Abstract
Background
In this study, the concentrations of inflammatory cytokines were measured in the bronchial epithelial lining fluid (ELF) and plasma in patients with acute hypoxemic respiratory failure (AHRF) secondary to severe coronavirus disease 2019 (COVID-19).
Methods
We comprehensively analyzed the concentrations of 25 cytokines in the ELF and plasma of 27 COVID-19 AHRF patients. ELF was collected using the bronchial microsampling method through an endotracheal tube just after patients were intubated for mechanical ventilation.
Results
Compared with those in healthy volunteers, the concentrations of interleukin (IL)-6 (median 27.6 pmol/L), IL-8 (1045.1 pmol/L), IL-17A (0.8 pmol/L), IL-25 (1.5 pmol/L), and IL-31 (42.3 pmol/L) were significantly greater in the ELF of COVID-19 patients than in that of volunteers. The concentrations of MCP-1 and MIP-1β were significantly greater in the plasma of COVID-19 patients than in that of volunteers. The ELF/plasma ratio of IL-8 was the highest among the 25 cytokines, with a median of 737, and the ELF/plasma ratio of IL-6 (median: 218), IL-1β (202), IL-31 (169), MCP-1 (81), MIP-1β (55), and TNF-α (47) were lower.
Conclusions
The ELF concentrations of IL-6, IL-8, IL-17A, IL-25, and IL-31 were significantly increased in COVID-19 patients. Although high levels of MIP-1 and MIP-1β were also detected in the blood samples collected simultaneously with the ELF samples, the results indicated that lung inflammation was highly compartmentalized. Our study demonstrated that a comprehensive analysis of cytokines in the ELF is a feasible approach for understanding lung inflammation and systemic interactions in patients with severe pneumonia.
Similar content being viewed by others
Background
Severe symptoms of coronavirus disease 2019 (COVID-19), such as acute hypoxemic respiratory failure (AHRF) and cytokine release syndrome, often lead to multiorgan failure and death [1]. Research has mainly focused on analyses of factors in the blood to study the impact of COVID-19 on immune function, especially in AHRF patients, due to the ease of access in using blood samples [2,3,4,5]. However, recent reports have shown that the bronchoalveolar immune response in COVID-19 patients presents a distinct local profile that significantly diverges from the immune response observed in the blood of these patients [6,7,8,9]. Notably, COVID-19 patients with AHRF were reported to have lower blood cytokine levels than those with bacterial sepsis [10]. These findings suggest a more complex and subtle immune mechanism in these patients, implying that a compartmentalized reaction within their lungs plays a significant role in the efficacy of therapeutic interventions [11, 12].
In a study of 27 COVID-19 patients with AHRF who required mechanical ventilation (MV), bronchial epithelial lining fluid (ELF) was collected via bronchial microsampling (MS) [13, 14]. This study analyzed 25 cytokine concentrations in both the ELF and plasma of COVID-19 patients using a multiplex bead-based assay and explored the relationship between lung injury severity, as depicted in chest computed tomography (CT) images, and disease duration influenced by viral mutations.
Materials and methods
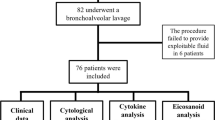
Patients
From March 2021 to March 2022, 27 patients who needed MV for COVID-19-related AHRF at Kyoto Prefectural University of Medicine participated in this study. Their treatments, pneumonia severity index (PSI) [15], Charlson Comorbidity Index (CCI) [16], and other comorbidities were documented (Additional file 1: Table S1, Additional file 2: Table S2). All patients received high-flow nasal cannula therapy before MV. Four patients, including one who received extracorporeal membrane oxygenation (ECMO), did not survive. The control data for both the ELF and plasma cytokine levels were obtained from six healthy volunteers without lung injury who underwent an elective surgery under anesthesia and tracheal intubation.
