Abstract
Background
The post-discharge prognosis of patients with sepsis remains a crucial issue; however, few studies have investigated the relationship between pre-sepsis health status and subsequent prognosis in a large population. This study aimed to examine the effect of the pre-sepsis care needs level on changes in care needs and mortality in patients with sepsis 1 year post-discharge.
Methods
This was a population-based retrospective cohort study including twelve municipalities in Japan that participated in the Longevity Improvement & Fair Evidence study between April 2014 and March 2022, with a total of 1,491,608 persons. The pre-hospitalization levels of care needs (baseline) were classified from low to high, as no care needs, support level and care needs level 1, care needs levels 2–3, and care needs levels 4–5 (fully dependent). The outcomes were changes in care needs level and mortality 1 year post-discharge, assessed by baseline care needs level using Cox proportional hazard models.
Results
The care needs levels of 17,648 patients analyzed at baseline were as follows: no care needs, 7982 (45.2%); support level and care needs level 1, 3736 (21.2%); care needs levels 2–3, 3089 (17.5%); and care needs levels 4–5, 2841 (16.1%). At 1 year post-discharge, the distribution of care needs were as follows: no care needs, 4791 (27.1%); support level and care needs level 1, 2390 (13.5%); care needs levels 2–3, 2629 (14.9%); care needs levels 4–5, 3373 (19.1%); and death, 4465 (25.3%). Patients with higher levels of care needs exhibited an increased association of all-cause mortality 1 year post-discharge after adjusting for confounders [hazard ratios and 95% confidence intervals: support level and care needs level 1, 1.05 (0.96, 1.15); care needs levels 2–3, 1.46 (1.33, 1.60); and care needs levels 4–5, 1.92 (1.75, 2.10); P for trend < 0.001].
Conclusions
Elevated care needs and mortality were observed in patients with sepsis within 1 year post-discharge. Older patients with sepsis and higher baseline levels of care needs had a high association of all-cause mortality 1 year post-discharge.
Similar content being viewed by others
Background
Sepsis is a serious condition associated with a high mortality rate (18–60%) [1]. Though long-term sequelae, including physical limitations, cognitive impairments, and exacerbation of chronic medical conditions, are often observed in patients who survive sepsis [1,2,3], in-hospital mortality associated with sepsis has decreased worldwide with the establishment of treatment guidelines [4]. The in-hospital mortality of sepsis has decreased significantly from 25.0% in 2010 to 18.3% in 2017 in Japan [5]. However, the post-discharge recovery of patients with sepsis, especially older patients with cognitive decline, remains a challenge requiring long-term care [2, 3]. Moreover, post-discharge mortality is a significant concern [6].
Long-term care (LTC) services are provided to older and disabled individuals in Japan as a social insurance program following the establishment of the LTC insurance system in 2000 [7]. An LTC accreditation review board, including medical specialists, was established based on nationally defined criteria to assess the requirements of LTC insurance beneficiaries and to determine the type and scope of LTC services they qualify for [8]. The care needs level (CNL) is significantly associated with activities of daily living (ADL) as determined by the Barthel Index score [9], cognitive decline [10, 11], and frailty [12]. Consequently, it has been used as a functional evaluation tool.
Previous studies have examined various risk factors for post-discharge mortality in patients with sepsis; however, the focus on the pre-sepsis health status was not sufficient in most of these studies [13,14,15,16]. A recent post-hoc analysis of a multicentre cohort study indicated that septic patients had a higher risk of new disability or death at 6 months compared with patients without sepsis [17]. Another study conducted in the USA found a high incidence of new functional limitations following sepsis, both in individuals who had no prior limitations and those with mild to moderate limitations before sepsis [18]. A comprehensive and dynamic description of the entire care process, from pre-sepsis to post-sepsis recovery, plays a crucial role in understanding the condition of survivors and improving their prognosis. Therefore, this population-based study used claims data to examine whether a higher pre-sepsis CNL is associated with worsening changes in CNL and increased mortality in patients with sepsis in Japan 1 year post-discharge.
Methods
Study design and setting
This retrospective population-based cohort study was performed using data from the Longevity Improvement and Fair Evidence (LIFE) study. Data regarding the design of the LIFE study and demographic characteristics of the participants have been documented in previous literature [19] and the “Supplementary Methods”.
The data from 12 of the 28 municipalities that participated in the LIFE study were included in this study because they provided a sufficient observation period and complete LTC insurance claims data necessary for our analysis. The claims data for the medical (inpatient and outpatient) and LTC services utilized by 1,491,608 persons between April 2014 and March 2022 were analyzed. Supplementary Table 1 presents the size of each municipality and the duration of data collection.
