Abstract
Over 16 million children have been detected positive for the coronavirus disease 2019 (COVID-19) in the United States since the outbreak of the pandemic. In general, children infected with severe acute respiratory syndrome coronavirus type 2 tend to have lighter symptoms than adults. However, in some cases, the infection can develop into severe forms, such as multisystem inflammatory syndrome in children. Moreover, long-term public health preventive interventions have had some negative effects on the physical and mental health of children. Given the important role that vaccination plays in reducing severe illness and mortality, it is essential for the efficient implementation of vaccination in the pediatric population. Nevertheless, parental distrust of vaccination, especially with regard to its safety and efficacy, hinders this process. Herein, we comprehensively summarize the available data on the safety and effectiveness of COVID-19 vaccine in children. The results show that the currently approved COVID-19 vaccine is safe and effective for children. Although two doses of vaccine in children seem insufficient to prevent Omicron infection, the booster dose provides enhanced protection against infection and severe illness. Most importantly, the bivalent vaccine has been approved for use in the pediatric population to extend the immune response to currently circulating Omicron variant. And the immune protection afforded to newborns after maternal vaccination appears to last only 6 months. Therefore, in the current situation where the rate of virus mutation is accelerating and the COVID-19 pandemic is still severe, it is crucial to extend vaccine protection to children over 6 months of age to weave a tighter safety net.
Similar content being viewed by others
Introduction
The coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, remains a major global healthy, social, and economic burden. It is characterized by the presence of respiratory disease with flu-like symptoms such as dry cough, body aches, and fever. In more severe cases, the disease can rapidly progress to pneumonia, acute respiratory syndrome, and even death [1]. As of June 7, 2023, there were more than 767 million confirmed cases worldwide, including more than 6.9 million deaths, and this number is rising sharply every day [2]. Moreover, SARS-CoV-2 causes acute respiratory infections of varying degrees of severity in different age groups. Older individuals (> 60 years) tend to have severe diseases and have the highest risk of death [3]. In contrast, most of the children with SARS-CoV-2 infection have a milder disease with common symptoms including fever, pharyngitis, cough, and diarrhea [4]. Still, in rare cases, children may also develop more serious consequences.
According to the latest data released by the Centers for Disease Control and Prevention, 17.2% of the nearly 100 million known cases of COVID-19 infection in the United States were in children [5]. Of the 16.3 million pediatric cases, 179,338 required hospitalization and intensive care [6]. Similar to adults, children who are obese, diabetic, or have immunocompromising conditions can increase the risk of admission to intensive care [7]. Although it is very rare, some previously healthy children may also experience severe diseases after the initial infection, such as multisystem inflammatory syndrome in children (MIS-C) [8]. Furthermore, considering the high proportion of children in COVID-19 cases, they may play an important role in the transmission of SARS-CoV-2, especially the highly transmissible Omicron variant [9, 10].
Although stringent public health interventions have been implemented to contain further transmission of SARS-CoV-2, including wearing facemasks, social distancing, and limiting social contact, the COVID-19 epidemic has not yet been fully controlled. Moreover, the above measures have created problems of educational disruption and social isolation, which may adversely affect the social and emotional development and mental health of children [11, 12]. It is also impossible for the public to comply with conservation measures for many years. Thus, there is a significant need to protect children through vaccination. In addition to the benefits to individuals, vaccination of children against COVID-19 can have beneficial knock-on effects in the community, thereby contributing to herd immunity in all age groups. But current data show that only 5.7% of children under four years old in Canada have received at least one dose of the vaccine [13]. Similarly, low vaccination rates were observed among children aged 2–4 and 5–11 years in the United States, with only 10.9% and 40.0% respectively [14]. Therefore, it is essential to summarize the available evidence and information to promote vaccination rates for children and to help achieve substantial control of community transmission in the future.
Methods and materials
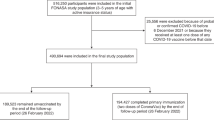
We reviewed the articles published on Google Scholar, PubMed, and Web of Science using the following terms: COVID-19, children, vaccination, Omicron, vaccine effectiveness, and bivalent vaccine. After an additional manual search and an extension of the search to the reference lists of all retrieved articles, 70 papers were finally included in our review. The types of studies included were prospective, retrospective, cross-sectional and case–control studies and one review. In addition, information from 14 official public health websites was also used.
Factors affecting vaccine uptake in children
It is well known that widespread COVID-19 vaccination is the most effective and cost-effective method to interrupt SARS-CoV-2 transmission. However, the lower COVID-19 vaccination rates among children seem not to achieve substantial control of community transmission, which may prolong the outbreaks and epidemics of disease. For underage children, parents are usually the primary decision-makers on their children’s vaccination. Hence, we searched three databases to find the relevant literatures published since 2022 on the determinants of parents’ unwillingness to vaccinate their children with COVID-19 vaccine and made Table 1 [15,16,17,18,19,20,21,22,23,24,25,26].
