Abstract
Background
In patients with adrenal insufficiency (AI), adrenal crisis (AC) represents a clinical emergency. Early recognition and prompt management of AC or AC-risk conditions in the Emergency Department (ED) can reduce critical episodes and AC-related outcomes. The aim of the study is to report the clinical and biochemical characteristics of AC presentation to improve their timely recognition and proper management in a ED setting.
Methods
Single-centre, retrospective, observational study on pediatric patients followed at the Department of Pediatric Endocrinology of Regina Margherita Children’s Hospital of Turin for primary AI (PAI) and central AI (CAI).
Results
Among the 89 children followed for AI (44 PAI, 45 CAI), 35 patients (21 PAI, 14 CAI) referred to the PED, for a total of 77 accesses (44 in patients with PAI and 33 with CAI). The main causes of admission to the PED were gastroenteritis (59.7%), fever, hyporexia or asthenia (45.5%), neurological signs and respiratory disorders (33.8%). The mean sodium value at PED admission was 137.2 ± 1.23 mmol/l and 133.3 ± 1.46 mmol/l in PAI and CAI, respectively (p = 0.05). Steroids administration in PED was faster in patients with CAI than in those with PAI (2.75 ± 0.61 and 3.09 ± 1.47 h from PED access, p = 0.83). Significant factors related to the development of AC were signs of dehydration at admission (p = 0.027) and lack of intake or increase of usual steroid therapy at home (p = 0.059). Endocrinological consulting was requested in 69.2% of patients with AC and 48.4% of subjects without AC (p = 0.032).
Conclusion
children with AI may refer to the PED with an acute life-threatening condition that needs prompt recognition and management. These preliminary data indicate how critical the education of children and families with AI is to improve the management at home, and how fundamental the collaboration of the pediatric endocrinologist with all PED personnel is in raising awareness of early symptoms and signs of AC to anticipate the proper treatment and prevent or reduce the correlated serious events.
Similar content being viewed by others
Background
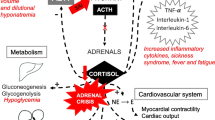
Adrenal Insufficiency (AI) is related to a dysfunction of the adrenal gland (primary adrenal insufficiency, PAI), or a reduced secretion of pituitary adrenocorticotrophic hormone (ACTH) or CRH (central adrenal insufficiency, CAI) [1,2,3].
The most common causes of PAI in children are congenital adrenal hyperplasia (CAH, 70% of PAI), isolated autoimmune adrenalitis (Addison disease, 15% of cases) or are part of autoimmune polyglandular syndromes, sepsis, bilateral adrenal haemorrhage associated with meningococcemia, and various genetic syndromes, as X linked adrenoleukodystrophy, Allgrove syndrome, DAX 1-deficiency and others (Table 1) [1,2,3,4]. A PAI determines inadequate glucocorticoids and mineralocorticoids secretion, while androgen secretion may be normal, reduced or increased depending on the underlying disease [1, 5].
The most common cause of CAI is iatrogenic suppression of the hypothalamic-pituitary adrenal (HPA) axis secondary to prolonged, high-dose glucocorticoid administration in chronic disease. Hypothalamic-pituitary diseases such as tumours, infiltrative lesions, congenital malformation, traumatic brain injury are the other frequent causes of CAI (Table 1) [6].
The clinical presentation of AI depends on the degree of impairment; the main symptoms include fatigue, nausea, muscle weakness and headache. Associated signs of AI can be dehydration, weight loss, lethargy, hyponatremia, hyperkalemia and hypoglycaemia. In case of PAI, elevated levels of ACTH and MSH for the absent negative feed-back from adrenals, lead to hyperpigmentation of the skin and mucous membranes, involving skin folds, armpits, groin, gums, and scars [1,2,3].
Diagnosis of AI is based on measurement of serum cortisol levels; a morning cortisol < 3 mcg/dl indicates AI, while cortisol levels > 15 mcg/dl rule out AI. For intermediate values it is mandatory to perform the dynamic test [6, 7].
