaB-interleukin-6 signalling pathway mediating vascular inflammation. Cardiovasc Res. 2010;86(2):211–8.
Liu T, Zhang L, Joo D, Sun SC. NF-kappaB signaling in inflammation. Signal Transduct Target Ther. 2017;2:17023.
Ma B, Hottiger MO. Crosstalk between Wnt/beta-catenin and NF-kappaB signaling pathway during inflammation. Front Immunol. 2016;7:378.
Sun J, Hobert ME, Duan Y, Rao AS, He TC, Chang EB, et al. Crosstalk between NF-kappaB and beta-catenin pathways in bacterial-colonized intestinal epithelial cells. Am J Physiol Gastrointest Liver Physiol. 2005;289(1):G129–37.
Ma B, van Blitterswijk CA, Karperien M. A Wnt/beta-catenin negative feedback loop inhibits interleukin-1-induced matrix metalloproteinase expression in human articular chondrocytes. Arthritis Rheum. 2012;64(8):2589–600.
Duan Y, Liao AP, Kuppireddi S, Ye Z, Ciancio MJ, Sun J. beta-Catenin activity negatively regulates bacteria-induced inflammation. Lab Investig. 2007;87(6):613–24.
Robinson KF, Narasipura SD, Wallace J, Ritz EM, Al-Harthi L. beta-Catenin and TCFs/LEF signaling discordantly regulate IL-6 expression in astrocytes. Cell Commun Signal. 2020;18(1):93.
Edara VV, Nooka S, Proulx J, Stacy S, Ghorpade A, Borgmann K. beta-Catenin regulates wound healing and IL-6 expression in activated human astrocytes. Biomedicines. 2020;8(11):479.
de Winter TJJ, Nusse R. Running against the Wnt: how Wnt/beta-catenin suppresses adipogenesis. Front Cell Dev Biol. 2021;9:627429.
Kang S, Bennett CN, Gerin I, Rapp LA, Hankenson KD, Macdougald OA. Wnt signaling stimulates osteoblastogenesis of mesenchymal precursors by suppressing CCAAT/enhancer-binding protein alpha and peroxisome proliferator-activated receptor gamma. J Biol Chem. 2007;282(19):14515–24.
Bulaklak K, Gersbach CA. The once and future gene therapy. Nat Commun. 2020;11(1):5820.
Goncalves GAR, Paiva RMA. Gene therapy: advances, challenges and perspectives. Einstein (Sao Paulo). 2017;15(3):369–75.
Chada S, Wiederhold D, Menander KB, Sellman B, Talbott M, Nemunaitis JJ, et al. Tumor suppressor immune gene therapy to reverse immunotherapy resistance. Cancer Gene Ther. 2022;29(6):825–34.
Nemunaitis J, Clayman G, Agarwala SS, Hrushesky W, Wells JR, Moore C, et al. Biomarkers Predict p53 gene therapy efficacy in recurrent squamous cell carcinoma of the head and neck. Clin Cancer Res. 2009;15(24):7719–25.
Funding
This work was supported by the Soonchunhyang University research fund, and the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2020R1F1A1072599).
Author information
Authors and Affiliations
Contributions
JJ, NHK, and MK are involved in study conception, collection and/or assembly of data, data analysis, and interpretation. JP, DL, YK, and WG are involved in collection and/or assembly of data and data analysis. YHC is involved in statistical processing and analysis. SAP is involved in study conception and design, data interpretation, manuscript writing and editing, and financial support. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All animal experiments were performed in accordance with the guidelines for animal treatment of Soonchunhyang University. All experimental protocols in our study were conducted on protocols approved by the Institutional Animal Care and Use Committee of the Soonchunhyang University (SCH21-0009).
Consent for publication
All authors approved submission of the manuscript.
Competing interests
The authors declare that there are no competing interests associated with the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
qRT-PCR primer sequences.
Additional file 2: Fig. S1.
Effect of adipocytes-Grem2 on IL-6 expression in breast cancer cells. Each adipocyte and MTV/TM-011 cells were co-cultured for 48 h in a transwell system (upper chamber: adipocytes, bottom: MTV/TM-011). RNA was isolated from MTV/TM-011 cells and the expression of the indicated genes was analyzed by qPCR. Two-sided t-test. **, p < 0.01.
Additional file 3: Fig. S2.
A MTV/TM-011 cells were treated with each adipocyte CM, IL-6 recombinant protein (25 ng/ml) and/or Serpine1 recombinant protein (25 ng/ml) and 3D invasion analysis was performed. Scale bar = 100 µm. B The relative invasion area was measured using the Image J. Two-way ANOVA. *, p < 0.05; ***, p < 0.001; ns not significant.
Additional file 4: Fig. S3.
Number of metastatic lung tumor nodules. The average number of lung metastatic nodules in each group was confirmed through H&E-stained slides of four representative lungs from each group. Two-way ANOVA. *, p < 0.05; ns not significant.
Additional file 5: Fig. S4.
Quantification of fluorescence images for Figure 6D. Based on the expression of the corresponding DAPI, the expression levels of vimentin, slug, or twist1 were determined and analyzed in three independent tissues. Two-way ANOVA. *, p < 0.05; **, p < 0.01; ***, p < 0.001; ns not significant.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jung, J., Kim, N.H., Kwon, M. et al. The inhibitory effect of Gremlin-2 on adipogenesis suppresses breast cancer cell growth and metastasis. Breast Cancer Res 25, 128 (2023). https://doi.org/10.1186/s13058-023-01732-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13058-023-01732-2