Based on the result, parental decisions about whether to vaccinate their children are complex and multidimensional, including individual/group determinants, contextual determinants, and vaccine determinants (Table 1). In terms of the individual determinants, some parents still believe that the prevalence of COVID-19 infection in children is minimal and they are unlikely to progress to serious diseases after infection. However, as mentioned above, current data suggest otherwise. Moreover, studies have demonstrated that children whose parents have received or are willing to receive COVID-19 vaccine are more likely to receive the vaccine. It is worth mentioning that a study found that parental acceptance of the COVID-19 vaccination for children was closely related to the acceptance of previous influenza vaccination. Specifically, parents who refused to have their children vaccinated against influenza were more than five times as likely to refuse to have their children vaccinated against COVID-19 than other parents [27].
The most common factors that influence vaccine acceptance at the contextual level are gender, race, and educational level. According to Table 1, fathers are more likely to vaccinate their children than mothers in general. Considering that females tend to experience more adverse events after receiving COVID-19 vaccine, they may be more concerned about the potential side effects of COVID-19 vaccine on their children [28]. However, this result differs from a previous study in Poland by Babicki et al. (2021) in which they found that fathers were less likely than mothers to believe that vaccines can protect the health of children [29]. This may be due to differences in the social roles of fathers or mothers between communities. With respect to ethnicity, Blacks and Hispanics have shown an increased distrust of COVID-19 vaccination given the potential for discrimination, racism, and abuse within the healthcare system. Moreover, the effect of parental education level on vaccine hesitancy is a controversial issue. On the one hand, the higher the level of parental education, the more confidence they have in vaccination. On the other hand, highly educated parents may expect more information about vaccines before deciding to vaccinate their children, thereby leading to vaccine hesitancy. Notably, conflicting media messages, especially a lot of misinformation and anti-vaccine propaganda, may have a negative impact on the willingness to vaccinate during the pandemic.
Additionally, the younger age of children was also one of the reasons why parents refuse to vaccinate them. One cross-sectional study conducted in the United States showed that only 40% of parents were willing to vaccinate their children aged between 6 months and 4 years against COVID-19 [30]. A similar level of COVID-19 vaccination acceptability was found among parents with children under 18 months in the United Kingdom [31]. Currently, the safety and efficacy of the vaccine have become the most important considerations for parents who are hesitant or reluctant to vaccinate their children due to the rapid development and the lack of adequate information on the COVID-19 vaccine. Thus, there is an urgent need to comprehensively summarize and discuss the relevant information on the safety and effectiveness of the COVID-19 vaccine for children in order to improve vaccine acceptance and coverage.
The safety and efficacy of COVID-19 vaccination among children
To date, the COVID-19 vaccine has shown favorable safety for children in most clinical studies [32, 33]. Although adverse events such as injection-site pain, fever, fatigue, and headache were reported after the vaccination in children, these symptoms were mild to moderate in severity and transient, resolving in a few days [34]. Moreover, there is no significant difference in the incidence of adverse reactions after vaccination in subjects aged 3–17 years and those aged 18–59 years or over 60 years or older [35, 36]. As a serious disease of cardiovascular system, myocarditis has been reported many times in pediatric patients with SARS-CoV-2 infection and has greatly increased the incidence rate and mortality of the SARS-CoV-2 in children [37, 38]. The appearance of myocarditis may be caused by an over-activation of the innate immune system and pro-inflammatory cytokine surge according to recent research [39]. Notably, the cases of myocarditis and pericarditis associated with the COVID-19 vaccine were also observed in the pediatric population, especially those following the mRNA vaccination. Moreover, this type of myocardial injury has typically presented in adolescent males and appears to be dose and interval dependent [40, 41]. Fortunately, these cases were of a mild and benign clinical course, and most patients recovered with only pain treatment. Although a few patients continued to have mild cardiac abnormalities during long-term follow-up, their incidence was significantly lower than after SARS-CoV-2 infection [42, 43].
As mentioned before, MIS-C is a hyper-inflammatory syndrome with multi-organ involvement caused by SARS-CoV-2 infection. There is evidence that children diagnosed with MIS-C have a robust and sustained immune response to SARS-CoV-2, including higher levels of spike protein and viral nucleocapsid protein antibodies [44]. Notably, if the COVID-19 vaccine can induce similar antibody responses in children as well, it may put otherwise healthy children at risk for serious outcomes following vaccination designed to prevent SARS-CoV-2 disease. Fortunately, hundreds of millions of children are vaccinated worldwide, but very few studies have reported vaccination as a potential trigger for the development of MIS-C in patients with no history of infection [45, 46]. Also, a national cohort study from France found a 94% reduction in the incidence of MIS-C among children aged 12–18 years after one dose of the BNT162b2 vaccine; no cases of MIS-C were reported among fully vaccinated children [47]. In line with this, Nygaard and colleagues (2022) found that the incidence of MIS-C was 11 per million vaccinated adolescents aged 5 to 17 years. In contrast, 183 cases of MIS-C were reported among one million SARS-CoV-2 infected individuals in the same age group [48]. The potential risk of vaccination on children’s health should be compared with the adverse consequences of COVID-19 rather than considered separately in view of the rapid and widespread spread of COVID-19.