Bronchial ELF
The bronchial ELF was collected using an MS probe (model BC-402C; Olympus, Tokyo, Japan) immediately after tracheal intubation [13, 14] (Fig. 1A). The probe was inserted into the segmental bronchus of the right lower lobe via an endotracheal tube; approximately 20 μL of ELF was retrieved from each probe; and this procedure was repeated nine times per patient.
A (1) The microsampling probe (model BC-402C, Olympus Tokyo, Japan) used for collecting bronchial epithelial lining fluid (ELF). (2) The probe tip is comprised of a 2.5-mm outer polyethylene sheath and a 1.9-mm inner polyester fiber rod probe, 20 mm in length, attached to a stainless-steel guide wire. (3) The process of extracting ELF by centrifugation. B The study analyzed cytokine concentrations in COVID-19 patients (normal) with acute hypoxemic respiratory failure (AHRF) compared to healthy volunteers (covid). (1) Cytokine concentrations in the ELF and (2) plasma are presented. C The ratio of bronchial ELF/plasma concentrations. The data included a box plot representing the 25th to 75th percentiles (interquartile range, IQR), the median (centerline), and whisker lines extending to the furthest data points within Q1–1.5 × IQR and Q3 + 1.5 × IQR. Outliers were identified beyond these limits. Significant differences (*p < 0.05) between the normal and COVID-19 patient groups are marked with an asterisk and were assessed using the Kruskal‒Wallis test with Bonferroni correction
Cytokine measurement
To analyze 25 types of cytokines (Additional file 3: Table S3), a multiplex bead-based assay (Bio-Plex Pro human cytokine GI-17-Plex for granulocyte colony-stimulating factor (G-CSF), granulocyte–macrophage colony-stimulating factor (GM-CSF), interferon-γ (IFN-γ), interleukin (IL)-1β, IL-2, IL-4, IL-5, IL-6, IL-7, IL-8, IL-10, IL12p70, monocyte chemotactic protein-1 (MCP-1), macrophage inflammatory protein-1β (MIP-1β), and tumor necrosis factor-α (TNF-α), and Th17-15-Plex panels for IL-17A, IL-17F, IL-21, IL-22, IL-23, IL-25, IL-31, IL-33, and soluble CD40 ligand (sCD40L), Bio-Rad, Hercules, CA, USA) was used. Values between zero and less than the manufacturer’s lower limit of quantification (LLOQ) were treated as the LLOQ.
Lung infiltration volume
All 27 patients received CT scans either before transfer or upon admission to the hospital. 3D Slicer software (ver.4.11) was used to calculate the lung infiltration volume (LIV) from chest CT images based on a recently reported method [17, 18].
Statistical analyses
This study used SPSS Version 27 for Kruskal–Wallis nonparametric tests and χ2 tests to compare group medians, with the data presented as medians with interquartile ranges (IQRs).
Results
Cytokine concentrations
The ELF cytokines IL-5, IL-7, IL-12p70, IL-13, and GM-CSF were undetectable in the ELF of 26 patients (Fig. 1B-1). There were increases in the other cytokines, with median levels of IL-8 at 1045.1 [IQR 178.4–11,688.0] pmol/L and IL-6 at 27.6 [5.2–151.2] pmol/L and measurable levels of IL-17A (0.8 [0.2–2.7] pmol/L), IL-25 (15.3 [0.4–3.9] pmol/L), and IL-31 (42.3 [2.4–85.9] pmol/L). The levels of typical inflammatory cytokines, such as MCP-1, MIP-1β, TNF-α, IL-1β, and IL-10, were not significantly greater in the patients than in healthy individuals.
The cytokines IFN-γ, sCD40L, IL-2, IL-4, IL-17A, IL-17F, IL-23, IL-25, and IL-31 were undetectable in the plasma of the 27 patients, and 26 patients had IL-7, IL-12p70, IL-21, and IL-22 levels that were below the detection limits (Fig. 1B-2). The detected cytokines included MCP-1, MIP-1β, IL-8, and TNF-α, and only the levels of MCP-1 (2.5 [1.1–5.0] pmol/L) and MIP-1β (0.7 [0.6–1.6] pmol/L) were significantly greater in the patients than in healthy volunteers. Low plasma levels of G-CSF (0.3 [< 0.3–0.4] pmol/L), IL-6 (0.2 [0.0–0.6] pmol/L), IL-10 (0.1 [< 0.1–0.2] pmol/L), IL-13 (0.03 [< 0.03–0.03] pmol/L), and IL-33 (0.24 [< 0.24–0.24] pmol/L) were also detected.
