Abstract
Background
We conducted a systematic review and meta-analysis of randomized controlled trials (RCTs) to assess the association of higher positive end-expiratory pressure (PEEP), as opposed to lower PEEP, with hospital mortality in adult intensive care unit (ICU) patients undergoing invasive mechanical ventilation for reasons other than acute respiratory distress syndrome (ARDS).
Methods
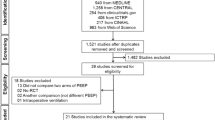
We performed an electronic search of MEDLINE, EMBASE, Scopus, Cochrane Central Register of Controlled Trials, CINAHL, and Web of Science from inception until June 16, 2021 with no language restrictions. In addition, a research-in-progress database and grey literature were searched.
Results
We identified 22 RCTs (2225 patients) comparing higher PEEP (1007 patients) with lower PEEP (991 patients). No statistically significant association between higher PEEP and hospital mortality was observed (risk ratio 1.02, 95% confidence interval 0.89–1.16; I2 = 0%, p = 0.62; low certainty of evidence). Among secondary outcomes, higher PEEP was associated with better oxygenation, higher respiratory system compliance, and lower risk of hypoxemia and ARDS occurrence. Furthermore, barotrauma, hypotension, duration of ventilation, lengths of stay, and ICU mortality were similar between the two groups.
Conclusions
In our meta-analysis of RCTs, higher PEEP, compared with lower PEEP, was not associated with mortality in patients without ARDS receiving invasive mechanical ventilation. Further large high-quality RCTs are required to confirm these findings.
Similar content being viewed by others
Background
Mechanical ventilation (MV) is a potentially life-saving strategy for critically ill patients; however, it can exacerbate or promote lung injury through several mechanisms, overall named ventilator-induced lung injury (VILI) [1]. These include alveolar overdistension (volutrauma and barotrauma) and repetitive opening and closing of the alveoli and small airways (atelectrauma) [2]. Positive end-expiratory pressure (PEEP) has been employed to prevent end-expiratory alveolar collapse and counteract mechanical strain, thus minimizing atelectrauma and alveolar overdistension, respectively [3]. Nonetheless, excessive PEEP may worsen mechanical stress [4, 5] and lead to hemodynamic impairment [6].
Patients suffering from the acute respiratory distress syndrome (ARDS) are more at risk of VILI owing to the small size of the ventilated lung regions and the high number of parenchymal heterogeneities, where mechanical injury may be amplified [7]. The use of higher PEEP, compared to lower PEEP, is associated with reduced mortality among patients with moderate-severe ARDS [8], who better respond to the application of PEEP in terms of increased size of ventilated lung [9], reduced atelectrauma [10], and improved oxygenation [11] than patients with mild ARDS.
Similar to patients with less severe ARDS, patients without ARDS may have a low potential for lung recruitment and be exposed to the increased risk of PEEP-related lung overdistension and hemodynamic compromise [5, 6, 12]. Recently, the restricted versus liberal positive end-expiratory pressure in patients without ARDS (RELAx) study provided evidence that a MV strategy using lower PEEP is non-inferior to a strategy based on higher PEEP in terms of the number of ventilator-free days at day 28 among intensive care unit (ICU) patients without ARDS [13]. A meta-analysis, overall including 1393 individuals from 21 randomized controlled trials (RCTs), showed that higher levels of PEEP were not associated with lower in-hospital mortality or shorter duration of ventilation, but with improved oxygenation and lower risk of hypoxemia and development of ARDS [14]. However, this meta-analysis did not include the RELAx trial, which is by far the largest RCT evaluating the role of PEEP in ICU patients without ARDS. We conducted this updated meta-analysis of RCTs to assess the association of higher PEEP, as opposed to lower PEEP, with hospital mortality in adult ICU patients intubated and mechanically ventilated for reasons other than ARDS.
Methods
Inclusion and exclusion criteria
The following participants, interventions, comparisons, outcomes, and study design (PICOS) question was employed: participants were adult patients undergoing invasive MV in the ICU for reasons other than ARDS; the intervention and comparison were higher PEEP and lower PEEP, respectively; the primary outcome was hospital mortality at the longest follow-up (secondary outcomes are listed in Additional File 1: Online Resource 1); study design was RCT. Studies not comparing different levels of PEEP at the same ventilatory settings were excluded.
Literature search
We performed an electronic search of MEDLINE, EMBASE, Scopus, Cochrane Central Register of Controlled Trials, CINAHL, and Web of Science from inception until June 16, 2021 with no language restrictions. In addition, a research-in-progress database (ClinicalTrials.gov) and grey literature (OpenGrey) were searched. All references of included articles and related reviews were hand searched. Conference proceedings were excluded.