Experiments on the effects of different COVID-19 vaccines have revealed that most COVID-19 vaccines were immunogenic and induced robust humoral responses in children [34, 49]. Moreover, there are non-inferior or even better immune responses in children and adolescents compared to that observed in adults. Concretely speaking, following two 3.0 µg doses of an inactivated SARS-CoV-2 vaccine (CoronaVac), the geometric mean titers (GMTs) of 142.2 in children 3–17 years old induced better immunogenicity than that elicited in adults aged 18–59 years (44.1) and those aged 60 years and older (42.2) with the same immunization schedule [32]. The neutralizing antibody response observed in aged 12–17 years after two doses of the mRNA vaccine was identical to that seen 18–24 years age group [50]. However, Xia et al. (2022) reported that seroconversion rate and neutralizing antibody titer in the 3–5 years age group are lower than those in adults aged 18–59 years on day 28 after one dose BBIBP vaccination [35]. Given those children aged 3–5 years may have less developed immune systems, this phenomenon was not surprising. It is universally acknowledged that the thymus gland of a young child is not fully developed. A thymic perivascular space constitutes the thymus, which contains granulocytes, mast cells, and other lymphoid cells and peaks in size between 10 and 25 years of age [51]. Additionally, young children have a reduced number and function of innate and adaptive immune cells and poorer production of immune media compared with adults [52]. It is worth mentioning that the serum conversion rates and neutralizing antibody titers in the age group of 3–5 years reached a level similar to that in the adult group after the second dose of the vaccine [35].
The intensity of the antibody response increased with increasing vaccine doses in all age groups of children (Table 2) [32,33,34,35, 49, 50, 53]. Specifically, from 3 to 17 years old, the neutralizing antibody titers induced by a 3.0 µg dose were higher than those of the 1.5 µg dose after the CoronaVac and the neutralizing antibody GMT of 2.0 µg BBIBP-CorV was significantly lower than that of the 4.0 and 8.0 µg [32, 35]. However, this does not mean that higher doses of vaccines should be offered to children, but rather that they should be considered in conjunction with potential adverse reactions caused by the vaccine. Moreover, the antibody titers induced by the same vaccine dose at different ages seem to be different (Table 2). In general, older children with more developed immune systems will produce higher neutralizing antibody titers. Nevertheless, the data in table two does not quite fit this pattern. In view of the small cumulative number of subjects, the outcome may have a certain partial bias. Hence, larger multicenter trials and sample analyses are required to produce convincing results.
It is well known that compared to the original SRAS-CoV-2 strain, the Omicron variant has multiple mutations in the spike protein, especially in the receptor binding domain and the N-terminal domain, leading to extensive immune escape [54]. Hence, some parents are concerned that the COVID-19 vaccine, which was designed based on wild-type viral strains, may not provide adequate immune protection for children (Table 1). Indeed, the vaccine effectiveness (VE) against symptomatic infection was significantly lower during the Omicron-dominant period than during the pre-Omicron period for adolescents aged 12 to 18 years after two doses of the BNT162b2 vaccine (Table 3) [55,56,57,58,59,60,61,62,63,64,65]. The vaccination program for the 5–11 years age group was only approved late in 2021, so all the VE studies for this age group were conducted during the Omicron period. A study from Italy reported that the VE against infection in this age group declined rapidly to 21.2% within 3 months after full vaccination [61]. Although the third monovalent dose increased protection against symptomatic infection, the VE of monovalent booster doses against COVID-19 associated hospitalization has also inevitably declined with the passage of time [66]. Notably, mRNA-1273.214 vaccine prepared from Wuhan-Hu-1 and Omicron BA.1 spike protein mRNAs induced a strong neutralizing antibody response to Omicron BA.4 and BA.5 subvariants in adults, which is thought to play a constructive role in defense against the evolving virus [67, 68]. So far, several studies have shown that the bivalent vaccine is safe and reliable in all age groups of children [69, 70]. Therefore, the Centers for Disease Control and Prevention and the American College of Obstetricians and Gynecologists recommend that children receive an age-appropriate dose of a bivalent mRNA booster ≥ 2 months after completion of a COVID-19 primary series or receiving a monovalent booster dose to expand the immune response against the currently prevalent Omicron variant and to improve the protective effect of the COVID-19 vaccine against severe disease [71, 72].
Recommendations for the age range of childhood vaccinations
Epidemiological evidence suggests that infants born to mothers who received two doses of the mRNA vaccine during pregnancy had a 61% lower risk of hospitalization for SARS-CoV-2 in the first 6 months of life [73]. However, the levels of anti-spike IgG declined steadily after 6 months of life, and protection against SARS-CoV-2 infection was significantly diminished [74]. A study conducted in Israel observed a higher risk of infection among infants aged 0–1 year than among older children [75]. This result is understandable because the immune system of infants is not fully developed and unable to produce sufficient immunoglobulins [76]. Moreover, high levels of the SARS-CoV-2 virus in asymptomatic children may allow transmission of infection to family members who are in close contact with them [77]. Thus, it is essential to vaccinate children over the age of 6 months. Studies have demonstrated that participants aged 6–23 months have a strong immune response after three doses. Their GMT was similar to that observed in the group of people aged 16–25 years received two doses of BNT162b2 vaccine [78]. Additionally, the majority of adverse events reported in these trials were mild to moderate in severity, with no serious vaccine-related adverse events reported [78]. Currently, several international organizations have suggested BNT162b2 and mRNA-1273 vaccines for children over 6 months of age (Table 4) [79,80,81,82,83,84].