The ACTH value can differentiate between PAI (ACTH above 2-fold upper normal values,) and CAI (inappropriately low-normal ACTH) [1, 5, 6].
PAI requires replacement therapy with both glucocorticoids (12–15 mg/mq/day) and mineralocorticoid (fludrocortisone 0.05–0.2 mg/day). In CAI, only cortisol replacement (10–12 mg/mq/day) is required, with no need for salt-retaining aldosterone replacement. The goal of therapy is to control the symptoms of AI with the lowest possible dose, without compromising the growth that is often observed in case of overtreatment [8, 9].
AC is a life-threatening emergency that requires prompt diagnosis and must be treated urgently. Literature data estimate an AC incidence of 5–10 episodes/100 patient-years and 1/200 episodes associated with a fatal outcome [10,11,12,13].
Stressful situations that can trigger AC include fever > 38 °C, intercurrent illness with vomiting, prolonged or massive diarrhea, infectious disease requiring antibiotics, acute trauma requiring medical intervention (such as fractures), anesthesia and associated surgical procedures [13, 14].
A serum cortisol concentration < 18 mcg/dL during acute illness can be indicative of AI. There is limited evidence to guide the optimal glucocorticoid dosing during stressful situations for children and adolescents with AI. Guidelines on stress cortisol requirements are based on the general evidence that conditions of maximal stress increase serum cortisol levels 2–3 times [11, 14].
After the diagnosis of AI, awareness and education about the symptoms and signs and treatment of cortisol deficiency to prevent AC should include the affected children and the family/caregivers and all healthcare professionals, from primary care physician to all ED personnel [14, 15].
Non-specific symptoms make the diagnosis of AC easily overlooked in the ED triage process; hypotension and hypoglycemia can develop suddenly, even after routine triage assessments, so providers must exercise a high index of suspicion for AC in any child who is at risk of AI [11, 12, 15].
Aim of this study is to provide useful information for emergency personnel to prevent, detect early and adequately treat AC in patients with AI during illness.
Methods
Patients with AI followed by the Department of Pediatric Endocrinology and admitted to the PED of the Regina Margherita Children’s Hospital of Turin, Italy, between January 1st, 2013 and March 1st, 2022, were enrolled in this single-centre, retrospective, observational study.
The diagnosis of AI and ED visits were identified according to the criteria of glucocorticoid or ACTH deficiency reported in the ICD-10- CM system (PAI or CAI). Patients’ data were retrospectively retrieved from patients’ records and included demographic data (age, sex, ethnic origin, and residence), clinical information (age at diagnosis, specific diagnosis, home therapies) and ED admission features (number of visits and clinical characteristics of AC, triage priority code, electrolytes and glycaemic values, acute phase treatment, need for endocrinologist consulting).
According to ICD-10-CM system, AC was defined as acute clinical deterioration precipitated by glucocorticoid deficiency or rapid clinical improvement after glucocorticoids administration, with at least two of the following symptoms or signs, i.e. severe fatigue, nausea and vomiting, somnolence, hypotension/sinus tachycardia relative to age-related norms, hyponatremia, hyperkalemia or hypoglycaemia.
Statistical analysis was performed using GraphPad 7 Software (GraphPad Software, La Jolla, CA, USA) and T-test, Wilcoxon-Mann-Whitney test and Chi Square were applied to compare the clinical and demographic characteristics of the patients.
The study was conducted according to the guidelines of the Declaration of Helsinki and received the approval of the Hospital Ethics Committee. Informed parental consent was obtained from each participant.
Results
The population with adrenal insufficiency (AI) followed by the Endocrinology Department of our Centre consisted of 89 children (56 boys, 33 girls). Of these, 44 were diagnosed as PAI (49.4%) and 45 as CAI (50.6%), due to different etiologies, represented in Fig. 1.
Demographic and clinical data of patients with PAI and CAI are represented in Table 2.