In Japan, all patients can receive full care during hospitalization. Decisions to withdraw care are usually made by medical institutions and teams in consultation with the patient and their family. These decisions are guided by careful ethical considerations to prioritize the patient's dignity and quality of life.
This study was approved by the Kyushu University Institutional Review Board for Clinical Research (approval no. 22114) and the Osaka University Institutional Review Board (approval no. 21107).
Study participants
Patients with sepsis were defined as individuals with suspected severe infection and acute organ dysfunction, based on previous research conducted in the United States and Japan [5, 20,21,22]. Presumed severe infection was determined through blood culture results and the initiation of new antibiotic treatments [5, 20, 21]. Acute organ dysfunction was diagnosed using diagnostic codes (renal dysfunction, hepatic dysfunction, thrombocytopenia, coagulopathy, or acidosis) and treatment records (initiation of vasopressor therapy for circulatory dysfunction, initiation of mechanical ventilation or oxygen therapy for respiratory dysfunction, or initiation of renal replacement therapy for renal dysfunction) [5, 21]. “Supplementary Methods”, Supplementary Table 2, and Supplementary Figs. 2A and 2B present the detailed definitions and corresponding codes.
Definition of CNL
The LTC is offered to all individuals aged over 65 and those aged 40–64 with specific disabilities. This system ensures that all eligible individuals receive the necessary care. Those who meet the eligibility criteria can obtain LTC services through a certification process that objectively assesses their CNL based on national standards [8]. This process is tailored to the specific needs of each applicant. Seven CNL Certificates, ranging from Support Level (SL) 1–2 to CNL 1–5, were issued based on assessment findings. SL 1 indicates the lowest level of care, whereas CNL 5 indicates disability requiring the highest care level. Detailed information is provided in the “Supplementary Methods” and Supplementary Table 6.
The patients’ monthly care needs were defined based on the LTC insurance and certification surveys as described in previous studies [23, 24] and classified into four categories: no care needs, SL&CNL 1, CNLs 2–3, and CNLs 4–5. The baseline CNL of patients with sepsis was defined as the CNL one month before admission in this study. The subsequent CNLs were assessed at five intervals: the month of discharge, 1 month post-discharge, 3 months post-discharge, 6 months post-discharge, and 1 year post-discharge.
Definition of death
The date of death was determined using the earliest date among the following records: date of death during hospitalization in diagnosis procedure combination claims, date of death in LTC insurance claims, and date of death according to the death identification logic in the national database, as described in a previous study [25]. The sensitivity and specificity of this method for defining the date of death were 92.9% and 99.7%, respectively, as described previously [25].
Endpoints
The changes in the CNL and all-cause death 1 year post-discharge were defined as the endpoints.
Covariates
The following covariates were defined based on the findings of a previous study [5]: sex, age at admission, city, comorbidities present in the 6 months before admission (including cancer, hypertension, diabetes mellitus, heart failure, cerebrovascular disease, ischemic heart disease, chronic respiratory disease, chronic renal failure, and dementia), site of infection (including respiratory, urogenital, abdominal, bone and soft tissue, blood and meninges or brain or spinal cord, multi-site infections, and infections of unknown origin), acute organ dysfunction, use of vasopressors, mechanical ventilation or oxygen therapy, antibiotic treatment duration, hospitalization duration, and intensive care unit (ICU) admission. Supplementary Tables 2 and 3 list the specific definition codes for these covariates.
Statistical analysis
The baseline characteristics were compared by categorizing the patients according to their baseline CNLs. Continuous variables are presented as medians and interquartile ranges (IQR), whereas categorical variables are presented as numbers and percentages.
The baseline and post-discharge CNLs were compared to illustrate the changes in the care needs post-discharge. The changes were categorized as follows: “improved,” a decrease in the CNL; “worsened,” an increase in the CNL; and “no change,” no alteration. An alluvial diagram (Naqvi, A. Stata package alluvial, Version 1.2, 2023 [computer software] https://github.com/asjadnaqvi/stata-alluvial) was used to illustrate the trends.
