Abstract
Background
The COVID-19 pandemic presented major challenges for critical care facilities worldwide. Infections which develop alongside or subsequent to viral pneumonitis are a challenge under sporadic and pandemic conditions; however, data have suggested that patterns of these differ between COVID-19 and other viral pneumonitides. This secondary analysis aimed to explore patterns of co-infection and intensive care unit-acquired infections (ICU-AI) and the relationship to use of corticosteroids in a large, international cohort of critically ill COVID-19 patients.
Methods
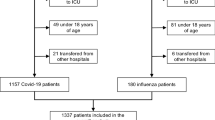
This is a multicenter, international, observational study, including adult patients with PCR-confirmed COVID-19 diagnosis admitted to ICUs at the peak of wave one of COVID-19 (February 15th to May 15th, 2020). Data collected included investigator-assessed co-infection at ICU admission, infection acquired in ICU, infection with multi-drug resistant organisms (MDRO) and antibiotic use. Frequencies were compared by Pearson’s Chi-squared and continuous variables by Mann–Whitney U test. Propensity score matching for variables associated with ICU-acquired infection was undertaken using R library MatchIT using the “full” matching method.
Results
Data were available from 4994 patients. Bacterial co-infection at admission was detected in 716 patients (14%), whilst 85% of patients received antibiotics at that stage. ICU-AI developed in 2715 (54%). The most common ICU-AI was bacterial pneumonia (44% of infections), whilst 9% of patients developed fungal pneumonia; 25% of infections involved MDRO. Patients developing infections in ICU had greater antimicrobial exposure than those without such infections. Incident density (ICU-AI per 1000 ICU days) was in considerable excess of reports from pre-pandemic surveillance. Corticosteroid use was heterogenous between ICUs. In univariate analysis, 58% of patients receiving corticosteroids and 43% of those not receiving steroids developed ICU-AI. Adjusting for potential confounders in the propensity-matched cohort, 71% of patients receiving corticosteroids developed ICU-AI vs 52% of those not receiving corticosteroids. Duration of corticosteroid therapy was also associated with development of ICU-AI and infection with an MDRO.
Conclusions
In patients with severe COVID-19 in the first wave, co-infection at admission to ICU was relatively rare but antibiotic use was in substantial excess to that indication. ICU-AI were common and were significantly associated with use of corticosteroids.
Trial registration ClinicalTrials.gov: NCT04836065 (retrospectively registered April 8th 2021).
Graphical abstract

Similar content being viewed by others
Background
The Coronavirus Disease 2019 (COVID-19) pandemic has led to heighted rates of critical illness and has placed intensive care units (ICU) under unprecedented strain [1]. Although mortality has improved [2, 3], patients continue to experience prolonged admissions to ICU and organ support.
A notable feature critical illness arising from COVID-19 has been the high reported rates of ICU-acquired infections (ICU-AI), most notably ventilator-associated pneumonia (VAP) [4,5,6] and invasive pulmonary aspergillosis [7, 8]. VAP rates of 40–70% of ventilated patients exceed rates amongst contemporaneous non-COVID-19 patients [4] and historic comparators with influenza [6]. Reported COVID-associated pulmonary aspergillosis (CAPA) rates vary, are likely to be susceptible to the surveillance criteria used [7], but approach those reported for influenza-associated aspergillosis [9] and indeed amongst non-neutropaenic patients with VAP [10]. Other fungal infections such as Mucor mycosis have also been identified [11]. Other ICU-AI, including primary and catheter-associated bacteraemias and urinary tract infections, have been subjected to less attention, but also show elevated prevalence [12, 13]. The use of immunomodulatory therapies in patients with COVID-19 has been widespread, even before definitive evidence was available from randomised trials [14].
Whilst ICU-AI appear to be highly prevalent, exceeding those seen in patients with other viral pneumonias [6], co-infection at presentation appears to be rare [15, 16], reportedly in the range of 3–8%. This differs from influenza where bacterial co-infection is common [17, 18] and mortality is frequently attributed to these co-infecting organisms [19]. Influenced by the experience of influenza and the anticipated risk of co-infection, initial guidelines advocated the use of early broad-spectrum antimicrobials in patients with severe COVID-19 disease [20].
This paper aims to describe the nature of co-infection and ICU-AI in the large UNITE-COVID cohort of patients admitted to critical care across 280 units in 46 countries over 5 continents during the first wave of COVID-19 [1]. In this paper, we investigate factors associated with the development of ICU-AI including the use of corticosteroids.
Methods
This study is a sub-analysis of the ESICM UNITE-COVID study, which has been extensively described elsewhere [1]. Briefly, UNITE-COVID is a multicenter, international, anonymized observational study carried out in 280 hospitals from 46 countries during ‘wave one’ (defined as 15th of February until 15th of May 2020). Patients who were under intensivist care on the day with the highest number of such patients during wave one were included and followed-up longitudinally for outcomes including ICU-acquired infections, antibiotic use and discharge or death. For each patient, data were collected from hospital admission until discharge.
The study received approval from Ghent University Hospital Ethics committee, registration BC-07826 and appropriate approvals at each participating site in line with local regulations (ClinicalTrials.gov registration: NCT04836065, retrospectively registered April 8th 2021).
Patients
Inclusion criteria were (1) age ≥ 18 years, (2) cared for by the critical care team in an ICU or other area of the hospital on the above-mentioned date, (3) had PCR (or equivalent technique) confirmed Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV2) infection and (4) had a diagnosis of COVID-19. Patients without a diagnosis of COVID-19 but documented SARS-CoV2 detection were excluded. Patients could only be included once. Informed consent was either obtained or waived according to the local ethics committee’s decision.
Data
Details of the data collection methods, the collected data, the data curation and the DAQCORD-checklist, are contained in the primary paper [1]. The data curation pipeline and data quality assessment (version 3.1) are publicly available [21]. All data were collected from the day of ICU admission until day 60 following inclusion, with antibiotic use data collected until day 30 after admission. For the purposes of this sub-analysis, we focused on investigator-identified infections at admission and during ICU stay as well as identified multi-resistant microorganisms. ICU-AI were defined as those developing after ICU admission and that were not detected at time of admission to ICU, as identified by the site investigator. Patients with missing data from the relevant field were excluded from that analysis. The case report form is included in the Additional file 1.
Statistical analysis
Categorical variables are expressed as frequencies (percentages), continuous variables are described with medians with interquartile range (IQR). Differences in categorical variables were calculated using a Pearson chi-squared test. The Mann–Whitney U test was used for comparison of non-normally distributed continuous variables. Comparison of non-normally distributed continuous variables with categorical variables was performed by means of the Kruskal–Wallis test. Statistical significance was defined as p < 0.05.
Statistical analysis was performed using R Statistical Software (R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria, 4.0.3).
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for reporting of observational studies in combination with the recommendations to optimize reporting of epidemiological studies on antimicrobial resistance and informing improvement in antimicrobial stewardship (STROBE-AMS) were followed throughout this manuscript. The case report form is viewable as Additional file 1.
We pre-defined factors thought likely to be associated with ICU-AI, namely age, sex, aggregate comorbidity score, use and duration of corticosteroids, need for invasive mechanical ventilation, vasopressors and renal replacement therapy, duration of ventilation and severity of respiratory failure. Severity of respiratory failure was assessed using an ordinal scale of maximal respiratory support similar to that used previously [22] scoring 0 for non-invasive support, 1 for invasive mechanical ventilation, 2 for neuromuscular blockade and 3 for prone ventilation or extra-corporeal membrane oxygenation (ECMO). The combined highest category was used as it was recognised that not all patients with most severe respiratory failure would be referred or accepted for ECMO. We examined univariate association with the development of ICU-acquired infection by pairwise analysis.
