Abstract
Background
Critical care of patients on extracorporeal membrane oxygenation (ECMO) with acute brain injury (ABI) is notable for a lack of high-quality clinical evidence. Here, we offer guidelines for neurological care (neurological monitoring and management) of adults during and after ECMO support.
Methods
These guidelines are based on clinical practice consensus recommendations and scientific statements. We convened an international multidisciplinary consensus panel including 30 clinician-scientists with expertise in ECMO from all chapters of the Extracorporeal Life Support Organization (ELSO). We used a modified Delphi process with three rounds of voting and asked panelists to assess the recommendation levels.
Results
We identified five key clinical areas needing guidance: (1) neurological monitoring, (2) post-cannulation early physiological targets and ABI, (3) neurological therapy including medical and surgical intervention, (4) neurological prognostication, and (5) neurological follow-up and outcomes. The consensus produced 30 statements and recommendations regarding key clinical areas. We identified several knowledge gaps to shape future research efforts.
Conclusions
The impact of ABI on morbidity and mortality in ECMO patients is significant. Particularly, early detection and timely intervention are crucial for improving outcomes. These consensus recommendations and scientific statements serve to guide the neurological monitoring and prevention of ABI, and management strategy of ECMO-associated ABI.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
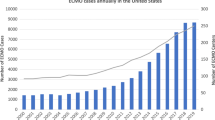
Extracorporeal membrane oxygenation (ECMO) is increasingly utilized, yet patients receiving ECMO support commonly experience major complications, including acute brain injury (ABI). ABI increases in-hospital mortality by a factor of 2–3 [1, 2]. ABI is more common in venoarterial (VA) ECMO than venovenous (VV) ECMO, especially for those with extracorporeal cardiopulmonary resuscitation (ECPR) with 27–32% of ABI during ECMO support (Table 1) despite its survival benefit [3, 4]. Although a protocolized neurological monitoring is shown to improve the detection of ABI, this is limited to a few ECMO centers [5]. The management of ECMO patients in the intensive care unit (ICU) is not standardized, and neurological monitoring and care vary significantly across ECMO centers, thus, the ICU management of patients with ABI during ECMO lacks high-quality evidence and recommendations.
As clinical experience accumulates and ECMO becomes more widely used, clinical guidelines and focused research on neurological monitoring and management of ABI are imperative to enhance ECMO patient care and improve early as well as long-term outcomes. This heterogeneity presents an opportunity to standardize and facilitate neurological care in ECMO [5].
To establish clinical guidelines on this topic, an international multidisciplinary panel of experts specialized in neurology, critical care, surgery, and other ECMO-related fields was assembled to provide clinical practice consensus recommendations and scientific statements in neurological monitoring and management of adult ECMO patients. These recommendations and statements have been promoted and endorsed by the Extracorporeal Life Support Organization (ELSO). We identified five key clinical areas needing recommendations: (1) neurological monitoring, (2) post-cannulation early physiological targets and their associations with ABI, (3) neurological therapy including medical and surgical intervention, (4) neurological prognostication, and (5) neurological follow-up and outcomes. Here, we present consensus recommendations based on the available evidence and related knowledge gaps warranting further investigations were also identified and summarized (Table 2).
Methods
Consensus guideline members
ELSO, an international non-profit consortium of healthcare institutions, researchers, and industry partners, developed this consensus statement. ELSO consists of 611 ECMO centers, with chapters in Europe, Asia–Pacific, North America, Latin America, Southwest Asia, and Africa.
An international multidisciplinary consensus panel of 30 experts, including neurologists, intensivists, surgeons, perfusionists, and other professionals in intensive care medicine with expertise or involvement in ECMO, from all ELSO chapters was assembled.
Each of the five-panel subgroups addressed a pre-selected clinical practice domain relevant to patients admitted to the ICU with ABI (ischemic stroke, ICH, or hypoxic-ischemic brain injury). Invited experts contributed to the guidelines through a three-phase process: (1) a literature search/review of neurological monitoring, management, and neurological ECMO outcomes, (2) summarizing the literature search/review, and (3) developing consensus guidelines using a modified Delphi method. The literature search and review performed comprehensively in PubMed on August 29, 2023 yielded up-to-date evidence on neurological monitoring and management strategies. Five key neurological areas needing recommendations were identified (see Introduction).
Guideline development
The selected articles were distributed to each subgroup. The subgroups summarized the findings and developed guidelines and recommendations for each subsection. Each subgroup nominated two leaders for cross-subgroup coordination. The consensus guideline members met regularly throughout the year in subgroup and whole-group settings to discuss their progress and reach a consensus on the finalized document. A modified Delphi process with three rounds of voting to assess the recommendation statements was implemented. Strong recommendation, weak recommendation, or no recommendation was defined when > 85%, 75–85%, and < 75% of panelists, respectively, agreed with a recommendation statement. Three rounds of voting and the authors’ comments about the expert consensus guideline appear in Supplemental Tables 1–3. The guidelines and recommendations were summarized and presented as 5 sections: (1) neurological assessment and monitoring; (2) bedside management; (3) interventional neurology, neurosurgery, and neurocritical care; (4) neurological prognostication; and (5) long-term outcome and quality of life.
Neurological assessment and monitoring
Neurological examination
Serial bedside examination remains the mainstay of neurological assessment in ECMO patients. However, neurological evaluation, especially early after ECMO cannulation, is frequently confounded by sedatives and paralytics, necessitating noninvasive multimodal neurological monitoring in patients with impaired consciousness. The data on ABI timing to ECMO cannulation/support are limited. Therefore, a baseline neurological assessment is recommended before and immediately after cannulation, followed by serial evaluations throughout ECMO support and after weaning. The ideal frequency of neurological examination is not yet established. Daily assessment by a neurologist/neurointensivist (if available) can improve neurological care. [5, 7] More frequent bedside nursing assessment, every 1–4 h based on ABI risk, is reasonable. Particularly, assessing signs of life (such as gasping, pupillary light response, and increased consciousness) is integral to the clinical examination, as these signs observed before, during resuscitation, and while on ECMO support may be associated with improved neurological outcomes [8]. Historically, the absence of brainstem reflexes with fixed, dilated pupils before cannulation was equated to irreversible ABI and a contraindication to ECMO. However, during cardiopulmonary resuscitation (CPR), fixed and dilated pupils are frequently seen after epinephrine administration, and patients have achieved favorable outcomes despite these findings [9].
Serial neurological examination should include mental status assessment, brainstem reflexes (pupillary light response and oculocephalic, corneal, and cough/gag reflexes), and motor exam. Standardized scoring tools such as the Glasgow Coma Scale and the Confusion Assessment Method should be used. Assessing the motor response of extremities in neurological examinations is only helpful when analgo-sedation and paralytic is lightened or off. Therefore, neurological exam for spinal cord injury, a rare but devastating injury, is very challenging [10]. Sensory exams are mostly limited in ECMO patients.
