Abstract
Background
The precise identification of the underlying causes of infectious diseases, such as severe pneumonia, is essential, and the development of next-generation sequencing (NGS) has enhanced the effectiveness of pathogen detection. However, there is limited information on the systematic assessment of the clinical use of targeted next-generation sequencing (tNGS) in cases of severe pneumonia.
Methods
A retrospective analysis was conducted on 130 patients with severe pneumonia treated in the ICU from June 2022 to June 2023. The consistency of the results of tNGS, metagenomics next-generation sequencing (mNGS), and culture with the clinical diagnosis was evaluated. Additionally, the results for pathogens detected by tNGS were compared with those of culture, mNGS, and quantitative reverse transcription PCR (RT-qPCR). To evaluate the efficacy of monitoring severe pneumonia, five patients with complicated infections were selected for tNGS microbiological surveillance. The tNGS and culture drug sensitisation results were then compared.
Results
The tNGS results for the analysis of the 130 patients showed a concordance rate of over 70% with clinical diagnostic results. The detection of pathogenic microorganisms using tNGS was in agreement with the results of culture, mNGS, and RT-qPCR. Furthermore, the tNGS results for pathogens in the five patients monitored for complicated infections of severe pneumonia were consistent with the culture and imaging test results during treatment. The tNGS drug resistance results were in line with the drug sensitivity results in approximately 65% of the cases.
Conclusions
The application of tNGS highlights its promise and significance in assessing the effectiveness of clinical interventions and providing guidance for anti-infection therapies for severe pneumonia.
Similar content being viewed by others
Background
Pneumonia is a globally prevalent infectious disease affecting various age groups. Inadequate treatment can lead to severe pneumonia, potentially causing multiorgan failure and death [1,2,3,4,5]. The timely and accurate identification of pathogens is crucial for improving the chances of survival in critically ill patients. Delayed or insufficient antimicrobial therapy may result in unfavourable outcomes [6,7,8]. Multiple pathogenic bacterial infections are common in people with long-term medical conditions or those who have received treatment, particularly during the COVID-19 pandemic [1, 9]. Hence, identifying pathogens is crucial for treating severe pneumonia.
Culture methods are extensively used to diagnose pneumonia, offering the benefits of cost-effectiveness, quantifying the presence of pathogens, and facilitating antibiotic susceptibility testing; however, cultures can be time-consuming and less effective in detecting atypical infections [10]. Next-generation sequencing (NGS) is a rapid and comprehensive method for detecting respiratory infections. It can better detect these pathogens than traditional assays and identify them in patients who test negative in culture tests [11]. The main challenges of NGS are its cost, complexity, and standardisation [12,13,14].
Metagenomics next-generation sequencing (mNGS) enables the quick and unbiased identification of harmful viruses, bacteria, fungi, and parasites. It can identify severe diseases and challenging infections that warrant urgent care [13, 15, 16]. Metagenomics is anticipated to become the first-line detection method for severe pneumonia [17]. Previously, we reported the significance of mNGS in ARDS diagnosis, treatment, and prognosis [16, 18]. Nevertheless, mNGS is a costly method for simultaneously conducting DNA and RNA tests and is influenced by human genetics. It yields relatively low data readouts from the pathogen genome, making its use challenging for regular and ongoing disease monitoring [19]. Unlike mNGS, targeted next-generation sequencing (tNGS) requires the development of precise primers or probes for pre-selected pathogens for panel construction. This method is cost-effective, highly specific, requires minimal sample quantities, and can avoid influence by human DNA [20]. tNGS has been used to identify pathogens in lung, bloodstream, bone and joint, and mycobacterial infections [21,22,23,24]. It has also been used to detect genes associated with treatment resistance [25, 26], demonstrating its potential for clinical applications [27, 28]. To date, the systematic evaluation of the clinical use of tNGS for severe pneumonia has been insufficient. This retrospective study therefore assessed the use of tNGS in the clinical management of severe pneumonia.
Materials and methods
Case recruitment and sample collection
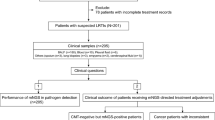
A retrospective analysis was conducted on patients with severe pneumonia admitted to the ICU of Jiangmen Central Hospital between June 2022 and June 2023. The study protocol was approved by the Ethics Review Committee of Jiangmen Central Hospital (No: 2021-15). Patients or their legal representatives provided their signatures on an informed consent form. A total of 130 patients were identified for analysis, and their clinical data were collected (Fig. 1A). The inclusion criteria were as follows: (1) meeting the diagnostic criteria for severe pneumonia and (2) being 18 years of age or older. The exclusion criteria included (1) the premature discontinuation of treatment and (2) insufficient case data.
