Abstract
Background
The PI3K/AKT/mTORC1 axis is implicated in hormone receptor-positive HER2-negative metastatic breast cancer (HR+ HER2− mBC) resistance to anti-estrogen treatments. Based on results of the BOLERO-2 trial, the mTORC1 inhibitor everolimus in combination with the steroidal aromatase inhibitor (AI) exemestane has become a standard treatment for patients with HR+ HER2− mBC resistant to prior non-steroidal AI therapy. In the recent SOLAR-1 trial, the inhibitor of the PI3K alpha subunit (p110α) alpelisib in combination with fulvestrant prolonged progression-free survival (PFS) when compared to fulvestrant alone in patients with PIK3CA-mutated HR+ HER2− mBC that progressed after/on previous AI treatment. Therefore, two different molecules targeting the PI3K/AKT/mTORC1 axis, namely everolimus and alpelisib, are available for patients progressing on/after previous AI treatment, but it is unclear how to optimize their use in the clinical practice.
Main body of the abstract
Here, we reviewed the available clinical evidence deriving from the BOLERO-2 and SOLAR-1 trials to compare efficacy and safety profiles of everolimus and alpelisib in advanced HR+ HER2− BC treatment. Adding either compound to standard endocrine therapy provided similar absolute and relative PFS advantage. In the SOLAR-1 trial, a 76% incidence of grade (G) 3 or 4 (G3/G4) adverse events was reported, while G3/G4 toxicities occurred in 42% of patients in the BOLERO-2 trial. While alpelisib was only effective in patients with PIK3CA-mutated neoplasms, retrospective analyses indicate that everolimus improves exemestane efficacy independently of PIK3CA mutational status.
Conclusions
Based on the available efficacy and safety data, the “new” alpelisib may be burdened by higher incidence of severe adverse events, higher costs, and anticancer efficacy that is limited to PIK3CA-mutated tumors when compared to the “old” everolimus. Therefore, the everolimus-exemestane combination remains an effective and reasonably well-tolerated therapeutic option for HR+ HER2− mBC patients progressing after/on previous AI treatment, independently of PIK3CA mutational status.
Similar content being viewed by others
Background
Endocrine therapy (ET) is the mainstay of treatment for patients with hormone receptor-positive (HR+) human epidermal growth factor receptor 2-negative (HER2−) metastatic breast cancer (mBC) [1]. However, tumors initially responding to ET, including the most recent ET-Cyclin-Dependent Kinase 4/6 (CDK4/6) inhibitor combinations, almost invariably develop resistance [2,3,4]. Hence, the identification of targeted therapies that are able to revert or delay endocrine resistance is a clinically relevant issue.
Aberrant signaling through the phosphatidylinositol 3-kinase/protein kinase B (AKT)/mechanistic target of rapamycin complex 1 (PI3K/AKT/mTORC1) cascade is clearly implicated in endocrine resistance, thus providing the rationale for combining inhibitors of this pathway with currently available ET [5,6,7]. Based on the results of the BOLERO-2 trial, the mTORC1 inhibitor everolimus (Eve) has been approved in combination with the aromatase inhibitor (AI) exemestane (Exe) for the treatment of HR+ HER2− mBC progressing on/after one line of non-steroidal aromatase inhibitor (NSAI) treatment [8]. More recently, the PI3Kα-specific inhibitor alpelisib (Alp) plus fulvestrant (Fulv) combination significantly prolonged progression-free survival (PFS) when compared to Fulv alone in patients with PIK3CA-mutated HR+ HER2− mBC, thus leading to FDA registration of Alp in this clinical setting [9]. Based on results of the SOLAR-1 study, Alp is increasingly considered by treating physicians and experts in the field as a candidate to replace Eve in HR+ HER2− mBC treatment [10].
Here, we review data from prospective trials to compare the antitumor efficacy and safety profile of Eve/ET and Alp/ET combinations in women with HR+ HER2− mBC. We also discuss how Alp and Eve could fit in the future treatment scenario of mBC.
Main text
The biology of the PI3K/AKT/mTORC1 axis
The insulin receptor (IR)/PI3K/AKT/mTORC1 pathway is the most commonly dysregulated pathway in human cancers and plays a crucial role in stimulating tumor cell metabolism, growth, proliferation, and motility [11]. PI3Ks include three classes of kinases with different structural properties and biological functions. Among different PI3Ks, class I PI3Ks, which include class IA (p110α, p110β, and p110δ) and class IB (p110γ) PI3Ks, have been found to be more commonly dysregulated in human cancers [11]. Enhanced activation of the IR/PI3K/AKT/mTORC1 axis can result from (a) increased extracellular concentration of growth factors activating oncogenic receptor tyrosine kinases (RTKs), such as IR or insulin-like growth factor 1 (IGF-1) receptor (IGF1R), on cell plasma membranes [12]; (b) activating mutations or overexpression of RTKs, including members of the HER family for class IA PI3Ks, or G protein-coupled receptors (GPCR) for class IB PI3Ks [13]; and (c) activating mutations or overexpression of downstream kinases, such as PI3K subunits, AKT and mTORC1, or inactivation of the phosphatase and tensin homolog deleted from chromosome 10 (PTEN), tuberous sclerosis complex 1/2 (TSC1/2), or liver kinase B1 (LKB1) tumor suppressor proteins [11].