Sedation
Adequate analgo-sedation is essential to ECMO support and minimizes adverse events [11]. ECMO circuitry and common concomitant impaired liver or kidney function alter medication pharmacokinetics. Standardized sedation protocols with validated scoring systems, such as the Richmond Agitation Sedation Scale, are recommended. Overall, intermittent (as-needed) analgo-sedation is preferred over continuous infusion. Short-acting, non-benzodiazepine sedatives could be considered [11]. Daily reassessment of sedation goals, stepwise sedation weaning, and sedation interruptions can improve neurological exams and ABI diagnosis [11].
Neurological monitoring
Standardized neurological monitoring, clinical assessment, and a sedation cessation protocol may increase ABI detection and improve neurological outcomes [8, 12]. In a single-center study (90% VA ECMO), autopsy shortly after ECMO decannulation showed that 68% of ECMO non-survivors had developed ABI [13]. In another cohort, 9 of 10 brains exhibited ABI at autopsy [14], suggesting that ABI incidence is likely higher than clinical detection. Early, accurate ABI detection with standardized neurological monitoring and early interventions is critical for mitigating ABI. Table 3 summarizes current neurological monitoring tools and their evidence (Supplemental Fig. 1), and Table 4 provides the consensus recommendations on neurological monitoring (Fig. 1). A concise review of sedation, disorders of consciousness and seizure is separately summarized in Supplemental File 1.
Bedside management
Arterial oxygen
The brain depends on aerobic glucose metabolism for energy, with an average cerebral consumption of 3.5 mL oxygen per 100 g of brain tissue per minute. Hyperoxemia (partial pressure of oxygen (PaO2) > 100 or 120 mmHg: mild; > 300 mmHg: severe) and hypoxemia (PaO2 < 60 or 70 mmHg) are associated with increased mortality in ICU patients, including subjects on ECMO [41, 42].
VV ECMO
Limited data exist on early (first 24 h) oxygen targets and neurological outcomes after VV ECMO cannulation. In a single-center observational cohort study, PaO2 < 70 mmHg (hypoxemia) was associated with ABI, especially ICH [43]. There are no data on hyperoxemia as it is not often an issue clinically in VV ECMO patients.
VA ECMO
In VA ECMO, when the heart recovers before lung recovery, cerebral hypoxemia (especially of the right side of the brain) may occur due to the “differential oxygenation” (also called “Harlequin Syndrome” or “North–South Syndrome”), which is monitored by arterial blood gases from right radial arterial line, especially for those supported with peripheral VA ECMO. Monitoring of cerebral oxygenation using NIRS may be useful in diagnosing differential oxygenation [15].
Severe hyperoxemia (PaO2 > 300 mmHg) within 24 h after the cannulation may be associated with ABI and poor neurologic outcomes [4, 42, 44]. As optimal oxygenation targets are unknown, it is reasonable to avoid early (within 24 h) severe hyperoxemia and hypoxemia by manipulating the fraction of delivered oxygen from the ECMO sweep gas (Fig. 2). Given the high-quality data are limited, it is crucial to prospectively study the impact of hyperoxemia on ABI and neurological outcomes in VA ECMO as a multi-institutional study with protocolized neurological monitoring and diagnostic ABI adjudication. Importantly, further research is necessary to investigate the impact of hyperoxemia on each major VA ECMO cohort: postcardiotomy shock, ECPR, and post-acute myocardial infarction (AMI) as well as non-AMI cardiogenic shock.
Arterial carbon dioxide
Severe acidosis and hypercapnia are common before ECMO cannulation, and both are rapidly corrected upon ECMO initiation by adjusting sweep gas flow across the oxygenator. Carbon dioxide is a potent cerebral vasodilator that increases cerebral blood flow[45] and neuronal metabolic demand [46]. Prolonged hypercapnia, common in pre-ECMO patients, may impair cerebral autoregulation, leading to high cerebral blood flow and a narrow regulatory pressure window [40, 47]. While high partial pressure of carbon dioxide (PaCO2) should be avoided, rapid correction of sustained high PaCO2, particularly soon after ECMO initiation, sometimes leads to rapid hypocapnia; it may cause cerebral vasoconstriction and a decrease in cerebral oxygen delivery, resulting in cerebral ischemia [46]. Routine use of full-dose anticoagulation therapy at ECMO initiation and thereafter may cause hemorrhagic conversion of an ischemic injury.
VV ECMO
In an ELSO registry analysis, a rapid early decrease in PaCO2 was independently associated with an increased risk of ICH in ARDS patients with VV ECMO [48]. An ELSO retrospective study of 11,972 VV ECMO patients showed that those with ΔPaCO2 > 50% in the peri-cannulation period were more likely to experience ABI (infarct and ICH) [49].
VA ECMO
A higher ΔPaCO2 in VA ECMO was associated with ICH in a single-center observational study [50]. However, an ELSO retrospective study of 3125 ECPR patients showed ΔPaCO2 higher in ABI than non-ABI, but ΔPaCO2 was not significantly associated with ABI [4]. These findings are limited by (a) a lack of sensitive, reliable, and readily available diagnostic markers of ABI, (b) retrospective observations, and (c) inconsistent arterial blood gas sampling. Further research with standardized neurological diagnostic/monitoring tools and granular arterial blood gas data is necessary. However, avoiding a large ΔPaCO2 > 50% in the peri-cannulation period for both VA and VV ECMO is reasonable.
Temperature
Inducing hypothermia during ischemia prolongs the tolerance of organs to ischemia, improving neurological outcomes [51]. Thus, it could be reasonable to use hypothermia in VA ECMO patients where cerebral ischemic and hypoperfusion time is prolonged. This rationale is even more important in patients who have already suffered severe hypoxic-ischemic brain injury, as in ECPR. However, as demonstrated by a meta-analysis of 2643 ECPR patients (35 studies), data on this topic are severely heterogeneous and limited to low-quality evidence [52]. One randomized controlled trial on cardiogenic shock patients requiring VA ECMO compared moderate hypothermia (33–34 °C) versus normothermia (36–37 °C), showing no mortality difference at 30 days [53]. This study was limited by (1) insufficient sample size due to inaccurate effect size estimation based on non-ECMO studies, (2) lack of formal neurological assessment, and (3) primary outcome being mortality outcome at 30 days instead of neurological outcomes at 90 or 180 days. The basic and preclinical science on hypothermia in ischemia is strong, and VA ECMO patients have a high incidence of ABI and prolonged absent/low cerebral perfusion. Also, bleeding complications and coagulopathy were similar between those with hypothermia vs. without in a meta-analysis of ECPR patients [52]. A robust multicenter prospective observation cohort study is needed to test the effect of hypothermia strategically in each major VA ECMO cohort. There is no data on hypothermia in VV ECMO patients.
Blood pressure
No data exists on early and optimal blood pressure (BP) goals and ABI prevention, especially for stroke or hypoxic-ischemic brain injury, as the timing of ABI is not well-defined during the peri-cannulation period. After acute ischemic stroke, permissive hypertension (BP ≤ 220/120 mmHg) is recommended by the AHA[54]; it is reasonable to target mean arterial blood pressure (MAP) that can provide adequate cerebral perfusion in the setting of acute ischemic stroke.