Controlled vocabulary terms (when available), text words, and keywords were variably combined with blocks of terms per concept: (“positive end-expiratory pressure” OR “PEEP”) AND (“randomized controlled trial” OR “RCT”). MEDLINE and Scopus search strategies were adapted for searches in other databases and are reported in Additional File 1: Online Resource 1.
Data collection
The search results were merged and duplicate records of the same report were removed. The remaining studies were stored using Microsoft Excel software (Microsoft Corporation, Redmond, WA). Titles and abstracts were independently screened by two authors (TP, AB) according to the inclusion criteria, and the full texts of potentially relevant reports were retrieved. Reasons for exclusions were detailed and studies that were uncertain for inclusion were listed (Additional File 1: Online Resource 2). The full-text reports were independently examined by four authors (TP, AB, ADC, and NS). Data from included studies were recorded using a Microsoft Excel specific report form. TP and AB independently verified all extracted data for accuracy. All disagreements were resolved by referral to a third author (LP) if necessary. When data about the primary outcome were missing, we planned to contact the corresponding author of the original study with a triple e-mail reminder.
Risk of bias assessment
The risk of bias (ROB) of the included studies was independently assessed by three authors (TP, PP, and FZ) according to the revised Cochrane ROB tool for randomized trials (RoB 2) [15]. RoB2 examines 5 domains of bias: (1) randomization process; (2) deviations from intended interventions; (3) missing outcome data; (4) measurement of the outcome; and (5) selection of the reported results. The overall RoB judgment at domain and study level was attributed according to the criteria specified in the RoB 2 tool [15]. The risk of bias of individual studies was examined at the study level. All disagreements were resolved by discussion or referral to a third author (LP) if necessary.
Data synthesis and analysis
Meta-analyses were performed using a random-effects model to account for between-study heterogeneity [16]. The treatment effect for continuous outcomes was analyzed with the inverse variance method and expressed as mean difference (MD) or standardized mean difference (SMD) with 95% confidence interval (CI), as appropriate. The treatment effect for dichotomous outcomes was analyzed with the Mantel–Haenszel method and expressed as risk ratio (RR) with 95% CI. The 95% prediction interval (PI) was reported alongside the 95% CI as an estimate of the dispersion of the true effect size across different study conditions. While CI indicates the effect size, PI represents the interval the mean effect of a new study will fall in when included.
Statistical heterogeneity for the outcomes among studies was assessed using the I2 test. We considered I2 ≥ 75% and p < 0.1 as high heterogeneity [16]. Publication bias was assessed by visually inspecting a funnel plot for potential asymmetry and Egger’s test was applied when the number of studies was adequate (n > 10). For the primary outcome and main secondary outcomes, we assessed the certainty of evidence using the grades of recommendation, assessment, development, and evaluation (GRADE) approach [17]. Where necessary, we converted the reported median and interquartile range to estimated mean and standard deviation using a standard approach [18].
We conducted several pre-specified sensitivity analyses to assess the impact of (1) different timing of measurement of the variables; (2) use of odds ratio versus RR as effect estimate in dichotomous variables; (3) exclusion of the studies at high risk of bias. Furthermore, the following pre-planned subgroup analyses were carried out: (1) medical versus surgical patients, which may represent different patient populations with different outcomes; (2) zero end-expiratory pressure (ZEEP) versus PEEP as lower PEEP, which may differently affect the outcome; (3) tidal volumes (TVs) greater versus lower than 8 mL/kg, which is the threshold for protective TVs that is commonly considered in non-ARDS patients [19]; (4) studies published after 2000 versus before 2000, when the landmark ARDSnet trial demonstrating a survival benefit associated with TV reduction in ARDS patients was published [20].
To investigate the influence of TVs on the effect size for the primary outcome and main secondary outcomes, we performed a post hoc meta-regression. Finally, we conducted a trial sequential analysis (TSA) considering a type I error of 5%, a power of 90%, and a hospital mortality proportion in the lower PEEP arm of 33% (median event proportion in this group among the included studies). The two-sided α-spending boundaries and futility area were computed with the O’Brien-Fleming function. An 11% relative risk reduction was calculated based on the lower limit of the 95% CI for the RR of the primary outcome in the meta-analysis, and the required information size was calculated accordingly.
All analyses were performed with Review Manager (version 5.3, Nordic Cochrane Centre, Cochrane Collaboration), R 4.0.3 with Rcmdr plugin (R Foundation for Statistical Computing, Vienna, Austria; https://www.R-project.org), and the Trial Sequential Analysis software (version 0.9.5.10, Copenhagen Trial Unit, Centre for Clinical Intervention Research, Copenhagen). For all analyses, two-sided p values < 0.05 were considered significant.