Conclusion
Children, as a special population, need to consider many influencing factors when receiving the COVID-19 vaccine. Among these, the most important considerations are the safety and efficacy of the vaccine. While there are some common adverse reactions to vaccination in children, these events are mild and transient, and disappear within a few days. Compared to adults, there was no significant difference in the incidence of adverse effects after vaccination in children. Although cases of vaccine-associated myocarditis have been identified in the pediatric population, such sequelae are rare and affected patients experience rapid resolution of symptoms and recovery of cardiac function in a short period of time. Additionally, vaccination of children not only induces a strong immune response, but also provides protection against symptomatic diseases, especially in preventing hospitalization. Notably, the protection afforded to children after two doses of vaccine appears to be relatively limited due to extensive immune escape of the omicron variant. The protection provided by three doses of monovalent vaccine still decreases rapidly over time. Fortunately, bivalent vaccines have been approved for use in children and may provide broader and longer-lasting immune protection.
The level of SARS-CoV-2 antibody provided by the mother significantly decreased after 6 months of birth. Given the high risk of infection and the high transmissibility of children after infection, it is essential to vaccinate children over 6 months of age in a timely manner. Only in this way can establish a stronger immune barrier as early as possible to deal with the constant mutation of the virus.
Data Availability
Not applicable.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- GMTs:
-
Geometric mean titers
- MIS-C:
-
Multisystem inflammatory syndrome in children
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- VE:
-
Vaccine effectiveness
References
World Health Organization. Coronavirus disease (COVID-19). https://www.who.int/health-topics/coronavirus#tab=tab_3
World Health Organization. WHO Coronavirus (COVID-19) dashboard. https://covid19.who.int/
Wu Z, McGoogan JM. Characteristics of and important lessons from the Coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. Apr 2020;323(13):1239–1242. https://doi.org/10.1001/jama.2020.2648
Zhang H, Penninger JM, Li Y, Zhong N, Slutsky AS. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46(4):586–90.
Centers for Disease Control and Prevention. Demographic Trends of COVID-19 cases and deaths in the US reported to CDC. https://covid.cdc.gov/covid-data-tracker/#demographics
Centers for Disease Control and Prevention. COVID data tracker. https://covid.cdc.gov/covid-data-tracker/#new-hospital-admissions
DeBiasi RL, Song X, Delaney M, Bell M, Smith K, Pershad J et al. Severe coronavirus disease-2019 in children and young adults in the Washington, DC, metropolitan region, J Pediatr, vol. 223, pp. 199–203. e1, 2020.
Feldstein LR, Rose EB, Horwitz SM, Collins JP, Newhams MM, Son MBF, et al. Multisystem inflammatory syndrome in US children and adolescents. N Engl J Med. 2020;383(4):334–46.
Rumain B, Schneiderman M, Geliebter A. Prevalence of COVID-19 in adolescents and youth compared with older adults in states experiencing surges. PLoS ONE. 2021;16(3):e0242587. https://doi.org/10.1371/journal.pone.0242587
Szablewski CM, Chang KT, Brown MM, Chu VT, Yousaf AR, Anyalechi N, et al. SARS-CoV-2 transmission and infection among attendees of an overnight Camp - Georgia, June 2020. MMWR Morb Mortal Wkly Rep. Aug 2020;69(31):1023–5. https://doi.org/10.15585/mmwr.mm6931e1
Lopez-Bueno R, Lopez-Sanchez GF, Casajus JA, Calatayud J, Tully MA, Smith L. Potential health-related behaviors for pre-school and school-aged children during COVID-19 lockdown: a narrative review. Prev Med. Feb 2021;143:106349. https://doi.org/10.1016/j.ypmed.2020.106349
McKune SL, Acosta D, Diaz N, Brittain K, Beaulieu DJ, Maurelli AT, et al. Psychosocial health of school-aged children during the initial COVID-19 safer-at-home school mandates in Florida: a cross-sectional study. BMC Public Health. Mar 29 2021;21(1):603. https://doi.org/10.1186/s12889-021-10540-2
Public Health Agency of Canada. COVID-19 vaccination coverage. https://www.canada.ca/en/public-health/services/diseases/coronavirus-disease-covid-19.html
Centers for Disease Control and Prevention. Trends in demographic characteristics of people receiving COVID-19 vaccinations in the United States. https://covid.cdc.gov/covid-data-tracker/#vaccination-demographics-trends