Higher BPs lead to increased afterload, which may hinder myocardial recovery (VA ECMO only), particularly when the left ventricle is not vented. In the absence of high-quality data, allowing patients with acute ischemic stroke to autoregulate is reasonable if the heart can tolerate it. After ICH, lower BP (systolic BP < 140 mmHg and MAP < 90 mmHg) is preferred due to anticoagulation-associated ICH [55]. Cerebral autoregulation function in the setting of non-pulsatile blood flow and ABI is an active research area, and autoregulatory dysfunction may contribute to ABI in ECMO (Supplemental File 2) [56].
Low pulse pressure (< 20 mmHg) in the first 24 h of VA ECMO was associated with ABI [57]. However, data are weak regarding improving pulse pressure with inotropes, or left ventricle venting in ECMO [58]. Evidence on BP goals for optimal cerebral perfusion in ECMO patients is sparse. Yet, individualized BP management tailored to dynamic cerebral autoregulation function is likely needed in this complex population. However, evidence as well as related therapeutic actions in this regard are still limited and represent mandatory objectives for future research to enhance ECMO patient management and most likely ABI complications prevention and/or reduction. A summary of consensus recommendations and evidence appears in Table 5 and Supplemental Table 4.
Interventional neurology, neurosurgery, and neurocritical care
ABI diagnosis in ECMO patients is based on comprehensive neurological assessment and brain imaging. Neurological assessment for acute stroke should include the Glasgow Coma Scale and the National Institutes of Health Stroke Scale. Non-contrast head CT is imperative to rule out ICH with acute neurological exam change. CT angiogram is needed to assess for large vessel occlusion.
Brain perfusion optimization
Managing intracranial pressure (ICP) and BP contributes to adequate brain perfusion in ABI patients. Elevating the head of the bed by 30 degrees might benefit patients with ABI and elevated ICP [61]. However, brain oxygenation and circulation improve in the supine position, benefiting perfusion-dependent patients with acute ischemic strokes. The head of the bed could be guided by monitoring surrogate markers of cerebral hemodynamics (i.e., transcranial Doppler ultrasound: cerebral blood flow velocity) and oxygenation (i.e., NIRS: regional saturation) [62, 63]. If the heart can tolerate a higher BP, it’s reasonable to target a higher BP target (although individualized BP goal is recommended) to achieve adequate cerebral perfusion pressure, such as permissive hypertension for ischemic stroke. However, increased BP is associated with hematoma extension in ICH, so reducing BP (systolic BP < 140 mmHg) is reasonable, as ECMO patients are usually on full anticoagulation at the time of ICH.
Managing ischemic stroke
Tissue plasminogen activator (tPA)
Non-contrast head CT is imperative to rule out bleeding in acute neurological change, particularly during ECMO. tPA is a time-dependent intervention in acute ischemic stroke. Intravenous tPA in the setting of ECMO carries a high risk of bleeding, especially with systemic anticoagulation and platelet dysfunction. Given these risks, the use of tPA is generally not indicated in ECMO patients. Although there is limited literature specifically addressing this issue, the consensus among experts is to avoid tPA (Fig. 3).
Recommendations for interventional neurology, neurosurgery & neurocritical care on ECMO. CT: computed tomography; ECMO: extracorporeal membrane oxygenation; ICH: intracranial hemorrhage; ICP: intracranial pressure; PbtO2: brain tissue oxygenation; tPA: tissue plasminogen activator; VV: venovenous; VA: venoarterial
Mechanical thrombectomy
CT angiogram is needed to rule out large vessel occlusion, typically accompanied by a CT perfusion scan to assess salvageable penumbra. Mechanical thrombectomy should be pursued for patients with large vessel occlusion detected by CT angiogram (accompanied by a CT perfusion scan to assess salvageable penumbra), by consulting stroke specialists, as tPA is generally not recommended in ECMO [64].
Decompressive craniectomy
Decompressive craniectomy may be indicated in patients with space-occupying lesions with acute intracranial hypertension, such as hemispheric infarction with malignant edema. Hyperosmolar therapy is indicated for cerebral edema [1]. Systemic anticoagulation monitoring and resumption are necessary post-operatively. Successful craniectomy has been reported for patients on ECMO [65]. As evidence is limited, the risks versus benefits of such an intervention should be judiciously discussed in a multidisciplinary manner.
Managing ICH
There are two primary considerations in ICH management. First, preventing hematoma expansion by BP control and discontinuing systemic anticoagulation is recommended. The duration of systemic anticoagulation varies based on the mode of ECMO. VV ECMO may allow anticoagulation discontinuation until decannulation based on multiple reports of heparin-free VV ECMO with a heparin-coated circuit [66]. In contrast, holding systemic anticoagulation carries a higher risk of thromboembolism with VA ECMO, especially the ECMO circuit [67, 68]. Early cessation without reversal and judicious resumption of anticoagulation with repeated neuroimaging appeared feasible in the cohort of patients with ECMO-associated ischemic stroke and ICH [37]. Second, surgical or minimally invasive surgery hematoma evacuation may be considered. There is limited data on neurosurgical interventions in ECMO[69] for patients with no other management options. Neurosurgery may be considered and utilized. Multidisciplinary discussion should be undertaken, involving neurosurgeons and neurologists in decision-making.
Intracranial pressure monitoring
While external ventricular drainage may be indicated in patients with ICH with intraventricular extension and hydrocephalus, ECMO is associated with coagulopathy and requires systemic anticoagulation. Therefore, external ventricular drain insertion is a high-risk procedure associated with intra- and post-procedural bleeding [69]. External ventricular drain may be considered in selected patients at risk of imminent death from intraventricular hemorrhage and hydrocephalus. Monitoring ICP or invasive brain tissue oxygenation may be used in patients at high risk of ICP. Invasive ICP and brain tissue oxygenation have not been shown to improve long-term outcomes and may increase the risk of parenchymal hemorrhage in ECMO patients.
Cerebral venous sinus thrombosis (CVST)
Diagnosis of CVST requires a high index of suspicion in patients with risk factors for thrombosis, including internal jugular vein cannulation. Particularly, large dual-lumen VV ECMO cannulas may be associated with ABI, possibly due to venous hypertension and cannula-related thrombosis [70]. Clinical diagnosis is challenging because of varying neurological manifestations, including non-specific symptoms such as headache, seizure, or encephalopathy [71]. The diagnosis is made with brain CT in ECMO. Systemic anticoagulation is the primary treatment; however, in deteriorating patients, endovascular mechanical thrombectomy in advanced centers may be considered [72]. Lumbar puncture or other spinal fluid drainage and acetazolamide may be considered for patients with increased ICP, along with anti-edema interventions (raising the head of the bed, hyperosmolar therapy, sedation/analgesia, etc.) [73]. In severe CVST cases with hemispheric cerebral edema, decompressive craniectomy may be considered. A summary of consensus recommendations and evidence is provided in Table 6 and Supplemental Table 5.
Neurological prognostication
ECPR
Neurological prognostication is imperative in patients supported by ECPR, in which severe hypoxic-ischemic brain injury may occur as a consequence of refractory cardiac arrest and/or due to inadequate ECMO flow and differential hypoxia. It provides families and caregivers critical information and guides treatment decisions based on the likelihood of a meaningful neurological recovery. As the data on neurological prognostication is limited [74], a comprehensive approach to prognostication is needed.