Once activated by upstream signals, the PI3K regulatory subunit p85α binds to the phospho-tyrosine residues on receptor protein kinases or adaptor proteins, such as insulin receptor substrate 1 (IRS1), and unleashes the PI3K catalytic subunit p110α (encoded by the PIK3CA gene), which is enabled to phosphorylate phosphatidylinositol 4,5-bisphosphate (PIP2) to phosphatidylinositol 3,4,5-triphosphate (PIP3) (Fig. 1) [14, 15]. On the other hand, mutated (i.e., constitutively active) PI3K subunits catalyze PIP3 biosynthesis independently of upstream signals; in particular, mutations of the PIK3CA gene are found in approximately 40% of HR+ HER2− BCs and cause constitutive PI3K activation [16, 17]. Once synthesized, PIP3 anchors the serine/threonine AKT kinase to the cell plasma membrane, where it activates mTORC1, either directly or through the inhibition of TSC1/TSC2 [11, 13, 17]. In turn, mTORC1 stimulates cell growth and proliferation by triggering protein translation initiation through phosphorylating eIF4E-binding proteins (4E-BPs) and S6 kinases (S6K1 and S6K2). mTORC1 also inhibits autophagy and stimulates lipogenesis via intermediate lipogenic transcriptional factors and mitochondrial biogenesis (Fig. 1). Overall, mTORC1 activation induces a global metabolic response leading to the stimulation of anabolic processes and macromolecule biosynthesis [18, 19].
In parallel with mTORC1 activation, constitutively active PI3K stimulates several biological processes that stimulate tumor cell proliferation, such as the Mitogen Activated Protein Kinase (MAPK) and estrogen receptor α (ERα) pathways [20], as well as the reprogramming of glucose and lipid metabolism via AKT activation and AMPK inhibition (Fig. 1) [15, 21].
Tumor suppressor enzymes prevent uncontrolled activation of the PI3K/AKT/mTORC1 cascade at different levels: among them, PTEN counteracts PI3K activity by dephosphorylating PIP3 to PIP2, while LKB1 indirectly inhibits mTORC1 via AMP-activated protein kinase (AMPK)-mediated activation of TSC1/2 [22, 23].
Notably, the PI3K/AKT/mTORC1 pathway is aberrantly activated in approximately 70% of BCs as a result of increased extracellular concentration of growth factors, activating mutations of genes encoding RTKs (e.g., IGFR1 and fibroblast growth factor receptor 1 [FGFR1]) or downstream oncogenes (e.g., PI3KCA or AKT), or, finally, loss-of-function or reduced levels of PTEN, LKB1, or inositol polyphosphate 4-phosphatase type II (INPP4B) tumor suppressor proteins [24, 25]. Among these alterations, PIK3CA mutations are by far the most common ones [16]. Oncogenic PIK3CA mutations include the following: the kinase domain H1047R mutation (exon 20), which results in higher binding affinity of PI3K to the plasma membrane and to PIP2; the helical domain E542K and E545K mutations (exon 9), which enable the direct interaction of PI3K catalytic subunit with IRS1 independently of p85 and IRS1 phosphorylation; and deletions in the C2 domain, which unleash inhibitory contacts with regulatory subunits [13, 14].
Alp selectively binds to and inhibits p110α, while Eve inhibits mTORC1 downstream of PI3K through allosteric binding. When used in in vitro models of HR+ HER2− BC, both PI3K and mTORC1 inhibitors demonstrated synergistic anticancer activity in combination with anti-estrogens. For instance, HR+ BC cells treated with letrozole (Let) plus Eve accumulate in the G1 phase of the cell cycle and undergo proliferation inhibition and apoptosis [26, 27]. Moreover, the mTORC1 inhibitor rapamycin reverts resistance to Fulv or tamoxifen (TAM) in HR+ BC cell lines, both alone and in combination with ET [27]. Finally, inhibitors of p110α and/or p110β showed synthetic lethal effects when combined with different ETs [5, 28, 29]. Mechanistically, these synergistic effects are the result of a crosstalk between the PI3K/AKT/mTORC1 and ER signaling pathways. One of mTORC1 targets, S6K1, is responsible for N-terminal ERα Activation Function 1 (AF1) domain phosphorylation on Serine167, thus leading to its ligand-independent transactivation [20]. Therefore, S6K-induced, ligand-independent activation of ERα can induce HR+ BC resistance to ET, thus providing strong preclinical rationale for combining PI3K/AKT/mTORC1 pathway inhibitors with ET to prevent/revert endocrine resistance.
Since Eve inhibits the PI3K/AKT/mTORC1 cascade downstream of PI3K, its antitumor activity should be independent of PIK3CA mutational status. Conversely, Alp selectively inhibits proliferation of PI3Kα-driven HR+ HER2− BC cells and causes regression of PIK3CA-mutated in vivo tumor models [6, 28]. Therefore, PIK3CA-mutated tumors are the best candidates to respond to Alp [30].
BOLERO-2 and SOLAR-1 trials: a comparison of efficacy and safety data
The BOLERO-2 and SOLAR-1 studies are the two randomized trials leading to Eve and Alp registration for HR+ HER2− mBC treatment in combination with standard ET. The main clinical and tumor characteristics of patients enrolled in the BOLERO-2 and SOLAR-1 (only PIK3CA-mutated cohort) trials are summarized in Table 1.
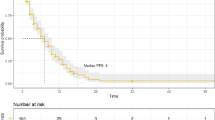
The BOLERO-2 was a double-blind, phase III study that investigated the efficacy of the Eve/Exe combination in HR+ HER2− mBC postmenopausal women previously treated with NSAIs [8]. Patients (n = 724) enrolled in the trial were randomized in a 2:1 ratio to receive Eve/Exe or placebo/Exe. The primary endpoint was PFS; secondary endpoints were overall survival (OS), overall response rate (ORR), and safety. Median PFS was 11.0 months in the experimental arm versus (vs.) 4.1 months in the control arm (hazard ratio [HR] 0.38; 95% confidence interval [CI] 0.31–0.48; p < 0.0001; Table 2), with an ORR of 12.6% vs. 2.1%, respectively [31]. No significant differences in terms of OS were observed between Eve/Exe and placebo/Exe (median 31.0 months vs. 26.6 months, respectively; HR 0.89; 95% CI 0.73–1.10; p = 0.14) [32]. As for the safety profile, severe (G3/G4) AEs occurred in 33% and 9% of patients receiving the experimental or standard treatment, respectively, with stomatitis (8% vs. < 1%), anemia (6% vs. < 1%), dyspnea (4% vs. 1%), hyperglycemia (6% vs. 1%), fatigue (5% vs. 1%), and pneumonitis (4% vs. 0%) being the most common ones [8, 33] (Table 3). Median duration of Eve treatment was 5.5 months, with the main cause of therapy discontinuation being disease progression (61.9% vs. 88.7% in the Eve and control arms, respectively), followed by AEs (26.3% vs. 5%, respectively). Notably, next-generation sequencing (NGS) analysis performed in archival tumor specimens from a subgroup (n = 302) of patients enrolled in the BOLERO-2 trial showed that Eve provides clinical benefit to patients with both PIK3CA-wild type (wt) (HR 0.37; 95% CI 0.25–0.55) and PIK3CA-mutated (HR 0.51; 95% CI 0.34–0.77) tumors [34].