The ratios of cytokine concentrations in the ELF to those in the plasma were calculated (Fig. 1C). The ELF/plasma ratio was the highest for IL-8, at a median of 737 [IQR 262–11,688] with a detection frequency (%df) of 96.3%, in 27 patients, with the second highest ratios being those of IL-6 (218 [39–1206], %df = 74.1%), IL-1β (202 [21–6434], 3.7%), IL-31 (169 [9–394], 0.0%), MCP-1 (81 [13–323], 96.3%), MIP-1β (55 [0–1121], 96.3%), and TNF-α (47 [7–1560], 81.5%). These ratios underscore the significant disparity in the cytokine concentrations in the ELF and those in the plasma in COVID-19 patients.
Pneumonia severity and cytokine levels
This study assessed 27 COVID-19 patients with AHRF across three pandemic phases in Japan: the 4th wave with the original variant (Mar-Jun 2021), the 5th wave with the Delta variant (Jul–Sep 2021), and the 6th wave with the Omicron variant (Jan-Mar 2022) (Additional file 4: Table S4, Additional file 5: Fig. S1). Notably, the CCI and creatinine levels were lower in the patients of the Delta wave than in those of the 4th wave (Additional file 4: Table S4). The PSI and ferritin levels were greater in the patients of the Omicron wave group than in those of the Delta wave group (Additional file 4: Table S4, Fig. 2B-1).
A The pneumonia severity index (PSI), lung infiltration volume (LIV), C-reactive protein (CRP) concentration in the blood, cytokine concentration in the ELF and plasma, provided therapies and comorbidities were recorded for individual patients in order of LIV, including deceased patients (marked by †). B Age, CRP in blood, total cytokine concentration in the ELF and plasma, LIV, and PSI were analyzed. (1) Comparisons among the chronological groups based on when they developed AHRF due to COVID-19. (2) Comparisons among the groups stratified by the severity of pneumonia using the PSI. (3) Comparison among the groups after patients were stratified by the severity of pneumonia using the LIV. The boxplots show the median, individual data points (colored dots), and whisker lines extending to Q1–1.5 × IQR and Q3 + 1.5 × IQR or the last data point within these values. Points outside these limits are considered outliers. Significance (†p < 0.05) was determined using the Kruskal‒Wallis test with Bonferroni correction for multiple comparisons. AHRF Acute hypoxemic respiratory failure, CRP C-reactive protein, ELF Epithelial lining fluid, IQR Interquartile range, LIV Lung infiltration volume (%) [17, 18], PSI Pneumonia severity index [15]
In a study of 27 patients, subgroups were created based on the PSI and LIV. PSI was categorized as mild (PSI < 90), moderate (90 ≦ PSI < 130), or severe (130 ≦ PSI) (Fig. 2B-2, Additional file 6: Table S5), while LIV was divided into mild (LIV < 40%), moderate (40% ≦ LIV < 50%), or severe (50% ≦ LIV) (Fig. 2A, B-3, Additional file 7: Table S6). The present study revealed that there were more female patients in the moderate PSI group and more older patients in the severe PSI group. Interestingly, the sum of the 25 cytokine concentrations in the ELF and plasma samples did not significantly differ among the PSI groups. The severe LIV subgroup had higher C-reactive protein levels than did the moderate LIV subgroup. Notably, the sum of the 25 cytokine concentrations in the ELF was lower in the severe LIV subgroup than in the moderate group, but no significant difference in plasma cytokine concentrations was observed among the LIV subgroups, indicating that there are different patterns of inflammation based on lung injury severity.