Reporting of this systematic review and meta-analysis conformed to preferred reporting items for systematic reviews and meta-analyses (PRISMA) standards (Additional File 1: Online Resource 3). This systematic review was registered in PROSPERO, an international prospective register of systematic reviews (www.crd.york.ac.uk/PROSPERO, CRD42021237164).
Results
We identified 8611 unique citations and assessed the full text of 50 articles for eligibility. Of these, 22 RCTs (2225 patients) [13, 21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41] comparing higher PEEP (1007 patients) with lower PEEP (991 patients) were included in the systematic review (Fig. 1). One study [40] did not report the number of randomized patients and the intermediate PEEP groups of four studies [23, 24, 31, 32] were excluded, hence the mismatch between the total number of included patients and the sum of the patients in the two groups. Data on the primary outcome were complete in the published reports of the studies.
The characteristics of the included RCTs are reported in Additional File 1: Online Resource 4. The studies were published between 1975 and 2020. Patient populations ranged from 15 to 969 patients. Ten studies (45%) enrolled post-cardiac surgery patients, six studies (27%) included patients with acute respiratory failure, four studies (18%) recruited patients with brain injury, and two studies (9%) non-hypoxemic patients. Higher PEEP ranged from 5 to 30 cmH2O (median 9 cmH2O, interquartile range [IQR] 8–10 cmH2O), whereas lower PEEP varied between ZEEP and 10 cmH2O (median 0 cmH2O, IQR 0–5 cmH2O). ZEEP was employed as lower PEEP in 13 studies (59%). PEEP was titrated arbitrarily in 17 studies (77%). TVs ranged between 6 and 15 mL/kg (median 8 mL/kg, IQR 7–11 mL/kg).
The overall risk of bias was judged to be high or moderate because of concerns related to the randomization process and the measurement of the outcome (Additional File 1: Online Resource 5).
The primary outcome was reported in 9 studies. Two hundred seventy-four patients out of 760 patients (36%) assigned to the higher PEEP group and 259 out of 742 patients (35%) assigned to the lower PEEP group died in the hospital (RR 1.02, 95% CI 0.89–1.16, p = 0.77; I2 = 0%, p = 0.62) (Fig. 2). The difference was not statistically significant. As shown in Additional File 1: Online Resource 6, higher PEEP was associated with improved arterial partial pressure of oxygen to fraction of inspired oxygen ratio (PaO2/FiO2), alveolar-arterial oxygen pressure difference (A-aDO2), and respiratory system compliance. Furthermore, we observed lower risk of hypoxemia and ARDS occurrence in the higher PEEP group. The risk of atelectasis, barotrauma, ventilator-associated pneumonia, and hypotension was similar in the 2 groups. Cardiac index, postoperative bleeding, and packed red blood cell transfusion were also no different, whereas central venous pressure was significantly higher in the higher PEEP group. Duration of ventilation, ICU and hospital length of stay, and ICU and 28-day mortality were similar between groups (Additional File 1: Online Resource 6).
Forest plots of primary outcome and main secondary outcomes. PEEP positive end-expiratory pressure, M–H Mantel–Haenszel, CI confidence interval, PaO2/FiO2 arterial partial pressure of oxygen to fraction of inspired oxygen ratio, SD standard deviation, IV inverse variance, ARDS acute respiratory distress syndrome
The presence of publication bias was strongly suspected from the visual inspection of the funnel plot for the duration of ventilation outcome (Additional File 1: Online Resource 7). Egger’s test was not applied because of the insufficient number of included studies. According to the GRADE approach, the certainty of evidence for hospital mortality was low (Table 1). We rated down the quality of evidence because of concerns related to the risk of bias.
The forest plots for sensitivity and subgroup analyses for hospital mortality are depicted in Fig. 3. None of the sensitivity or subgroup analyses for the primary and secondary outcomes significantly affected our results (Additional File 1: Online Resource 8, 9). We observed a significantly lower incidence of hypoxemia with higher PEEP in studies comparing higher PEEP with ZEEP versus studies comparing higher PEEP with lower PEEP (3 studies with ZEEP, 2 studies with PEEP; test for subgroup differences p = 0.02) (Additional File 1: Online Resource 9). A post hoc meta-regression revealed a significant negative association between TVs and the risk of hypoxemia (coefficient − 0.41, 95% CI − 0.77 to − 0.06, p = 0.02) (Additional File 1: Online Resource 10). The trial sequential analysis showed that the required information size of 6845 patients was not reached and the cumulative Z-score did not cross the monitoring boundaries (Additional File 1: Online Resource 11).