All the patients underwent extubation and mechanical ventilation in the ICU. Fibreoptic bronchoscopy was used to acquire bronchoalveolar lavage fluid (BALF) or sputum for microbiological testing. Pharyngeal swab samples were obtained from a subset of the patients. Upon the transfer of the patients to the ICU, we retained initial samples from patients who had received a diagnosis of severe pneumonia within 24 h. Additional samples were collected weekly for re-examination. Subsequently, the samples were sent to a clinical laboratory for microbiological analyses. The remaining specimens were sent to the clinical experimental centre and dispatched to the GenePlus-Beijing Institute (Beijing, China) for mNGS and tNGS (Fig. 1B), and Hybribio Co., Ltd. (Guangzhou, China) conducted quantitative reverse transcription PCR (RT-qPCR) analyses.
Clinical treatment of patients with severe pneumonia
Patients received treatment based on the Chinese guidelines for diagnosing and treating community-acquired pneumonia in adults [29] and the Chinese guidelines for diagnosing hospital-acquired pneumonia and ventilator-associated pneumonia in adults [30]. These guidelines were used in combination with the clinical indicators of infection and imaging data. If the exact microbes that caused the infection could not be positively identified, empirical treatments with anti-infection drugs were administered, and antimicrobial therapy was subsequently modified based on the microbiological test results.
Concordance evaluation
Evaluating the concordance of the tNGS, mNGS, and culture results relative to the clinical diagnoses involved a thorough assessment by three experienced clinicians holding the title of associate senior clinician or higher and having over 10 years of ICU experience. The clinicians integrated the results to reach final diagnoses. The diagnoses considered the clinical characteristics of the patients, results of standard pathogenic tests, NGS results, pathological data, imaging findings, and other relevant factors.
NGS, culture, and RT-qPCR microbiology testing
Of 130 samples, 126 were BALF, and the remaining 4 were sputum samples (Mycobacterium tuberculosis infection). The detailed steps are provided in Additional file 1.
Statistical analysis
Continuous variables that exhibited a normal distribution were represented as the mean ± standard deviation (\(\overline{\text{x}}\) ± s), but those that did not conform to a normal distribution were represented as the median with the interquartile range [M (P25, P75)]. Group comparisons were conducted using unpaired t-tests or Mann–Whitney U tests. The frequencies and percentages [N (%)] were utilised for categorical variables, and comparisons between groups were conducted using either the χ2 test. The positive group identified using both methods served as the reference diagnostic criterion. A graph depicting the receiver operating characteristic (ROC) curve and area under the curve (AUC), together with a 95% confidence interval, was generated. Heatmaps were generated using the ggplot package in R or Multiple Experiment Viewer software. Data analyses were performed using GraphPad Prism 9.3 software (GraphPad Software, Inc.), R 4.3.1 software (http://www.r-project.org, The R Foundation), and Multiple Experiment Viewer software (https://sourceforge.net/projects/mev-tm4/). Differences were deemed statistically significant if P < 0.05 (two-sided).
Results
General information on the patients
A total of 130 patients with severe pneumonia were included in this study. The patient demographic information, underlying medical conditions, and specific treatments received in the ICU are presented in Table 1.
Evaluation of the concordance of the three methods (tNGS, culture, and mNGS) with clinical diagnoses
We evaluated the concordance among the three methods and clinical diagnoses in several subcategories of infections (Fig. 2A, B). In Group 1, all three assays exhibited a clinical concordance of more than 85% (Fig. 2C). The clinical concordance between mNGS and culture was lower than that of tNGS in Groups 2 and 4; the concordance rates of tNGS were 76.0% and 86.7%, respectively (Fig. 2D, F). Groups 3 and 5 exhibited considerably worse clinical culture concordance than did the other methods. The outcomes of tNGS and mNGS were comparable, with tNGS attaining concordance rates of 88.2% and 72.2%, respectively (Fig. 2E, G).