Clinical examination plays a pivotal role in prognostication. Practitioners should first rule out potential confounding factors, such as sedatives, significant electrolyte disturbances, and hypothermia, to prevent an overly pessimistic prognosis. Daily clinical/neurological assessments are recommended for patients undergoing targeted temperature management, with the most crucial evaluation conducted after rewarming [74]. Attention should be given to pupillary and corneal reflexes [75, 76]. Clinicians must exercise caution to mitigate the “self-fulfilling prophecy” bias, which occurs when prognostic test results indicating poor outcomes influence treatment decisions [77].
A comprehensive prognostication strategy should include electrophysiological tests, the evaluation of biomarkers of ABI, and neuroimaging (Table 7). Notwithstanding, new modalities are under investigation and will hopefully provide additional clues in such a setting regarding early and enhanced detection of ABI as well as prognostication in ECMO patients [78, 79]. An unfavorable neurological outcome in patients without ECMO and cardiac arrest is strongly suggested by at least two indicators of severe ABI. These include the absence of pupillary and corneal reflexes at ≥ 72 h, bilateral lack of N20 cortical waves in somatosensory evoked potentials (SSEP) at ≥ 24 h, highly malignant EEG patterns at > 24 h, neuron-specific enolase levels exceeding 60 μg/L at 48 h or 72 h, status myoclonus ≤ 72 h, and extensive diffuse anoxic injury observed on brain CT/MRI [74, 80]. This approach has not been validated in ECMO patients and has limited evidence [30].
Neuron-specific enolase values are often higher in ECMO patients due to ongoing hemolysis [30, 85]. The most accurate neuron-specific enolase threshold for predicting an unfavorable neurological outcome in ECPR remains unknown, possibly exceeding 100 μg/L. There are sparse data on ECMO patients regarding other biomarkers, such as neurofilament light chain or tau. A combination of clinical, biomarker, electrophysiological, and neuroimaging assessment may effectively predict a neurological outcome within the first week following cardiac arrest [81]. However, limited data exist for this approach in ECMO patients; further research is needed to validate its utility. A summary of consensus recommendations and evidence is provided in Table 7.
Other neurological diseases
Neurological prognostication in other ABI (non-hypoxic-ischemic brain injury) with ECMO is challenging and relies on less robust data than cardiac arrest. In the context of stroke (ischemic and hemorrhagic), clinical factors impacting outcomes include neurological exam, age, functionality (i.e., modified Rankin Scale), size, and stroke location. For example, age and the location of intracerebral hemorrhage may contribute to neurological prognosis [86]. However, decisions regarding withdrawal of life-sustaining therapy should be highly individualized with multidisciplinary discussions and considered patient preferences, as data on ECMO patients are sparse.
ICH while the patient is anticoagulated during ECMO carries extremely high mortality and morbidity, as shown in large ELSO registry-based investigations [87, 88]. However, these studies did not account for withdrawing life-sustaining therapy in ECMO. Without data, no recommendations for neurological prognostication in ECMO patients can be made.
Brain death on ECMO
A systematic review reported that an apnea test could be included in brain-death criteria in ECMO patients by reducing sweep gas flow or adding exogenous carbon dioxide [89]. When an apnea test is challenging due to hemodynamic/cardiopulmonary instability, a cerebral angiogram or nuclear scan (radionuclide brain scan) is preferred [89]. We provide recommendations on apnea tests in ECMO patients (Supplemental Fig. 2).
Goals of care discussion
Goals of care and end-of-life discussions are often culturally influenced or determined. Therefore, it is difficult to propose international guidelines for such. No patient-level research guides communicating with families or managing ECMO discontinuation [82]. Families of ECMO patients experience significant anxiety, depression, and post-traumatic stress disorder long after hospital discharge [83]. Frequent family conversations/meetings should focus on informed consent, early goal-setting with timelines and re-evaluation, clear communication, and emotional support with compassion [82]. Ethics should be discussed openly, including whether to continue or discontinue care and resource allocation issues [82]. Routine use of ethics consultation within 72 h of cannulation, if the resource is available, can mitigate ethical conflicts by setting clear expectations [84]. Withdrawal from ECMO should be a structured process involving preparatory family meetings and clinical aspects, including symptom management, technical circuit management, and bereavement support, containing family and staff support.[90].
Long-term outcome and quality of life
Sparse information exists on long-term outcomes. Long-term MRI found cerebral infarction or hemorrhage in 37–52% of adult ECMO survivors [59, 60]. Cognitive impairment and neuroradiologic findings were associated [59, 60]. ECMO patients often suffer long-term psychiatric disorders, including organic mental disorders, obsessive–compulsive disorders, and post-traumatic stress disorders [91]. The incidence of neuroradiologic findings was significantly higher in VA ECMO patients than VV ECMO patients [59]. Given the high frequency, a routine, long-term, structured, standardized follow-up program is recommended for all ECMO centers. Such programs should encompass disease-specific care for underlying and acquired conditions, focusing on neurological and psychiatric disorders. Program design depends on the availability of institutional and international resources. ECMO centers should adapt follow-up programs their specific patient populations and resources while adhering to the recommendations outlined in Table 8.
Neurological outcomes and quality of life
Assessing ECMO survivors’ quality of life is crucial to understanding the overall impact of ECMO. It is preferable to use internationally recognized, validated tests at standardized intervals. Establishing uniform measures of cognitive function in ECMO patients may clarify outcomes in future studies. Therefore, all patients should have their modified Rankin Scale assessed at discharge and during each follow-up. Additional detailed assessments may be performed based on local practices and patient conditions (e.g., Glasgow Outcome Scale Extended, Montreal Cognitive Assessment). A summary of consensus recommendations and evidence is provided in Table 8 and Supplemental Fig. 3.
Conclusions
The impact of ABI on morbidity and mortality in ECMO patients is high, and early ABI detection and timely intervention may improve outcomes. Therefore, standardized neurological monitoring and neurological expertise are recommended for ECMO patients. These consensus recommendations and scientific statements serve to guide the neurological monitoring and prevention of ABI, and management strategy of ECMO-associated ABI These recommendations strongly benefit from multidisciplinary care, where it is available, to maximize the chances of favorable long-term outcomes and a good quality of life. Further research on predisposing factors, prevention, neuroimaging and management are ongoing or further required in an attempt to reduce or prevent such dreadful adverse events in ECMO patients.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- ABI:
-
Acute brain injury
- AMI:
-
Acute myocardial infarction
- BP:
-
Blood pressure
- CT:
-
Computed tomography
- ECMO:
-
Extracorporeal membrane oxygenation
- ECPR:
-
Extracorporeal cardiopulmonary resuscitation
- EEG:
-
Electroencephalogram
- ELSO:
-
Extracorporeal Life Support Organization
- ICH:
-
Intracranial hemorrhage
- ICP:
-
Intracranial pressure
- ICU:
-
Intensive care unit
- MRI:
-
Magnetic resonance imaging
- NIRS:
-
Near-infrared spectroscopy
- PaCO2 :
-
Partial pressure of carbon dioxide
- PaO2 :
-
Partial pressure of oxygen
- rSO2 :
-
Regional oxygen saturation
- SSEP:
-
Somatosensory evoked potential
- tPA:
-
Tissue plasminogen activator
- VA:
-
Venoarterial
- VV:
-
Venovenous
References
Cho SM, Farrokh S, Whitman G, Bleck TP, Geocadin RG. Neurocritical care for extracorporeal membrane oxygenation patients. Crit Care Med. 2019;47(12):1773–81.