Discussion
In our recent study of 23 COVID-19 patients during Japan's third and fourth waves of the pandemic, including those on ECMO and those with severe AHRF, 109 cytokines were analyzed [19]. Significant increases in cytokines such as IL-11, M-CSF, stromal cell-derived factor-1 (SDF-1), and soluble tumor necrosis factor receptor 2 (sTNF-R2) were detected, suggesting a link between hematopoietic progenitor cell differentiation and Th1-derived hyperinflammation. Interestingly, the levels of traditional inflammatory cytokines such as IL-1β, IL-6, and TNF-α were not dramatically elevated. These findings indicate that cytokine storms in COVID-19 patients involve different cytokines than those typically associated with inflammation, which highlights the need to understand lung-specific inflammatory responses.
Bronchoscopic MS, a method for directly collecting ELF using a polyester fiber rod probe, was first reported by Ishizaka et al. in 2001 [13]. This technique has been applied for measuring antibiotics and conducting proteomic analyses of the patients’ ELF samples [14, 20]. In this study, we used the MS method for comprehensive cytokine analysis of the ELF in COVID-19 patients. While BAL fluid (BALF) is traditionally used for lung cytokine measurement, obtaining BALF samples carries risks such as pathogen exposure and is challenging in severely ill patients because it can potentially cause hypoxemia and pulmonary edema. MS is less invasive for collecting undiluted ELF, but due to its localized sampling, ELF samples may not reflect all the conditions throughout the lung as comprehensively as BALF samples can.
The cytokine discrepancy between the ELF and blood suggests that the lung inflammation in COVID-19 patients is distinct from that in the systemic circulation of these patients, indicating that there is localized inflammation within the lungs of these patients rather than mere secondary spillover effects. This finding emphasizes the compartmentalization of pulmonary cytokines. However, this study was limited because measurements were taken just once after tracheal intubation, thus preventing observations of the cytokine changes over time. Intriguingly, patients with severe lung disease had lower total cytokine levels in their ELF than patients with other severity levels. Although the Omicron variant is less virulent and causes fewer severe cases, it significantly harms the lungs of immunocompromised elderly individuals. This underscores the inadequacy of solely using a blood cytokine analysis for understanding the pathology of lung injury and systemic manifestations in COVID-19 patients. ELF analysis via MS provides crucial insights into lung-specific inflammation, aiding in comprehending the complex pathology of COVID-19, particularly in patients with AHRF and worsening health.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- AHRF:
-
Acute hypoxemic respiratory failure
- MV:
-
Mechanical ventilation
- ELF:
-
Epithelial lining fluid
- MS:
-
Microsampling
- CT:
-
Computed tomography
- PSI:
-
Pneumonia severity index
- CCI:
-
Charlson Comorbidity Index
- ECMO:
-
Extracorporeal membrane oxygenation
- LLOQ:
-
Lower limit of quantification
- G-CSF:
-
Granulocyte colony-stimulating factor
- GM-CSF:
-
Granulocyte–macrophage colony-stimulating factor
- IFN-γ:
-
Interferon-γ
- IL:
-
Interleukin
- MCP-1:
-
Monocyte chemotactic protein-1
- MIP-1β:
-
Macrophage inflammatory protein-1β
- TNF-α:
-
Tumor necrosis factor-α
- sCD40L:
-
Soluble CD40 ligand
- LIV:
-
Lung infiltration volume
- IQR:
-
Interquartile range
- %df:
-
Detection frequency
- BALF:
-
Bronchoalveolar lavage fluid
References
Moore JB, June CH. Cytokine release syndrome in severe COVID-19. Science. 2020;368:473–4. https://doi.org/10.1126/science.abb8925.
Chen LYC, Quach TTT. COVID-19 cytokine storm syndrome: a threshold concept. Lancet Microbe. 2021;2:e49–50. https://doi.org/10.1016/S2666-5247(20)30223-8.