The infection status of 130 patients as well as the evaluation of the concordance between three methods (tNGS, culture, and mNGS) and the clinical diagnostic results. A Categorization of pathogenic infections in patients. B The subgroup profiles in which the concordance evaluation was conducted. C–G Evaluation of the concordance of tNGS, culture and mNGS methods with clinical diagnosis in different subgroups. Concordant and partial concordant (not affecting clinical judgement) were deemed to be consistent with the final diagnoses, and the remaining cases were considered incongruous with the final diagnoses. (H) Differences in clinical concordance between tNGS and the other two methods were compared using the χ2 test
The clinical consistency discrepancy between tNGS and the other methods was assessed. The concordance between tNGS and diagnosis was substantially greater (P < 0.001) than that between culture and mNGS in Groups 2 and 4 (Fig. 2H). This investigation was conducted during the COVID-19 and influenza epidemics. Both COVID-19 and influenza viruses belong to the category of RNA viruses; however, only DNA sequencing was used for mNGS. This may have influenced the decreased clinical consistency of mNGS in Groups 2 and 4. Based on the results, tNGS demonstrated excellent clinical diagnostic concordance across all infection types.
Comparison between tNGS with culture for the detection of common clinical microorganisms
We selected 24 bacteria or fungi frequently found in clinical diagnoses and conducted a comparative analysis using tNGS and culture techniques. A cluster analysis revealed that almost 70% of the detections made using tNGS and culture had a concordance rate of up to 90%. Most of the disease-causing bacteria, which had a detection concordance of less than 90%, were identified as positive by tNGS but were undetected by culture (tNGS+culture−) (Fig. 3A).
Comparison of tNGS with culture for clinical microorganism detection. A Cluster analysis of pathogen detection in tNGS versus culture. B–H When tNGS detection was positive, it was divided into two groups with positive or negative culture detection and the RPM values of tNGS of the two groups were compared. The ROC curves were plotted using both positive tNGS and culture results as criteria
Additional statistical tests were conducted to investigate the factors contributing to detection rates below 90%. These tests disclosed that RPM values for tNGS were notably higher (P < 0.05) in (tNGS+culture+) samples than for (tNGS+culture−) samples (Fig. 3B–F). Compared to that for Corynebacterium striatum, Pseudomonas aeruginosa, and Acinetobacter baumannii (AUC > 0.800), there was a lower degree of differentiation for Stenotrophomonas maltophilia and Klebsiella pneumoniae (AUC < 0.750). For Streptococcus pneumoniae and Candida albicans, comparisons were not made because of the limited number of samples (Fig. 3G–H). tNGS is, therefore, more sensitive than culture in identifying bacteria and fungi.
Comparison between tNGS and mNGS for the detection of common clinical microorganisms
We selected 31 microorganisms commonly encountered in clinical diagnoses, including bacteria, fungi, and viruses, and compared their detection results using tNGS and mNGS. A cluster analysis showed that approximately 80% of the tNGS and mNGS detection results had a concordance rate of up to 90%. Pathogenic microorganisms with a detection concordance below 90% were predominantly positive in tNGS and negative in mNGS (tNGS+mNGS−) (Fig. 4A). Common pathogenic microorganisms, including Streptococcus pneumoniae, Staphylococcus aureus, Pseudomonas aeruginosa, Acinetobacter baumannii, and Klebsiella pneumoniae, were identified with an accuracy rate of ≥ 83%. In contrast, atypical harmful microorganisms, including Legionella pneumophila, Pneumocystis jirovecii, Chlamydia pneumoniae, and Mycoplasma pneumoniae, were detected with a perfect concordance rate of ≥ 95%.
Comparison of tNGS with mNGS for clinical microorganism detection. A Cluster analysis of pathogen detection in tNGS versus mNGS. B–G When tNGS detection was positive, it was divided into two groups with positive or negative mNGS detection, and the RPM values of tNGS of the two groups were compared. In addition, when mNGS was positive, it was categorized into two groups with positive or negative tNGS results, and the RPM values of mNGS in the two groups were compared
We further investigated the reasons for the detection rates below 90%. For Epstein-barr virus (EBV) and Human Cytomegalovirus (HCMV), the RPM of tNGS in (tNGS+mNGS+) samples was not significantly different (P > 0.05) from that of (tNGS+mNGS−) samples. Moreover, there were no cases in which the (tNGS−mNGS+) samples (Fig. 4B, C). A possible explanation for this may be the low specificity of the probes used to detect EBV and HCMV in the tNGS panel.