Lorusso R, Gelsomino S, Parise O, Di Mauro M, Barili F, Geskes G, Vizzardi E, Rycus PT, Muellenbach R, Mueller T, et al. Neurologic injury in adults supported with veno-venous extracorporeal membrane oxygenation for respiratory failure: findings from the extracorporeal life support organization database. Crit Care Med. 2017;45(8):1389–97.
Ubben JFH, Heuts S, Delnoij TSR, Suverein MM, van de Koolwijk AF, van der Horst ICC, Maessen JG, Bartos J, Kavalkova P, Rob D, et al. Extracorporeal cardiopulmonary resuscitation for refractory OHCA: lessons from three randomized controlled trials-the trialists’ view. Eur Heart J Acute Cardiovasc Care. 2023;12(8):540–7.
Shou BL, Ong CS, Premraj L, Brown P, Tonna JE, Dalton HJ, Kim BS, Keller SP, Whitman GJR, Cho SM. Arterial oxygen and carbon dioxide tension and acute brain injury in extracorporeal cardiopulmonary resuscitation patients: analysis of the extracorporeal life support organization registry. J Heart Lung Transplant. 2023;42(4):503–11.
Ong CS, Etchill E, Dong J, Shou BL, Shelley L, Giuliano K, Al-Kawaz M, Ritzl EK, Geocadin RG, Kim BS, et al. Neuromonitoring detects brain injury in patients receiving extracorporeal membrane oxygenation support. J Thorac Cardiovasc Surg. 2023;165(6):2104–10.
Shoskes A, Migdady I, Rice C, et al. Brain injury is more common in venoarterial extracorporeal membrane oxygenation than venovenous extracorporeal membrane oxygenation: a systematic review and meta-analysis. Crit Care Med. 2020;48(12):1799–808. https://doi.org/10.1097/CCM.0000000000004618.
Cho SM, Ziai W, Mayasi Y, Gusdon AM, Creed J, Sharrock M, Stephens RS, Choi CW, Ritzl EK, Suarez J, et al. Noninvasive neurological monitoring in extracorporeal membrane oxygenation. ASAIO J. 2020;66(4):388–93.
Debaty G, Lamhaut L, Aubert R, Nicol M, Sanchez C, Chavanon O, Bouzat P, Durand M, Vanzetto G, Hutin A, et al. Prognostic value of signs of life throughout cardiopulmonary resuscitation for refractory out-of-hospital cardiac arrest. Resuscitation. 2021;162:163–70.
Desai M, Wang J, Zakaria A, Dinescu D, Bogar L, Singh R, Dalton H, Osborn E. Fixed and dilated pupils, not a contraindication for extracorporeal support: a case series. Perfusion. 2020;35(8):814–8.
Le Guennec L, Shor N, Levy B, Lebreton G, Leprince P, Combes A, Dormont D, Luyt CE. Spinal cord infarction during venoarterial-extracorporeal membrane oxygenation support. J Artif Organs. 2020;23(4):388–93.
Crow J, Lindsley J, Cho SM, Wang J, Lantry JH 3rd, Kim BS, Tahsili-Fahadan P. Analgosedation in critically Ill adults receiving extracorporeal membrane oxygenation support. ASAIO J. 2022;68(12):1419–27.
Cho SM, Ziai W, Geocadin R, Choi CW, Whitman G. Arterial-sided oxygenator clot and TCD emboli in VA-ECMO. Ann Thorac Surg. 2018;107(1):326–7.
Cho S-M, Geocadin RG, Caturegli G, Chan V, White B, Dodd-o J, Kim BS, Sussman M, Choi CW, Whitman G, et al. Understanding characteristics of acute brain injury in adult ECMO: an autopsy study. Crit Care Med. 2020;94:1650.
Mateen FJ, Muralidharan R, Shinohara RT, Parisi JE, Schears GJ, Wijdicks EF. Neurological injury in adults treated with extracorporeal membrane oxygenation. Arch Neurol. 2011;68(12):1543–9.
Zhao D, Shou BL, Caturegli G, et al. Trends on near-infrared spectroscopy associated with acute brain injury in venoarterial extracorporeal membrane oxygenation. ASAIO J. 2023;69(12):1083–9. https://doi.org/10.1097/MAT.0000000000002032.
Pozzebon S, Blandino Ortiz A, Franchi F, et al. Cerebral near-infrared spectroscopy in adult patients undergoing veno-arterial extracorporeal membrane oxygenation. Neurocrit Care. 2018;29(1):94–104. https://doi.org/10.1007/s12028-018-0512-1.
Bertini P, Marabotti A, Paternoster G, et al. Regional cerebral oxygen saturation to predict favorable outcome in extracorporeal cardiopulmonary resuscitation: a systematic review and meta-analysis. J Cardiothorac Vasc Anesth. 2023;37(7):1265–72. https://doi.org/10.1053/j.jvca.2023.01.007.
Joram N, Beqiri E, Pezzato S, et al. Continuous monitoring of cerebral autoregulation in children supported by extracorporeal membrane oxygenation: a pilot study. Neurocrit Care. 2021;34(3):935–45. https://doi.org/10.1007/s12028-020-01111-1.
Tian F, Farhat A, Morriss MC, et al. Cerebral hemodynamic profile in ischemic and hemorrhagic brain injury acquired during pediatric extracorporeal membrane oxygenation. Pediatr Crit Care Med. 2020;21(10):879–85. https://doi.org/10.1097/PCC.0000000000002438.
Caturegli G, Zhang LQ, Mayasi Y, et al. Characterization of cerebral hemodynamics with TCD in patients undergoing VA-ECMO and VV-ECMO: a prospective observational study. Neurocrit Care. 2023;38(2):407–13. https://doi.org/10.1007/s12028-022-01653-6.
Kavi T, Esch M, Rinsky B, Rosengart A, Lahiri S, Lyden PD. Transcranial doppler changes in patients treated with extracorporeal membrane oxygenation. J Stroke Cerebrovasc Dis. 2016;25(12):2882–5. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.07.050.
Caturegli G, Kapoor S, Ponomarev V, et al. Transcranial Doppler microemboli and acute brain injury in extracorporeal membrane oxygenation: a prospective observational study. JTCVS Tech. 2022;15:111–22. https://doi.org/10.1016/j.xjtc.2022.07.026.
Oddo M, Taccone FS, Petrosino M, et al. The Neurological Pupil index for outcome prognostication in people with acute brain injury (ORANGE): a prospective, observational, multicentre cohort study. Lancet Neurol. 2023;22(10):925–33. https://doi.org/10.1016/S1474-4422(23)00271-5.