Byrne A, Thompson LA, Filipp SL, Ryan K. COVID-19 vaccine perceptions and hesitancy amongst parents of school-aged children during the pediatric vaccine rollout. Vaccine. Nov 2022;40(46):6680–6687. https://doi.org/10.1016/j.vaccine.2022.09.090
Bianco A, Della Polla G, Angelillo S, Pelullo CP, Licata F, Angelillo IF. Parental COVID-19 vaccine hesitancy: a cross-sectional survey in Italy. Expert Rev Vaccines. Apr 2022;21(4):541–7. https://doi.org/10.1080/14760584.2022.2023013
Fisher CB, Bragard E, Jaber R, Gray A. COVID-19 vaccine hesitancy among parents of children under five years in the United States. Vaccines (Basel). Aug 2022;10(8). https://doi.org/10.3390/vaccines10081313
Krakowczyk JB, Bauerle A, Pape L, Kaup T, Nulle L, Teufel M, et al. COVID-19 vaccine for children: vaccination willingness of parents and its Associated Factors-A Network Analysis. Vaccines (Basel). 2022;10(7):20. https://doi.org/10.3390/vaccines10071155
Letterie MC, Patrick SW, Halvorson AE, Dupont WD, Carroll KN, Zickafoose JS, et al. Factors Associated with parental COVID-19 Vaccination Acceptance. Clin Pediatr (Phila). Jun 2022;61:5–6. https://doi.org/10.1177/00099228221084829
Tang S, Liu X, Jia Y, Chen H, Zheng P, Fu H, et al. Education level modifies parental hesitancy about COVID-19 vaccinations for their children. Vaccine. Jan 2023;41(2):496–503. https://doi.org/10.1016/j.vaccine.2022.11.060
Kitro A, Sirikul W, Dilokkhamaruk E, Sumitmoh G, Pasirayut S, Wongcharoen A, et al. COVID-19 vaccine hesitancy and influential factors among thai parents and guardians to vaccinate their children. Vaccine X. Aug 2022;11:100182. https://doi.org/10.1016/j.jvacx.2022.100182
Zhou X, Wang S, Zhang K, Chen S, Chan PS, Fang Y, et al. Changes in parents’ COVID-19 vaccine hesitancy for children aged 3–17 years before and after the rollout of the National Childhood COVID-19 Vaccination Program in China: repeated cross-sectional surveys. Vaccines (Basel). Sep 2022;10(9). https://doi.org/10.3390/vaccines10091478
Lau EYH, Li JB, King Chung Chan D. Intention to vaccinate young children against COVID-19: a large-scale survey of Hong Kong parents. Hum Vaccin Immunother. Nov 30 2022;18(5):2065838. https://doi.org/10.1080/21645515.2022.2065838
Willis DE, Schootman M, Shah SK, Reece S, Selig JP, Andersen JA, et al. Parent/guardian intentions to vaccinate children against COVID-19 in the United States. Hum Vaccin Immunother. Nov 30 2022;18(5):2071078. https://doi.org/10.1080/21645515.2022.2071078
Takahashi Y, Ishitsuka K, Sampei M, Okawa S, Hosokawa Y, Ishiguro A, et al. COVID-19 vaccine literacy and vaccine hesitancy among pregnant women and mothers of young children in Japan. Vaccine. Nov 2022;40(47):6849–6856. https://doi.org/10.1016/j.vaccine.2022.09.094
Humble RM, Sell H, Wilson S, Sadarangani M, Bettinger JA, Meyer SB, et al. Parents’ perceptions on COVID-19 vaccination as the new routine for their children ≤ 11 years old. Prev Med. Aug 2022;161:107125. https://doi.org/10.1016/j.ypmed.2022.107125
Letterie MC, Patrick SW, Halvorson AE, Dupont WD, Carroll KN, Zickafoose JS, et al. Factors Associated with parental COVID-19 Vaccination Acceptance. Clin Pediatr. 2022;61:5–6.
Green MS, Peer V, Magid A, Hagani N, Anis E, Nitzan D. Gender differences in adverse events following the Pfizer-BioNTech COVID-19 Vaccine. Vaccines (Basel). Feb 2022;10(2). https://doi.org/10.3390/vaccines10020233
Babicki M, Pokorna-Kalwak D, Doniec Z, Mastalerz-Migas A. Attitudes of parents with regard to vaccination of children against COVID-19 in Poland. A Nationwide Online Survey. Vaccines (Basel). 2021;9(10):17. https://doi.org/10.3390/vaccines9101192
Mangat C, Rich J, Sanghavi D, Schmidt R, Milosavljevic N, Linh T, et al. Parents’ perspective on COVID-19 vaccine in children 6 months through 4 years: a cross-sectional study from Northwest Wisconsin. BMJ Open. Sep 17 2022;12(9):e065453. https://doi.org/10.1136/bmjopen-2022-065453
Bell S, Clarke R, Mounier-Jack S, Walker JL, Paterson P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: a multi-methods study in England. Vaccine. Nov 2020;38(49):7789–7798. https://doi.org/10.1016/j.vaccine.2020.10.027
Han B, Song Y, Li C, Yang W, Ma Q, Jiang Z, et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine (CoronaVac) in healthy children and adolescents: a double-blind, randomised, controlled, phase 1/2 clinical trial. Lancet Infect Dis. 2021;21(12):1645–53.
