Abstract
Background
Heart rate, acidosis, consciousness, oxygenation, and respiratory rate (HACOR) have been used to predict noninvasive ventilation (NIV) failure. However, the HACOR score fails to consider baseline data. Here, we aimed to update the HACOR score to take into account baseline data and test its predictive power for NIV failure primarily after 1–2 h of NIV.
Methods
A multicenter prospective observational study was performed in 18 hospitals in China and Turkey. Patients who received NIV because of hypoxemic respiratory failure were enrolled. In Chongqing, China, 1451 patients were enrolled in the training cohort. Outside of Chongqing, another 728 patients were enrolled in the external validation cohort.
Results
Before NIV, the presence of pneumonia, cardiogenic pulmonary edema, pulmonary ARDS, immunosuppression, or septic shock and the SOFA score were strongly associated with NIV failure. These six variables as baseline data were added to the original HACOR score. The AUCs for predicting NIV failure were 0.85 (95% CI 0.84–0.87) and 0.78 (0.75–0.81) tested with the updated HACOR score assessed after 1–2 h of NIV in the training and validation cohorts, respectively. A higher AUC was observed when it was tested with the updated HACOR score compared to the original HACOR score in the training cohort (0.85 vs. 0.80, 0.86 vs. 0.81, and 0.85 vs. 0.82 after 1–2, 12, and 24 h of NIV, respectively; all p values < 0.01). Similar results were found in the validation cohort (0.78 vs. 0.71, 0.79 vs. 0.74, and 0.81 vs. 0.76, respectively; all p values < 0.01). When 7, 10.5, and 14 points of the updated HACOR score were used as cutoff values, the probability of NIV failure was 25%, 50%, and 75%, respectively. Among patients with updated HACOR scores of ≤ 7, 7.5–10.5, 11–14, and > 14 after 1–2 h of NIV, the rate of NIV failure was 12.4%, 38.2%, 67.1%, and 83.7%, respectively.
Conclusions
The updated HACOR score has high predictive power for NIV failure in patients with hypoxemic respiratory failure. It can be used to help in decision-making when NIV is used.
Similar content being viewed by others
Introduction
Noninvasive ventilation (NIV) reduces inspiratory muscle effort and improves oxygenation in hypoxemic patients with acute respiratory failure [1]. As it offers several major advantages over invasive ventilation (e.g., preserving the ability to swallow, cough, and communicate verbally), NIV is widely used to avoid intubation [2]. However, the rate of NIV failure is 40–54% in hypoxemic patients [3,4,5,6]. Moreover, NIV failure is associated with increased mortality [7, 8]. Among patients who experience NIV failure, late failure further increases mortality [5, 9]. Therefore, early identification of patients at high risk for NIV failure and early application of invasive ventilation may reduce mortality.
Our team previously developed a scale that produces the HACOR score, which takes into account heart rate, acidosis, consciousness, oxygenation, and respiratory rate (Additional file 1: Table 1), to predict NIV failure in patients with hypoxemic respiratory failure [5]. This scale was developed based on data from a respiratory intensive care unit (ICU). Although it has high predictive power for NIV failure, extensive use of the scale may be limited by the fact that the majority of respiratory failure results from respiratory etiology. Furthermore, baseline data such as the presence of acute respiratory distress syndrome (ARDS), septic shock, immunosuppression, organ failure, and so on are also associated with NIV failure [6, 7, 10, 11]. Because these baseline data may improve the predictive power of the score, we aimed to incorporate them into the HACOR score to improve its predictive power for NIV failure in patients with hypoxemic respiratory failure.
Methods
This multicenter prospective observational study was performed in 17 hospitals in China from September 2017 to September 2021 and one hospital in Turkey from November 2018 to August 2020. The study protocol was approved by the ethics committee of the First Affiliated Hospital of Chongqing Medical University (No. 2016150) and the ethics committee of Istanbul University Cerrahpasa (No. 88295). Informed consent was obtained from patients or their family members.