Miroz JP, Ben-Hamouda N, Bernini A, et al. Neurological pupil index for early prognostication after venoarterial extracorporeal membrane oxygenation. Chest. 2020;157(5):1167–74. https://doi.org/10.1016/j.chest.2019.11.037.
Magalhaes E, Reuter J, Wanono R, et al. Early EEG for prognostication under venoarterial extracorporeal membrane oxygenation. Neurocrit Care. 2020;33(3):688–94. https://doi.org/10.1007/s12028-020-01066-3.
Amorim E, Firme MS, Zheng WL, et al. High incidence of epileptiform activity in adults undergoing extracorporeal membrane oxygenation. Clin Neurophysiol. 2022;140:4–11. https://doi.org/10.1016/j.clinph.2022.04.018.
Sinnah F, Dalloz MA, Magalhaes E, et al. Early electroencephalography findings in cardiogenic shock patients treated by venoarterial extracorporeal membrane oxygenation. Crit Care Med. 2018;46(5):e389–94. https://doi.org/10.1097/CCM.0000000000003010.
Peluso L, Rechichi S, Franchi F, et al. Electroencephalographic features in patients undergoing extracorporeal membrane oxygenation. Crit Care. 2020;24(1):629. https://doi.org/10.1186/s13054-020-03353-z.
Cho SM, Choi CW, Whitman G, et al. Neurophysiological findings and brain injury pattern in patients on ECMO. Clin EEG Neurosci. 2021;52(6):462–9. https://doi.org/10.1177/1550059419892757.
Ben-Hamouda N, Ltaief Z, Kirsch M, et al. Neuroprognostication under ecmo after cardiac arrest: Are classical tools still performant? Neurocrit Care. 2022;37(1):293–301. https://doi.org/10.1007/s12028-022-01516-0.
Kim YO, Ko RE, Chung CR, et al. Prognostic value of early intermittent electroencephalography in patients after extracorporeal cardiopulmonary resuscitation. J Clin Med. 2020;9(6):1745. https://doi.org/10.3390/jcm9061745.
Lidegran MK, Mosskin M, Ringertz HG, Frenckner BP, Linden VB. Cranial CT for diagnosis of intracranial complications in adult and pediatric patients during ECMO: clinical benefits in diagnosis and treatment. Acad Radiol. 2007;14(1):62–71. https://doi.org/10.1016/j.acra.2006.10.004.
Cvetkovic M, Chiarini G, Belliato M, et al. International survey of neuromonitoring and neurodevelopmental outcome in children and adults supported on extracorporeal membrane oxygenation in Europe. Perfusion. 2023;38(2):245–60. https://doi.org/10.1177/02676591211042563.
Malfertheiner MV, Koch A, Fisser C, et al. Incidence of early intra-cranial bleeding and ischaemia in adult veno-arterial extracorporeal membrane oxygenation and extracorporeal cardiopulmonary resuscitation patients: a retrospective analysis of risk factors. Perfusion. 2020;35:8–17. https://doi.org/10.1177/0267659120907438.
Lockie CJA, Gillon SA, Barrett NA, et al. Severe respiratory failure, extracorporeal membrane oxygenation, and intracranial hemorrhage. Crit Care Med. 2017;45(10):1642–9. https://doi.org/10.1097/CCM.0000000000002579.
Zotzmann V, Rilinger J, Lang CN, et al. Early full-body computed tomography in patients after extracorporeal cardiopulmonary resuscitation (eCPR). Resuscitation. 2020;146:149–54. https://doi.org/10.1016/j.resuscitation.2019.11.024.
Prokupets R, Kannapadi N, Chang H, et al. Management of anticoagulation therapy in ECMO-associated ischemic stroke and intracranial hemorrhage. Innovations (Phila). 2023;18(1):49–57. https://doi.org/10.1177/15569845221141702.
Cho SM, Wilcox C, Keller S, et al. Assessing the SAfety and FEasibility of bedside portable low-field brain Magnetic Resonance Imaging in patients on ECMO (SAFE-MRI ECMO study): study protocol and first case series experience. Crit Care. 2022;26(1):119. https://doi.org/10.1186/s13054-022-03990-6.
Lorusso R, Taccone FS, Belliato M, et al. Brain monitoring in adult and pediatric ECMO patients: the importance of early and late assessments. Minerva Anestesiol. 2017;83(10):1061–74. https://doi.org/10.23736/S0375-9393.17.11911-5.
Khanduja S, Kim J, Kang JK, et al. Hypoxic-ischemic brain injury in ecmo: pathophysiology, neuromonitoring, and therapeutic opportunities. Cells. 2023;12(11):1546. https://doi.org/10.3390/cells12111546.
de Jonge E, Peelen L, Keijzers PJ, Joore H, de Lange D, van der Voort PH, Bosman RJ, de Waal RA, Wesselink R, de Keizer NF. Association between administered oxygen, arterial partial oxygen pressure and mortality in mechanically ventilated intensive care unit patients. Crit Care. 2008;12(6):R156.
Al-Kawaz MN, Canner J, Caturegli G, Kannapadi N, Balucani C, Shelley L, Kim BS, Choi CW, Geocadin RG, Whitman G, et al. Duration of hyperoxia and neurologic outcomes in patients undergoing extracorporeal membrane oxygenation. Crit Care Med. 2021;49(10):e968–77.
Akbar AF, Shou BL, Feng CY, Zhao DX, Kim BS, Whitman G, Bush EL, Cho SM, Investigators H. Lower oxygen tension and intracranial hemorrhage in veno-venous extracorporeal membrane oxygenation. Lung. 2023;201(3):315–20.
Cho SM, Canner J, Chiarini G, Calligy K, Caturegli G, Rycus P, Barbaro RP, Tonna J, Lorusso R, Kilic A, et al. Modifiable risk factors and mortality from ischemic and hemorrhagic strokes in patients receiving venoarterial extracorporeal membrane oxygenation: results from the extracorporeal life support organization registry. Crit Care Med. 2020;48(10):e897–905.
Harper AM, Bell RA. The effect of metabolic acidosis and alkalosis on the blood flow through the cerebral cortex. J Neurol Neurosurg Psychiatry. 1963;26(4):341–4.
Dulla CG, Dobelis P, Pearson T, Frenguelli BG, Staley KJ, Masino SA. Adenosine and ATP link PCO2 to cortical excitability via pH. Neuron. 2005;48(6):1011–23.
Meng L, Gelb AW. Regulation of cerebral autoregulation by carbon dioxide. Anesthesiology. 2015;122(1):196–205.
Deng B, Ying J, Mu D. Subtypes and mechanistic advances of extracorporeal membrane oxygenation-related acute brain injury. Brain Sci. 2023;13(8):1165.
Cavayas YA, Munshi L, Del Sorbo L, Fan E. The early change in Pa. Am J Respir Crit Care Med. 2020;201(12):1525–35.