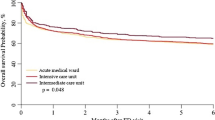
Detailed information of follow-up is provided in “Supplementary Method” and Supplementary Fig. 1. The Kaplan–Meier method was used to calculate the cumulative probabilities of death within 1 year post-discharge according to the baseline CNL of the patients with sepsis. Cox proportional hazard regression models were used to calculate the hazard ratios (HRs) and 95% confidence intervals (CIs) to further analyze this association. Detail information of covariates is provided in “Supplementary Method” and Supplementary Table 3. We included these covariates in multivariable Cox models to control for their effects. Model 1 was adjusted for sex, age at the time of admission, and the city of residence. Model 2 was further adjusted for prior comorbidities, acute organ involvement, and treatment (detailed in “Supplementary Methods”). The same model was used to test for linear trends by assigning ordinal numbers (1–4) to each baseline CNL category. We conducted a stratified analysis based on ICU admission status to investigate the association between baseline CNL and 1-year post-discharge mortality for patients both with and without ICU admission. The interaction term of baseline CNL with ICU was included in the Cox proportional hazards regression models. The P-interaction values were computed using likelihood ratio tests.
Because a prior research shows that sepsis mortality differs across sex and age groups [26], we stratified the association between baseline CNL and all-cause mortality by sex (men or women) and age (by median: ≤ 80 years or > 80 years) in the subgroup analysis. For the analysis of the association between changes in CNLs from preadmission to discharge and 1-year mortality, we categorized cases where the CNL worsened by one level or more as “Worsened,” cases with no change as “No change,” and cases with improvement as “Improved.” We further included in-hospital deaths among sepsis patients to explore the association between baseline CNL and in-hospital mortality. Adjusting for the same variables, we used a logistic regression model to investigate this association. In the current study, the medical claim database was utilized, and since it contained no missing data, imputation was not required.
Statistical significance was set at two-sided P values of < 0.05. All statistical analyses were performed using Stata version 18.0 (Stata Corporation, College Station, TX, USA).
Results
Figure 1 presents the flowchart of the study. A total of 26,857 patients with sepsis were selected from among 1,491,608 persons. Patients aged < 65 years at the time of hospitalization (n = 2520) and those who died in the hospital (n = 5410) were excluded. The 6-month period before hospitalization was set as the lookback period to define comorbidities. Patients with a lookback period of < 6 months (n = 1279) were excluded; 17,648 patients with sepsis were included.
Among the 17,648 patients with sepsis, 4465 deaths were recorded during the 1-year follow-up period post-discharge, of which 1891 (42.4%) were women. Among the 4465 patients who died, the last recorded CNL was as follows: 1184 patients (26.5% of deaths) had no care needs, 473 patients (10.6%) were in the SL & CNL1 group, 914 patients (20.5%) were in the CNL2-3 group, and 1894 patients (42.4%) were in the CNL4-5 group. Table 1 presents the patient characteristics stratified according to the baseline CNL. The number of patients in each CNL group was 7982 (45.2%), 3736 (21.2%), 3089 (17.5%), and 2841 (16.1%) for no care needs, SL & CNL 1, CNLs 2–3, and CNLs 4–5, respectively. Women comprised 49.9% of the 17,648 patients with sepsis, and the median age was 83 years. Compared with the patients with no care needs at baseline, the patients with higher CNLs were older, more likely to be women, and had a higher prevalence of cerebrovascular disease and dementia; however, the prevalence of cancer was lower among these patients. Regarding the sites of infection, respiratory (21.8%), abdominal (14.7%), and multi-site infections (11.5%) were common among patients with no care needs; respiratory (19.7%), multiple (18.7%), and urogenital (11.9%) infections were common among patients in the CNLs 4–5 group. Renal dysfunction (42.3%) was the most common type of acute organ dysfunction, and its proportion increased with the care needs. Among the patients with sepsis, 24.2% required ICU admission, with a median (IQR) length of hospital stay of 24 (13, 46) days.
Table 2 and Fig. 2 present changes in the CNL among the patients with sepsis 1 year post-discharge. The care levels were as follows: no care needs, 4791 patients (27.1%); SL & CNL 1, 2390 patients (13.5%); CNLs 2–3, 2629 patients (14.9%); CNLs 4–5, 3373 patients (19.1%). A total of 8392 patients [47.6%] required care needs, and 4465 patients (25.3%) died 1 year post-discharge. Among them, 253 (1.4%) demonstrated an improvement, 9216 (52.2%) showed no changes, and 3714 (21.0%) experienced worsening in their CNLs compared to their baseline CNLs. A higher CNL at baseline was associated with a higher proportion of deaths 1 year post-discharge. Specifically, among the 1567 (the proportion of deaths: 19.6%, calculated as 1567/7982, representing the proportion of deaths within this group), 879 (23.5%), 956 (30.9%), and 1063 (37.4%) patients who died, the baseline CNLs were categorized as no care needs, SL & CNL 1, CNLs 2–3, and CNLs 4–5, respectively. Supplementary Table 4 details the changes in CNLs and deaths. The proportion of deaths was higher in the group with a higher baseline CNL regardless of the months of follow-up. In addition, the percentage of patients with sepsis who had no care needs reduced from 45.2% (7982/17,648 patients) at baseline to 36.2% (6393 patients) at the time of discharge; this proportion decreased further to 27.1% 1 year post-discharge.