For Corynebacterium striatum, Human alphaherpesvirus 1, and Acinetobacter baumannii, the RPM values for tNGS were significantly higher (P < 0.001) in (tNGS+mNGS+) samples than in (tNGS+mNGS−) samples. Moreover, there was no notable disparity (P > 0.05) in the RPM values of mNGS between (tNGS+mNGS+) samples and (tNGS−mNGS+) samples. The RPM values of mNGS in (tNGS−mNGS+) samples were nearly zero (Fig. 4D–F). Additionally, the RPM values of tNGS and mNGS for Candida albicans were relatively low, suggesting that tNGS is less effective in detecting Candida albicans (Fig. 4G). tNGS and mNGS therefore possess comparable capabilities for identifying harmful microbes; however, their effectiveness in identifying certain viruses needs to be improved.
Comparison between tNGS and RT-qPCR for the detection of COVID-19 and influenza viruses
To evaluate the efficacy of tNGS in detecting RNA viruses, we compared tNGS and RT-qPCR in detecting COVID-19 and influenza A/B viruses. The concordance between RT-qPCR and tNGS exceeded 88% (Fig. 5A).
Comparison of tNGS with RT-qPCR for COVID-19, influenza A virus and influenza B virus detections. A Cluster analysis of tNGS versus RT-qPCR for COVID-19, influenza A virus and influenza B virus detections. B and E In COVID-19 and influenza A virus, the RPM values of tNGS in the two groups were compared. The ROC curves were plotted using both positive tNGS and RT-qPCR results as criteria. C, D, and F In COVID-19 and influenza A virus, the CT values of the RT-qPCR of the two groups are compared
For the influenza B virus, the tNGS and RT-qPCR results were consistent. When compared with the COVID-19 detection results, the RPM of tNGS was considerably higher (P = 0.010) in (tNGS+qPCR+) samples than in (tNGS+qPCR−) samples (Fig. 5B). The CT value of qPCR was also markedly lower (P < 0.001) in (tNGS+qPCR+) samples than in (tNGS−qPCR+) samples (Fig. 5C–D). The N and ORF1ab genes were the two components of the COVID-19 qPCR detection, and a higher viral load was indicated by a lower CT value. Both tNGS and qPCR therefore exhibited excellent sensitivity. Findings similar to those of COVID-19 were also observed for the influenza A virus. Nevertheless, tNGS showed limited discriminatory ability because there were only two (tNGS+qPCR−) samples (Fig. 5E–F). Therefore, tNGS is proficient in identifying COVID-19 and influenza A/B viruses, and its detection capability is likely equivalent to that of qPCR.
We also performed a preliminary analysis of COVID-19 viral loads at different locations in 19 cases from the same patient. In approximately 75% of the patients, the CT values of the qPCR for both COVID-19 genes in the swab samples were lower than those of the BALF samples. The viral loads in the swab samples were therefore relatively higher than those in the BALF (Additional file 2: Supplementary Fig. 1).
An assessment of tNGS for clinical microbial surveillance
To assess the effectiveness of tNGS in monitoring the conditions of critically ill patients, we examined five patients who presented with complicated infections. The outcomes of tNGS microbial semi-quantitative testing were compared with culture results throughout the monitoring of the treatment process. Imaging data and medications for anti-infection therapy were also considered. On average, the tNGS results were consistent with the culture and imaging findings, demonstrating that tNGS is effective in tracking microorganisms during treatments for severe pneumonia. The detailed description of the case is provided in Additional file 3.
To evaluate the results of tNGS resistance detection, three prevalent drug-resistant bacteria were chosen to compare tNGS and culture drug sensitivity results. The concordance between the tNGS and drug sensitivity results was 65.6% for Pseudomonas aeruginosa, 68.4% for Acinetobacter baumannii, and 65.6% for Klebsiella pneumoniae (Additional file 2: Supplementary Fig. 2).
Discussion
Microbial infections commonly associated with severe pneumonia include those caused by bacterial, fungal, viral, and atypical pathogens [31]. Identifying pathogenic microorganisms is essential for diagnosing and treating severe pneumonia and can enable physicians to develop rational antibiotic treatment plans that reduce drug resistance and enhance infection control. This study found that tNGS results had a concordance rate of > 70% with clinical diagnoses in patients with severe pneumonia. The results of tNGS were consistent with those of culture, mNGS, and RT-qPCR. Several studies have exhibited similar sensitivity and specificity between tNGS and mNGS in different sample types [12, 32]. The tNGS panel used in this study was a primer or probe specifically constructed for 306 pathogens (Additional file 4). We found that tNGS has high detection efficacy for both common and atypical pathogenic microorganisms, and there were no unusual or unique pathogens that were beyond the detection capabilities of tNGS. Furthermore, tNGS has a superior average detection time compared to culture or mNGS. We chose four tuberculosis patients to investigate the efficacy of the tNGS test, and all of them tested positive for Mycobacterium tuberculosis. Importantly, tNGS allows the simultaneous acquisition of data on drug resistance genes and pathogen reports. This would enable clinics to promptly identify pathogens and provide information on drug resistance, thereby facilitating treatment guidance.