To adjust for the pre-defined confounders in our analysis, we used propensity matching [23]. The patient cohort of interest was matched using the R library MatchIt [24] using the “full” matching method [23, 24] as this produced the best match based on standard mean differences. Propensity-matched analysis was restricted to patients who were mechanically ventilated during their ICU stay and who had near-complete data across the fields of interest. Patients with data missing across multiple fields of interest were excluded, where data were missing from one field multiple chained imputation (R library MICE [25]) was employed. We used a 1-to-1 matching of treated to controls in all the analysis except for the tocilizumab treatment analysis where the low number of treated patients allowed a ratio of one treated to three controls without losing match accuracy (Additional file 2: Model Formula S1). Initial analysis excluded those with respiratory co-infection on admission, with inclusion of these patients in a sensitivity analysis.
Results
Data were available from 4994 patients; demographic and clinical features of these patients have been described previously [1]. Overall 4129 (83%) were mechanically ventilated during their ICU stay, 2325 (47%) within 24 h of admission, whilst a further 1677 (34%) were ventilated later in their stay.
Co-infection
Bacterial pulmonary co-infection was detected in 716 patients (14%). Despite this, antibacterials were administered to 85% of patients. The immunomodulatory azithromycin made up 19% of all antibacterials, with 35% of all patients being prescribed this drug (Additional file 2: Table S1). Intubation at admission was associated with a significantly greater rate of antibacterial prescription (90% vs 86%, p = 0.0014), as was suspicion of co-infection (98% vs 86%, p < 0.001). 6% of patients received antifungals at admission (Additional file 2: Table S2). Patients with co-infection at ICU admission had similar pre-ICU hospital length of stay, a median of 1 day (IQR 0–4) with co-infection vs 2 days (IQR 0–4) for those without co-infection (p = 0.06).
A comparison of inflammatory parameters between those with and without assessed co-infection at admission is shown in Fig. 1. Although several achieved statistically significant differences, there was substantial overlap between the groups.
ICU-acquired infections
ICU-AI were common, with 2715 (54%) patients developing a total of 4737 infections (median 2 infections per patient infected). The most common infection was bacterial pneumonia (reported in 77% of patients developing infections), followed by non-catheter-associated bacteraemia (seen in 26% of patients that developed an infection). Fungal respiratory infections were identified in 9% of all patients, and 16% of that developed an infection (Table 1). Of the patients with infection, 25% had an infection with an MDRO. The most prevalent MDRO’s were extended spectrum beta-lactamase producers (ESBL) (7.75%) and Methecillin-resistant Staphylococcus aureus (MRSA) (4.75%) (Additional file 2: Table S3).
Patients received a significant burden of antibiotic exposure during their admission, with a median 7 (IQR 0–17) days alive without antibiotics during the 30-day follow-up. The development of ICU-AI was associated with greater use of antibiotics; a median of 5 (IQR 0–14) antibiotic-free days in those with ICU-AI vs a median of 12 (IQR 0–23) in those without infection.
Factors associated with ICU-AI
Factors evaluated for association with ICU-AI are shown in Table 2. ICU-AI was associated with longer ICU length of stay (median 24 days (IQR 16–35) days vs 11 days (IQR 6–17) (p < 0.001), as was infection with MDRO (29 days (IQR 19–43) days for MDRO vs 23 days (IQR 15–33) for those with non-MDRO infection (p < 0.001).
Receipt of antibiotics at admission was associated with development of subsequent infection (58% vs 46% of those not receiving antibiotics, p < 0.001), but was not significantly associated with development of MDRO infection (24% vs 20%, p = 0.2). Fewer antimicrobial-free days were associated with a higher prevalence of MDRO infection (median antimicrobial-free days 2 (IQR 0–9) for patients with an MDRO infection vs 6 days (IQR 0–15) for patients without an MDRO infection, p < 0.01). Corticosteroid use was higher amongst patients developing infection in ICU (58% vs 43%). Steroid use was heterogenous across centres (Fig. 2) with the dominant indications being hyperinflammation and pneumonitis, which together made up 65% of indications recorded (Additional file 2: Table S4). Shock was the indication in 16% of cases.
Propensity-matched analysis.
Following the finding of an increased risk of infection amongst patients receiving corticosteroids in univariate analysis, we undertook a propensity-matched analysis to further understand this relationship, undertaking matching for pre-defined factors thought to be associated with infection (Table 2). Heterogeneity of steroid use between units extended to both the percentage of patients receiving steroids in each centre and the duration of therapy (Fig. 2). Additional file 2: Fig. S1 shows the selection of the matched cohort. Using 1:1 matching, 1086 were entered into this analysis, and matching was highly effective (Fig. 3), with absolute standardised mean differences after matching all less than 0.1. The calculated pseudo-R2 was 0.33 (details in Additional file 2).
Propensity score (PS) matching for corticosteroid matching parameters compared to the input cohort. A density plots and histograms showing the effect of PS matching on distributions. B Covariance balance ‘love’ plot illustrating the effect of PS on standardised mean difference. C Numeric summary statistics following PS matching. Reporting percentages for categorical variables, mean for non-skewed parameters, and median for skewed parameters. Last two entries below the thick line are outcome measures and were not used for matching
In the matched cohort, the relationship between steroids and infection was maintained: 71% of those receiving steroids developed ICU-AI vs 52% of those not in receipt of steroids (p < 0.001). The main indications for steroids in the propensity-matched cohort were hyper-inflammation and shock (Additional file 2: Table S5). Steroid use was also associated with MDRO infections (17% of infections in patients on steroids were with MDRO organisms, vs 5% of those not on steroids (p < 0.001). Duration of steroid administration was also associated with ICU-AI in this analysis, with those developing ICU-AI receiving steroids for a median of 8 days (IQR 3–14)) vs 5 days (IQR 3–10) for those not developing infection. The median time spent in ICU before steroid administration was 2 days (IQR 0–8) in patients who did not develop an infection in ICU and 6 days (IQR 1–13) in those who did. The mortality rate was higher in the steroid treatment cohort with 37% compared to 30% in the non-steroid cohort (p = 0.02).
As a sensitivity analysis, inclusion of those who had co-infection on admission did not significantly alter the results of the propensity-matched analysis (Additional file 2: results).
Rates of tocilizumab use were much lower than corticosteroids, with only 132 patients receiving this. In a 1:1 match using the same matching variables and matching method, tocilizumab use was not associated with an increase in the risk of ICU-AI: 56% of patients without tocilizumab developed infection vs 46% of those receiving this agent (p = 0.04). Details of the matching are shown in Additional file 2: Figs. S2 and S3.
Discussion
This study describes the largest ICU cohort with COVID-19 so far reported and covers patients from a wide range of countries. The rate of co-infection, at 14%, is above the 3–10% reported in other studies [15, 16, 18, 26] including those that were restricted to critically ill patients [26]. Although there was a marginal effect of co-infection on the use of antibiotics at admission, the great majority of patients received antibiotics despite the absence of assessed co-infection. At the time of data collection, guidelines indicated that broad spectrum antibiotics should be administered to all patients with severe disease [20].