Forest plots of sensitivity and subgroup analyses for hospital mortality. Sensitivity analyses to assess the impact of the use of odds ratio versus risk ratio as effect estimate (top left) and the exclusion of the studies at high risk of bias (middle left) are reported. Subgroup analyses comparing medical versus surgical patients (bottom left), zero end-expiratory pressure versus positive end-expiratory pressure (PEEP) as lower PEEP (top right), tidal volumes greater versus lower than 8 mL/kg (middle right), and publication year after 2000 versus before 2000 (bottom right) are depicted. PEEP positive end-expiratory pressure, M–H Mantel–Haenszel, CI confidence interval, ZEEP zero end-expiratory pressure, TV tidal volume
Discussion
Our systematic review identified 22 RCTs, overall including 2225 patients, that evaluated the association of higher PEEP, compared to lower PEEP, with hospital mortality in unselected adult ICU patients intubated and mechanically ventilated for reasons other than ARDS. We concluded that hospital mortality was similar between the two groups with low certainty of evidence.
With respect to the secondary outcomes, higher PEEP was associated with higher PaO2/FiO2 ratio and lower A-aDO2, higher respiratory system compliance, and lower risk of hypoxemia and ARDS occurrence. Other secondary outcomes (e.g., occurrence of atelectasis, barotrauma, ventilation-associated pneumonia, hypotension, duration of ventilation, ICU and hospital stay, and ICU mortality) were similar between the two groups. The overall certainty of evidence was judged to be low or moderate for most secondary outcomes.
The role of PEEP during MV in patients with ARDS has been a matter of intense research. Based primarily on the results of an individual patient data meta-analysis reporting lower hospital mortality with higher PEEP among patients with moderate-severe ARDS [8], higher PEEP was suggested with a conditional recommendation in the most recent guidelines on MV in patients with ARDS [42].
The net benefit or harm of PEEP may depend on lung recruitability, i.e., the reaeration of non-aerated and/or poorly aerated lung tissue [5]. Nevertheless, the importance of lung recruitability and patient’s response to recruitment maneuvers are currently not fully understood. Patients without ARDS, like those with ARDS, may exhibit low lung recruitability and develop end-inspiratory alveolar overdistention, increased intrapulmonary shunt and dead space, and higher right ventricular afterload with higher PEEP [12]. These patients may benefit from a MV strategy including lower TVs, which were associated with improved clinical outcomes [43,44,45]. However, the effect of PEEP in patients without ARDS is still not well understood. To our knowledge, this is the second systematic review and meta-analysis to compare different levels of PEEP in ICU patients without ARDS. Similar to our findings, a previous work concluded that ventilation with higher PEEP is not associated with lower hospital mortality or shorter duration of ventilation, but with higher PaO2/FiO2 and lower occurrence of ARDS and hypoxemia [14]. We believe our work has some strengths compared to the previously published meta-analysis. Three studies were not confirmed for inclusion in our work because of noninvasive application of PEEP [46], crossover design [47], and differential utilization of recruitment maneuvers in the two groups [48]. On the other hand, five additional studies were selected [13, 25, 27, 29, 30]. Among these, the recent RELAx trial found that the use of lower PEEP was non-inferior to higher PEEP in terms of 28-day ventilator-free days [13]. Additionally, no difference between the groups in the occurrence of pulmonary complications, lengths of stay, and mortality was reported [13]. This trial is by far the largest RCT on this topic, accounting for more than 40% of patients included in our systematic review.
Despite the higher number of included patients and stricter selection criteria than the previous meta-analysis [14], we did not identify any association of higher PEEP with clinical outcomes, except for ARDS occurrence, but confirmed its association with physiological outcomes such as oxygenation. Several reasons may account for this.
First, PEEP may not be the most important target for preventing VILI in patients without ARDS. Driving pressure (DP), i.e., the difference between plateau pressure and total PEEP [49], and mechanical power (MP), i.e., the total inflation energy transferred from the mechanical ventilator to the lungs [50], have been recently proposed as reliable mediators of the injurious effects of MV in patients with ARDS [51,52,53,54]. Notably, patients without ARDS may benefit from lower DP [55,56,57] and MP [58], although the evidence is still controversial [59, 60]. Moreover, TVs may be a better surrogate of the risk of VILI in these patients with near-normal respiratory system compliance [61]. Therefore, titrating MV settings on DP and MP rather than PEEP or monitoring DP and MP during PEEP titration may be more effective in minimizing the risk of VILI in non-ARDS patients.
Second, the low certainty of evidence for hospital mortality, related to the high risk of bias of the studies contributing to this outcome, limits the strength of our conclusions. Rigorous RCTs with more selected patient populations would contribute to clarifying whether patients without ARDS may benefit from higher PEEP. Moreover, despite the overall low-moderate statistical heterogeneity, clinical heterogeneity among patient populations and outcome definitions (e.g., ARDS, barotrauma, pneumonia) was relevant in the studies included in our meta-analysis. This may have confounded the association between the level of PEEP and clinical outcomes.