Nonetheless, this study identified pathogens exhibiting a slightly lower level of concordance (< 90%) with the reference technique. This can be attributed to the technical aspects of tNGS. The enrichment process enhances the minimum detectable level of tNGS, allowing the identification of diseases that cannot be detected using culture or mNGS. Examples include Acinetobacter baumannii, Pseudomonas aeruginosa, and Corynebacterium striatum. Previous studies have also shown that enrichment enhances both the fragment reads of pathogens and coverage of the pathogen genome, thereby aiding accurate pathogen identification [14, 20]. The ability of tNGS to detect a greater number of infections than culture methods may be due to variability in the minimum detection limits among various diseases. Examining tNGS probes targeting Stenotrophomonas maltophilia and Klebsiella pneumoniae demonstrated that these probes were built with a higher degree of caution than probes designed for other strains specific to these species. The design prioritised genus-level sequences and inadequately covered species-specific sequences, leading to a failure to categorise species-level readings in many instances and a somewhat higher limit of detection. An analogous issue has been reported before [12]. Our data suggest that the minimum detectable level of tNGS for EBV and HCMV is less significant than that for other viruses in comparison with mNGS. The probes used for all viruses encompassed the complete genome and exhibited minimal variation in the tNGS design. Notably, HCMV and EBV can also be detected in the human respiratory system, which may affect patient outcomes [33]. In addition, low Candida albicans and Aspergillus loads may have been undetected, likely due to the vast genome of the fungus and inadequate probe laydowns. A recent survey also emphasised the necessity of a focused design for tNGS to identify fungi [12].
In this study, five patients with complex infections underwent culture and tNGS semi-quantitative microbiological surveillance. The anti-infection drug prescriptions were modified based on the findings of microbiological tests and additional clinical indicators. tNGS, when used as an enhanced internal reference, is therefore valuable for monitoring pathogenic microorganisms during the treatment of severe pneumonia. Several studies have indicated that adopting qPCR or mNGS techniques to continuously monitor variations in pathogens can be beneficial for understanding patient conditions [34, 35]. When using mNGS to identify pathogens, it is not feasible to evaluate changes in pathogens longitudinally based on the detected reads. Fortunately, the inclusion of specific internal references mitigated the influence of the host and enabled comparisons across samples collected at different timepoints [36, 37].
Numerous studies have explored the benefits of tNGS in detecting drug resistance [26, 38], particularly in tuberculosis resistance [23, 39,40,41]. tNGS may offer clinicians timely information for the appropriate selection of antimicrobial medicines. Although tNGS is proficient in identifying pertinent drug resistance genes, it is still not capable of substituting for drug sensitivity outcomes.
The major limitation of this study is that the comparison between RNA sequencing using tNGS and mNGS was incomplete because the mNGS assay only uses DNA sequencing. In addition, the duration of this investigation was brief, and the number of samples was restricted. The samples were primarily collected during the COVID-19 and influenza epidemics, leading to minimal detection of DNA virus. Further studies are required to increase the number of samples and integrate prospective and controlled trials, thereby broadening our understanding of the clinical significance of tNGS testing for severe pneumonia.
Conclusion
Although tNGS is more sensitive than conventional culture for identifying pathogens that cause severe pneumonia, it cannot fully replace drug sensitivity results. In contrast to mNGS, however, tNGS has an analogous capacity to identify clinical microorganisms, making it helpful for clinical efficacy monitoring and guiding choices for anti-infection treatments. Although mNGS has a wider detection range and covers more pathogens, tNGS may become widely employed for clinical infectious diseases as costs continue to drop, because it can account for DNA and RNA pathogens in a single assay, which is more advantageous from a health economics perspective.