The finding of high rates of ICU-AI, with over half of all patients developing such infections, is consistent with previous reports from critically ill COVID-19 patients which have largely focussed on ventilator-associated pneumonia [4,5,6], and bacteraemia [12, 13], notably also the predominant infections encountered in this cohort. Whilst debate continues regarding the true incidence of CAPA [27, 28], in this study we found fungal pulmonary infections complicated the stay of 9% of all patients. This is a lower prevalence than some reports [8], but may reflect underdiagnosis as at the time of data collection CAPA was a novel diagnosis [7]. The rate of ICU-AI reported far-exceeds pre-pandemic rates reported by the European Centres for Disease Control (ECDC) [29]. In 2017, ECDC reported rates of ICU-acquired infection were 8.3% for all patients staying more than 2 days in ICU, with pneumonia complicating 6% of stays, bloodstream infections (BSI) 4% and urinary tract infections (UTI) 2% [29]. Whilst diagnostic uncertainty caused by tracheal colonisation and viral pneumonitis may confound the incidence of ICU-acquired pneumonia, such uncertainty is unlikely to be present with infections at other sites. Studies from multiple units which have used rigorous diagnostic criteria have found a similarly high rate of bacterial pneumonia [4,5,6] reporting prevalences of 44 to 50%. We cannot be certain that some identified ICU-AIs were not, in-fact, missed co-infections, and this could influence the relationship between initial antibiotics and subsequent detected ICU-AI. However, previous studies of ICU-AI have shown clinicians can readily distinguish the two [30, 31]. This is unlikely to alter the results of our findings, as including patients with identified co-infection did not substantially alter the results from the propensity-score-matched analysis (Additional file 2: results). The high rate of secondary infection seen in this current cohort was reflected in associated exposure to antibiotics, and strikingly, a substantial proportion of antibiotic use was not targeted towards either co-infection or ICU-AI. MDRO were encountered in a quarter of all those developing ICU-AI, similar to the prevalence reported in other large surveys of infection in ICU [32]. The association between duration of antimicrobial therapy and development of MDROs may reflect the selective pressure of prolonged antimicrobial infection but may also reflect the perceived need for prolonged antimicrobial therapy in patients who develop MDRO infections.
The reasons for the high rates of ICU-AI amongst patients with COVD remain uncertain and cannot be completely explained by prolonged duration of organ support [4, 6]. The ECDC 2017 report notes median incident density of 3.7/1000 ICU days (IQR 0.8–4.9) for pneumonia, 1.9/1000 ICU days (IQR 0.4–3.1) for all BSIs and 2.4/1000 ICU days (IQR 0–3.7) for UTI [29]. The incident density shown in Table 1 is in considerable excess of these. In this study, we identified a significant association between the use of corticosteroids and the development of such infections and infections with MDRO, which was maintained after adjustment for potential confounders. As an observational study, however, we cannot exclude residual confounding as a cause of this association. In this study, corticosteroids were not associated with increased survival, so it is unlikely that their use increased infection due to patients surviving long enough to develop an infection in ICU. The finding of increased unadjusted mortality amongst patients receiving steroids may reflect differences between patients selected for corticosteroid therapy, although other reports have noted similar effects even after adjusting for clinical variables [33, 34].
The literature concerning the effect of corticosteroids on ICU-AIs is divergent, with reports of both increased [35] and decreased infection rates [36]. In the randomised trials examining the use of corticosteroids in COVID-19 [37,38,39,40,41] an association was not found with secondary infections. However, the largest of these studies [38, 41] did not specifically look for secondary infections. Two smaller studies [39, 40] reported no significant differences, although the overall rates of secondary infection were lower than those reported here and elsewhere in the literature [4,5,6, 12, 13]. Our study is observational, and so we cannot exclude unmeasured cofounders. However, it reports data from ‘wave one’ before the announcement of the results of the landmark RECOVERY trial [38] and corticosteroid use varied markedly between centres (Fig. 2). Furthermore, a wide range of steroid doses and durations of therapy were deployed early in the pandemic. It may be that prolonged and high-dose courses of corticosteroids explain why our results diverge from those reported in clinical trials [39, 40]. Other observational studies have found a relationship between corticosteroid use and subsequent pneumonia in single centre [42] and multi-centre cohorts [34, 43], with the Dupuis and colleagues study noting a relationship between steroid dose and infection risk [34]. It is possible that steroids were prescribed because of secondary infection i.e. a reverse causal relationship, though we did not find an excess of shock amongst patients receiving steroids who developed secondary infection (Additional file 2: Table S5). It was, perhaps, surprising to find that tocilizumab was not associated with an increased risk of ICU-acquired infection and indeed the effect seen was in the opposite direction. We note a similar finding recently reported in a single centre study of catheter-related blood stream infections, where dexamethasone but not tocilizumab was associated with increased risk of infection [44]. It is possible that this finding resulted from failure to diagnose infection due to supressed inflammatory responses, most especially C-reactive protein and procalcitonin concentrations [45]. Alternatively, if tocilizumab was reserved for later in patient stays, it may have been withheld in patients in whom there was suspicion of secondary infection; however, lack of data on the relative timing of these events makes these hypotheses speculative.
This study has a number of strengths, among them that it is the largest study of critically ill patients with COVID-19 reported to date and provides data from a wide range of geographic locations and healthcare settings. However, the data collected were limited by the feasibility of collecting data from hundreds of geographically diverse sites during the early phase of the pandemic. As such we had to rely on investigator ascertainment of the presence of infection, which may not have been standard across sites and did not collect details of microbiological cultures beyond the presence or absence of specific MDROs. That the rates of ICU-AI were similar to those reported from smaller, but more rigorously controlled studies are reassuring [4,5,6, 11, 12], and patterns seen were similar across all infections, as well as the more objective measures of MDRO rates and antibiotic use. With widespread use of antibiotics noted, it is possible that these would mask the detection of ICU-AI and that the rates of ICU-AI are actually higher than we report, although this is unlikely to alter the relationships seen with the therapeutic agents examined. We did not collect data on formulation or dose of corticosteroid used and therefore cannot assess the impact that variations in these may have had.
Conclusions
In conclusion, this study has demonstrated widespread use of antibiotics in critically ill patients during the first wave of COVID-19. Although this use may appear indiscriminate, their use at admission was in line with guidelines extant at the time of patient inclusion [20]. Admissions with bacterial co-infection were relatively rare, and there was significant potential to limit antibiotic use at this point. Although ICU-AI were common, driving antibiotic use, this use extended beyond patients with secondary infections, indicating potential for further reduction in antibiotic utilisation. The finding of an association between corticosteroid use and ICU-AI requires further exploration, as do strategies for infection diagnosis in the presence of concurrent anti-cytokine therapies.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. The data curation pipeline and data quality assessment (version 3.1) are publicly available https://doi.org/10.5281/zenodo.6063905
Change history
17 August 2022
A Correction to this paper has been published: https://doi.org/10.1186/s13054-022-04124-8
Abbreviations
- BSI:
-
Blood stream infection
- COVID-19:
-
Coronavirus disease 19
- CAPA:
-
COVID-associated pulmonary aspergillosis
- ECMO:
-
Extra-corporeal membrane oxygenation
- ECDC:
-
European Centres for Disease Control
- ESBL:
-
Extended spectrum beta-lactamase producers
- ICU:
-
Intensive care unit
- ICU-AI:
-
Intensive care unit-acquired infection
- MDRO:
-
Multi-drug resistant organisms
- MRSA:
-
Methecillin-resistant Staphylococcus aureus
- SARS-CoV2:
-
Severe Acute Respiratory Syndrome Coronavirus-2
- STROBE:
-
The Strengthening the Reporting of Observational Studies in Epidemiology
- STROBE-AMS:
-
The Strengthening the Reporting of Observational Studies in Epidemiology antimicrobial resistance and informing improvement in antimicrobial stewardship
- UTI:
-
Urinary tract infection
- VAP:
-
Ventilator-associated pneumonia
References
Greco M, Corte TD, Ercole A, et al. Clinical and organizational factors associated with mortality during the peak of first COVID-19 wave: the global UNITE-COVID study. Intens Care Med. 2022. https://doi.org/10.1007/s00134-022-06705-1.
Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323(16):1574–81.
Zhang J, Dong X, Cao Y, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;395(10223):507–12.
Maes M, Higginson E, Pereira-Dias J, et al. Ventilator-associated pneumonia in critically ill patients with COVID-19. Crit Care. 2021;25(1):25.
Pickens CO, Gao CA, Cuttica MJ, et al. Bacterial superinfection pneumonia in patients mechanically ventilated for COVID-19 pneumonia. Am J Resp Crit Care. 2021;204(8):921–32.
Rouzé A, Martin-Loeches I, Povoa P, et al. Relationship between SARS-CoV-2 infection and the incidence of ventilator-associated lower respiratory tract infections: a European multicenter cohort study. Intens Care Med. 2021;47(2):188–98.
Verweij PE, Brüggemann RJM, Azoulay E, et al. Taskforce report on the diagnosis and clinical management of COVID-19 associated pulmonary aspergillosis. Intens Care Med. 2021;47(8):819–34.
Bartoletti M, Pascale R, Cricca M, et al. Epidemiology of invasive pulmonary aspergillosis among COVID-19 intubated patients: a prospective study. Clin Infect Dis. 2020;73(11):ciaa1065.
Schauwvlieghe AFAD, Rijnders BJA, Philips N, et al. Invasive aspergillosis in patients admitted to the intensive care unit with severe influenza: a retrospective cohort study. Lancet Resp Med. 2018;6(10):782–92.
Loughlin L, Hellyer TP, White PL, et al. Pulmonary aspergillosis in patients with suspected ventilator-associated pneumonia in UK ICUs. Am J Respir Crit Care Med. 2020;202(8):1125–32.
Patel A, Agarwal R, Rudramurthy SM, et al. Multicenter epidemiologic study of coronavirus disease-associated mucormycosis, India. Emerg Infect Dis. 2021;27(9):2349–59.
Grasselli G, Scaravilli V, Mangioni D, et al. Hospital-acquired infections in critically ill patients with COVID-19. Chest. 2021;160(2):454–65.
Bardi T, Pintado V, Gomez-Rojo M, et al. Nosocomial infections associated to COVID-19 in the intensive care unit: clinical characteristics and outcome. Eur J Clin Microbiol. 2021;40(3):495–502.
Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–81.
Lansbury L, Lim B, Baskaran V, Lim WS. Co-infections in people with COVID-19: a systematic review and meta-analysis. J Infect. 2020;81(2):266–75.
Rawson TM, Moore LSP, Zhu N, et al. Bacterial and fungal co-infection in individuals with coronavirus: a rapid review to support COVID-19 antimicrobial prescribing. Clin Infect Dis. 2020;71(9):ciaa530.
Klein EY, Monteforte B, Gupta A, et al. The frequency of influenza and bacterial coinfection: a systematic review and meta-analysis. Influenza Other Resp. 2016;10(5):394–403.
Rouzé A, Martin-Loeches I, Povoa P, et al. Early bacterial identification among intubated patients with COVID-19 or influenza pneumonia: a European Multicenter Comparative Clinical Trial. Am J Resp Crit Care. 2021;204(5):546–56.
Jia L, Xie J, Zhao J, et al. Mechanisms of severe mortality-associated bacterial co-infections following influenza virus infection. Front Cell Infect Mi. 2017;7:338.
Alhazzani W, Møller MH, Arabi YM, et al. Surviving sepsis campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intens Care Med. 2020;46(5):854–87.
Ercole A, PW E, H_J de G, et al (2021) UNITE-COVID data curation pipeline. v3.1.0. zenodo. https://doi.org/10.5281/zenodo.6063905
Lockhart SM, Griffiths H, Petrisor B, et al. The excess insulin requirement in severe COVID-19 compared to non-COVID-19 viral pneumonitis is related to the severity of respiratory failure and pre-existing diabetes. Endocrinol Diabetes Metab. 2021;4(3):e00228.
Austin PC. An Introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46(3):399–424.
Ho DE, Imai K, King G, Stuart EA. MatchIt : nonparametric preprocessing for parametric causal inference. J Stat Softw. 2011;42(8):1–28.
van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):1–67.
Baskaran V, Lawrence H, Lansbury LE, et al. Co-infection in critically ill patients with COVID-19: an observational cohort study from England. J Med Microbiol. 2021;70(4): 001350.
Zhang SX, Balada-Llasat JM, Pancholi P, Sullivan KV, Riedel S, (FDLC) FDLC. COVID-associated pulmonary aspergillosis in the United States: is it rare or have we missed the diagnosis? J Clin Microbiol. 2021;59(10):e01135-21.
Rouzé A, Lemaitre E, Martin-Loeches I, et al. Invasive pulmonary aspergillosis among intubated patients with SARS-CoV-2 or influenza pneumonia: a European multicenter comparative cohort study. Crit Care. 2022;26(1):11.
European Centre for Disease Prevention and Control. Healthcare-associated infections acquired in intensive care units. In: ECDC. Annual epidemiological report for 2017. Stockholm: ECDC; 2019.
Morris AC, Anderson N, Brittan M, et al. Combined dysfunctions of immune cells predict nosocomial infection in critically ill patients. Br J Anaes. 2013;111(5):778–87.
Morris AC, Datta D, Shankar-Hari M, et al. Cell-surface signatures of immune dysfunction risk-stratify critically ill patients: INFECT study. Intens Care Med. 2018;44(5):627–35.
Vincent JL, Sakr Y, Singer M, et al. Prevalence and outcomes of infection among patients in intensive care units in 2017. JAMA. 2020;323(15):1478–510.
Jung C, Wernly B, Fjølner J, et al. Steroid use in elderly critically ill COVID-19 patients. Eur Respir J. 2021;58(4):2100979.
Dupuis C, de Montmollin E, Buetti N, et al. Impact of early corticosteroids on 60-day mortality in critically ill patients with COVID-19: a multicenter cohort study of the OUTCOMEREA network. PLoS ONE. 2021;16(8):e0255644.
Sprung CL, Annane D, Keh D, et al. Hydrocortisone therapy for patients with septic shock. N Engl J Med. 2008;358(2):111–24.
Roquilly A, Mahe PJ, Seguin P, et al. Hydrocortisone therapy for patients with multiple trauma: the randomized controlled HYPOLYTE study. JAMA. 2011;305(12):1201–9.
The WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19. JAMA. 2020;324(13):1330–41.
RECOVERY Collaborative Group, Horby P, Lim WS, Emberson JR, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384(8):693–704.
Tomazini BM, Maia IS, Cavalcanti AB, et al. Effect of dexamethasone on days alive and ventilator-free in patients with moderate or severe acute respiratory distress syndrome and COVID-19. JAMA. 2020;324(13):1307–16.
Dequin PF, Heming N, Meziani F, et al. Effect of hydrocortisone on 21-day mortality or respiratory support among critically ill patients with COVID-19. JAMA. 2020;324(13):1298–306.