The SOLAR-1 study was a double-blind, phase III trial that randomized 571 postmenopausal women (n = 571; 99.83%) or men (n = 1; 0.17%) previously treated with an AI to receive Alp plus Fulv or placebo plus Fulv [9]. The determination of PIK3CA gene mutational status in tumor tissue specimens was mandatory before patient enrollment. Indeed, based on PIK3CA status (mutated vs. wt), patients were assigned to two different cohorts; then, they were randomized in a 1:1 ratio to receive the experimental (Alp/Fulv) or standard (placebo/Fulv) treatment. The primary endpoint of the SOLAR-1 trial was PFS in the cohort of PIK3CA-mutated patients, i.e., those patients with the highest chances to benefit from the experimental treatment based on previous preclinical and clinical studies [30, 35]. Secondary endpoints included OS in the cohort of patients with PIK3CA-mutated tumors, PFS and OS in the PIK3CA-wt cohort, ORR, clinical benefit, and treatment safety in the whole patient population. Notably, less than 7% of patients in all treatment arms had received previous treatment with CDK4/6 inhibitors. After a median follow-up of 20 months, median PFS for patients in the PIK3CA-mutated cohort was 11 months in the experimental arm vs. 5.7 months in the control arm (HR 0.65; 95% CI 0.50–0.85; p < 0.0001 Table 2), with an ORR of 26.6% and 12.8%, respectively. In the cohort of patients with PIK3CA-wt tumors, the experimental treatment was associated with a non-significant difference in terms of median PFS (7.4 vs. 5.6 months, respectively; HR 0.85; 95% CI 0.58–1.25). G3 and G4 AEs occurred in 64.4% and 11.6%, respectively, of Alp/Fulv-treated patients, and in 30.3% and 5.2%, respectively, of placebo/Fulv-treated subjects. The most common G3/G4 AEs in the experimental arm were hyperglycemia (36.6%), rash (9.9%), and diarrhea (6.7%). With a median duration of exposure to Alp of 5.5 months, the most frequent reasons of treatment discontinuation were disease progression (55% vs. 68% in the Alp/Fulv and placebo/Fulv groups, respectively) and the occurrence of AEs (25% vs. 4.2%, respectively), with hyperglycemia and rash being the most common AEs leading to permanent treatment discontinuation (Table 3). Regarding Alp-induced hyperglycemia, patients with fasting plasma glucose levels equal to 140 mg/dl or higher than 140 mg/dl received metformin as per SOLAR-1 protocol. Therefore, metformin administration was started before patients developed grade 3 or 4 hyperglycemia (fasting plasma glucose levels > 250 mg/dl) in most of the cases. Despite this practice, the incidence of severe hyperglycemia in Alp-treated patients was 36.6%, and it reasonable to speculate that it might have been even superior without the precocious administration of metformin [36].
Even if the BOLERO-2 and SOLAR-1 trials enrolled patients with overall similar characteristics at baseline (Table 1), some differences need to be highlighted: (a) the BOLERO-2 trial enrolled patients with ECOG PS of 0–2, while the SOLAR-1 trial only enrolled patients with an ECOG PS of 0–1; (b) patients with previously treated and stable brain metastases were included in the SOLAR-1, but not in the BOLERO-2 trial; (c) enrollment of male patients was allowed in the SOLAR-1, but not in the BOLERO-2 trial; however, only one male patient was finally enrolled in the SOLAR-1 study; (d) patients with type 1 or uncontrolled type 2 diabetes mellitus were excluded from the SOLAR-1 but not from the BOLERO-2 trial; (e) a higher percentage of patients in the SOLAR-1 trial (52.1% in the PIK3CA-mutated cohort) received Alp/Fulv as their first-line treatment for advanced disease when compared to patients treated with Eve/Exe in the BOLERO-2 study (20.6%) [37]; (f) 26% of patients treated with Eve/Exe in the BOLERO-2 trial had received previous chemotherapy for the treatment of advanced disease, whereas these patients were excluded from the SOLAR-1 study; (g) 11.8% of patients with PIK3CA-mutated tumors treated with Alp/Fulv in the SOLAR-1 trial had endocrine-sensitive disease, which was an exclusion criterion in the BOLERO-2 trial; and (h) the type of ET combined with the experimental drug was different in the two studies (Exe and Fulv, respectively).
Except for the inclusion of patients with brain metastases, the SOLAR-1 trial enrolled a more selected population of HR+ HER2− mBC patients with less pretreated and potentially more endocrine-sensitive disease. This could at least in part explain the longer PFS observed in patients in the control arm of the SOLAR-1 trial (5.7 months) when compared to patients in the control arm of the BOLERO-2 study (4.1 months in the overall population; 2.8 months in a subgroup of patients with PIK3CA-mutated tumors [34]). Despite these differences, the absolute PFS advantage provided by the addition of Eve or Alp to standard ET was similar (6.9 and 5.3 months, respectively, when considering the whole population of patients enrolled in the BOLERO-2 trial and patients with PIK3CA-mutated neoplasms in the SOLAR-1 study; 3.9 and 5.3 months, respectively, when considering only patients with PIK3CA-mutated tumors in both studies). The relative PFS advantage associated with Eve (HR 0.36) was higher than the relative benefit associated with Alp (HR 0.65) when considering all patients enrolled in the BOLERO-2 trial, while it was similar in subgroups of patients with PIK3CA-mutated tumors (0.51 and 0.65, respectively) [34]. The rate of treatment discontinuation was high in both studies (about 25%), but the incidence of G3/G4 AEs was considerably higher in both the treatment (76% vs. 42%, respectively) and control (35.5% vs. 9%, respectively) arm of the SOLAR-1 trial.