Silva MJA, Ribeiro LR, Gouveia MIM, Marcelino BDR, Santos CSD, Lima KVB, et al. Hyperinflammatory response in COVID-19: a systematic review. Viruses. 2023. https://doi.org/10.3390/v15020553.
Ragab D, Salah Eldin H, Taeimah M, Khattab R, Salem R. The COVID-19 cytokine storm; what we know so far. Front Immunol. 2020;11:1446. https://doi.org/10.3389/fimmu.2020.01446.
Calabrese F, Lunardi F, Baldasso E, Pezzuto F, Kilitci A, Olteanu GE, et al. Comprehensive bronchoalveolar lavage characterization in COVID-19 associated acute respiratory distress syndrome patients: a prospective cohort study. Respir Res. 2023;24:152. https://doi.org/10.1186/s12931-023-02464-9.
Zeng HL, Chen D, Yan J, Yang Q, Han QQ, Li SS, et al. Proteomic characteristics of bronchoalveolar lavage fluid in critical COVID-19 patients. FEBS J. 2021;288:5190–200. https://doi.org/10.1111/febs.15609.
Liao L, Yang GH. Clinical significance of cellular immunity function and inflammatory factors assays in alveolar lavage fluid for severe COVID-19 pneumonia. J Med Virol. 2021;93:2979–87. https://doi.org/10.1002/jmv.26827.
Saris A, Reijnders TDY, Nossent EJ, Schuurman AR, Verhoeff J, van Asten S, et al. Distinct cellular immune profiles in the airways and blood of critically ill patients with COVID-19. Thorax. 2021;76:1010–9. https://doi.org/10.1136/thoraxjnl-2020-216256.
de Brabander J, Boers LS, Kullberg RFJ, Zhang S, Nossent EJ, Heunks LMA, et al. Persistent alveolar inflammatory response in critically ill patients with COVID-19 is associated with mortality. Thorax. 2023;78:912–21. https://doi.org/10.1136/thorax-2023-219989.
Kox M, Waalders NJB, Kooistra EJ, Gerretsen J, Pickkers P. Cytokine levels in critically ill patients with COVID-19 and other conditions. JAMA. 2020;324:1565–7. https://doi.org/10.1001/jama.2020.17052.
Bendib I, Beldi-Ferchiou A, Schlemmer F, Surenaud M, Maitre B, Plonquet A, et al. Alveolar compartmentalization of inflammatory and immune cell biomarkers in pneumonia-related ARDS. Crit Care. 2021;25:23. https://doi.org/10.1186/s13054-020-03427-y.
Jouan Y, Baranek T, Si-Tahar M, Paget C, Guillon A. Lung compartmentalization of inflammatory biomarkers in COVID-19-related ARDS. Crit Care. 2021;25:120. https://doi.org/10.1186/s13054-021-03513-9.
Ishizaka A, Watanabe M, Yamashita T, Ogawa Y, Koh H, Hasegawa N, et al. New bronchoscopic microsample probe to measure the biochemical constituents in epithelial lining fluid of patients with acute respiratory distress syndrome. Crit Care Med. 2001;29:896–8. https://doi.org/10.1097/00003246-200104000-00043.
Kipnis E, Hansen K, Sawa T, Moriyama K, Zurawel A, Ishizaka A, et al. Proteomic analysis of undiluted lung epithelial lining fluid. Chest. 2008;134:338–45. https://doi.org/10.1378/chest.07-1643.
Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336:243–50. https://doi.org/10.1056/NEJM199701233360402.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. https://doi.org/10.1016/0021-9681(87)90171-8.
Lanza E, Muglia R, Bolengo I, Santonocito OG, Lisi C, Angelotti G, et al. Quantitative chest CT analysis in COVID-19 to predict the need for oxygenation support and intubation. Eur Radiol. 2020;30:6770–8. https://doi.org/10.1007/s00330-020-07013-2.
Sudo K, Sawa T, Kushimoto K, Yoshii R, Yuasa K, Inoue K, et al. Choice of respiratory therapy for COVID-19 patients with acute hypoxemic respiratory failure: a retrospective case series study. PeerJ. 2023;11: e15174. https://doi.org/10.7717/peerj.15174.