Post-discharge outcomes of the patients with sepsis stratified according to baseline care needs levels. The alluvial diagram depicts the change in CNLs a month before hospitalization to 1 year after discharge in patients with sepsis Numbers in the line indicate the patient count in each stratum, with the line thickness proportional to these counts. Green represents death, orange represents CNLs 4–5, blue represents CNLs 2–3, purple represents SL & CNL 1, and red represents ‘No care needs.’ Consistent colors are used to represent the same categories before and after changes in CNLs. Strata with < 200 patients are not individually labeled. Detailed data are presented in Supplementary Table 4. CN, care needs; CNL, care needs level; SL, support level
Supplementary Figure 3 and Table 3 present the association between the baseline CNL and all-cause death in patients with sepsis within 1 year post-discharge. The Kaplan–Meier curves revealed that patients with sepsis who had elevated baseline CNLs exhibited a higher cumulative probability of all-cause mortality than those with no care needs (Supplementary Fig. 3). The incidence of post-discharge death in the no care needs, SL & CNL 1, CNLs 2–3, and CNLs 4–5 groups were 67, 82, 115, and 146 per 100,000 person-days, respectively (Table 3). Compared with that of patients with sepsis, who had no care needs at baseline, the HRs and 95% CIs in the multivariable model (HR2) were as follows: SL & CNL 1, 1.05 (0.96, 1.15); CNLs 2–3, 1.46 (1.33, 1.60); and CNLs 4–5, 1.92 (1.75, 2.10). A higher CNL at baseline was associated with an increased risk of mortality within 1 year post-discharge in patients with sepsis (P for trend < 0.001). Table 3 also indicated that baseline CNL was associated with increased mortality 1 year after discharge in both ICU and non-ICU patients with sepsis. Specifically, the hazard ratios (HRs) and 95% confidence intervals (CIs) for baseline CNL levels 4–5 were 1.97 (1.61, 2.40) for ICU sepsis patients and 1.90 (1.71, 2.11) for non-ICU sepsis patients.
Supplementary Table 5 presents the results of the analysis stratified according to sex and age. An elevated baseline CNL in patients with sepsis was associated with higher mortality within 1 year post-discharge regardless of sex or age (≤ 80 or > 80 years). We found that both an increase and a decrease in CNL were not associated with 1-year mortality when compared to those whose CNL remained unchanged in Supplementary Table 7. Supplementary Table 8 indicated that a higher baseline CNL was associated with an increased risk of in-hospital death [odds ratio (OR) and 95% CI for CNLs 4–5: 1.25 (1.13, 1.39), P for trend < 0.001].
Discussion
Our study described the entire care process from pre-sepsis to post-sepsis recovery and analyzed the effect of the baseline CNL on the post-discharge survival of patients with sepsis. The present study revealed an improvement in CNL 1 year post-discharge in a few patients with sepsis and a worsening of the CNL or even death in approximately half of the cohort 1 year post-discharge. Furthermore, the baseline CNL was associated with an increased risk of all-cause mortality 1 year post-discharge in patients with sepsis. In general, functional status is predictive of functional decline and death irrespective of sepsis. The findings of the present study address a gap in the field of sepsis regarding the association between the pre-sepsis health status and functional outcomes after recovery. Furthermore, these findings offer valuable insights that could inform strategies to enhance recovery and reduce mortality in patients with sepsis.
The present study revealed that patients with sepsis continued to require significant care 1 year post-discharge. Approximately 50% of patients (n = 8392) required care 1 year post-discharge, whereas the CNL worsened compared with that at baseline in 21.0% of patients (n = 3714). Among the patients with no care needs at baseline, the proportion of patients requiring care increased to 20.4% 1 year post-discharge. The number of patients who did not require care decreased each month. A previous study conducted in the USA also found that severe sepsis in older adults was independently associated with significant and persistent new cognitive impairment and functional disability among 516 survivors [18]. Additionally, although recent studies suggested that there was no significant difference in health-related quality of life or disability between sepsis patients and non-sepsis patients after ICU admission, sepsis patients often incurred higher ICU costs or had higher subsequent mortality [17, 27]. A study conducted in Australia compared the WHO Disability Assessment Schedule 2.0 score changes in 282 sepsis survivors one month before ICU admission, and at 3 and 6 months after ICU admission [17]. The study found that disability increased at 3 months post-discharge but showed no significant difference at 6 months [17]. Our study, which evaluated CNL in a larger population, revealed post-discharge functional changes in sepsis patients. This further emphasized that even individuals who originally had no care needs might experience functional decline after discharge, leading to an increase in CNL levels.