Other prospective studies investigating Eve or Alp
After the publication of the BOLERO-2 study, other prospective phase IIIb–IV trials (4EVER [38], BRAWO [39], STEPAUT [40], BALLET [41], EVEREXES [42]) investigated the efficacy and tolerability of Eve/Exe in more heterogeneous patient cohorts when compared to patients enrolled in the BOLERO-2 trial (Table 4) [8]. In particular, the 4EVER, BRAWO, and BALLET studies enrolled patients independently of the number of previous chemotherapy lines for advanced disease, as well as of previous Exe treatment, thus more faithfully recapitulating patients treated in the real-world clinical practice [38, 39, 41]. For instance, 60% and 53.7% of patients in the BALLET and 4EVER studies, respectively, had received previous chemotherapy for advanced disease when compared to 26% of patients in the BOLERO-2 study. Nonetheless, activity and efficacy data from these studies were similar to those from the BOLERO-2 trial, with ORR ranging from 8.2% (BRAWO) to 15.8% (EVEREXES), and mPFS ranging from 5.6 months (4EVER) to 9.5 months (STEPAUT, EVEREXES). The safety profile of Eve/Exe was also consistent with data from the BOLERO-2 study, with the most commonly observed G3/G4 toxicities being stomatitis (range 3.9–10.6%), dyspnea (range 2–4.7%), asthenia/fatigue (range 1.5–3.6%), and hyperglycemia (range 2.9–7%). Treatment discontinuation rates due to AEs ranged from 17.1% (BALLET) to 26% (BRAWO). While the safety profile of Eve/Exe in elderly patients (> 70 years) in the BALLET study was overall similar to that observed in the BOLERO-2 trial, incidence of G3/G4 AEs, dose reductions/interruptions, and treatment discontinuations due to AEs were higher in the elderly vs. non-elderly population [41].
Altogether, real-world data corroborate the efficacy of Eve in combination with ET for the treatment of HR+ HER2− mBC. Subgroup analyses of these studies indicate that ORR and PFS may be lower in patients treated with a higher number of previous therapy lines, with previous exposure to chemotherapy, or treated with lower Eve treatment intensity [38,39,40]. Finally, no ORR or PFS differences have been described based on prior treatment with Exe [38]. Of note, the introduction of prophylactic dexamethasone oral solution for the prevention or management of Eve-induced stomatitis has remarkably improved the safety profile of Eve through reducing one of the most common and disturbing toxicities related to the use of this compound [50].
More recently, the phase II BOLERO-4 study evaluated Eve plus Let as a first-line treatment in 202 postmenopausal women with HR+ HER2 mBC, who received second-line Eve/Exe on progression. First-line Eve/Let was associated with mPFS of 22.0 months (95% CI 18.1–25.1), while mOS was not reached. Of note, mPFS was 3.7 months (95% CI 1.9–7.4 months) with second-line Eve/Exe treatment (50 patients) [43]. While these data indicate that Eve/Let is an effective first-line combination treatment, they also show that Eve continuation after disease progression is a poorly effective therapeutic strategy. Other phase II studies evaluating Eve in combination with Let, Fulv, Exe, or TAM in patients with mBC progressing on/after prior NSAI therapy showed interesting activity and efficacy, in the absence of relevant unforetold toxicities [44,45,46,47,48,49].
As for Alp, small prospective trials published before the SOLAR-1 study evaluated the Let/Alp or Fulv/Alp combinations in patients with HR+ HER2− mBC progressing after previous ET. Consistent with SOLAR-1 results, these studies reported an incidence of G3/G4 hyperglycemia and rash in the 10–38.1% and 8–27.8% ranges, respectively, with longer mPFS in patients with PIK3CA-mutated neoplasms (Table 5) [30, 35, 51].
Discussion
The recent registration of the Alp/Fulv combination for the treatment of PIK3CA-mutated HR+ HER2− mBC has been considered a biologically and clinically relevant advancement [10]. Indeed, Alp is the first compound that provided clinically meaningful benefit in a subgroup of HR+ HER2− mBC patients that can be identified on the basis of a specific genetic tumor biomarker.
Based on the comparison of efficacy and safety results of the BOLERO-2 and the SOLAR-1 studies, Eve or Alp in combination with standard ET provide similar PFS benefit when compared to ET alone; however, Alp/Fulv is associated with overall higher incidence of G3/G4 AEs despite the fact that patients in the SOLAR-1 trial had more favorable clinical characteristics, including better ECOG PS, absence of uncontrolled diabetes mellitus at enrollment, and the fact that metformin was administered as per protocol if fasting blood glucose concentration was 140 mg/dl or higher [36]. The toxicity profiles of Eve and Alp, which are partially non-overlapping, indicate that ongoing or future trials aiming to combine these compounds may result in exaggerated incidence of AEs, unless dosages of both drugs are reduced (NCT02077933).
Another crucial difference between Eve and Alp consists in the fact that patients with both PIK3CA-mutated and PIK3CA-wt tumors benefit from adding Eve to ET, while Alp selectively benefits patients with PIK3CA-mutated tumors, which account for approximately 40% of the HR+ HER2− BCs [16]. From a biological point of view, this is expected because Eve inhibits the PI3K/AKT/mTORC1 axis downstream of PI3K, i.e., independently of PIK3CA mutations or other PI3K/AKT/mTORC1 activating mechanisms. From a clinical point of view, this implies that Alp is not effective in about 60% of all HR+ HER2− mBC patients (i.e., those with PIK3CA-wt disease). On the other hand, Eve and Alp may provide similar relative PFS advantage in patients with PIK3CA-mutated neoplasms [30, 34]; however, this hypothesis derives from a NGS subanalysis of the BOLERO-2 trial and should be confirmed in prospective studies directly comparing Eve and Alp in patients with PIK3CA-mutated HR+ HER2− mBC.