Creech CB, Anderson E, Berthaud V, Yildirim I, Atz AM, Melendez Baez I, et al. Evaluation of mRNA-1273 Covid-19 vaccine in children 6 to 11 years of age. N Engl J Med. 2022;386(21):2011–23.
Frenck RW Jr, Klein NP, Kitchin N, Gurtman A, Absalon J, Lockhart S, et al. Safety, immunogenicity, and efficacy of the BNT162b2 Covid-19 vaccine in adolescents. N Engl J Med. 2021;385(3):239–50.
Xia S, Zhang Y, Wang Y, Wang H, Yang Y, Gao GF, et al. Safety and immunogenicity of an inactivated COVID-19 vaccine, BBIBP-CorV, in people younger than 18 years: a randomised, double-blind, controlled, phase 1/2 trial. Lancet Infect Dis. 2022;22(2):196–208.
Xia S, Zhang Y, Wang Y, Wang H, Yang Y, Gao GF, et al. Safety and immunogenicity of an inactivated SARS-CoV-2 vaccine, BBIBP-CorV: a randomised, double-blind, placebo-controlled, phase 1/2 trial. Lancet Infect Dis. 2021;21(1):39–51.
Lara D, Young T, Del Toro K, Chan V, Ianiro C, Hunt K, et al. Acute fulminant myocarditis in a pediatric patient with COVID-19 infection. Pediatrics. Aug 2020;146(2). https://doi.org/10.1542/peds.2020-1509
Trogen B, Gonzalez FJ, Shust GF. COVID-19-associated myocarditis in an adolescent. Pediatr Infect Dis J. Aug 2020;39(8):e204-e205. https://doi.org/10.1097/INF.0000000000002788
Bozkurt B, Kamat I, Hotez PJ. Myocarditis with COVID-19 mRNA vaccines. Circulation. Aug 2021;144(6):471–484. https://doi.org/10.1161/CIRCULATIONAHA.121.056135
Snapiri O, Rosenberg Danziger C, Shirman N, Weissbach A, Lowenthal A, Ayalon I, et al. Transient Cardiac Injury in Adolescents receiving the BNT162b2 mRNA COVID-19 vaccine. Pediatr Infect Dis J. 2021;40(10):e360–e. https://doi.org/10.1097/INF.0000000000003235
Minocha PK, Better D, Singh RK, Hoque T. Recurrence of Acute Myocarditis temporally Associated with receipt of the mRNA coronavirus Disease 2019 (COVID-19) vaccine in a male adolescent. J Pediatr. Nov 2021;238:321–3. https://doi.org/10.1016/j.jpeds.2021.06.035
Hadley SM, Prakash A, Baker AL, de Ferranti SD, Newburger JW, Friedman KG, et al. Follow-up cardiac magnetic resonance in children with vaccine-associated myocarditis. Eur J Pediatr. Jul 2022;181(7):2879–83. https://doi.org/10.1007/s00431-022-04482-z
Patel T, Kelleman M, West Z, Peter A, Dove M, Butto A, et al. Comparison of multisystem inflammatory syndrome in children-related myocarditis, classic viral myocarditis, and COVID-19 vaccine-related myocarditis in children. J Am Heart Assoc. May 2022;11(9):e024393. https://doi.org/10.1161/JAHA.121.024393
Rostad CA, Chahroudi A, Mantus G, Lapp SA, Teherani M, Macoy L, et al. Quantitative SARS-CoV-2 serology in children with multisystem inflammatory syndrome (MIS-C). Pediatrics. Dec 2020;146(6). https://doi.org/10.1542/peds.2020-018242
Yalcinkaya R, Oz FN, Polat M, Ucan B, Teke TA, Kaman A, et al. A case of Multisystem Inflammatory Syndrome in a 12-Year-old male after COVID-19 mRNA vaccine. Pediatr Infect Dis J. 2022;41(3):e87–e. https://doi.org/10.1097/INF.0000000000003432
Chai Q, Nygaard U, Schmidt RC, Zaremba T, Moller AM, Thorvig CM. Multisystem inflammatory syndrome in a male adolescent after his second Pfizer-BioNTech COVID-19 vaccine. Acta Paediatr. Jan 2022;111(1):125–7. https://doi.org/10.1111/apa.16141
Levy M, Recher M, Hubert H, Javouhey E, Flechelles O, Leteurtre S, et al. Multisystem inflammatory syndrome in children by COVID-19 vaccination status of adolescents in France. JAMA. Jan 2022;327(3):281–283. https://doi.org/10.1001/jama.2021.23262
Nygaard U, Holm M, Hartling UB, Glenthoj J, Schmidt LS, Nordly SB, et al. Incidence and clinical phenotype of multisystem inflammatory syndrome in children after infection with the SARS-CoV-2 delta variant by vaccination status: a danish nationwide prospective cohort study. Lancet Child Adolesc Health. Jul 2022;6(7):459–65. https://doi.org/10.1016/S2352-4642(22)00100-6
Anderson EJ, Creech CB, Berthaud V, Piramzadian A, Johnson KA, Zervos M, et al. Evaluation of mRNA-1273 vaccine in children 6 months to 5 years of age. N Engl J Med. 2022;387(18):1673–87.