Availability of data and materials
The datasets analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- ICU:
-
Intensive care unit
- NGS:
-
Next-generation sequencing
- mNGS:
-
Metagenomics next-generation sequencing
- tNGS:
-
Targeted next-generation sequencing
- COVID-19:
-
Corona virus disease 2019
- RT-qPCR:
-
Quantitative reverse transcription PCR
- BALF:
-
Bronchoalveolar lavage fluid
- ROC:
-
Receiver operating characteristic curve
- AUC:
-
Area under the curve
- EBV:
-
Epstein-barr virus
- HCMV:
-
Human cytomegalovirus
References
Cillóniz C, Torres A, Niederman MS. Management of pneumonia in critically ill patients. BMJ (Clin Res Ed). 2021;375:e065871.
De Pascale G, Bello G, Tumbarello M, Antonelli M. Severe pneumonia in intensive care: cause, diagnosis, treatment and management: a review of the literature. Curr Opin Pulm Med. 2012;18(3):213–21.
Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, Gattinoni L, van Haren F, Larsson A, McAuley DF, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315(8):788–800.
Bein T, Grasso S, Moerer O, Quintel M, Guerin C, Deja M, Brondani A, Mehta S. The standard of care of patients with ARDS: ventilatory settings and rescue therapies for refractory hypoxemia. Intens Care Med. 2016;42(5):699–711.
Griffiths MJD, McAuley DF, Perkins GD, Barrett N, Blackwood B, Boyle A, Chee N, Connolly B, Dark P, Finney S, et al. Guidelines on the management of acute respiratory distress syndrome. BMJ Open Respir Res. 2019;6(1):e000420.
Kalil AC, Metersky ML, Klompas M, Muscedere J, Sweeney DA, Palmer LB, Napolitano LM, O’Grady NP, Bartlett JG, Carratalà J, et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the infectious diseases society of America and the American thoracic society. Clin Infect Dis. 2016;63(5):e61–111.
Olson G, Davis AM. Diagnosis and treatment of adults with community-acquired pneumonia. JAMA. 2020;323(9):885–6.
Torres A, Niederman MS, Chastre J, Ewig S, Fernandez-Vandellos P, Hanberger H, Kollef M, Li Bassi G, Luna CM, Martin-Loeches I, et al. ERS/ESICM/ESCMID/ALAT guidelines for the management of hospital-acquired pneumonia and ventilator-associated pneumonia: Guidelines for the management of hospital-acquired pneumonia (HAP)/ventilator-associated pneumonia (VAP) of the European Respiratory Society (ERS), European Society of Intensive Care Medicine (ESICM), European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and Asociación Latinoamericana del Tórax (ALAT). Eur Respir J. 2017;50(3):1700582.
Deng X, Achari A, Federman S, Yu G, Somasekar S, Bártolo I, Yagi S, Mbala-Kingebeni P, Kapetshi J, Ahuka-Mundeke S, et al. Metagenomic sequencing with spiked primer enrichment for viral diagnostics and genomic surveillance. Nat Microbiol. 2020;5(3):443–54.
Buchan BW, Armand-Lefevre L, Anderson N. Molecular diagnosis of pneumonia (including multiplex panels). Clin Chem. 2021;68(1):59–68.
Yang L, Haidar G, Zia H, Nettles R, Qin S, Wang X, Shah F, Rapport SF, Charalampous T, Methe B, et al. Metagenomic identification of severe pneumonia pathogens in mechanically-ventilated patients: a feasibility and clinical validity study. Respir Res. 2019;20(1):265.
Gaston DC, Miller HB, Fissel JA, Jacobs E, Gough E, Wu J, Klein EY, Carroll KC, Simner PJ. Evaluation of metagenomic and targeted next-generation sequencing workflows for detection of respiratory pathogens from bronchoalveolar lavage fluid specimens. J Clin Microbiol. 2022;60(7):e0052622.
Xie Y, Du J, Jin W, Teng X, Cheng R, Huang P, Xie H, Zhou Z, Tian R, Wang R, et al. Next generation sequencing for diagnosis of severe pneumonia: China, 2010–2018. J Infect. 2019;78(2):158–69.
Zhao N, Cao J, Xu J, Liu B, Liu B, Chen D, Xia B, Chen L, Zhang W, Zhang Y, et al. Targeting RNA with Next- and third-generation sequencing improves pathogen identification in clinical samples. Adv Sci (Weinh). 2021;8(23):e2102593.
Qi C, Hountras P, Pickens CO, Walter JM, Kruser JM, Singer BD, Seed P, Green SJ, Wunderink RG. Detection of respiratory pathogens in clinical samples using metagenomic shotgun sequencing. J Med Microbiol. 2019;68(7):996–1002.