Although indirect comparisons between independent trials cannot be used to draw definitive conclusions about different therapeutic approaches, and since no head-to-head trials can be expected soon, the available clinical evidence indicates that the “new” and more expensive Alp might be more toxic than the “old” Eve and has less broad clinical effectiveness (i.e., limited to patients with PIK3CA-mutated disease). For these reasons, the raising enthusiasm around Alp as a potential substitute of Eve in HR+ HER2− mBC treatment is not fully justified. The Eve/Exe combination remains a valid, and in many cases preferable (e.g., PIK3CA-wt neoplasms, or in diabetic or malnourished patients), treatment option for HR+ HER2− mBC patients undergoing disease progression on/after prior AI therapy.
Further clinical studies are needed to compare the efficacy and safety profile of Eve and Alp in HR+ HER2− mBC patients progressing on/after ET-CDK4/6 inhibitor treatment, which now represents the standard first- or second-line treatment in this clinical setting [2,3,4, 52,53,54]. In this clinical setting, the Eve/Exe combination and fulvestrant monotherapy remain two valid treatment options for patients with PIK3CA-wt neoplasms, while patients with PIK3CA-mutated neoplasms could potentially benefit from either fulvestrant/Alp or Eve/Exe. However, in the absence of clinical evidence, it is difficult to make clear clinical recommendations about the most effective second-line therapy in patients with PIK3CA-mutated or PIK3CA-wt tumors progressing on prior ET plus CDK 4/6 inhibitor-containing therapy. In patients with PIK3CA-mutated neoplasms, the sequential use of Eve and Alp in different treatment lines also deserves clinical investigation, at least in patients with PIK3CA-mutated disease; indeed, in the proof-of-concept phase III BELLE-3 trial, the pan-class I PI3K inhibitor buparlisib improved PFS when compared to the placebo in patients undergoing disease progression after prior Eve treatment, with an HR of 0.50 in the subgroup of PIK3CA-mutated neoplasms [55].
Conclusions
When compared to the “old” everolimus, the “new” alpelisib may be burdened by higher incidence of severe adverse events, more narrow anticancer activity, and also higher costs after the approval of generic everolimus tablets (https://www.patient.novartisoncology.com/piqray-cost/; fda.gov/drugs/generic-drugs/overview-basics). The everolimus-exemestane combination remains an effective and reasonably well-tolerated second-line therapeutic option after progression to first-line AI plus/minus CDK 4/6 inhibitor treatment in HR+ HER2− mBC patients with PIK3CA-wt disease, as well as in patients with PIK3CA-mutated neoplasms who have contraindications to alpelisib, or those experiencing severe AEs during alpelisib/fulvestrant therapy.
Availability of data and materials
All data generated or analyzed during this study are included in this published article (and its supplementary information files).
Abbreviations
- AE:
-
Adverse event
- AI:
-
Aromatase inhibitor
- Alp:
-
Alpelisib
- AMPK:
-
AMP-activated protein kinase
- CDK 4/6:
-
Cyclin-Dependent Kinase 4/6
- CI:
-
Confidence interval
- ER:
-
Estrogen receptor
- ET:
-
Endocrine therapy
- Eve:
-
Everolimus
- FGFR1:
-
Fibroblast growth factor receptor 1
- Fulv:
-
Fulvestrant
- GPCR:
-
G protein-coupled receptor
- HER2:
-
Human epidermal growth factor receptor 2
- HR:
-
Hazard ratio
- HR+:
-
Hormone receptor-positive
- IGF-1:
-
Insulin-like growth factor 1
- INPP4B:
-
Inositol polyphosphate 4-phosphatase type II (INPP4B)
- IR:
-
Insulin receptor
- IRS1:
-
Insulin receptor substrate 1
- LKB1:
-
Liver kinase B1
- mBC:
-
Metastatic breast cancer
- mPFS:
-
Median progression-free survival
- mTORC1:
-
Mammalian target of rapamycin complex 1
- NSAI:
-
Non-steroidal aromatase inhibitor
- ORR:
-
Overall response rate
- OS:
-
Overall survival
- PI3K:
-
Phosphoinositide 3-kinase
- PIP2:
-
Phosphatidylinositol 4,5-bisphosphate
- PIP3:
-
Phosphatidylinositol 3,4,5-triphosphate
- PETN:
-
Phosphatase and tensin homolog deleted from chromosome 10
- S6K:
-
S6 kinase
- TSC 1/2:
-
Tuberous sclerosis complex 1/2
- 4E-BP1:
-
eIF4E-binding proteins
References
Harbeck N, Gnant M. Breast cancer. Lancet. 2017;389(10074):1134–50.
Finn RS, Martin M, Rugo HS, Jones S, Im SA, Gelmon K, Harbeck N, Lipatov ON, Walshe JM, Moulder S, et al. Palbociclib and letrozole in advanced breast cancer. N Engl J Med. 2016;375(20):1925–36.
Hortobagyi GN, Stemmer SM, Burris HA, Yap YS, Sonke GS, Paluch-Shimon S, Campone M, Blackwell KL, Andre F, Winer EP, et al. Ribociclib as first-line therapy for HR-positive, advanced breast cancer. N Engl J Med. 2016;375(18):1738–48.
Goetz MP, Toi M, Campone M, Sohn J, Paluch-Shimon S, Huober J, Park IH, Tredan O, Chen SC, Manso L, et al. MONARCH 3: abemaciclib as initial therapy for advanced breast cancer. J Clin Oncol. 2017;35(32):3638–46.