Third, the existence of specific subgroups of patients without ARDS that may mostly benefit from higher PEEP might be hypothesized. However, although we performed several sensitivity and subgroup analyses, including a meta-regression, we could not identify any of such subgroups. Worth mentioning, the choice of PEEP in most studies was made arbitrarily and not individualized according to patients’ response to PEEP or to lung recruitability. Although the improved oxygenation with higher PEEP could depend on alveolar recruitment and reduced intrapulmonary shunt, which may protect against VILI, the use of excessive PEEP could lead to alveolar overdistension, cardiac dysfunction, and reduced oxygen delivery in patients with low lung recruitability regardless of arterial oxygenation [62]. Indeed, a strategy based on titration of the ventilator settings, i.e., tidal volume, PEEP, and recruitment maneuvers, on lung morphology, i.e., focal or non-focal injury distribution, may reduce mortality in ARDS patients [63]. Oxygenation may not be the best physiologic endpoint as regards the effect of PEEP. In fact, respiratory system compliance or DP may be better indices of the balance between recruitment and overdistension associated with variations of PEEP. Unfortunately, no studies provided data on DP and only 3 studies (189 patients) included compliance among the outcomes, thus limiting our confidence in our results. Furthermore, occurrence of hypotension and barotrauma, and measurements of cardiac index and dead space were only reported in a minority of studies. The trial sequential analysis showed that, although further studies are needed, these are unlikely to show any association of PEEP with mortality; this may suggest that patient selection criteria need to be modified in future studies, for example, taking lung recruitability into account.
Finally, physiological benefits may be most likely to translate into clinical advantages when baseline physiological derangements are severe enough. However, baseline oxygenation and compliance, when reported, were near-normal for most patients [13, 24, 28,29,30,31,32, 34, 37,38,39].
Our study has several limitations. First, we restricted our research to 6 databases and decided not to include conference proceedings. Therefore, we cannot exclude that other studies could have been identified by exploring other databases and that publication bias may have ensued from our search strategy. In addition, we did not perform an individual patient data meta-analysis, thus potentially missing patient subgroups benefiting from higher or lower PEEP. However, we used a reproducible and comprehensive literature search strategy, including clinical trials and grey literature, and we employed clearly defined inclusion criteria and duplicate independent citation review, data extraction, and quality assessment. Second, as the included studies were published over a 45-year period, the heterogeneous clinical protocols and outcome definitions may limit the reliability of our findings. Importantly, very different levels of PEEP and TV were applied in the studies. However, we excluded studies changing MV settings other than PEEP to avoid potential confounding factors. Additionally, our subgroup analyses on the use of ZEEP versus PEEP, TV greater versus lower than 8 mL/kg, and publication year after versus before 2000 did not identify any clinically significant variation in the intervention effect. Finally, statistical heterogeneity was relevant for some secondary outcomes. Notwithstanding, we performed several subgroup analyses and a post hoc meta-regression, which partially explained the reported heterogeneity.
Conclusions
In our meta-analysis of RCTs including a recent well-powered high-quality RCT, higher PEEP, compared with lower PEEP, was not associated with mortality in patients without ARDS receiving invasive MV. Further large high-quality RCTs are required to confirm these findings.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- MV:
-
Mechanical ventilation
- VILI:
-
Ventilator-induced lung injury
- PEEP:
-
Positive end-expiratory pressure
- ARDS:
-
Acute respiratory distress syndrome
- RELAx:
-
Restricted versus liberal positive end-expiratory pressure in patients without ARDS
- ICU:
-
Intensive care unit
- RCT:
-
Randomized controlled trial
- PICOS:
-
Participants, interventions, comparisons, outcomes, and study design
- ROB:
-
Risk of bias
- MD:
-
Mean difference
- SMD:
-
Standardized mean difference
- CI:
-
Confidence interval
- RR:
-
Risk ratio
- PI:
-
Prediction interval
- GRADE:
-
Grades of recommendation, assessment, development, and evaluation
- ZEEP:
-
Zero end-expiratory pressure
- TV:
-
Tidal volume
- TSA:
-
Trial sequential analysis
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- PaO2/FiO2 :
-
Arterial partial pressure of oxygen to fraction of inspired oxygen ratio
- A-aDO2 :
-
Alveolar-arterial oxygen pressure difference
- DP:
-
Driving pressure
- MP:
-
Mechanical power
References
Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med. 2013;369:2126–36.
Katira BH. Ventilator-induced lung injury: classic and novel concepts. Respir Care. 2019;64:629–37.
Cipulli F, Vasques F, Duscio E, Romitti F, Quintel M, Gattinoni L. Atelectrauma or volutrauma: the dilemma. J Thorac Dis. 2018;10:1258–64.