Patients admitted to the ICU for NIV due to hypoxemic respiratory failure were enrolled. However, patients who were younger than 16 years old, who experienced hypercapnic respiratory failure, who required emergency intubation, who underwent the use of NIV after extubation, who received NIV after accidental extubation, and who received NIV because of acute exacerbation of chronic obstructive pulmonary disease were excluded. Patients who received NIV because of high-flow nasal cannula failure or had undergone NIV more than 2 h before being admitted to the participating center were also excluded. Emergency intubation means that intubation was required immediately because the patient was in respiratory or cardiac arrest, was experiencing respiratory pauses with loss of consciousness, or was gasping for air.
All patients who used NIV were managed by attending physicians, respiratory therapists, and nurses in charge based on current guidelines, consensus, and previously published methods [5, 12,13,14,15]. The indications for NIV were as follows: (1) respiratory rate > 25 breaths/min, (2) clinical presentation of respiratory distress at rest (such as active contraction of the accessory inspiratory muscles or paradoxical abdominal motion), or (3) PaO2 < 60 mmHg at room air or PaO2/FiO2 < 300 mmHg with supplemental oxygen. If supplemental oxygen was used, FiO2 was estimated as follows: FiO2 (%) = 21 + 4 × flow (L/min) [16, 17]. However, the use of NIV was at the physician’s discretion. Continuous positive airway pressure (CPAP) or bilevel positive pressure ventilation was used to relieve patients’ dyspnea. Parameters were increased gradually based on patients’ tolerance. CPAP, expiratory positive airway pressure, or positive end expiratory pressure was usually maintained between 4 and 10 cmH2O. Inspiratory pressure was maintained between 10 and 20 cmH2O. The fractional concentration of oxygen was set to achieve peripheral oxygen saturation greater than 92%. In addition, appropriate strategies were used to improve NIV tolerance, such as controlling leakage, keeping the anchoring system as comfortable as possible, providing adequate humidification, alternatively using different interfaces, and administering sedation [18].
We encouraged patients to use NIV as long as possible initially. If their respiratory distress was relieved and oxygenation improved, NIV was used intermittently until patients could be completely liberated. If respiratory failure progressively deteriorated, intubation for invasive mechanical ventilation was performed. The major criteria for intubation were as follows: respiratory or cardiac arrest, PaO2/FiO2 < 100 mmHg after NIV intervention, the development of conditions necessitating intubation to protect the airway (coma or seizure disorders) or to manage copious tracheal secretions, and hemodynamic instability without response to fluids or vasoactive agents [5, 19]. Minor criteria were as follows: PaO2/FiO2 < 150 mmHg after NIV intervention, respiratory rate > 35 breaths/min, lack of improvement in respiratory muscle fatigue, and acidosis with pH < 7.35. Intubation was recommended if one major criterion or more than two minor criteria were reached. However, the decision to intubate was at the discretion of the attending physician. The need for intubation was defined as NIV failure [6].
We collected baseline data, vital signs, and arterial blood gas (ABG) from initiation to 24 h of NIV. Baseline data included ICU type, age, sex, reason for NIV, underlying disease, severity of disease (assessed by sequential organ failure assessment [SOFA] score), presence of COVID-19, presence of septic shock, and presence of ARDS. The presence of COVID-19 means that hypoxemic acute respiratory failure resulted from SARS-CoV-2 infection. Vital signs included consciousness (assessed by the Glasgow Coma Scale), heart rate, respiratory rate, systolic blood pressure, and diastolic blood pressure. The SOFA score was calculated before NIV. Urine output was obtained from medical records. If urine output was not available from medical records, it was estimated by the patient. Pneumonia was diagnosed based on current guidelines (i.e., a radiographic infiltrate that is new or progressive along with clinical findings suggesting infection, including the new onset of fever, purulent sputum, leukocytosis, shortness of breath, and a decline in oxygenation) [20, 21].
The aim of the current study was to update the HACOR score to predict NIV failure in hypoxemic patients. We used data collected in nine hospitals in Chongqing, China (N = 1451), to train the scale (training cohort). Data from another eight hospitals elsewhere in China and one hospital in Turkey (N = 728) were used to validate the scale (external validation cohort). The current reporting is based on transparent reporting of a multivariable prediction model for individual prognosis or diagnosis [22].