Overall, patients with sepsis require a prolonged period of care or more expensive care post-discharge [3, 28,29,30,31]. However, the duration and level of care vary from country to country owing to differences in health and care systems. Therefore, assessing the prognosis of patients with sepsis quantitatively and intuitively in different countries using these indicators is difficult. In contrast, the present study described the dynamic process of care for patients with sepsis from the pre-admission period to 1 year post-discharge, based on the insurance system in Japan, using levels of care that were closely related to the living status of older patients [9,10,11,12].
Patients with sepsis often experience cognitive impairments post-discharge. Moreover, these patients have an increased risk of developing cancer and may even be readmitted owing to the recurrence of sepsis [15, 28, 31,32,33]. These health-related issues can worsen the CNL [28]; thus, patients with sepsis must be monitored post-discharge.
The present study revealed that 25.3% of patients with sepsis aged 65 years died 1 year post-discharge from 2014 to 2020. Two studies conducted in France reported that the mortality rates of patients with sepsis in the first year post-discharge were 22.9% from 2015 to 2018, and 22.3% in 2018 [15, 28]. A study conducted in the United States reported that the mortality rate was 24% in the patients with sepsis 1 year post-discharge from 2009 to 2019 [16]. A study conducted in Germany reported that 30.7% of patients with sepsis died within the first year from 2013 to 2014 [29]. Although our study population was older than those in other studies, the similar mortality in sepsis patients might be explained by multiple factors, including race, treatment protocols in different countries, and data collection period. The present study revealed that the baseline CNL was associated with an increased mortality risk 1 year post-discharge in patients with sepsis. Previous studies have reported multiple risk factors for all-cause death post-discharge in patients with sepsis, including age, comorbidities, and the site of infection [13,14,15,16]. However, most of these studies did not focus on the relationship between the pre-sepsis CNL and mortality 1 year post-discharge. Only one study conducted in England mentioned that pre-admission dependence may be associated with mortality risk in patients with sepsis [13].
The present study revealed a linear trend between baseline CNL and the risk of all-cause death 1 year post-discharge in patients with sepsis, even after adjusting for potential confounding factors. CNL, which includes physical, psychological, and social factors, is assessed by experts from different disciplines using uniform national standards and reflects the health status of older patients [8]. Patients with high CNLs at baseline exhibited low levels of self-care or poor cognitive function prior to the development of sepsis. Consequently, compared with those with no care needs at baseline, these patients were vulnerable and were at a significantly higher risk of all-cause mortality after developing sepsis. Patients with a high CNL at baseline should be considered high-risk and monitored carefully in terms of clinical management and prognostic follow-ups. Further in-depth studies must be conducted to explore targeted interventions such as changes of post-sepsis care practices [34] to improve the survival rates of patients with high CNL at baseline post-discharge.
Previous studies have generally viewed sepsis from the perspective of hospital admission as the starting point. This approach may be suitable for healthy patients; however, it is inappropriate for older patients with poor health statuses [2]. The present study provides insight into the association between the pre-sepsis status and mortality risk 1 year post-discharge. Furthermore, it also describes the changes in CNL from pre-admission to 1 year post-discharge. The best practices outlined in the International Guidelines for Management of Sepsis and Septic Shock 2021 for adult patients with sepsis or septic shock include discussing goals of care and prognosis with patients and their families and conducting follow-ups for physical, cognitive, and emotional problems post-discharge [34]. The findings of the present study provide important reference points for practical recommendations. For patients with sepsis who have a high CNL level pre-admission, we recommend adequate and standardized treatment for sepsis as outlined in the latest guidelines to minimize deterioration in prognosis, along with comprehensive rehabilitation, and post-discharge care and follow-up [34,35,36].