Investigators TWC for the RC, Angus DC, Derde L, et al. Effect of hydrocortisone on mortality and organ support in patients with severe COVID-19. JAMA. 2020;324(13):1317–29.
Martínez-Martínez M, Plata-Menchaca EP, Nuvials FX, Roca O, Ferrer R. Risk factors and outcomes of ventilator-associated pneumonia in COVID-19 patients: a propensity score matched analysis. Crit Care. 2021;25(1):235.
Scaravilli V, Guzzardella A, Madotto F, et al. Impact of dexamethasone on the incidence of ventilator-associated pneumonia in mechanically ventilated COVID-19 patients: a propensity-matched cohort study. Crit Care. 2022;26(1):176.
Meynaar IA, van Rijn S, Ottens TH, van Burgel ND, van Nieuwkoop C. Increased risk of central line-associated bloodstream infection in COVID-19 patients associated with dexamethasone but not with interleukin antagonists. Intens Care Med. 2022. https://doi.org/10.1007/s00134-022-06750-w.
Kooistra EJ, van Berkel M, van Kempen NF, et al. Dexamethasone and tocilizumab treatment considerably reduces the value of C-reactive protein and procalcitonin to detect secondary bacterial infections in COVID-19 patients. Crit Care. 2021;25(1):281.
Acknowledgements
We want to thank Guy Francois of the European Society of Intensive Care Medicine for his support. We thank the ESICM COVID UNITE National Coordinators for their help: Bangladesh: Tarikul Hamid; Belgium: Jan De Waele; Brazil: Ederlon Rezende; Canada: Michael Sklar; Chile: Patricio Vargas; China: Bin Du; Colombia: Luis Felipe Reyes; Ecuador: Diego Morocho Tutillo; Germany: Björn Weiss; Greece: Despoina Koulenti; India: Sameer Jog; Ireland: Alistair Nichol; Italy: Katia Donadello; Kenya: Demet S. Sulemanji; Lybia: Muhammed Elhadi; Mexico: Silvio A. Ñmendys-Silva; Netherlands: Paul Elbers; Pakistan: Madiha Hashmi; Peru: Juan Luis Pinedo Portilla; Portugal: Pedro Povoa; Qatar: Abdurrahmaan Ali Elbuzidi; Russian Federation: Vitaly Gusarov; Saudi Arabia: Yaseen Arabi; Singapore: Jensen Ng Jiansheng; Spain: Laura Galarza Barrachina; Turkey: Arzu Topeli; United Kingdom: Alasdair Jubb; United States: Nathan D. Nielsen. The full list of ESICM UNITE-COVID authors is noted below
The ESICM UNITE COVID study group members
ARGENTINA: Hospital de Agudos Santojanni (Buenos Aires): Marco Bezzi; Hospital Universitario Austral (Buenos Aires): Alicia Gira;
AUSTRIA: Medical University of Graz (Graz): Philipp Eller;
BANGLADESH: Asgar Ali Hospital (Dhaka): Tarikul Hamid; Central Police Hospital (Dhaka): Injamam Ull Haque;
BELGIUM: AZ Rivierenland (Bornem): Wim De Buyser; CHIREC Hospitals (Brussels): Antonella Cudia, Daniel De Backer, Pierre Foulon; Cliniques de l'Europe, St-Michel (Brussels): Vincent Collin; Universitair Ziekenhuis Gent (Gent): Jan De Waele, Jolien Van Hecke; UZ Brussel (Jette): Elisabeth De Waele, Claire Van Malderen; CH Jolimont (La Louvière): Jean-Baptiste Mesland; CHU Charleroi (Lodelinsart): Michael Piagnerelli; CHU Ambroise Pare (Mons): Lionel Haentjens; Clinique Saint-Pierre (Ottignies): Nicolas De Schryver; GZA Ziekenhuizen (Wilrijk): Jan Van Leemput, Philippe Vanhove; Mont-Godinne University Hospital, CHU UCL Namur (Yvoir): Pierre Bulpa;
BULGARIA: Multidisciplinary Hospital for Pulmonary Diseases St. Sofia (Sofia): Viktoria Ilieva;
CANADA: Brampton Civic Hospital (Brampton): David Katz; North York General Hospital (Toronto): Anna Geagea; William Osler Health System—Etobicoke General Hospital (Toronto): Alexandra Binnie;
CHILE: Complejo Asistencial Dr. Victor Rios Ruiz (Los Angeles): Fernando Tirapegui; Hospital Clínico Fusat (Rancagua): Gustavo Lago; Clínica Alemana de Santiago (Santiago): Jerónimo Graf, Rodrigo Perez-Araos; Hospital del Salvador (Santiago): Patricio Vargas; Facultad de Medicina, Escuela de Medicina, Universidad Andrés Bello (Viña del Mar): Felipe Martinez; Hospital Naval Almirante Nef (Viña del Mar): Eduardo Labarca;
COLOMBIA: Hospital San Jose (Bogota): Daniel Molano Franco; Universidad de La Sabana (Chía) and Clínica Universidad de La Sabana (Chía): Daniela Parra-Tanoux, Luis Felipe Reyes; Ces Clinic (Medellin): David Yepes;
CROATIA: University Hospital Split (Split): Filip Periš, Sanda Stojanović Stipić;
ECUADOR: Hospital General Guasmo Sur (Guayaquil): Cynthia Vanessa Campozano Burgos, Paulo Roberto Navas Boada; Hospital de Especialidades Portoviejo (Portoviejo): Jose Luis Barberan Brun, Juan Pablo Paredes Ballesteros;
EGYPT: Gamal Abdelnasser (Alexandria): Ahmed Hammouda; Wingat Royal Hospital (Alexandria): Omar Elmandouh; Luxor Pyretic Medical Centre (Armant): Ahmed Azzam; Assiut University Hospital (Assiut): Aliae Mohamed Hussein; Aswan University (Aswan): Islam Galal; Ain-Shams University Hospitals (Cairo): Ahmed K. Awad; Kasr Al Ainy Cairo University Hospital (Cairo): Mohammed A Azab; Misr International Hospital (Cairo): Maged Abdalla, Hebatallah Assal, Mostafa Alfishawy; El-Sheikh Zayed Specialized Hospital (Giza): Sherief Ghozy; Mansoura University Hospitals (Mansoura): Samar Tharwat; Elmenshawy General Hospital (Tanta): Abdullah Eldaly;
ESTONIA: Tartu University Hospital (Tartu): Veronika Reinhard;
FRANCE: Hôpital d’Instruction des Armées Percy (Clamart): Anne Chrisment, Chrystelle Poyat; Hôpital Nord Franche-Comté (Trevenans): Julio Badie, Fernando Berdaguer Ferrari;
GERMANY: Charité—Universitätsmedizin Berlin, ICU 8i (Berlin): Björn Weiss; Charité—Universitätsmedizin Berlin, ICU 43i (Berlin): Karl Friedrich Kuhn; Charité—Universitätsmedizin Berlin, ICU 44i (Berlin): Julius J. Grunow; Charité—Universitätsmedizin Berlin, ICU 144i (Berlin): Marco Lorenz; Charité—Universitätsmedizin Berlin, 203i (Berlin): Stefan Schaller; University Hospital Dresden (Dresden): Peter Spieth; Bethesda Krankenhaus Bergedorf (Hamburg): Marc Bota; University Hospital Leipzig (Leipzig): Falk Fichtner; Klinikum Rechts der Isar der TUM, IS1/M2B (Munich): Kristina Fuest; Klinikum Rechts der Isar der TUM, R3A (Munich): Tobias Lahmer; University Hospital of Wurzburg (Wurzburg): Johannes Herrmann, Patrick Meybohm;