Ali K, Berman G, Zhou H, Deng W, Faughnan V, Coronado-Voges M, et al. Evaluation of mRNA-1273 SARS-CoV-2 vaccine in adolescents. N Engl J Med. 2021;385(24):2241–51.
Siegrist C-A, Aspinall R. B-cell responses to vaccination at the extremes of age. Nat Rev Immunol. 2009;9(3):185–94.
Singh G, Tucker EW, Rohlwink UK. Infection in the developing brain: the role of unique systemic Immune Vulnerabilities. Front Neurol. 2022;12:2659.
Walter EB, Talaat KR, Sabharwal C, Gurtman A, Lockhart S, Paulsen GC, et al. Evaluation of the BNT162b2 Covid-19 vaccine in children 5 to 11 years of age. N Engl J Med. 2022;386(1):35–46.
Hu J, Peng P, Cao X, Wu K, Chen J, Wang K, et al. Increased immune escape of the new SARS-CoV-2 variant of concern Omicron. Cell Mol Immunol. Feb 2022;19(2):293–5. https://doi.org/10.1038/s41423-021-00836-z
Cohen-Stavi CJ, Magen O, Barda N, Yaron S, Peretz A, Netzer D, et al. BNT162b2 vaccine effectiveness against Omicron in Children 5 to 11 years of age. N Engl J Med. Jul 21 2022;387(3):227–36. https://doi.org/10.1056/NEJMoa2205011
Piche-Renaud PP, Swayze S, Buchan SA, Wilson SE, Austin PC, Morris SK, et al. COVID-19 vaccine effectiveness against Omicron infection and hospitalization. Pediatrics. Mar 2023;151(4):e2022059513. https://doi.org/10.1542/peds.2022-059513
Fleming-Dutra KE, Britton A, Shang N, Derado G, Link-Gelles R, Accorsi EK, et al. Association of prior BNT162b2 COVID-19 vaccination with symptomatic SARS-CoV-2 infection in children and adolescents during Omicron predominance. JAMA. Jun 2022;327(22):2210–2219. https://doi.org/10.1001/jama.2022.7493
Tan SHX, Cook AR, Heng D, Ong B, Lye DC, Tan KB. Effectiveness of BNT162b2 vaccine against Omicron in children 5 to 11 years of age. N Engl J Med. Aug 2022;387(6):525–32. https://doi.org/10.1056/NEJMoa2203209
Price AM, Olson SM, Newhams MM, Halasa NB, Boom JA, Sahni LC, et al. BNT162b2 protection against the Omicron variant in children and adolescents. N Engl J Med. May 2022;386(20):1899–909. https://doi.org/10.1056/NEJMoa2202826
Dorabawila V, Hoefer D, Bauer UE, Bassett M, Lutterloh E, Rosenberg E. Effectiveness of the BNT162b2 vaccine among children 5–11 and 12–17 years in New York after the emergence of the Omicron variant, MedRxiv, p. 2022.02. 25.22271454, 2022.
Sacco C, Manso MD, Mateo-Urdiales A, Rota MC, Petrone D, Riccardo F, et al. Effectiveness of BNT162b2 vaccine against SARS-CoV-2 infection and severe COVID-19 in children aged 5–11 years in Italy: a retrospective analysis of January-April, 2022. Lancet. Jul 2022;400(10346):97–103. https://doi.org/10.1016/S0140-6736(22)01185-0
Leung D, Rosa Duque JS, Yip KM, So HK, Wong WHS, Lau YL. “Effectiveness of BNT162b2 and CoronaVac in children and adolescents against SARS-CoV-2 infection during Omicron BA.2 wave in Hong Kong. Commun Med (Lond). Jan 2023;3(1):3. https://doi.org/10.1038/s43856-022-00233-1
Reis BY, Barda N, Leshchinsky M, Kepten E, Hernan MA, Lipsitch M, et al. Effectiveness of BNT162b2 vaccine against Delta variant in adolescents. N Engl J Med. Nov 2021;385(22):2101–3. https://doi.org/10.1056/NEJMc2114290
Olson SM, Newhams MM, Halasa NB, Price AM, Boom JA, Sahni LC, et al. Effectiveness of BNT162b2 vaccine against critical Covid-19 in adolescents. N Engl J Med. Feb 2022;386(8):713–23. https://doi.org/10.1056/NEJMoa2117995
Oliveira CR, Niccolai LM, Sheikha H, Elmansy L, Kalinich CC, Grubaugh ND, et al. Assessment of clinical effectiveness of BNT162b2 COVID-19 vaccine in US adolescents. JAMA Netw Open. Mar 2022;5(3):e220935. https://doi.org/10.1001/jamanetworkopen.2022.0935
Link-Gelles R, Levy ME, Gaglani M, Irving SA, Stockwell M, Dascomb K, et al. Effectiveness of 2, 3, and 4 COVID-19 mRNA vaccine doses among immunocompetent adults during periods when SARS-CoV-2 Omicron BA.1 and BA.2/BA.2.12.1 sublineages predominated - VISION network, 10 states, December 2021-June 2022. MMWR Morb Mortal Wkly Rep. Jul 2022;71(29):931–939. https://doi.org/10.15585/mmwr.mm7129e1
Chalkias S, Harper C, Vrbicky K, Walsh SR, Essink B, Brosz A, et al. A Bivalent Omicron-Containing booster vaccine against Covid-19. N Engl J Med. Oct 6 2022;387:1279–91. https://doi.org/10.1056/NEJMoa2208343
Wei Z, He J, Wang C, Bao J, Leng T, Chen F. The importance of booster vaccination in the context of Omicron wave. Front Immunol. 2022;13:977972. https://doi.org/10.3389/fimmu.2022.977972
Hause AM. Safety Monitoring of Bivalent COVID-19 mRNA vaccine booster doses among children aged 5–11 Years—United States, October 12–January 1, 2023, MMWR Morb Mortal Wkly Rep, vol. 72, 2023.