Crowder RJ, Phommaly C, Tao Y, Hoog J, Luo J, Perou CM, Parker JS, Miller MA, Huntsman DG, Lin L, et al. PIK3CA and PIK3CB inhibition produce synthetic lethality when combined with estrogen deprivation in estrogen receptor-positive breast cancer. Cancer Res. 2009;69(9):3955–62.
Miller TW, Hennessy BT, Gonzalez-Angulo AM, Fox EM, Mills GB, Chen H, Higham C, Garcia-Echeverria C, Shyr Y, Arteaga CL. Hyperactivation of phosphatidylinositol-3 kinase promotes escape from hormone dependence in estrogen receptor-positive human breast cancer. J Clin Invest. 2010;120(7):2406–13.
Miller TW, Balko JM, Arteaga CL. Phosphatidylinositol 3-kinase and antiestrogen resistance in breast cancer. J Clin Oncol. 2011;29(33):4452–61.
Baselga J, Campone M, Piccart M, Burris HA 3rd, Rugo HS, Sahmoud T, Noguchi S, Gnant M, Pritchard KI, Lebrun F, et al. Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer. N Engl J Med. 2012;366(6):520–9.
Andre F, Ciruelos E, Rubovszky G, Campone M, Loibl S, Rugo HS, Iwata H, Conte P, Mayer IA, Kaufman B, et al. Alpelisib for PIK3CA-mutated, hormone receptor-positive advanced breast cancer. N Engl J Med. 2019;380(20):1929–40.
Stirrups R. Alpelisib plus fulvestrant for PIK3CA-mutated breast cancer. Lancet Oncol. 2019;20(7):e347.
Janku F, Yap TA, Meric-Bernstam F. Targeting the PI3K pathway in cancer: are we making headway? Nat Rev Clin Oncol. 2018;15(5):273–91.
Pollak M. Insulin and insulin-like growth factor signalling in neoplasia. Nat Rev Cancer. 2008;8(12):915–28.
Baselga J. Targeting the phosphoinositide-3 (PI3) kinase pathway in breast cancer. Oncologist. 2011;16(Suppl 1):12–9.
Hanker AB, Kaklamani V, Arteaga CL. Challenges for the clinical development of PI3K inhibitors: strategies to improve their impact in solid tumors. Cancer Discov. 2019;9(4):482–91.
Fruman DA, Chiu H, Hopkins BD, Bagrodia S, Cantley LC, Abraham RT. The PI3K pathway in human disease. Cell. 2017;170(4):605–35.
Cancer Genome Atlas N. Comprehensive molecular portraits of human breast tumours. Nature. 2012;490(7418):61–70.
Goncalves MD, Hopkins BD, Cantley LC. Phosphatidylinositol 3-kinase, growth disorders, and cancer. N Engl J Med. 2018;379(21):2052–62.
Dowling RJ, Topisirovic I, Fonseca BD, Sonenberg N. Dissecting the role of mTOR: lessons from mTOR inhibitors. Biochim Biophys Acta. 2010;1804(3):433–9.
Kim J, Guan KL. mTOR as a central hub of nutrient signalling and cell growth. Nat Cell Biol. 2019;21(1):63–71.
Yamnik RL, Holz MK. mTOR/S6K1 and MAPK/RSK signaling pathways coordinately regulate estrogen receptor alpha serine 167 phosphorylation. FEBS Lett. 2010;584(1):124–8.
Vernieri C, Casola S, Foiani M, Pietrantonio F, de Braud F, Longo V. Targeting cancer metabolism: dietary and pharmacologic interventions. Cancer Discov. 2016;6(12):1315–33.
Hosford SR, Dillon LM, Bouley SJ, Rosati R, Yang W, Chen VS, Demidenko E, Morra RP Jr, Miller TW. Combined inhibition of both p110alpha and p110beta isoforms of phosphatidylinositol 3-kinase is required for sustained therapeutic effect in PTEN-deficient, ER(+) breast cancer. Clin Cancer Res. 2017;23(11):2795–805.
Andrade-Vieira R, Goguen D, Bentley HA, Bowen CV, Marignani PA. Pre-clinical study of drug combinations that reduce breast cancer burden due to aberrant mTOR and metabolism promoted by LKB1 loss. Oncotarget. 2014;5(24):12738–52.
Rodon J, Tabernero J. Improving the armamentarium of PI3K inhibitors with isoform-selective agents: a new light in the darkness. Cancer Discov. 2017;7(7):666–9.
Hopkins BD, Pauli C, Du X, Wang DG, Li X, Wu D, Amadiume SC, Goncalves MD, Hodakoski C, Lundquist MR, et al. Suppression of insulin feedback enhances the efficacy of PI3K inhibitors. Nature. 2018;560(7719):499–503.
Boulay A, Rudloff J, Ye J, Zumstein-Mecker S, O'Reilly T, Evans DB, Chen S, Lane HA. Dual inhibition of mTOR and estrogen receptor signaling in vitro induces cell death in models of breast cancer. Clin Cancer Res. 2005;11(14):5319–28.
Ghayad SE, Bieche I, Vendrell JA, Keime C, Lidereau R, Dumontet C, Cohen PA. mTOR inhibition reverses acquired endocrine therapy resistance of breast cancer cells at the cell proliferation and gene-expression levels. Cancer Sci. 2008;99(10):1992–2003.
Bosch A, Li Z, Bergamaschi A, Ellis H, Toska E, Prat A, Tao JJ, Spratt DE, Viola-Villegas NT, Castel P, et al. PI3K inhibition results in enhanced estrogen receptor function and dependence in hormone receptor-positive breast cancer. Sci Transl Med. 2015;7(283):283ra251.
Chen IC, Hsiao LP, Huang IW, Yu HC, Yeh LC, Lin CH, Wei-Wu Chen T, Cheng AL, Lu YS. Phosphatidylinositol-3 kinase inhibitors, buparlisib and alpelisib, sensitize estrogen receptor-positive breast cancer cells to tamoxifen. Sci Rep. 2017;7(1):9842.