GREECE: General Hospital of Eleusis ‘Thriasion’ (Eleusis): Nikolaos Markou; George Papanikolaou General Hospital (Exohi-Thessaloniki): Georgia Vasileiadou; University Hospital Attikon: (Haidari): Evangelia Chrysanthopoulou; General Hospital of Larissa (Larissa): Panagiotis Papamichalis; University General Hospital of Thessaloniki AHEPA (Thessaloniki): Ioanna Soultati;
INDIA: Deenanath Mangeshkar Hospital and Research Center (Pune): Sameer Jog; Tata Memorial Hospital, Homi Bhabha National University (Mumbai): Kushal Kalvit; Sheila Nainan Myatra;
IRELAND: Cavan General Hospital (Cavan): Ivan Krupa; Our Lady of Lourdes Hospital (Drogheda): Aisa Tharwat; St Vincent's University Hospital (Dublin): Alistair Nichol; Galway University Hospitals (Galway): Aine McCarthy;
IRAN: Imam Reza Hospital (Tabriz): Ata Mahmoodpoor;
ITALY: Sant'Orsola University Hospital (Bologna): Tommaso Tonetti; Santissima Trinità Hospital (Cagliari): Paolo Isoni; Arcispedale Sant’Anna (Ferrara): Savino Spadaro, Carlo Alberto Volta; University of Foggia Ospedali riuniti Foggia (Foggia): Lucia Mirabella; AOU G. Martino (Messina): Alberto Noto; Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico (Milan): Gaetano Florio, Amedeo Guzzardella, Chiara Paleari; IRCCS Humanitas Research Hospital (Milan): Federica Baccanelli, Marzia Savi; Gemelli IRCCS (Rome): Massimo Antonelli; San Luca (Trecenta Rovigo): Barbara Vaccarini; Città della Salute e della Scienza—Presidio Molinette (Turin): Giorgia Montrucchio, Gabriele Sales; University Hospital Integrated Trust (AOUI) Of Verona (Verona): Katia Donadello, Leonardo Gottin, Enrico Polati; San Bortolo Hospital (Vicenza): Silvia De Rosa;
KENYA: MP Shah Hospital (Nairobi): Demet Sulemanji;
LIBYA: Almwasfat Hospital (Tripoli): Abdurraouf Abusalama; Tripoli University Hospital (Tripoli): Muhammed Elhadi;
MEXICO: Hospital General De Ecatepec Las Americas (Ecatepec de Morelos): Montelongo Felipe De Jesus; Hospital civil nuevo dr Juan I Menchaca (Guadalajara Jalisco): Daniel Rodriguez Gonzalez; Hospital de Especialidades Dr.Antonio Fraga Mouret CMN La Raza (Mexico): Nancy Canedo, Alejandro Esquivel Chavez;
MOROCCO: Ibn Sina University Hospital (Rabat): Tarek Dendane;
NETHERLANDS: Ziekenhuisgroep Twente(Almelo): Bart Grady, Ben de Jong; Amsterdam UMC, VUmc site (Amsterdam): Eveline van der Heiden, Patrick Thoral; Onze Lieve Vrouwe Gasthuis (Amsterdam): Bas van den Bogaard; Gelre Ziekenhuizen (Apeldoorn): Peter E. Spronk; Haaglanden Medisch Centrum (Den Haag): Sefanja Achterberg; Deventer Ziekenhuis (Deventer): Melanie Groeneveld; Albert Schweitzer Hospital (Dordrecht): Ralph K.L. So, Calvin de Wijs; Catharina Ziekenhuis (Eindhoven): Harm Scholten; Medisch Spectrum Twente (Enschede): Albertus Beishuizen, Alexander D. Cornet; Martiniziekenhuis (Groningen): Auke C. Reidinga; University Medical Center Groningen (Groningen): Hetty Kranen, Roos Mensink; Spaarne Gasthuis (Haarlem): Sylvia den Boer, Marcel de Groot; Tjongerschans Heerenveen (Heerenveen): Oliver Beck; Medical Centre Leeuwarden (Leeuwarden): Carina Bethlehem; Maastricht University Medical Center (Maastricht): Bas van Bussel; Radboudumc (Nijmegen): Tim Frenzel; Elisabeth TweeSteden Ziekenhuis (ETZ) (Tilburg): Celestine de Jong, Rob Wilting; University Medical Center Utrecht (Utrecht): Jozef Kesecioglu; VieCuri Medical Center (Venlo): Jannet Mehagnoul-Schipper;
NIGERIA: University of Port Harcourt Teaching Hospital (Port Harcourt): Datonye Alasia;
PAKISTAN: Ziauddin Hospital Clifton Campus (Karachi): Ashok Kumar; Bahria International Hospital (Lahore): Ahad Qayyum, Muhammad Rana;
PALESTINE: Alshifaa Hospital (Gaza): Mustafa Abu Jayyab;
PERU: Hospital Nacional Dos de Mayo (Lima): Rosario Quispe Sierra;
PHILIPINES: Asian Hospital and Medical Center (Muntinlupa): Aaron Mark Hernandez;
PORTUGAL: Hospital de Cascais—Dr. José de Almeida (Alcabideche): Lúcia Taborda; Hospital Prof. Dr. Fernando da Fonseca, E.P.E. (Amadora): Tiago Ramires; Centro Hospitalar e Universitário de Coimbra (Coimbra): Catarina Silva; Centro Hospitalar de Leiria (Leiria): Carolina Roriz; Hospital São Francisco Xavier (Lisboa): Pedro Póvoa; Hospital Beatriz Ângelo (Loures): Patricia Patricio; Centro Hospitalar e Universitário São João, Infectious Diseases Intensive Care Unit (Porto): Maria Lurdes Santos; Centro Hospitalar Universitário de São João, Serviço de Medicina Intensiva (Porto): Vasco Costa, Pedro Cunha; Centro Hospitalar Universitário do Porto, Hospital Santo Antonio (Porto): Celina Gonçalves; Centro Hospitalar de Entre o Douro e Vouga (Santa Maria da Feira): Sandra Nunes; Hospital Pedro Hispano (Senhora da Hora): João Camões; Centro Hospitalar Vila Nova de Gaia/Espinho (Vila Nova de Gaia): Diana Adrião; Centro Hospitalar de Tondela-Viseu, EPE (Viseu): Ana Oliveira;
QATAR: Hamad Medical Corporation (Doha): Alwakra Hospital (Alwakra): Ali Omrani; Hamad General Hospital, HGH ICU (Doha): Muna Al Maslamani; Hamad General Hospital, HMC- MICU (Doha): Abdurrahmaan Suei elbuzidi; Hamad Medical Corporation, Accident and Emergency (Doha): Bara Mahmoud Al qudah; Hazem Mubarak General Hospital, HMGH-1 (Doha): Abdel Rauof Akkari, Mohamed Alkhatteb; Hazem Mubarak General Hospital, HMGH-2 (Doha): Anas Baiou; Hazem Mubarak General Hospital, HMGH-3: Ahmed Husain; Hazem Mubarak General Hospital, HMGH-4 (Doha): Mohamed Alwraidat, Ibrahim Abdulsalam Saif; Hazem Mubarak General Hospital, HMGH-5 (Doha): Dana Bakdach; Hazem Mubarak General Hospital, HMGH-6 (Doha): Amna Ahmed, Mohamed Aleef; The Cuban Hospital, TCH ICU (Dukhan): Awadh Bintaher;
ROMANIA: Clinical Emergency County Hospital (Cluj-Napoca): Cristina Petrisor;