Shou BL, Ong CS, Zhou AL, Al-Kawaz MN, Etchill E, Giuliano K, Dong J, Bush E, Kim BS, Choi CW, et al. Arterial carbon dioxide and acute brain injury in venoarterial extracorporeal membrane oxygenation. ASAIO J. 2022;42(4):503–11.
van der Worp HB, Sena ES, Donnan GA, Howells DW, Macleod MR. Hypothermia in animal models of acute ischaemic stroke: a systematic review and meta-analysis. Brain. 2007;130(Pt 12):3063–74.
Huang M, Shoskes A, Migdady I, Amin M, Hasan L, Price C, Uchino K, Choi CW, Hernandez AV, Cho SM. Does targeted temperature management improve neurological outcome in extracorporeal cardiopulmonary resuscitation (ECPR)? J Intensive Care Med. 2022;37(2):157–67.
Levy B, Girerd N, Amour J, Besnier E, Nesseler N, Helms J, Delmas C, Sonneville R, Guidon C, Rozec B, et al. Effect of moderate hypothermia vs normothermia on 30-day mortality in patients with cardiogenic shock receiving venoarterial extracorporeal membrane oxygenation: a randomized clinical trial. JAMA. 2022;327(5):442–53.
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke. 2018;49(3):e46–110.
Minhas JS, Moullaali TJ, Rinkel GJE, Anderson CS. Blood pressure management after intracerebral and subarachnoid hemorrhage: the knowns and known unknowns. Stroke. 2022;53(4):1065–73.
Kazmi SO, Sivakumar S, Karakitsos D, Alharthy A, Lazaridis C. Cerebral pathophysiology in extracorporeal membrane oxygenation: pitfalls in daily clinical management. Crit Care Res Pract. 2018;2018:3237810.
Shou BL, Wilcox C, Florissi I, Kalra A, Caturegli G, Zhang LQ, Bush E, Kim B, Keller SP, Whitman GJR, et al. Early low pulse pressure in VA-ECMO is associated with acute brain injury. Neurocrit Care. 2023;38(3):612–21.
Lee SI, Lim YS, Park CH, Choi WS, Choi CH. Importance of pulse pressure after extracorporeal cardiopulmonary resuscitation. J Card Surg. 2021;36(8):2743–50.
Risnes I, Wagner K, Nome T, et al. Cerebral outcome in adult patients treated with extracorporeal membrane oxygenation. Ann Thorac Surg. 2006;81(4):1401–6. https://doi.org/10.1016/j.athoracsur.2005.10.008.
von Bahr V, Kalzen H, Hultman J, et al. Long-term cognitive outcome and brain imaging in adults after extracorporeal membrane oxygenation. Crit Care Med. 2018;46(5):e351–8. https://doi.org/10.1097/CCM.0000000000002992.
Ropper AH, O’Rourke D, Kennedy SK. Head position, intracranial pressure, and compliance. Neurology. 1982;32(11):1288–91.
Blanco P, Abdo-Cuza A. Transcranial Doppler ultrasound in neurocritical care. J Ultrasound. 2018;21(1):1–16.
Miller C, Armonda R. Participants in the International Multi-disciplinary Consensus conference on Multimodality Monitoring of cerebral blood flow and ischemia in the critically ill. Neurocrit Care. 2014;21(2):1–26.
Raha O, Hall C, Malik A, D’Anna L, Lobotesis K, Kwan J, Banerjee S. Advances in mechanical thrombectomy for acute ischaemic stroke. BMJ Med. 2023;2(1): e000407.
Friesenecker BE, Peer R, Rieder J, Lirk P, Knotzer H, Hasibeder WR, Mayr AJ, Dunser MW. Craniotomy during ECMO in a severely traumatized patient. Acta Neurochir (Wien). 2005;147(9):993–6.
Ryu KM, Chang SW. Heparin-free extracorporeal membrane oxygenation in a patient with severe pulmonary contusions and bronchial disruption. Clin Exp Emerg Med. 2018;5(3):204–7.
Lamarche Y, Chow B, Bedard A, Johal N, Kaan A, Humphries KH, Cheung A. Thromboembolic events in patients on extracorporeal membrane oxygenation without anticoagulation. Innovations (Phila). 2010;5(6):424–9.
Fina D, Matteucci M, Jiritano F, Meani P, Lo Coco V, Kowalewski M, Maessen J, Guazzi M, Ballotta A, Ranucci M, Lorusso R. Extracorporeal membrane oxygenation without therapeutic anticoagulation in adults: a systematic review of the current literature. Int J Artif Organs. 2020;43(9):570–8.
Fletcher-Sandersjoo A, Thelin EP, Bartek J Jr, Elmi-Terander A, Broman M, Bellander BM. Management of intracranial hemorrhage in adult patients on extracorporeal membrane oxygenation (ECMO): an observational cohort study. PLoS ONE. 2017;12(12): e0190365.
Mazzeffi M, Kon Z, Menaker J, Johnson DM, Parise O, Gelsomino S, Lorusso R, Herr D. Large dual-lumen extracorporeal membrane oxygenation cannulas are associated with more intracranial hemorrhage. ASAIO J. 2019;65(7):674–7.
Idiculla PS, Gurala D, Palanisamy M, Vijayakumar R, Dhandapani S, Nagarajan E. Cerebral venous thrombosis: a comprehensive review. Eur Neurol. 2020;83(4):369–79.
Saposnik G, Barinagarrementeria F, Brown RD Jr, Bushnell CD, Cucchiara B, Cushman M, deVeber G, Ferro JM, Tsai FY, Stroke C, American Heart Association, et al. Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(4):1158–92.
Einhaupl K, Stam J, Bousser MG, De Bruijn SF, Ferro JM, Martinelli I, Masuhr F. European federation of neurological S: EFNS guideline on the treatment of cerebral venous and sinus thrombosis in adult patients. Eur J Neurol. 2010;17(10):1229–35.
Nolan JP, Sandroni C, Bottiger BW, Cariou A, Cronberg T, Friberg H, Genbrugge C, Haywood K, Lilja G, Moulaert VRM, et al. European resuscitation council and european society of intensive care medicine guidelines 2021: post-resuscitation care. Resuscitation. 2021;161:220–69.
Nutma S, Ruijter BJ, Beishuizen A, Tromp SC, Scholten E, Horn J, van den Bergh WM, van Kranen-Mastenbroek VH, Thomeer EC, Moudrous W, et al. Myoclonus in comatose patients with electrographic status epilepticus after cardiac arrest: corresponding EEG patterns, effects of treatment and outcomes. Resuscitation. 2023;186: 109745.
Peluso L, Oddo M, Minini A, Citerio G, Horn J, Di Bernardini E, Rundgren M, Cariou A, Payen JF, Storm C, et al. Neurological pupil index and its association with other prognostic tools after cardiac arrest: a post hoc analysis. Resuscitation. 2022;179:259–66.
Elmer J, Kurz MC, Coppler PJ, Steinberg A, DeMasi S, De-Arteaga M, Simon N, Zadorozhny VI, Flickinger KL, Callaway CW, et al. Time to awakening and self-fulfilling prophecies after cardiac arrest. Crit Care Med. 2023;51(4):503–12.