Juric D, Janku F, Rodon J, Burris HA, Mayer IA, Schuler M, Seggewiss-Bernhardt R, Gil-Martin M, Middleton MR, Baselga J, et al. Alpelisib plus fulvestrant in PIK3CA-altered and PIK3CA-wild-type estrogen receptor-positive advanced breast cancer: a phase 1b clinical trial. JAMA Oncol. 2019:5(2):e184475e184475.
Yardley DA, Noguchi S, Pritchard KI, Burris HA 3rd, Baselga J, Gnant M, Hortobagyi GN, Campone M, Pistilli B, Piccart M, et al. Everolimus plus exemestane in postmenopausal patients with HR(+) breast cancer: BOLERO-2 final progression-free survival analysis. Adv Ther. 2013;30(10):870–84.
Piccart M, Hortobagyi GN, Campone M, Pritchard KI, Lebrun F, Ito Y, Noguchi S, Perez A, Rugo HS, Deleu I, et al. Everolimus plus exemestane for hormone-receptor-positive, human epidermal growth factor receptor-2-negative advanced breast cancer: overall survival results from BOLERO-2dagger. Ann Oncol. 2014;25(12):2357–62.
Rugo HS, Pritchard KI, Gnant M, Noguchi S, Piccart M, Hortobagyi G, Baselga J, Perez A, Geberth M, Csoszi T, et al. Incidence and time course of everolimus-related adverse events in postmenopausal women with hormone receptor-positive advanced breast cancer: insights from BOLERO-2. Ann Oncol. 2014;25(4):808–15.
Hortobagyi GN, Chen D, Piccart M, Rugo HS, Burris HA 3rd, Pritchard KI, Campone M, Noguchi S, Perez AT, Deleu I, et al. Correlative analysis of genetic alterations and everolimus benefit in hormone receptor-positive, human epidermal growth factor receptor 2-negative advanced breast cancer: results from BOLERO-2. J Clin Oncol. 2016;34(5):419–26.
Mayer IA, Abramson VG, Formisano L, Balko JM, Estrada MV, Sanders ME, Juric D, Solit D, Berger MF, Won HH, et al. A phase Ib study of alpelisib (BYL719), a PI3Kalpha-specific inhibitor, with letrozole in ER+/HER2- metastatic breast cancer. Clin Cancer Res. 2017;23(1):26–34.
Park J, Shin SW. Alpelisib for PIK3CA-mutated advanced breast cancer. N Engl J Med. 2019;381(7):686.
Beck JT, Hortobagyi GN, Campone M, Lebrun F, Deleu I, Rugo HS, Pistilli B, Masuda N, Hart L, Melichar B, et al. Everolimus plus exemestane as first-line therapy in HR(+), HER2(-) advanced breast cancer in BOLERO-2. Breast Cancer Res Treat. 2014;143(3):459–67.
Tesch H, Stoetzer O, Decker T, Kurbacher CM, Marme F, Schneeweiss A, Mundhenke C, Distelrath A, Fasching PA, Lux MP, et al. Efficacy and safety of everolimus plus exemestane in postmenopausal women with hormone receptor-positive, human epidermal growth factor receptor 2-negative locally advanced or metastatic breast cancer: results of the single-arm, phase IIIB 4EVER trial. Int J Cancer. 2019;144(4):877–85.
Lüftner DS, Schuetz F, Schneeweiss A, Grischke E-M, Bloch W, Decker T, Uleer C, Salat C, Forster F, Schmidt M, Mundhenke C, Tesch H, Jackisch C, Fischer T, Guderian G, Hanson S, Fasching P. Everolimus + exemestane for HR+ advanced breast cancer in routine clinical practice- final results from the non-interventional trial, BRAWO. Cancer Res. 2019;79(4 Suppl):Abstract nr P6–18-08.
Steger GG, Bartsch R, Pfeiler G, Petru E, Greil R, Helfgott R, Egle D, Ohler L, Lang A, Tinchon C, Haslbauer F, Redl A, Hennebelle M, Miraz B, Winiger-Candolfi I, Gnant M. Efficacy and safety of everolimus plus exemestane in HR+, HER2--advanced breast cancer progressing on/after prior endocrine therapy, in routine clinical practice: 2nd interim analysis from STEPAUT. Cancer Res. 2017;77(4 Suppl):P4–22–20.
Jerusalem G, Mariani G, Ciruelos EM, Martin M, Tjan-Heijnen VC, Neven P, Gavila JG, Michelotti A, Montemurro F, Generali D, et al. Safety of everolimus plus exemestane in patients with hormone-receptor-positive, HER2-negative locally advanced or metastatic breast cancer progressing on prior non-steroidal aromatase inhibitors: primary results of a phase IIIb, open-label, single-arm, expanded-access multicenter trial (BALLET). Ann Oncol. 2016;27(9):1719–25.
Im YH, Uslu R, Lee KS, Nagarkar RV, Sohn J, Altundag AS, Chang YC, Abdel-Razeq H, Im SA, Jeong J, Park HY, Arpornwirat W, Bastick PA, Le TA, Arikan OO, Xue HL, Canatar A, Valenti R, Kim SB. Clinical effectiveness of everolimus and exemestane in advanced breast cancer patients from Asia and Africa: first efficacy andupdated safety results from the phase IIIb EVEREXES Study. Cancer Res. 2016;76(4 Suppl):P4–13–09.
Royce M, Bachelot T, Villanueva C, Ozguroglu M, Azevedo SJ, Cruz FM, Debled M, Hegg R, Toyama T, Falkson C, et al. Everolimus plus endocrine therapy for postmenopausal women with estrogen receptor-positive, human epidermal growth factor receptor 2-negative advanced breast cancer: a clinical trial. JAMA Oncol. 2018;4(7):977–84.