RUSSIA: State budgetary healthcare institution ‘Research Institute-regional clinical hospital named after Professor Ochapovsky S.V’ (Krasnodar): Evgeniy Popov; City Clinical Hospital № 40 (Moscow): Ksenia Popova; Federal State Budgetary Institution ‘National Medical and Surgical Center named after N.I. Pirogov’ of the Ministry of Healthcare of the Russian Federation (Moscow): Mariia Dementienko; FGBU ‘National Medical-Surgery Hospital by N.I.Pirogov’ (Moscow): Boris Teplykh; FSBI < National Medical Research Center for Obstetrics, Gynaecology and Perinatology named after Academician V.I. Kulakov > Ministry of Healthcare of the Russian Federation (Moscow): Alexey Pyregov; Moscow City Hospital N. 52 (Moscow): Liubov Davydova; Privolzhskiy District Medical Center (Nizhny Novgorod): Belskii Vladislav; Novosibirsk State University with clinical facility City Clinical Hospital #25 (Novosibirsk): Elena Neporada, Ivan Zverev; Botkin's Hospital (St. Petersburg): Svetlana Meshchaninova; First Pavlov State Medical University of St. Petersburg, Anesthesiology and Intensive Care №2 (St. Petersburg): Dmitry Sokolov; First Pavlov State Medical University of St. Petersburg, ICU №2 (St. Petersburg): Elena Gavrilova; First Pavlov State Medical University of St. Petersburg, Scientific Clinical Center of Anesthesiology and Resuscitation (St. Petersburg): Irena Shlyk; Saint Petersburg State Medical Institution ‘City Hospital No. 38 named after N. A. Semashko’ (St. Petersburg): Igor Poliakov; War Veteran’s Hospital, CПб ГБУЗ Гocпитaль для вeтepaнoв вoйн (St. Petersburg): Mapинa Bлacoвa;
SAUDI ARABIA: Pharmacy Practice Department, Faculty of Pharmacy, King Abdulaziz University Hospital (Jeddah): Ohoud Aljuhani, Amina Alkhalaf; King Abdulaziz Medical City (Riyadh): Felwa Bin Humaid, Yaseen Arabi; King Saud Medical City: Ahmed Kuhail; Prince Sultan Medical Military Center, GICU1 (Riyadh): Omar Elrabi; Prince Sultan Medical Military Center, GICU2 (Riyadh): Madihah Alghnam;
SINGAPORE: Ng Teng Fong General Hospital, Jurong Health, NUHS (Singapore): Amit Kansal; Sengkang General Hospital (Singapore): Vui Kian Ho; Tan Tock Seng Hospital (Singapore): Jensen Ng;
SPAIN: Complejo Hospitalario Universitario de A Coruña (A Coruña): Raquel Rodrígez García, Xiana Taboada Fraga; Hospital General La Mancha Centro (Alcázar de San Juan): Mª del Pilar García-Bonillo, Antonio Padilla-Serrano; Hospital Universitario San Agustín (Aviles): Marta Martin Cuadrado; Hospital Clinic Barcelona (Barcelona): Carlos Ferrando; Hospital General Universitario de Castellon (Castellon de la Plana): Ignacio Catalan-Monzon, Laura Galarza; Hospital Universitario de Getafe (Getafe): Fernando Frutos-Vivar, Jorge Jimenez, Carmen Rodríguez-Solis; Hospital San Jorge (Huesca): Enric Franquesa-Gonzalez; Complejo Hospitalario Insular Materno Infantil (Las Palmas de Gran Canaria): Guillermo Pérez Acosta, Luciano Santana Cabrera; Hospital Universitario Severo Ochoa (Leganes): Juan Pablo Aviles Parra, Francisco Muñoyerro Gonzalez; Hospital Rafael Mendez (Lorca): Maria del Carmen Lorente Conesa; Hospital Universitario Lucus Augusti (Lugo): Ignacio Yago Martinez Varela; Hospital HM Sanchinarro (Madrid): Orville Victoriano Baez Pravia; Hospital Universitario de Torrejón (Madrid): Maria Cruz Martin Delgado, Carlos Munoz de Cabo; Hospital Universitario Fundacion Jimenez Diaz (Madrid): Ana-Maria Ioan, Cesar Perez-Calvo, Arnoldo Santos; Hospital Universitario Infanta Leonor (Madrid): Ane Abad-Motos, Javier Ripolles-Melchor; Hospital Universitario La Paz (Madrid): Belén Civantos Martin, Santiago Yus Teruel; Hospital Universitario Príncipe de Asturias (Madrid): Juan Higuera Lucas; Hospital Universitario Ramón y Cajal (Madrid): Aaron Blandino Ortiz, Raúl de Pablo Sánchez; Regional University Hospital of Malaga (Malaga): Jesús Emilio Barrueco-Francioni; Hospital Universitario Central de Asturias (Oviedo): Lorena Forcelledo Espina; Hospital Quironsalud Palmaplanas (Palma de Mallorca): José M. Bonell-Goytisolo; H.U. Son Llàtzer (Palma de Mallorca): Iñigo Salaverria, Antonia Socias Mir; Complejo Hospitalario Universitario de Santiago de Compostela (Santiago de Compostela): Emilio Rodriguez-Ruiz; Complejo Asistencial de Segovia (Segovia): Virginia Hidalgo Valverde, Patricia Jimeno Cubero; Hospital Nuestra Señora Del Prado (Talavera de la Reina): Francisca Arbol Linde, Nieves Cruza Leganes; Hospital Provincial de Toledo (Toledo): Juan Maria Romeu; Hospital Verge de la Cinta (Tortosa): Pablo Concha; Hospital Universitario Río Hortega, Servicio de Medicina Intensiva (Valladolid): José Angel Berezo-Garcia, Virginia Fraile; Hospital Universitario Río Hortega, Servicio de Medicina Intensiva, Unidad 2 (Valladolid): Cristina Cuenca-Rubio, David Perez-Torres; Hospital Clínic Universitari de Valencia (Valencia): Ainhoa Serrano; Hospital Universitario de La Plana (Vila-Real): Clara Martínez Valero; Hospital Comarcal Vinaroz (Vinaroz): Andrea Ortiz Suner; Hospital Universitario de Alava (Vitoria-Gasteiz): Leire Larrañaga, Noemi Legaristi; Hospital Virgen de la Concha (Zamora): Gerardo Ferrigno;
SUDAN: Aliaa Specialist Hospital (Omdurman): Safa Khlafalla;
SURINAME: Academisch Ziekenhuis Paramaribo (Paramaribo): Rosita Bihariesingh-Sanchit;
SWEDEN: Hallands Sjukhus (Halmstad): Frank Zoerner; Karolinska University Hospital (Huddinge): Jonathan Grip, Kristina Kilsand; Sunderby Hospital (Luleå): Jonas Österlind; Akademiska Sjukhuset, Uppsala Univeristy Hospital (Uppsala): Magnus von Seth; Västerviks Sjukhus (Västerviks): Johan Berkius;
SWITZERLAND: Clinica Luganese Moncucco (Lugano): Samuele Ceruti, Andrea Glotta;
TURKEY: Ankara City Hospital / General Hospital (Ankara): Seval Izdes; Ankara City Hospital Orthopedics and Neurology Hospital (Ankara): Işıl Özkoçak Turan; Gulhane Egitim ve Arastirma Hastanesi (Ankara): Ahmet Cosar; Hacettepe University (Ankara): Burcin Halacli; University of Health Sciences Kecioren Training and Research Hospital (Ankara): Necla Dereli; Derince Research and Education Hospital, Health Sciences University (Derince / Kocaeli): Mehmet Yilmaz; Düzce University School of Medicine (Düzce): Türkay Akbas; Gaziantep University (Gaziantep): Gülseren Elay; Giresun Üniversitesi Prof. Dr. A. İlhan Özdemir Eğitim Araştırma Hastanesi (Giresun): Selin Eyüpoğlu; Kartal Dr. Lütfí Kirdar Şehír Hastanesí (Istanbul): Yelíz Bílír, Kemal Tolga Saraçoğlu; SBU Kanuni Sultan Suleyman Education and Training Hospital (Istanbul): Ebru Kaya, Ayca Sultan Sahin; Ege University School of Medicine (Izmir): Pervin Korkmaz Ekren; Niğde Research and Training Hospital (Niğde): Tuğçe Mengi; Sakarya University Education Research Hospital (Sakarya): Kezban Ozmen Suner, Yakup Tomak; Kanuni Education and Training Hospital (Trabzon): Ahmet Eroglu;