Statistical analysis
We used SPSS (version 25.0) and R (version 4.0.5) to analyze the data. Given an estimated NIV failure rate of 44% and estimated sensitivity and specificity of more than 70% (assuming the expected standard error of 5%), at least 734 patients were required to update the HACOR score for α = 0.05 [5]. Multiple imputations were performed to address missing data. The area under the receiver operating characteristic curve (AUC) was used to analyze the predictive power of NIV failure. A p value less than 0.05 was considered to be statistically significant.
The data from the training cohort were used to update the HACOR score. First, we selected variables via elastic net regularization, using logistic models and tenfold cross-validation, selecting the regularization parameter λ when binomial deviation was within one standard error of the minimum [23, 24]. Collinearity between continuous variables was identified if the absolute value of the correlation coefficients was > 0.7 [25]. The selected variables were used to develop a basic score for predicting NIV failure. Then, we combined this basic score and the original HACOR score to create the updated HACOR score. The final model for goodness of fit was tested using the Hosmer–Lemeshow test. Details of the development of the updated HACOR score in the training cohort can be seen in Additional file 1: Method 1. The predictive powers for NIV failure of the original and updated HACOR scores were compared with the Hanley and McNeil method [26]. For clinical reference, three cutoff values were selected for probabilities of NIV failure equal to 25%, 50%, and 75% [27]. Probabilities of NIV failure of less than 25%, 25–50%, 50–75%, and more than 75% were defined as low, moderate, high, and very high risk for NIV failure, respectively. According to the original HACOR study, patients with HACOR scores ≤ 5 and > 5 were defined as being at low and high risk for NIV failure, respectively [5].
Results
Demographic characteristics
The flow of patient screening is summarized in Additional file 1: Fig. 1. In the training cohort, 24 patients had missing data (0.2% for ABG before NIV, 1.4% for ABG after 1–2 h of NIV, and 0.07% for SOFA score). In the validation cohort, 18 patients had missing data (0.1% for ABG before NIV, 0.1% for heart rate before NIV, and 2.2% for ABG after 1–2 h of NIV). All missing data were interpolated by multiple imputations.
In the training cohort, 529 patients (36.5%) experienced NIV failure (Table 1). In the validation cohort, 328 patients (45.1%) experienced NIV failure. In both cohorts, about half of patients were from medical ICUs, one-third were from mixed ICUs, and the rest were from surgical ICUs.
In the training cohort, patients who experienced NIV failure were more likely to have septic shock, pneumonia, pulmonary ARDS, hypertension, chronic kidney disease, and immunosuppression compared to those who experienced successful NIV. However, they were less likely to have pancreatitis and cardiogenic pulmonary edema (CPE). These results were confirmed in the validation cohort.
Development of the updated HACOR score in the training cohort
Details of the development of the updated HACOR score are summarized in Additional file 1: Method 1. A diagnosis of pneumonia was a risk factor for NIV failure, and a diagnosis of CPE was a protective factor identified by elastic net logistic regression (Additional file 1: Figs. 2 and 3). The presence of pulmonary ARDS, immunosuppression, or septic shock and the SOFA score before NIV were risk factors for NIV failure. Thus, we updated the HACOR score to take these six pre-NIV variables into account (Additional file 1: Tables 2–4).
Therefore, the updated HACOR score is as follows: original HACOR score + 0.5 × SOFA + 2.5 if pneumonia is diagnosed – 4 if CPE is diagnosed + 3 if pulmonary ARDS is present + 1.5 if immunosuppression is present + 2.5 if septic shock is present. The p value for goodness of fit was 0.21 when the Hosmer–Lemeshow test was used. This indicates that the final model was properly fitted.
The predictive powers for NIV failure of the original and updated HACOR scores
In both cohorts, the AUCs for predicting NIV failure were higher when tested by the updated HACOR score than the original HACOR score from initiation to 24 h of NIV (all p values < 0.01; Table 2). The AUCs for predicting NIV failure were 0.85 (95% confidence interval 0.84–0.87) and 0.78 (0.75–0.81) tested by the updated HACOR score assessed after 1–2 h of NIV in the training and validation cohorts, respectively. The AUCs in the different subgroups are summarized in Table 3.