Limitations
The present study has certain limitations. First, the accuracy of the definition of sepsis remains uncertain. The definition of sepsis requires laboratory data for the Sequential Assessment of Sepsis-Related Organ Failure score [22]. However, ICD codes were used to define organ dysfunction, as described in previous studies, due to the absence of laboratory data in the claims dataset [5, 21], potentially affecting the accuracy of the sepsis diagnosis. Second, septic shock could not be analyzed according to the sepsis-3 criteria as the serum lactate data were not available [22]. Septic shock is the most severe form of sepsis, characterized by multiple organ failure and life-threatening conditions such as low blood pressure, resulting in a higher mortality rate compared to sepsis alone [22]. Therefore, future studies must explore the association between the CNL at baseline and mortality in patients with septic shock. Third, the findings of the present study may have limited applicability to other countries as the structure of long-term care differs from country to country; the CNL in this study was specifically obtained in Japan. Fourth, residual confounders may have affected our results as this was a retrospective study conducted using an administrative database. Fifth, due to the data being sourced from healthcare claims data, it was not possible to ascertain specific causes of death. Therefore, only all-cause mortality was analyzed. Sixth, we acknowledged that our study was constrained by the lack of data on accepted measures for assessing acute disease severity, intensity of treatment, and withholding of care. This limitation may affect our assessment of association between baseline CNL and mortality among patients with sepsis. Seventh, we could not exclude the impact of cancer on our results, even though we adjusted for cancer in the multivariable model. The proportion of cancer patients was lower among those with high CNL in Table 1, which may be due to the higher in-hospital mortality rate among cancer patients with high CNL. Eighth, a significant proportion of patients were classified under the “unknown” category for infection sites. This classification was based on prior researches using Japanese insurance data [5, 37]. In our study, 36.9% of patients fell into this category, aligning with the range reported in previous studies (23–44%) [5, 37]. However, since the claims data we used do not include detailed infection site information, our ability to accurately identify the source of infection was limited.
Conclusions
Elevated CNLs and mortality were observed in patients with sepsis 1 year post-discharge. Even patients with no care needs at baseline developed care needs due to functional deterioration after discharge. Older patients with sepsis with high baseline CNLs had a high association of all-cause mortality a year post-discharge.
Availability of data and materials
The authors do not have permission to share the data. Inquiries regarding the data used in the present study can be addressed to the corresponding author. Researchers interested in LIFE studies can refer to https://life.hcam.med.kyushu-u.ac.jp/.
Abbreviations
- ADL:
-
Activities of daily living
- CI:
-
Confidence intervals
- CNL:
-
Care needs level
- HR:
-
Hazard ratio
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- LIFE:
-
Longevity Improvement and Fair Evidence
- LTC:
-
Long-term care
- SL:
-
Support level
References
Cecconi M, Evans L, Levy M, Rhodes A. Sepsis and septic shock. Lancet. 2018;392(10141):75–87. https://doi.org/10.1016/s0140-6736(18)30696-2.
Prescott HC, Angus DC. Enhancing recovery from sepsis: a review. JAMA. 2018;319(1):62–75. https://doi.org/10.1001/jama.2017.17687.
Prescott HC, Langa KM, Liu V, Escobar GJ, Iwashyna TJ. Increased 1-year healthcare use in survivors of severe sepsis. Am J Respir Crit Care Med. 2014;190(1):62–9. https://doi.org/10.1164/rccm.201403-0471OC.
Bauer M, Gerlach H, Vogelmann T, Preissing F, Stiefel J, Adam D. Mortality in sepsis and septic shock in Europe, North America and Australia between 2009 and 2019—results from a systematic review and meta-analysis. Crit Care. 2020;24(1):239. https://doi.org/10.1186/s13054-020-02950-2.
Imaeda T, Nakada TA, Takahashi N, Yamao Y, Nakagawa S, Ogura H, et al. Trends in the incidence and outcome of sepsis using data from a Japanese nationwide medical claims database-the Japan Sepsis Alliance (JaSA) study group. Crit Care. 2021;25(1):338. https://doi.org/10.1186/s13054-021-03762-8.
Shankar-Hari M, Ambler M, Mahalingasivam V, Jones A, Rowan K, Rubenfeld GD. Evidence for a causal link between sepsis and long-term mortality: a systematic review of epidemiologic studies. Crit Care. 2016;20:101. https://doi.org/10.1186/s13054-016-1276-7.
Iwagami M, Tamiya N. The long-term care insurance system in Japan: past, present, and future. JMA J. 2019;2(1):67–9. https://doi.org/10.31662/jmaj.2018-0015.
Tsutsui T, Muramatsu N. Care-needs certification in the long-term care insurance system of Japan. J Am Geriatr Soc. 2005;53(3):522–7. https://doi.org/10.1111/j.1532-5415.2005.53175.x.
Matsuda T, Iwagami M, Suzuki T, Jin X, Watanabe T, Tamiya N. Correlation between the Barthel Index and care need levels in the Japanese long-term care insurance system. Geriatr Gerontol Int. 2019;19(11):1186–7. https://doi.org/10.1111/ggi.13777.