Hause AM, Marquez P, Zhang B, Myers TR, Gee J, Su JR, et al. Safety monitoring of bivalent COVID-19 mRNA vaccine booster doses among persons aged ≥ 12 years—United States, August 31–October 23, 2022. Morb Mortal Wkly Rep. 2022;71(44):1401–6.
The American College of Obstetricians and Gynecologists. COVID-19 vaccination considerations for obstetric–Gynecologic care. https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/12/covid-19-vaccination-considerations-for-obstetric-gynecologic-care?utm_source=redirect&utm_medium=web&utm_campaign=int.
Centers for Disease Control and Prevention. Interim clinical considerations for Use of COVID-19 vaccines currently approved or authorized in the United States. https://www.cdc.gov/vaccines/covid-19/clinical-considerations/interim-considerations-us.html
Halasa NB, Olson SM, Staat MA, Newhams MM, Price AM, Boom JA, et al. Effectiveness of maternal vaccination with mRNA COVID-19 vaccine during pregnancy against COVID-19-Associated hospitalization in infants aged < 6 months – 17 states, July 2021-January 2022. MMWR Morb Mortal Wkly Rep. Feb 2022;71(7):264–70. https://doi.org/10.15585/mmwr.mm7107e3
Burns MD, Muir C, Atyeo C, Davis JP, Demidkin S, Akinwunmi B, et al. Relationship between anti-spike antibodies and risk of SARS-CoV-2 infection in infants born to COVID-19 vaccinated mothers. Vaccines (Basel). Oct 2022;10(10):1696. https://doi.org/10.3390/vaccines10101696
Dattner I, Goldberg Y, Katriel G, Yaari R, Gal N, Miron Y, et al. The role of children in the spread of COVID-19: using household data from Bnei Brak, Israel, to estimate the relative susceptibility and infectivity of children. PLoS Comput Biol. 2021;17(2):e1008559.
Brandtzaeg P. Mucosal immunity: integration between mother and the breast-fed infant. Vaccine. 2003;21(24):3382–3388.
Posfay-Barbe KM, Wagner N, Gauthey M, Moussaoui D, Loevy N, Diana A, et al. COVID-19 in children and the dynamics of infection in families. Pediatrics. Aug 2020;146(2):e20201576. https://doi.org/10.1542/peds.2020-1576
Food D, Administration, Vaccines, Committee RBPA. FDA briefing document: EUA amendment request for Pfizer-BioNTech COVID-19 vaccine for use in children 6 months through 4 years of age. 2022.
World Health Organization. The Pfizer BioNTech (BNT162b2) COVID-19 vaccine: what you need to know. https://www.who.int/news-room/feature-stories/detail/who-can-take-the-pfizer-biontech-covid-19--vaccine-what-you-need-to-know
World Health Organization. The Moderna COVID-19 (mRNA-1273) vaccine: what you need to know. https://www.who.int/news-room/feature-stories/detail/the-moderna-covid-19-mrna-1273-vaccine-what-you-need-to-know
Food US. and Drug Administration. Coronavirus (COVID-19) update: FDA authorizes updated (bivalent) COVID-19 vaccines for children down to 6 months of age. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-updated-bivalent-covid-19-vaccines-children-down-6-months
Centers for Disease Control and Prevention. Stay up to date with COVID-19 vaccines including boosters. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html#2nd-dose
European Medicines Agency. Comirnaty. https://www.ema.europa.eu/en/medicines/human/EPAR/comirnaty
European Medicines Agency. Spikevax (previously COVID-19 vaccine Moderna) https://www.ema.europa.eu/en/medicines/human/EPAR/spikevax
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Wen J, Li J and Zhu S conceived the idea, analyzed the data, and drafted the manuscript; Du X, Li A, Zhang S and Shen S contributed towards the conception, wrote part of the article; Zhang Z, Yang L, and Sun C made great efforts to polish and revise the manuscript; all authors provided critical review and approved the final manuscript before submission.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wen, J., Du, X., Li, A. et al. Dilemmas and options for COVID-19 vaccination in children. Ital J Pediatr 49, 103 (2023). https://doi.org/10.1186/s13052-023-01513-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13052-023-01513-9