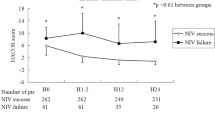
From initiation to 24 h of NIV, the updated HACOR score was much higher in patients who experienced NIV failure than those who experienced successful NIV (Fig. 1). The rate of NIV failure increased with an increase in the updated HACOR score, whether it was assessed before NIV or after 1–2, 12, or 24 h of NIV (Additional file 1: Figs. 4 and 5). In patients at low risk as assessed by the original HACOR score, the rate of NIV failure was greater than 50% if the updated HACOR score was more than 12 (Fig. 2). In contrast, in patients at high risk as assessed by the original HACOR score, the rate of NIV failure was low in most cases if the updated HACOR score was less than 8.
Updated HACOR scores of patients with successful NIV and NIV failure from initiation to 24 h of NIV. Data are means and standard deviations. *p < 0.01 for the comparison of patients with successful NIV versus NIV failure. H0 = before NIV, H1-2 = after 1–2 h of NIV, H12 = after 12 h of NIV, H24 = after 24 h of NIV, NIV = noninvasive ventilation, HACOR = heart rate, acidosis, consciousness, oxygenation, and respiratory rate
Rate of NIV failure within 24 h of NIV. A1, B1, and C1 indicate the rate of NIV failure in different subgroups classified by updated HACOR scores among patients with an original HACOR score ≤ 5. A2, B2, and C2 indicate the rate of NIV failure in different subgroups classified by updated HACOR scores among patients with an original HACOR score > 5. NIV = noninvasive ventilation, HACOR = heart rate, acidosis, consciousness, oxygenation, and respiratory rate
When 7, 10.5, and 14 points of updated HACOR score were selected as cutoff values, the probability of NIV failure was 25%, 50%, and 75%, respectively. The predictive power is reported in Table 4. Using the three cutoff values, we classified patients as being at low (≤ 7), moderate (7.5–10.5), high (11–14), and very high (> 14) risk for NIV failure. The cumulative incidence of NIV failure is summarized in Fig. 3. For all patients, the rate of NIV failure was 12.4%, 38.2%, 67.1%, and 83.7% among patients with a low, moderate, high, and very high probability of NIV failure, respectively.
Cumulative incidence of NIV failure in patients at low, moderate, high, and very high risk for NIV failure when the updated HACOR score is assessed after 1–2 h of NIV. Patients with updated HACOR scores of ≤ 7, 7.5–10.5, 11–14, and > 14, respectively, were classified as being at low, moderate, high, and very high risk for NIV failure. NIV = noninvasive ventilation, HACOR = heart rate, acidosis, consciousness, oxygenation, and respiratory rate
Discussion
The current study evaluates and confirms the power of an updated HACOR score that incorporates data on six baseline variables to predict NIV failure. The predictive power for NIV failure tested by the updated HACOR score was significantly improved compared to that of the original HACOR score. Three cutoff values indicating low, moderate, high, and very high probability of NIV failure were developed to aid clinical staff in decision-making.
The original HACOR score assessed heart rate, acidosis, consciousness, oxygenation, and respiratory rate [5]. The predictive power for NIV failure was high in the original study. However, the predictive power in the current study was not as good. In patients at low risk as assessed by the original HACOR score, the rate of NIV failure was high if the updated HACOR score was high. In contrast, in patients at high risk as assessed by the original HACOR score, the rate of NIV failure was low in most cases if the updated HACOR score was low. The reasons for this are as follows: The original HACOR score was developed based on vital signs and ABG results only. However, patients with different baseline data have different risks for NIV failure even when they have similar vital signs and ABG results. The presence of pulmonary ARDS, septic shock, immunosuppression, and organ failure at baseline are associated with NIV failure [6, 7, 10, 11, 28]. Moreover, patients with CPE have a very low rate of NIV failure, which acts as a protective factor against NIV failure [29, 30]. In this study, we incorporated these pre-NIV variables into the original HACOR score to update the score. That is why the predictive power was significantly improved.