Lin HR, Otsubo T, Imanaka Y. The effects of dementia and long-term care services on the deterioration of care-needs levels of the elderly in Japan. Medicine. 2015;94(7): e525. https://doi.org/10.1097/md.0000000000000525.
Lin HR, Otsubo T, Imanaka Y. Survival analysis of increases in care needs associated with dementia and living alone among older long-term care service users in Japan. BMC Geriatr. 2017;17(1):182. https://doi.org/10.1186/s12877-017-0555-8.
Takahashi K, Saito M, Inaba S, Morofuji T, Aisu H, Sumimoto T, et al. Contribution of the long-term care insurance certificate for predicting 1-year all-cause readmission compared with validated risk scores in elderly patients with heart failure. Open Heart. 2016;3(2): e000501. https://doi.org/10.1136/openhrt-2016-000501.
Shankar-Hari M, Rubenfeld GD, Ferrando-Vivas P, Harrison DA, Rowan K. Development, validation, and clinical utility assessment of a prognostic score for 1-year unplanned rehospitalization or death of adult sepsis survivors. JAMA Netw Open. 2020;3(9): e2013580. https://doi.org/10.1001/jamanetworkopen.2020.13580.
Soussi S, Sharma D, Jüni P, Lebovic G, Brochard L, Marshall JC, et al. Identifying clinical subtypes in sepsis-survivors with different one-year outcomes: a secondary latent class analysis of the FROG-ICU cohort. Crit Care. 2022;26(1):114. https://doi.org/10.1186/s13054-022-03972-8.
Pandolfi F, Brun-Buisson C, Guillemot D, Watier L. One-year hospital readmission for recurrent sepsis: associated risk factors and impact on 1-year mortality—a French nationwide study. Crit Care. 2022;26(1):371. https://doi.org/10.1186/s13054-022-04212-9.
Engoren M, Maile MD, Seelhammer T, Freundlich RE, Schwann TA. Postdischarge survival after sepsis: a cohort study. Anesth Analg. 2023;137(6):1216–25. https://doi.org/10.1213/ane.0000000000006744.
Hodgson CL, Higgins AM, Bailey M, Barrett J, Bellomo R, Cooper DJ, et al. Comparison of 6-month outcomes of sepsis versus non-sepsis critically ill patients receiving mechanical ventilation. Crit Care. 2022;26(1):174. https://doi.org/10.1186/s13054-022-04041-w.
Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787–94. https://doi.org/10.1001/jama.2010.1553.
Fukuda H, Ishiguro C, Ono R, Kiyohara K. The longevity improvement & fair evidence (LIFE) study: overview of the study design and baseline participant profile. J Epidemiol. 2023;33(8):428–37. https://doi.org/10.2188/jea.JE20210513.
Rhee C, Dantes R, Epstein L, Murphy DJ, Seymour CW, Iwashyna TJ, et al. Incidence and trends of sepsis in US Hospitals using clinical vs claims data, 2009–2014. JAMA. 2017;318(13):1241–9. https://doi.org/10.1001/jama.2017.13836.
Oami T, Imaeda T, Nakada TA, Abe T, Takahashi N, Yamao Y, et al. Mortality analysis among sepsis patients in and out of intensive care units using the Japanese nationwide medical claims database: a study by the Japan Sepsis Alliance study group. J Intensive Care. 2023;11(1):2. https://doi.org/10.1186/s40560-023-00650-x.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–10. https://doi.org/10.1001/jama.2016.0287.
Ohbe H, Nakajima M, Miyamoto Y, Shibahashi K, Matsui H, Yasunaga H, et al. 1-Year functional outcomes after cardiopulmonary resuscitation for older adults with pre-existing long-term care needs. Age Ageing. 2023;52(5):afad072. https://doi.org/10.1093/ageing/afad072.
Ohbe H, Ouchi K, Miyamoto Y, Ishigami Y, Matsui H, Yasunaga H, et al. One-year functional outcomes after invasive mechanical ventilation for older adults with preexisting long-term care-needs. Crit Care Med. 2023;51(5):584–93. https://doi.org/10.1097/ccm.0000000000005822.
Kubo S, Noda T, Nishioka Y, Myojin T, Nakanishi Y, Furihata S, et al. Mortality tracking using the national database of health insurance claims and specific health checkups of Japan (NDB). Jpn J Med Inform. 2021;40(6):319–35. https://doi.org/10.14948/jami.40.319.
Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. Lancet. 2020;395(10219):200–11. https://doi.org/10.1016/s0140-6736(19)32989-7.
Thompson K, Taylor C, Jan S, Li Q, Hammond N, Myburgh J, et al. Health-related outcomes of critically ill patients with and without sepsis. Intensive Care Med. 2018;44(8):1249–57. https://doi.org/10.1007/s00134-018-5274-x.
Pandolfi F, Brun-Buisson C, Guillemot D, Watier L. Care pathways of sepsis survivors: sequelae, mortality and use of healthcare services in France, 2015–2018. Crit Care. 2023;27(1):438. https://doi.org/10.1186/s13054-023-04726-w.
Fleischmann-Struzek C, Rose N, Freytag A, Spoden M, Prescott HC, Schettler A, et al. Epidemiology and costs of postsepsis morbidity, nursing care dependency, and mortality in Germany, 2013 to 2017. JAMA Netw Open. 2021;4(11):e2134290. https://doi.org/10.1001/jamanetworkopen.2021.34290.
Liu V, Lei X, Prescott HC, Kipnis P, Iwashyna TJ, Escobar GJ. Hospital readmission and healthcare utilization following sepsis in community settings. J Hosp Med. 2014;9(8):502–7. https://doi.org/10.1002/jhm.2197.
Jones TK, Fuchs BD, Small DS, Halpern SD, Hanish A, Umscheid CA, et al. Post-acute care use and hospital readmission after sepsis. Ann Am Thorac Soc. 2015;12(6):904–13. https://doi.org/10.1513/AnnalsATS.201411-504OC.
Hästbacka J, But A, Strandberg G, Lipcsey M. Risk of malignant disease in 1-year sepsis survivors, a registry-based nationwide follow-up study. Crit Care. 2023;27(1):376. https://doi.org/10.1186/s13054-023-04654-9.
Wang HE, Kabeto MM, Gray M, Wadley VG, Muntner P, Judd SE, et al. Trajectory of cognitive decline after sepsis. Crit Care Med. 2021;49(7):1083–94. https://doi.org/10.1097/ccm.0000000000004897.
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: International Guidelines for Management of Sepsis and Septic Shock 2021. Crit Care Med. 2021;49(11):e1063–143. https://doi.org/10.1097/ccm.0000000000005337.
Egi M, Ogura H, Yatabe T, Atagi K, Inoue S, Iba T, et al. The Japanese Clinical Practice Guidelines for management of sepsis and septic shock 2020 (J-SSCG 2020). J Intensive Care. 2021;9(1):53. https://doi.org/10.1186/s40560-021-00555-7.
Jouffroy R, Djossou F, Neviere R, Jaber S, Vivien B, Heming N, et al. The chain of survival and rehabilitation for sepsis: concepts and proposals for healthcare trajectory optimization. Ann Intensive Care. 2024;14(1):58. https://doi.org/10.1186/s13613-024-01282-6.
Oami T, Abe T, Nakada TA, Imaeda T, Aizimu T, Takahashi N, et al. Association between hospital spending and in-hospital mortality of patients with sepsis based on a Japanese nationwide medical claims database study. Heliyon. 2024;10(1): e23480. https://doi.org/10.1016/j.heliyon.2023.e23480.
Acknowledgements
We thank all the municipalities for their participation in the LIFE Study. This study was supported by the Advanced Clinical Epidemiology Investigator’s Research Project at Osaka University Graduate School of Medicine.
Funding
This study was funded by Grants-in-Aid for Scientific Research, Fundamental Research A, from the Japan Society for the Promotion of Science (grant number JP20H00563) and the JST FOREST Program (grant number JPMJFR205J). This study was also supported by the Advanced Clinical Epidemiology Investigator’s Research Project at Osaka University Graduate School of Medicine (Osaka University OUMP 3–1 and 1–3).
Author information
Authors and Affiliations
Contributions
HF designed the Longevity Improvement and Fair Evidence (LIFE)-based study and collected relevant data. FM and MM managed the LIFE data. SG, AT, TK, LZ, NN, YS, MK, and SK designed the study. SG performed statistical analyses and drafted the manuscript. All authors reviewed and revised the manuscript for significant intellectual content and consent to the its submission for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Kyushu University Institutional Review Board for Clinical Research (approval no. 22114) and Osaka University Institutional Review Board (approval no. 21107).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ge, S., Zha, L., Tanaka, A. et al. Post-discharge functional outcomes in older patients with sepsis. Crit Care 28, 281 (2024). https://doi.org/10.1186/s13054-024-05080-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-024-05080-1