UNITED ARAB EMIRATES: Mediclinic City Hospital (Dubai): Asad Alsabbah;
UNITED KINGDOM: Aberdeen Royal Infirmary (Aberdeen): Katie Hanlon; Belfast City Hospital (Belfast): Kevin Gervin, Sean McMahon; Ulster Hospital (Belfast): Samantha Hagan; Queen Elizabeth Hospital, University Hospitals Birmingham NHS Foundation Trust (Birmingham): Caroline V Higenbottam, Randeep Mullhi, Lottie Poulton, Tomasz Torlinski; Royal Blackburn Hospital (Blackburn): Allen Gareth, Nick Truman; West Suffolk Hospital NHS foundation Trust (Bury St Edmunds): Gopal Vijayakumar; Cambridge University Hospitals (Cambridge): Chris Hall, Alasdair Jubb; Royal Papworth Hospital NHS Foundation Trust (Cambridge): Lenka Cagova, Nicola Jones; Countess Of Chester (Chester): Sam Graham, Nicole Robin; Darlington Memorial Hospital (Darlington): Amanda Cowton; Altnagelvin Hospital—WHSCT (Derry): Adrian Donnelly; Doncaster Royal Infirmary (Doncaster): Natalia Singatullina; University Hospital of North Durham (Durham): Melanie Kent; Royal Devon & Exeter NHS Foundation Trust (Exeter): Carole Boulanger; Royal Surrey Hospital (Guildford): Zoë Campbell, Elizabeth Potter; Royal Gwent Hospital (Gwent): Natalie Duric, Tamas Szakmany; Harefield Hospital, Royal Brompton and Harefield NHS Foundation Trust (Harefield): Orinta Kviatkovske, Nandor Marczin; The Princess Alexandra Hospital NHS Trust (Harlow): Caroline Ellis, Rajnish Saha; Harrogate District Hospital (Harrogate): Chunda Sri-Chandana; NHS University Hospital Crosshouse (Kilmarnock): John Allan; Kingston Hospital (Kingston upon Thames): Lana Mumelj, Harish Venkatesh; University Hospitals of Morecambe Bay NHS Foundation Trust, Royal Lancaster Infirmary (Lancaster): Vera Nina Gotz; St Helens and Knowsley Teaching Hospitals NHS Trust (Liverpool): Anthony Cochrane; Guy's & St Thomas' Hospital (London): Nuttha Lumlertgul, Barbara Ficial; Homerton University Hospital NHS Foundation Trust (London): Susan Jain; Royal Brompton Hospital, Royal Brompton and Harefield NHS Foundation Trust (London): Giulia Beatrice Crapelli, Aikaterini Vlachou; Maidstone Hospital (Maidstone): David Golden; Borders General Hospital (Melrose): Sweyn Garrioch; James Cook University (Middlesbrough): Jeremy Henning, Gupta Loveleena; The Tunbridge Wells Hospital (Pembury): Miriam Davey; Queen's Hospital (Romford): Lina Grauslyte, Erika Salciute-Simene; Salisbury NHS Foundation Trust (Salisbury): Martin Cook; Stepping Hill Hospital (Stockport): Danny Barling, Phil Broadhurst; University Hospital of North Tees (Stockton-on-Tees): Sarah Purvis; Royal Cornwall Hospitals NHS Trust (Truro): Spivey Michael; Warwick Hospital (Warwick): Benjamin Shuker; Royal Hampshire County Hospital (Winchester): Irina Grecu; Queen Elizabeth Hospital (Woolwich): Daniel Harding; Bassetlaw District General Hospital (Worksop): Natalia Singatullina;
UNITED STATES: University of New Mexico School of Medicine (Albuquerque, NM): James T. Dean, Nathan D. Nielsen; Brooklyn VA Medical Center (Brooklyn, VA): Sama Al-Bayati; SUNY Downstate Medical Center (Brooklyn, NY): Mohammed Al-Sadawi; Cooper University Hospital (Camden, NJ): Mariane Charron; St. Joseph Hospital (Denver, CO): Peter Stubenrauch; Ochsner Medical Center (New Orleans, LA): Jairo Santanilla, Catherine Wentowski; University of Utah Health (Salt Lake City, UT): Dorothea Rosenberger; Stony Brook University Hospital (Stony Brook, NY): Polikseni Eksarko, Randeep Jawa.
Funding
European Society of Intensive Care Medicine. ACM is supported by a Clinician Scientist Fellowship from the Medical Research Council (MR/V006118/1).
Author information
Authors and Affiliations
Consortia
Contributions
Conceptulalisation: ACM, AE, PP, MC, JdW. Methodology: KK, TdC, AE, HJdG, PE. Software: KK, TdC, AE, HJdG, PE. Formal analysis: KK, TdC. Investigation: ACM, AE, PE, PP, RM, DK, SJ, NN, AJ, JdW. Provision of resources: MC, JdW. Data curation: TdC, AE, HJdG. Writing -original draft: ACM, KK, TdC, JdW. Writing -review and editing: ACM, KK, TdC, AE, PE, PP, RM, DK, SJ, NN, AJ, MC, JdW. Supervision: ACM, MC, JdW. Project administration: MC, JdW. Funding: JdW. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study received approval from Ghent University Hospital Ethics committee, registration BC-07826 and appropriate approvals at each participating site in line with local regulations. Where required by local regulations consent for inclusion was sought from the patient or their representative, other sites approved consent waiver for use of anonymised, routinely collected data.
Consent to publish
Not applicable. No individual patient data are included.
Competing interests
ACM sits on the scientific advisory board of Cambridge Infection Diagnostics. PP received fees for consulting and lectures to Gilead, Pfizer, MSD and Sanofi. NN has received consulting honoraria from Johnson & Johnson and serves on the scientific advisory board of Adrenomed. The other authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: an error in the article title was corrected.
Supplementary Information
Additional file 1:
Case report form.
Additional file 2:
Supplemental data.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Conway Morris, A., Kohler, K., De Corte, T. et al. Co-infection and ICU-acquired infection in COVID-19 ICU patients: a secondary analysis of the UNITE-COVID data set. Crit Care 26, 236 (2022). https://doi.org/10.1186/s13054-022-04108-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-022-04108-8