Cho SM, Khanduja S, Kim J, Kang JK, Briscoe J, Arlinghaus LR, Dinh K, Kim BS, Sair HI, Wandji AN, Moreno E, Torres G, Gavito-Higuera J, Choi HA, Pitts J, Gusdon AM, Whitman GJ. detection of acute brain injury in intensive care unit patients on ECMO support using ultra-low-field portable mri: a retrospective analysis compared to head CT. Diagnostics (Basel). 2024;14(6):606.
Cho SM, Khanduja S, Wilcox C, Dinh K, Kim J, Kang JK, Chinedozi ID, Darby Z, Acton M, Rando H, Briscoe J, Bush E, Sair HI, Pitts J, Arlinghaus LR, Wandji AN, Moreno E, Torres G, Akkanti B, Gavito-Higuera J, Keller S, Choi HA, Kim BS, Gusdon A, Whitman GJ. Clinical use of bedside portable low-field brain magnetic resonance imaging in patients on ECMO: The results from multicenter SAFE MRI ECMO study. Res Sq [Preprint]. 2024
Rajajee V, Muehlschlegel S, Wartenberg KE, Alexander SA, Busl KM, Chou SHY, Creutzfeldt CJ, Fontaine GV, Fried H, Hocker SE, et al. Guidelines for neuroprognostication in comatose adult survivors of cardiac arrest. Neurocrit Care. 2023;38(3):533–63.
Sandroni C, D’Arrigo S, Cacciola S, et al. Prediction of good neurological outcome in comatose survivors of cardiac arrest: a systematic review. Intensive Care Med. 2022;48(4):389–413. https://doi.org/10.1007/s00134-022-06618-z.
Moynihan KM, Dorste A, Siegel BD, Rabinowitz EJ, McReynolds A, October TW. Decision-making, ethics, and end-of-life care in pediatric extracorporeal membrane oxygenation: a comprehensive narrative review. Pediatr Crit Care Med. 2021;22(9):806–12. https://doi.org/10.1097/PCC.0000000000002766.
Onrust M, Lansink-Hartgring AO, van der Meulen I, Luttik ML, de Jong J, Dieperink W. Coping strategies, anxiety and depressive symptoms in family members of patients treated with extracorporeal membrane oxygenation: a prospective cohort study. Heart Lung Mar. 2022;52:146–51. https://doi.org/10.1016/j.hrtlng.2022.01.002.
Wirpsa MJ, Carabini LM, Neely KJ, Kroll C, Wocial LD. Mitigating ethical conflict and moral distress in the care of patients on ECMO: impact of an automatic ethics consultation protocol. J Med Ethics. 2021. https://doi.org/10.1136/medethics-2020-106881.
Petermichl W, Philipp A, Hiller KA, Foltan M, Floerchinger B, Graf B, Lunz D. Reliability of prognostic biomarkers after prehospital extracorporeal cardiopulmonary resuscitation with target temperature management. Scand J Trauma Resusc Emerg Med. 2021;29(1):147.
Gregorio T, Pipa S, Cavaleiro P, Atanasio G, Albuquerque I, Castro Chaves P, Azevedo L. Original intracerebral hemorrhage score for the prediction of short-term mortality in cerebral hemorrhage: systematic review and meta-analysis. Crit Care Med. 2019;47(6):857–64.
Cho SM, Canner J, Caturegli G, Choi CW, Etchill E, Giuliano K, Chiarini G, Calligy K, Rycus P, Lorusso R, et al. Risk factors of ischemic and hemorrhagic strokes during venovenous extracorporeal membrane oxygenation: analysis of data from the extracorporeal life support organization registry. Crit Care Med. 2021;49(1):91–101.
Hwang J, Kalra A, Shou BL, Whitman G, Wilcox C, Brodie D, Zaaqoq AM, Lorusso R, Uchino K, Cho SM. Epidemiology of ischemic stroke and hemorrhagic stroke in venoarterial extracorporeal membrane oxygenation. Crit Care. 2023;27(1):433.
Lie SA, Hwang NC. Challenges of brain death and apnea testing in adult patients on extracorporeal corporeal membrane oxygenation-a review. J Cardiothorac Vasc Anesth. 2019;33(8):2266–72.
Machado DS, Garros D, Montuno L, Avery LK, Kittelson S, Peek G, Moynihan KM. Finishing well: compassionate extracorporeal membrane oxygenation discontinuation. J Pain Symptom Manage. 2022;63(5):e553–62.
Kalra A, Kang JK, Khanduja S, Menta AK, Ahmad SA, Liu O, Rodriguez E, Spann M, Hernandez AV, Brodie D, et al. Long-term neuropsychiatric, neurocognitive, and functional outcomes of patients receiving ECMO. Neurology. 2024;102(3): e208081.
Risnes I, Heldal A, Wagner K, et al. Psychiatric outcome after severe cardio-respiratory failure treated with extracorporeal membrane oxygenation: a case-series. Psychosomatics. 2013;54(5):418–27. https://doi.org/10.1016/j.psym.2013.02.008.
Janssen MF, Bonsel GJ, Luo N. Is EQ-5D-5L better than EQ-5D-3L? A head-to-head comparison of descriptive systems and value sets from seven countries. Pharmacoeconomics. 2018;36(6):675–97. https://doi.org/10.1007/s40273-018-0623-8.
Funding
Dr. Cho is supported by NIH (1K23HL157610, 1R21NS135045). Dr. Brodie received research support from and consults for LivaNova.
Author information
Authors and Affiliations
Contributions
S.-M.C. prepared the first draft, led the conceptualization and approach, and finalized the guidelines. A.M.Z. and R.L. provided critical revision and contributed in finalizing the guidelines as co-chairs. J.H. and G.C. provided tables and contributed to the first draft. M.A. created all figures and supplemental figures. M.A., N.B., J.B., D.B., H.J.D, R.D., A.E., P.T.F., H.F., J.F., A.H., J.-S.J., C.L., G.M., G.P., A.P., J.P., L.R., K.R., D.D., D.R., L.S., F.S.T., and G.W. were divided into 6 writing groups and prepared each section of the guidelines (6 sections).
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable as this is a consensus guidelines article.
Competing interests
Dr. Cho is a consultant for Hyperfine, Inc. and supported by NIH (1K23HL157610 and 1R21NS135045). Dr. Brodie received research support from and consults for LivaNova. He has been on the medical advisory boards for Xenios, Medtronic, Inspira, and Cellenkos. He is the President-elect of the Extracorporeal Life Support Organization (ELSO) and the Chair of the Executive Committee of the International ECMO Network (ECMONet), and he writes for UpToDate. Dr. Daniel is supported by MH CZ (DRO-VFN64165) and receives consulting honoraria from Abiomed and Resuscitec. Dr. Lorusso received research support from Medtronic and LivaNova, is consultant for Medtronic and Livanova, Member of the Medical Advisory Board of Eurosets and Xenios, and receives speaker fee from Abiomed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cho, SM., Hwang, J., Chiarini, G. et al. Neurological monitoring and management for adult extracorporeal membrane oxygenation patients: Extracorporeal Life Support Organization consensus guidelines. Crit Care 28, 296 (2024). https://doi.org/10.1186/s13054-024-05082-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-024-05082-z