Chiumello D, Carlesso E, Cadringher P, Caironi P, Valenza F, Polli F, et al. Lung stress and strain during mechanical ventilation for acute respiratory distress syndrome. Am J Respir Crit Care Med. 2008;178:346–55.
Sahetya SK, Goligher EC, Brower RG. Fifty years of research in ARDS. Setting positive end-expiratory pressure in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195:1429–38.
Cortes-Puentes GA, Oeckler RA, Marini JJ. Physiology-guided management of hemodynamics in acute respiratory distress syndrome. Ann Transl Med. 2018;6:353.
Gattinoni L, Marini JJ, Pesenti A, Quintel M, Mancebo J, Brochard L. The «baby lung» became an adult. Intensive Care Med. 2016;42:663–73.
Briel M, Meade M, Mercat A, Brower RG, Talmor D, Walter SD, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA. 2010;303:865.
Gattinoni L, Caironi P, Cressoni M, Chiumello D, Ranieri VM, Quintel M, et al. Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med. 2006;354:1775–86.
Caironi P, Cressoni M, Chiumello D, Ranieri M, Quintel M, Russo SG, et al. Lung opening and closing during ventilation of acute respiratory distress syndrome. Am J Respir Crit Care Med. 2010;181:578–86.
Goligher EC, Kavanagh BP, Rubenfeld GD, Adhikari NKJ, Pinto R, Fan E, et al. Oxygenation response to positive end-expiratory pressure predicts mortality in acute respiratory distress syndrome. A secondary analysis of the LOVS and ExPress trials. Am J Respir Crit Care Med. 2014;190:70–6.
Luecke T, Pelosi P. Clinical review: positive end-expiratory pressure and cardiac output. Crit Care. 2005;9:607.
Writing Committee and Steering Committee for the RELAx Collaborative Group, Algera AG, Pisani L, Serpa Neto A, den Boer SS, Bosch FFH, et al. Effect of a lower vs higher positive end-expiratory pressure strategy on ventilator-free days in ICU patients without ARDS: a randomized clinical trial. JAMA. 2020;324:2509.
The PROVE Network Investigators, Serpa Neto A, Filho RR, Cherpanath T, Determann R, Dongelmans DA, et al. Associations between positive end-expiratory pressure and outcome of patients without ARDS at onset of ventilation: a systematic review and meta-analysis of randomized controlled trials. Ann Intensive Care. 2016;6:109.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Deeks JJ, Higgins JPT, Altman DG, editors. Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JPT, Thomas J, Chandler J, et al, editors. Cochrane handbook for systematic reviews of interventions version 6.1 (updated September 2020). Cochrane. 2020. https://training.cochrane.org/.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135.
Ferguson ND. Low tidal volumes for all? JAMA. 2012;308:1689.
Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301–8.
Good JT, Woh JF, Anderson JT, Dreisin RB, Petty TL. The routine use of positive end-expiratory pressure after open heart surgery. Chest. 1979;76:397–400.
Zurick AM, Urzua J, Ghattas M, Cosgrove DM, Estafanous FG, Greenstreet R. failure of positive end-expiratory pressure to decrease postoperative bleeding after cardiac surgery. Ann Thorac Surg. 1982;34:608–11.
Marvel SL, Elliott CG, Tocino I, Greenway LW, Metcalf SM, Chapman RH. Positive end-expiratory pressure following coronary artery bypass grafting. Chest. 1986;90:537–41.
Michalopoulos A, Anthi A, Rellos K, Geroulanos S. Effects of positive end-expiratory pressure (PEEP) in cardiac surgery patients. Respir Med. 1998;92:858–62.
Collier B, Kolff J, Devineni R, Gonzalez LS. Prophylactic positive end-expiratory pressure and reduction of postoperative blood loss in open-heart surgery. Ann Thorac Surg. 2002;74:1191–4.
Dyhr T, Laursen N, Larsson A. Effects of lung recruitment maneuver and positive end-expiratory pressure on lung volume, respiratory mechanics and alveolar gas mixing in patients ventilated after cardiac surgery. Acta Anaesthesiol Scand. 2002;46:717–25.
Koutsoukou A, Perraki H, Raftopoulou A, Koulouris N, Sotiropoulou C, Kotanidou A, et al. Respiratory mechanics in brain-damaged patients. Intensive Care Med. 2006;32:1947–54.
Holland A, Thuemer O, Schelenz C, van Hout N, Sakka SG. Positive end-expiratory pressure does not affect indocyanine green plasma disappearance rate or gastric mucosal perfusion after cardiac surgery. Eur J Anaesthesiol. 2007;24:141–7.