Bachelot T, Bourgier C, Cropet C, Ray-Coquard I, Ferrero JM, Freyer G, Abadie-Lacourtoisie S, Eymard JC, Debled M, Spaeth D, et al. Randomized phase II trial of everolimus in combination with tamoxifen in patients with hormone receptor-positive, human epidermal growth factor receptor 2-negative metastatic breast cancer with prior exposure to aromatase inhibitors: a GINECO study. J Clin Oncol. 2012;30(22):2718–24.
Kornblum N, Zhao F, Manola J, Klein P, Ramaswamy B, Brufsky A, Stella PJ, Burnette B, Telli M, Makower DF, et al. Randomized phase II trial of fulvestrant plus everolimus or placebo in postmenopausal women with hormone receptor-positive, human epidermal growth factor receptor 2-negative metastatic breast cancer resistant to aromatase inhibitor therapy: results of PrE0102. J Clin Oncol. 2018;36(16):1556–63.
Schmid P, Zaiss M, Harper-Wynne C, Ferreira M, Dubey S, Chan S, Makris A, Nemsadze G, Brunt AM, Kuemmel S, et al. Fulvestrant plus vistusertib vs fulvestrant plus everolimus vs fulvestrant alone for women with hormone receptor-positive metastatic breast cancer: the MANTA phase 2 randomized clinical trial. JAMA Oncol. 2019;5(11):1556–63.
Safra T, Kaufman B, Kadouri L, Efrat Ben-Baruch N, Ryvo L, Nisenbaum B, Evron E, Yerushalmi R. Everolimus plus letrozole for treatment of patients with HR(+), HER2(-) advanced breast cancer progressing on endocrine therapy: an open-label, phase II trial. Clin Breast Cancer. 2018;18(2):e197–203.
Jerusalem G, de Boer RH, Hurvitz S, Yardley DA, Kovalenko E, Ejlertsen B, Blau S, Ozguroglu M, Landherr L, Ewertz M, et al. Everolimus plus exemestane vs everolimus or capecitabine monotherapy for estrogen receptor-positive, HER2-negative advanced breast cancer: the BOLERO-6 randomized clinical trial. JAMA Oncol. 2018;4(10):1367–74.
Yardley DA, Liggett W, Mainwaring M, Castrellon A, Blakely L, Hemphill B, Anz B 3rd, Young RR, Shastry M, DeBusk LM, et al. A phase II open label study of everolimus in combination with endocrine therapy in resistant hormone receptor-positive HER2-negative advanced breast cancer. Clin Breast Cancer. 2019.
Rugo HS, Seneviratne L, Beck JT, Glaspy JA, Peguero JA, Pluard TJ, Dhillon N, Hwang LC, Nangia C, Mayer IA, et al. Prevention of everolimus-related stomatitis in women with hormone receptor-positive, HER2-negative metastatic breast cancer using dexamethasone mouthwash (SWISH): a single-arm, phase 2 trial. Lancet Oncol. 2017;18(5):654–62.
Rugo HS, Ruiz Borrego M, Chia SKL, Juric D, Turner NC, Drullinsky P, Lerebours F, Bianchi GV, Nienstedt CC, Ridolfi A, Thuerigen A, Ciruelos E. Alpelisib (ALP) + endocrine therapy (ET) in patients (pts) with PIK3CA-mutated hormone receptor-positive (HR+), human epidermal growth factor-2-negative (HER2-) advanced breast cancer (ABC): first interim BYLieve study results. J Clin Oncol. 2019;37(15, Suppl):1040.
Cristofanilli M, Turner NC, Bondarenko I, Ro J, Im SA, Masuda N, Colleoni M, DeMichele A, Loi S, Verma S, et al. Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. Lancet Oncol. 2016;17(4):425–39.
Slamon DJ, Neven P, Chia S, Fasching PA, De Laurentiis M, Im SA, Petrakova K, Bianchi GV, Esteva FJ, Martin M, et al. Phase III randomized study of ribociclib and fulvestrant in hormone receptor-positive, human epidermal growth factor receptor 2-negative advanced breast cancer: MONALEESA-3. J Clin Oncol. 2018;36(24):2465–72.
Sledge GW Jr, Toi M, Neven P, Sohn J, Inoue K, Pivot X, Burdaeva O, Okera M, Masuda N, Kaufman PA, et al. MONARCH 2: abemaciclib in combination with fulvestrant in women with HR+/HER2- advanced breast cancer who had progressed while receiving endocrine therapy. J Clin Oncol. 2017;35(25):2875–84.
Di Leo A, Johnston S, Lee KS, Ciruelos E, Lonning PE, Janni W, O'Regan R, Mouret-Reynier MA, Kalev D, Egle D, et al. Buparlisib plus fulvestrant in postmenopausal women with hormone-receptor-positive, HER2-negative, advanced breast cancer progressing on or after mTOR inhibition (BELLE-3): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2018;19(1):87–100.
Acknowledgements
We thank the Associazione Italiana per la Ricerca sul Cancro (AIRC, MFAG#22977: PI: Claudio Vernieri) and the Scientific Directorate of Fondazione IRCCS Istituto Nazionale dei Tumori for supporting our research.
Funding
C.V. is supported by the Associazione Italiana per la Ricerca sul Cancro (AIRC, MFAG#22977) and by the Scientific Directorate of Fondazione IRCCS Istituto Nazionale dei Tumori.
Author information
Authors and Affiliations
Contributions
CV conceived the work. All authors contributed to the data acquisition and analysis. All authors contributed to the manuscript draft. CV was responsible for the critical revision of the final manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any data from human participants or animals.
Consent for publication
Not applicable
Competing interests
F.d.B. received personal fees from Novartis for expert presentations and as a member of the advisory board. No other disclosures were reported.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Vernieri, C., Corti, F., Nichetti, F. et al. Everolimus versus alpelisib in advanced hormone receptor-positive HER2-negative breast cancer: targeting different nodes of the PI3K/AKT/mTORC1 pathway with different clinical implications. Breast Cancer Res 22, 33 (2020). https://doi.org/10.1186/s13058-020-01271-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13058-020-01271-0