Takashima Y, Inaba T, Matsuyama T, Yoshii K, Tanaka M, Matsumoto K, et al. Potential marker subset of blood-circulating cytokines on hematopoietic progenitor-to-Th1 pathway in COVID-19. Front Med. 2024;2024:11. https://doi.org/10.3389/fmed.2024.1319980.
Yamazaki K, Ogura S, Ishizaka A, Oh-hara T, Nishimura M. Bronchoscopic microsampling method for measuring drug concentration in epithelial lining fluid. Am J Respir Crit Care Med. 2003;168:1304–7. https://doi.org/10.1164/rccm.200301-111OC.
Acknowledgements
On the basis of this clinical study, we would like to express our thanks to the clinicians in the intensive care unit, Infectious Disease Department, and emergency department, as well as the ward nurses and laboratory technicians at KPUM Hospital for their dedicated support in managing COVID-19 patients. We would like to express our gratitude to Prof. Akitoshi Ishizaka, former professor of the Department of Respiratory Medicine at Keio University, who has passed away, and to Prof. Satoru Hashimoto, former manager of the Critical Care Division at KPUM Hospital, for their technical advice on the microsampling method. We also extend our thanks to Dr. J. Ludovic Croxford from Edanz (https://jp.edanz.com/ac), Dr. T. Fernanda, and the team from Springer Nature Author Services (https://authorservices.springernature.com/) for editing a draft of this manuscript.
Funding
This study was supported in part by the Japan Agency for Medical Research and Development [AMED Grant Number JP20fk0108270].
Author information
Authors and Affiliations
Contributions
KS and TS developed the initial idea for this study and were responsible for selecting the survey. KS extracted the data and conducted a comprehensive search of the databases. MK, KKa, KKu, RY, KI, MY, TM, and BO participated in patient management. YT, MT, KM, KT, and TI supported the use of multiplex bead-based assays and laboratory examinations. All the authors contributed to the research design, interpretation of the results, and conception of the writing of the article. K.S. and T.S. analyzed the data and drafted the article. KK, KT, BO, and TI reviewed the article and provided suggestions for improvement. All the authors have carefully examined the manuscript and agreed with the ideas presented. All the authors meet the ICMJE authorship criteria and have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki. This retrospective observational study was conducted in combination with the Kyoto Prefectural University of Medicine (KPUM) COVID-19 Registry Study (ERB-C-1810-3; approved by the Institutional Review Board of KPUM on 3 September 2020), and cytokine concentrations were analyzed in tracheal and bronchial secretions from healthy adults (ERB-C-2179; approved by the Institutional Review Board of KPUM on 1 December 2021). Informed consent was obtained from all participants and/or their legal guardian(s), and all methods were performed according to the relevant guidelines and regulations.
Availability of data and materials
The dataset (DataSet_SudoK_etal.xlsx) used and/or analyzed during this study is downloadable as Additional file 8.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Major characteristics of the patients and volunteers.
Additional file 2: Table S2.
Specific medications used in the COVID-19 patients with acute hypoxemic respiratory failure.
Additional file 3: Table S3.
Measurement range and detection sensitivity of cytokines according to examples from the Bio-Rad BioPlex Pro® manual.
Additional file 4: Table S4.
Major characteristics of the three chronological groups.
Additional file 5: Fig. S1.
The overview of the individual patients in chronological order.
Additional file 6: Table S5.
Major characteristics of the three PSI groups.
Additional file 7: Table S6.
Major characteristics of the three LIV groups.
Additional file 8:
Dataset file.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sudo, K., Kinoshita, M., Kawaguchi, K. et al. Case study observational research: inflammatory cytokines in the bronchial epithelial lining fluid of COVID-19 patients with acute hypoxemic respiratory failure. Crit Care 28, 134 (2024). https://doi.org/10.1186/s13054-024-04921-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-024-04921-3