Korovesi I, Papadomichelakis E, Orfanos SE, Giamarellos-Bourboulis EJ, Livaditi O, Pelekanou A, et al. Exhaled breath condensate in mechanically ventilated brain-injured patients with no lung injury or sepsis. Anesthesiology. 2011;114:1118–29.
Korovesi I, Kotanidou A, Papadomichelakis E, Livaditi O, Sotiropoulou C, Koutsoukou A, et al. Exhaled nitric oxide and carbon monoxide in mechanically ventilated brain-injured patients. J Breath Res. 2016;10:017107.
Borges DL, Nina VJS, Costa MAG, Baldez TEP, dos Santos NP, Lima IM, et al. Effects of different PEEP levels on respiratory mechanics and oxygenation after coronary artery bypass grafting. Rev Bras Cir Cardiovasc. 2013;28:380–5.
Lago Borges D, José da Silva Nina V, Pereira Baldez TE, de Albuquerque Gonçalves Costa M, Pereira dos Santos N, Mendes Lima I, et al. Effects of positive end-expiratory pressure on mechanical ventilation duration after coronary artery bypass grafting: a randomized clinical trial. Ann Thorac Cardiovasc Surg. 2014;20:773–7.
Feeley TW, Saumarez R, Klick JM, Saumarez R, Mcnabb TG, Skillman JJ. Positive end-expiratory pressure in weaning patients from controlled ventilation. A prospective randomised trial. Lancet. 1975;306:725–9.
Weigelt JA. Early positive end-expiratory pressure in the adult respiratory distress syndrome. Arch Surg. 1979;114:497.
Pepe PE, Hudson LD, Carrico CJ. Early application of positive end-expiratory pressure in patients at risk for the adult respiratory-distress syndrome. N Engl J Med. 1984;311:281–6.
Nelson LD, Civetta JM, Hudson-Civetta J. Titrating positive end-expiratory pressure therapy in patients with early, moderate arterial hypoxemia. Crit Care Med. 1987;15:14–9.
Manzano F, Fernández-Mondéjar E, Colmenero M, Poyatos ME, Rivera R, Machado J, et al. Positive-end expiratory pressure reduces incidence of ventilator-associated pneumonia in nonhypoxemic patients. Crit Care Med. 2008;36:2225–31.
Lesur O, Remillard M-A, St-Pierre C, Falardeau S. Prophylactic positive end-expiratory pressure and postintubation hemodynamics: an interventional, randomized study. Can Respir J. 2010;17:e45-50.
Ma C, Liang D, Zheng F. Effect of high positive end-expiratory pressure for mechanical ventilation in the treatment of neurological pulmonary edema. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2014;26:339–42.
Murphy DA, Finlayson DC, Craver JM, Jones EL, Kopel M, Tobia V, et al. Effect of positive end-expiratory pressure on excessive mediastinal bleeding after cardiac operations. A controlled study. J Thorac Cardiovasc Surg. 1983;85:864–9.
Vigil AR, Clevenger FW. The effects of positive end-expiratory pressure on intrapulmonary shunt and ventilatory dead space in nonhypoxic trauma patients. J Trauma. 1996;40:618–23.
Fan E, Del Sorbo L, Goligher EC, Hodgson CL, Munshi L, Walkey AJ, et al. An official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine clinical practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195:1253–63.
Futier E, Constantin J-M, Paugam-Burtz C, Pascal J, Eurin M, Neuschwander A, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369:428–37.
Serpa Neto A, Simonis FD, Barbas CSV, Biehl M, Determann RM, Elmer J, et al. Association between tidal volume size, duration of ventilation, and sedation needs in patients without acute respiratory distress syndrome: an individual patient data meta-analysis. Intensive Care Med. 2014;40:950–7.
Neto AS, Simonis FD, Barbas CSV, Biehl M, Determann RM, Elmer J, et al. Lung-protective ventilation with low tidal volumes and the occurrence of pulmonary complications in patients without acute respiratory distress syndrome: a systematic review and individual patient data analysis. Crit Care Med. 2015;43:2155–63.
Carroll GC, Tuman KJ, Braverman B, Logos WG, Wool N, Goldin M, et al. Minimal positive end-expiratory pressure (PEEP) may be “best PEEP.” Chest. 1988;93:1020–5.
Cujec B. Positive End-Expiratory pressure increases the right-to-left shunt in mechanically ventilated patients with patent foramen ovale. Ann Intern Med. 1993;119:887.
Celebi S, Koner O, Menda F, Korkut K, Suzer K, Cakar N. The pulmonary and hemodynamic effects of two different recruitment maneuvers after cardiac surgery. Anesth Analg. 2007;104:384–90.
Amato MBP, Barbas CSV, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi-Filho G, et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998;338:347–54.