In addition, the original HACOR score was developed and validated using data from a respiratory ICU. All patients had a respiratory etiology and were managed by respiratory physicians. However, the updated HACOR score was developed in nine hospitals and validated in another nine hospitals. The patients had different etiologies, came from different ICUs, and were managed by different physicians. Therefore, the patients and physicians in the updated HACOR study were more representative of the real world. This is another reason for the better predictive power of the updated HACOR score than the original one.
The use of NIV in patients with de novo acute respiratory failure, pneumonia, or ARDS is controversial because of the high risk for NIV failure [3, 4, 9, 30]. In some cases, the rate of NIV failure can reach 70% [31]. Guidelines contain no recommendations for using NIV with these patients [12]. In our study, the updated HACOR score had high predictive power for NIV failure in these patients whether it was assessed after 1–2, 12, or 24 h of NIV. A higher updated HACOR score indicates a higher risk for NIV failure. Therefore, the updated HACOR score provides an important reference point for clinical staff managing NIV. In patients at high risk for NIV failure identified by the updated HACOR score, early intubation can be considered.
A good risk scoring system can help clinical staff manage their patients. In our study, the updated HACOR score assessed after 1–2 h of NIV had high predictive power for NIV failure. It can identify patients who are more likely to experience intubation in the future. As late NIV failure is associated with increased mortality [5, 9], close monitoring, more staffing, and better device supply may benefit high-risk patients.
In routine clinical work, physicians may partly refer to the values of PaO2/FiO2 ratio, respiratory rate, and pH before they decided intubation. However, how to combine these variables and other risk factors together to make more suitable decision-making is difficult. One may consider more in PaO2/FiO2 ratio, and the other may consider more in respiratory rate. In other words, the weight is different for different physicians. The main contribution of the updated HACOR score is to calculate the weight in each variable. It took into account the major risk factors and quantitatively calculated the weight in each variable. Although the updated HACOR score may be explained by self-fulfilling prophecy in part, it provides more useful information for physicians to make reasonable decision.
This study has several limitations. First, we enrolled only 47 patients with COVID-19 in this study. This small subsample size may diminish the predictive power for NIV failure. Clinicians should be cautious when assessing the updated HACOR score in COVID-19 patients. Second, although we suggested intubation criteria, the decision to intubate was at the discretion of the attending physician. However, this reflects true conditions in the real world and thus may partly improve the generalizability of the updated HACOR score. Third, the benefit of an updated HACOR score is unclear, as the current study was observational in design. The effects of an updated HACOR score should be strictly demonstrated in randomized controlled trials. Fourth, we did not predefine the interface or a sedation plan. These issues were determined by the attending physicians in charge. Whether the interface or sedation plan is associated with NIV failure is unclear. Fifth, the expired tidal volume (standardization to predicted body weight) is associated with NIV failure [4]. In our study, most of the ventilators have used single-limb circuit. It is unable to measure expired tidal volume. In addition, the predicted body weight is unavailable because we did not record the patient’s height. So, we did not include the tidal volume in the model.
Conclusions
The updated HACOR score, which combines data on six baseline variables and the five original scale items, has significantly improved predictive power for NIV failure compared to the original HACOR score. A higher score indicates a higher risk for NIV failure. Patients with updated HACOR scores of ≤ 7, 7.5–10.5, 11–14, and > 14, respectively, were classified as having a low, moderate, high, and very high probability of NIV failure. This updated score provides a reference for clinical staff in decision-making.
Availability of data and materials
The dataset used and/or analyzed during the current study is available from the corresponding author on reasonable request.
Abbreviations
- HACOR:
-
Heart rate, acidosis, consciousness, oxygenation, and respiratory rate
- NIV:
-
Noninvasive ventilation
- AUC:
-
Area under the receiver operating characteristic curve
- CI:
-
Confidence interval
- OR:
-
Odds ratio
- ARDS:
-
Acute respiratory distress syndrome
- CPE:
-
Cardiogenic pulmonary edema
- SOFA:
-
Sequential organ failure assessment
- ICU:
-
Intensive care unit
- GCS:
-
Glasgow Coma Scale
- SE:
-
Sensitivity
- SP:
-
Specificity
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- + LR:
-
Positive likelihood ratio
- –LR:
-
Negative likelihood ratio
References
L’Her E, Deye N, Lellouche F, et al. Physiologic effects of noninvasive ventilation during acute lung injury. Am J Respir Crit Care Med. 2005;172:1112–8.