Zhang P, Chen Y, Li S, Li C, Zhang S, Zheng W, Chen Y, Ma J, Zhang X, Huang Y, et al. Metagenomic next-generation sequencing for the clinical diagnosis and prognosis of acute respiratory distress syndrome caused by severe pneumonia: a retrospective study. PeerJ. 2020;8:e9623.
Charalampous T, Alcolea-Medina A, Snell LB, Alder C, Tan M, Williams TGS, Al-Yaakoubi N, Humayun G, Meadows CIS, Wyncoll DLA, et al. Routine metagenomics service for ICU patients with respiratory infection. Am J Respir Crit Care Med. 2024;209(2):164–74.
Zhang P, Liu B, Zheng W, Chen Y, Wu Z, Lu Y, Ma J, Lu W, Zheng M, Wu W, et al. Pulmonary microbial composition in sepsis-induced acute respiratory distress syndrome. Front Mol Biosci. 2022;9:862570.
Jacob JJ, Veeraraghavan B, Vasudevan K. Metagenomic next-generation sequencing in clinical microbiology. Indian J Med Microbiol. 2019;37(2):133–40.
Wylie TN, Wylie KM, Herter BN, Storch GA. Enhanced virome sequencing using targeted sequence capture. Genome Res. 2015;25(12):1910–20.
Huang C, Huang Y, Wang Z, Lin Y, Li Y, Chen Y, Chen X, Zhang C, Li W, Zhang W, et al. Multiplex PCR-based next generation sequencing as a novel, targeted and accurate molecular approach for periprosthetic joint infection diagnosis. Front Microbiol. 2023;14:1181348.
Jordana-Lluch E, Gimenez M, Quesada MD, Rivaya B, Marco C, Dominguez MJ, Armestar F, Martro E, Ausina V. Evaluation of the broad-range PCR/ESI-MS technology in blood specimens for the molecular diagnosis of bloodstream infections. PLoS ONE. 2015;10(10):e0140865.
Mansoor H, Hirani N, Chavan V, Das M, Sharma J, Bharati M, Oswal V, Iyer A, Morales M, Joshi A, et al. Clinical utility of target-based next-generation sequencing for drug-resistant TB. Int J Tuberc Lung Dis Off J Int Union Tuberc Lung Dis. 2023;27(1):41–8.
Poulsen SH, Søgaard KK, Fuursted K, Nielsen HL. Evaluating the diagnostic accuracy and clinical utility of 16S and 18S rRNA gene targeted next-generation sequencing based on five years of clinical experience. Infect Dis (London, England). 2023;55(11):767–75.
Murphy SG, Smith C, Lapierre P, Shea J, Patel K, Halse TA, Dickinson M, Escuyer V, Rowlinson MC, Musser KA. Direct detection of drug-resistant Mycobacterium tuberculosis using targeted next generation sequencing. Front Public Health. 2023;11:1206056.
Serpa PH, Deng X, Abdelghany M, Crawford E, Malcolm K, Caldera S, Fung M, McGeever A, Kalantar KL, Lyden A, et al. Metagenomic prediction of antimicrobial resistance in critically ill patients with lower respiratory tract infections. Genome Med. 2022;14(1):74.
Ballester LY, Luthra R, Kanagal-Shamanna R, Singh RR. Advances in clinical next-generation sequencing: target enrichment and sequencing technologies. Expert Rev Mol Diagn. 2016;16(3):357–72.
Deng Z, Li C, Wang Y, Wu F, Liang C, Deng W, Wang Y. Targeted next-generation sequencing for pulmonary infection diagnosis in patients unsuitable for bronchoalveolar lavage. Front Med (Lausanne). 2023;10:1321515.
Respiratory Branch of Chinese Medical Association O: Chinese Adult Community Acquired Pneumonia Diagnosis and Treatment Guide (2016 year version). Chin J Tuberculosis Respir Dis 2016;39(4):253–279.
Department of infectious diseases chinese medical association respiratory branch o: chinese adult hospital acquired pneumonia and ventilator-associated pneumonia diagnosis and treatment guide (2018 Edition). Chin J Tuberculosis Respir Dis 2018;41(4):255–280
Lee KY. Pneumonia, acute respiratory distress syndrome, and early immune-modulator therapy. Int J Mol Sci. 2017;18(2):388.
Li S, Tong J, Liu Y, Shen W, Hu P. Targeted next generation sequencing is comparable with metagenomic next generation sequencing in adults with pneumonia for pathogenic microorganism detection. J Infect. 2022;85(5):e127–9.