Cressoni M, Gotti M, Chiurazzi C, Massari D, Algieri I, Amini M, et al. Mechanical power and development of ventilator-induced lung injury. Anesthesiology. 2016;124:1100–8.
Amato MBP, Meade MO, Slutsky AS, Brochard L, Costa ELV, Schoenfeld DA, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372:747–55.
The LUNG SAFE Investigators and the ESICM Trials Group, Laffey JG, Bellani G, Pham T, Fan E, Madotto F, et al. Potentially modifiable factors contributing to outcome from acute respiratory distress syndrome: the LUNG SAFE study. Intensive Care Med. 2016;42:1865–76.
Zhang Z, Zheng B, Liu N, Ge H, Hong Y. Mechanical power normalized to predicted body weight as a predictor of mortality in patients with acute respiratory distress syndrome. Intensive Care Med. 2019;45:856–64.
Tonna JE, Peltan I, Brown SM, Herrick JS, Keenan HT. Mechanical power and driving pressure as predictors of mortality among patients with ARDS. Intensive Care Med. 2020;46:1941–3.
Park M, Ahn HJ, Kim JA, Yang M, Heo BY, Choi JW, et al. Driving pressure during thoracic surgery. Anesthesiology. 2019;130:385–93.
Neto AS, Hemmes SNT, Barbas CSV, Beiderlinden M, Fernandez-Bustamante A, Futier E, et al. Association between driving pressure and development of postoperative pulmonary complications in patients undergoing mechanical ventilation for general anaesthesia: a meta-analysis of individual patient data. Lancet Respir Med. 2016;4:272–80.
Neto AS, Barbas CSV, Simonis FD, Artigas-Raventós A, Canet J, Determann RM, et al. Epidemiological characteristics, practice of ventilation, and clinical outcome in patients at risk of acute respiratory distress syndrome in intensive care units from 16 countries (PRoVENT): an international, multicentre, prospective study. Lancet Respir Med. 2016;4:882–93.
For the PROVE Network Investigators, Serpa Neto A, Deliberato RO, Johnson AEW, Bos LD, Amorim P, Pereira SM, et al. Mechanical power of ventilation is associated with mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med. 2018;44:1914–22.
Schmidt MFS, Amaral ACKB, Fan E, Rubenfeld GD. Driving pressure and hospital mortality in patients without ARDS. Chest. 2018;153:46–54.
Lanspa MJ, Peltan ID, Jacobs JR, Sorensen JS, Carpenter L, Ferraro JP, et al. Driving pressure is not associated with mortality in mechanically ventilated patients without ARDS. Crit Care. 2019;23:424.
Serpa Neto A, Hemmes SNT, Barbas CSV, Beiderlinden M, Biehl M, Binnekade JM, et al. Protective versus conventional ventilation for surgery. Anesthesiology. 2015;123:66–78.
Suter PM, Fairley HB, Isenberg MD. Optimum end-expiratory airway pressure in patients with acute pulmonary failure. N Engl J Med. 1975;292:284–9.
Constantin J-M, Jabaudon M, Lefrant J-Y, Jaber S, Quenot J-P, Langeron O, et al. Personalised mechanical ventilation tailored to lung morphology versus low positive end-expiratory pressure for patients with acute respiratory distress syndrome in France (the LIVE study): a multicentre, single-blind, randomised controlled trial. Lancet Respir Med. 2019;7:870–80.
Acknowledgements
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
TP and PN contributed substantially to the conception and design of the study. TP, AB, ADC, and NS contributed substantially to the acquisition of data. TP, AB, ADC, FZ, PP, LP, and GL contributed substantially to the analysis and interpretation of the data. TP drafted the article. All authors provided critical revision of the article and final approval of the version submitted for publication and have agreed both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
PN received royalties from Intersurgical for Helmet Next invention and speaking fees from Philips, Resmed, MSD, and Novartis outside the submitted work. All other authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional File 1: Online Resource 1.
Methods. Online Resource 2. Included studies and major exclusions. Online Resource 3. Preferred reporting items for systematic reviews and meta-analyses checklist. Online Resource 4. Characteristics of included studies. Online Resource 5. Risk of bias assessment. Online Resource 6. Primary and secondary outcomes. Online Resource 7. Funnel plots. Online Resource 8. Sensitivity analyses. Online Resource 9. Subgroup analyses. Online Resource 10. Meta-regression. Online Resource 11. Trial sequential analysis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pettenuzzo, T., Boscolo, A., De Cassai, A. et al. Higher versus lower positive end-expiratory pressure in patients without acute respiratory distress syndrome: a meta-analysis of randomized controlled trials. Crit Care 25, 247 (2021). https://doi.org/10.1186/s13054-021-03669-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-021-03669-4