Jaber S, Bellani G, Blanch L, et al. The intensive care medicine research agenda for airways, invasive and noninvasive mechanical ventilation. Intensive Care Med. 2017;43:1352–65.
Tonelli R, Fantini R, Tabbì L, et al. Early inspiratory effort assessment by esophageal manometry predicts noninvasive ventilation outcome in de novo respiratory failure. A pilot study. Am J Respir Crit Care Med. 2020;202:558–67.
Carteaux G, Millán-Guilarte T, De Prost N, et al. Failure of noninvasive ventilation for de novo acute hypoxemic respiratory failure: Role of tidal volume. Crit Care Med. 2016;44:282–90.
Duan J, Han X, Bai L, et al. Assessment of heart rate, acidosis, consciousness, oxygenation, and respiratory rate to predict noninvasive ventilation failure in hypoxemic patients. Intensive Care Med. 2017;43:192–9.
Thille AW, Contou D, Fragnoli C, et al. Non-invasive ventilation for acute hypoxemic respiratory failure: intubation rate and risk factors. Crit Care. 2013;17:R269.
Cortegiani A, Madotto F, Gregoretti C, et al. Immunocompromised patients with acute respiratory distress syndrome: secondary analysis of the LUNG SAFE database. Crit Care. 2018;22:157.
Avdeev SN, Yaroshetskiy AI, Tsareva NA, et al. Noninvasive ventilation for acute hypoxemic respiratory failure in patients with COVID-19. Am J Emerg Med. 2021;39:154–7.
Carrillo A, Gonzalez-Diaz G, Ferrer M, et al. Non-invasive ventilation in community-acquired pneumonia and severe acute respiratory failure. Intensive Care Med. 2012;38:458–66.
Duan J, Chen L, Liang G, et al. Noninvasive ventilation failure in patients with hypoxemic respiratory failure: the role of sepsis and septic shock. Ther Adv Respir Dis. 2019;13:1753466619888124.
Rodríguez A, Ferri C, Martin-Loeches I, et al. Risk factors for noninvasive ventilation failure in critically ill subjects with confirmed influenza infection. Respir Care. 2017;62:1307–15.
Rochwerg B, Brochard L, Elliott MW, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50:1602426.
Luo Q, Chen RC. The consensus of application of noninvasive positive pressure ventilation in clinical practices. Zhonghua Jie He He Hu Xi Za Zhi. 2009;32:86–98.
Nava S, Hill N. Non-invasive ventilation in acute respiratory failure. Lancet. 2009;374:250–9.
Ferrer M, Esquinas A, Leon M, et al. Noninvasive ventilation in severe hypoxemic respiratory failure: a randomized clinical trial. Am J Respir Crit Care Med. 2003;168:1438–44.
Branson RD, Hess DR, Chatbum RL. Respiratory care equipment. Philadelphia: J.B. Lippincott Company; 1995. p. 55–62.
Wang K, Zhao W, Li J, et al. The experience of high-flow nasal cannula in hospitalized patients with 2019 novel coronavirus-infected pneumonia in two hospitals of Chongqing, China. Ann Intensive Care. 2020;10:37.
Cammarota G, Simonte R, De Robertis E. Comfort during non-invasive nentilation. Front Med (Lausanne). 2022;9: 874250.
Antonelli M, Conti G, Esquinas A, et al. A multiple-center survey on the use in clinical practice of noninvasive ventilation as a first-line intervention for acute respiratory distress syndrome. Crit Care Med. 2007;35:18–25.
Levy ML, Le Jeune I, Woodhead MA, et al. Primary care summary of the British Thoracic Society Guidelines for the management of community acquired pneumonia in adults: 2009 update. Endorsed by the Royal College of General Practitioners and the Primary Care Respiratory Society UK. Prim Care Respir J. 2010;19:21–7.