Naigeon M, Roulleaux Dugage M, Danlos FX, Boselli L, Jouniaux JM, de Oliveira C, Ferrara R, Duchemann B, Berthot C, Girard L, et al. Human virome profiling identified CMV as the major viral driver of a high accumulation of senescent CD8(+) T cells in patients with advanced NSCLC. Sci Adv. 2023;9(45):eadh0708.
Ziegler I, Cajander S, Rasmussen G, Ennefors T, Mölling P, Strålin K. High nuc DNA load in whole blood is associated with sepsis, mortality and immune dysregulation in Staphylococcus aureus bacteraemia. Infect Dis (London, England). 2019;51(3):216–26.
De Vlaminck I, Khush KK, Strehl C, Kohli B, Luikart H, Neff NF, Okamoto J, Snyder TM, Cornfield DN, Nicolls MR, et al. Temporal response of the human virome to immunosuppression and antiviral therapy. Cell. 2013;155(5):1178–87.
Zhou H, Ouyang C, Han X, Shen L, Ye J, Fang Z, Chen W, Chen A, Ma Q, Hua M, et al. Metagenomic sequencing with spiked-in internal control to monitor cellularity and diagnosis of pneumonia. J Infect. 2022;84(1):e13–7.
Carbo EC, Russcher A, Kraakman MEM, de Brouwer CS, Sidorov IA, Feltkamp MCW, Kroes ACM, Claas ECJ, de Vries JJC. Longitudinal monitoring of DNA viral loads in transplant patients using quantitative metagenomic next-generation sequencing. Pathogens (Basel, Switzerland). 2022;11(2):236.
Gali KV, St Jacques RM, Daniels CID, O’Rourke A, Turner L. Surveillance of carbapenem-resistant organisms using next-generation sequencing. Front Public Health. 2023;11:1184045.
Cabibbe AM, Spitaleri A, Battaglia S, Colman RE, Suresh A, Uplekar S, Rodwell TC, Cirillo DM. Application of targeted next-generation sequencing assay on a portable sequencing platform for culture-free detection of drug-resistant tuberculosis from clinical samples. J Clin Microbiol. 2020;58(10):10.
de Araujo L, Cabibbe AM, Mhuulu L, Ruswa N, Dreyer V, Diergaardt A, Gunther G, Claassens M, Gerlach C, Utpatel C, et al. Implementation of targeted next-generation sequencing for the diagnosis of drug-resistant tuberculosis in low-resource settings: a programmatic model, challenges, and initial outcomes. Front Public Health. 2023;11:1204064.
Schwab TC, Perrig L, Göller PC, Guebely De la Hoz FF, Lahousse AP, Minder B, Günther G, Efthimiou O, Omar SV, Egger M, et al. Targeted next-generation sequencing to diagnose drug-resistant tuberculosis: a systematic review and meta-analysis. Lancet Infect Dis. 2024;22:S1473.
Acknowledgements
We would like to thank Editage (www.editage.cn) for English language editing.
Funding
This study was supported by the grants from the National Natural Science Foundation of China (82273384), the Science and Technology Project of Guangdong Province (2021A1515220180, 2020A1515011421), the China Postdoctoral Science Foundation Grant (2019M660206), the Jiangmen Basic and Applied Basic Research Key Programs (JZ202202) and the Jiangmen Healthcare Science and Technology Program (2024YL01075).
Author information
Authors and Affiliations
Contributions
WZ, YH and XZ conceived and designed the study. PZ, BL and SZ drafted the manuscript, analysed the data and plotted the figures. XC and LZ are responsible for collating the clinical data. XZ, DG and JC helped with data analysis. SX, ZW, XC, and ML were responsible for the organisation of clinical data and judgement of consistency evaluation. WL and MZ were responsible for sample collection and processing. RC, RG and YZ assisted in the interpretation of sequencing data. JW, QF and GH checked and interpreted the microbial detection results. YC and WZ were responsible for patient enrolment and sampling. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The protocol used in this study was approved by the Ethics Review Committee of Jiangmen Central Hospital (No: 2021-15). Informed consent was obtained from patients or their families.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, P., Liu, B., Zhang, S. et al. Clinical application of targeted next-generation sequencing in severe pneumonia: a retrospective review. Crit Care 28, 225 (2024). https://doi.org/10.1186/s13054-024-05009-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-024-05009-8