Kalil AC, Metersky ML, Klompas M, et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;63:e61–111.
Collins GS, Reitsma JB, Altman DG, et al. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ. 2015;350: g7594.
Leisman DE, Harhay MO, Lederer DJ, et al. Development and reporting of prediction models: Guidance for authors from editors of respiratory, sleep, and critical care journals. Crit Care Med. 2020;48:623–33.
Lyu M, Zhou J, Jiao L, et al. Deciphering a TB-related DNA methylation biomarker and constructing a TB diagnostic classifier. Mol Ther Nucleic Acids. 2022;27:37–49.
Dormann CF, Elith J, Bacher S, et al. Collinearity: a review of methods to deal with it and a simulation study evaluating their performance. Echography. 2013;36:27–46.
Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983;148:839–43.
Confalonieri M, Garuti G, Cattaruzza MS, et al. A chart of failure risk for noninvasive ventilation in patients with COPD exacerbation. Eur Respir J. 2005;25:348–55.
Shu W, Guo S, Yang F, et al. Association between ARDS etiology and risk of noninvasive ventilation failure. Ann Am Thorac Soc. 2022. https://doi.org/10.1513/AnnalsATS.202102-161OC.
Tallman TA, Peacock WF, Emerman CL, et al. Noninvasive ventilation outcomes in 2,430 acute decompensated heart failure patients: an ADHERE registry analysis. Acad Emerg Med. 2008;15:355–62.
Ozyilmaz E, Ugurlu AO, Nava S. Timing of noninvasive ventilation failure: causes, risk factors, and potential remedies. BMC Pulm Med. 2014;14:19.
Rana S, Jenad H, Gay PC, et al. Failure of non-invasive ventilation in patients with acute lung injury: observational cohort study. Crit Care. 2006;10:R79.
Acknowledgements
We thank all the staff members in participating centers to help in data collection.
Funding
This study was supported by Pei Yu Ji Jin of the First Affiliated Hospital of Chongqing Medical University (PYJJ201707).
Author information
Authors and Affiliations
Contributions
JD conceived the study and took responsibility for the integrity of the study. JD, LC, XL, SB, YL, and KW joined in study design, study management, data collection, data analysis, and manuscript preparation. SW, FY, DH, QC, BW, BC, LL, MT, GY, FD, TH, ZZ, ZT, XH, LJ, LB, WH, and RZ joined in patient screening, data collection, data management, and data interpretation, and revised the manuscript. AME and BM joined in manuscript preparation. All authors contributed to the intellectual content of the manuscript and approved the manuscript version submitted for publication. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study protocol was approved by the ethics committee of the First Affiliated Hospital of Chongqing Medical University and Istanbul University Cerrahpasa (No. 2016150 and 88295, respectively). Informed consent was obtained from patients or their family members. And current study was performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
We declare that we have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Supplementary Table 1. Points for each variable in the original HACOR score. Supplementary Table 2. Variables left in the elastic net logistic regression for predicting NIV failure in the training cohort from baseline data. Supplementary Table 3. Basic score for predicting NIV failure in the training cohort. Supplementary Table 4. Combining the basic score and the original HACOR score to predict NIV failure in the training cohort. Supplementary Figure 1. Flow of patient screening and enrollment. Supplementary Figure 2. Change in variable counts in the elastic net logistic regression. Supplementary Figure 3. The selection of variables in the elastic net logistic regression by 10-fold cross-validation. Supplementary Figure 4. Rate of NIV failure in patients in the training cohort with different updated HACOR scores. Supplementary Figure 5. Rate of NIV failure in patients in the validation cohort with different updated HACOR scores. Supplementary Method 1. Details of the development of the updated heart rate, acidosis, consciousness, oxygenation, and respiratory rate (HACOR) score in the training cohort.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Duan, J., Chen, L., Liu, X. et al. An updated HACOR score for predicting the failure of noninvasive ventilation: a multicenter prospective observational study. Crit Care 26, 196 (2022). https://doi.org/10.1186/s13054-022-04060-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-022-04060-7