Mean age at diagnosis was 1.72 ± 0.58 and 5.32 ± 0.77 years for patients affected by PAI and CAI respectively.
During the study period, 35 patients accessed to the PED of the same hospital, 21 with PAI (47.7%) and 14 with CAI (31.1%) [p = 0.1]. AC was detected in 13/35 children (37,1%), 10/13 in children affected with PAI (77%) and 3/13 in children with CAI (23%). A total of 77 ED accesses were registered, 44 (57.1%) in patients with PAI and 33 (42.9%) with CAI. Among ED accesses 26/77 (33.8%) presented AC, with no difference between children with PAI and CAI forms.
Mean age at ED access was 5.56 ± 1.03 years for patients with PAI and 5.37 ± 1.04 years for patients with CAI (p = 0.89).
Regarding home therapy, the mean hydrocortisone dosage at ED admission was 13.7 ± 0.95 mg/m2/day in patients with PAI, while 14.3 ± 0.73 mg/m2 /day in patients with CAI (p = 0.65). Patients with PAI also required fludrocortisone treatment at a mean dosage of 100 ± 50 mcg/day.
At diagnosis all patients were instructed to increase the hydrocortisone dosage in case of stressful situations. However, at the ED survey patients had not changed their usual steroid therapy in 58.4% of cases, 14.3% doubled and 18.2% tripled their usual dose, the 6.5% has missed steroid administration or was unable to take the usual steroid dose, with no difference between PAI and CAI patients. Intramuscular administration of hydrocortisone was required in 2 only patients.
At access to the ED, the yellow code was the main triage code assigned, due to moderately critical conditions of the patients (65.2%). In 93.5% of ED accesses, patients communicated to the triage setting to suffer from AI.
The main causes of hospitalization were signs of gastroenteritis, with vomiting and/or diarrhea (59.7%), followed by other causes including fever, hyporexia or asthenia (45.5%), neurological signs and respiratory disorders (33.8%), while only 2.6% and 1.3% had signs of dehydration or hypoglycaemia, respectively. Laboratory tests performed at ED access revealed a higher prevalence of hyponatremia and hypoglycemia than in patients without AC. The mean glucose value in patients with PAI was 73.6 ± 10.9 mg/dl, while 84.8 ± 12.4 mg/dl in patients with CAI (p = 0.5). The mean sodium value was 137.2 ± 1.23 mmol/l and 133.3 ± 1.46 mmol/l in PAI and CAI, respectively (p = 0.05).
During the ED access, 56% of patients received endovenous steroid therapy and 49.4% parenteral hydration; almost all patients with AC received parenteral hydration (12/13, 92.3%) with normal saline (2/12, 16.7%), dextrose solution (9/12, 75%) or both (1/12, 8.3%).
In the PED, steroids were administered earlier in patients with CAI than with PAI (2.75 ± 0.61 and 3.09 ± 1.47 h from PED access, p = 0.83).
Children who developed AC were treated with a slightly but not significantly lower dose of hydrocortisone than those who did not show AC (11.90 and 12.30 mcg/kg/day, respectively, p = 0.608).
The risk factors for the development of AC according to multivariate regression analysis were the signs of dehydration at presentation (p = 0.027) and failure to take or increase the usual steroid therapy at home (75% of patients with AC did not increase home therapy as recommended, p = 0.059).
No significant differences were observed in clinical features among patients who developed AC compared to patients who did not developed AC.
Patients with AC for whom pediatric endocrinological consulting was requested were significantly higher than those without AC (9/13, 69.2% and 10/22, 45.4%, respectively, p = 0.032). Almost all ED accesses of patients with AC resulted in hospitalization (24/26, 92.3%); the main diagnoses at ED discharge were dehydration and hypoglycaemia.
Discussion
AI is a rare disease that requires replacement treatment to restore well-being and to prevent life-threatening events.
AC occurs with an acute deterioration in health status associated with acute hemodynamic imbalance, with hypotension or sinus tachycardia, or marked metabolic disorders, i.e. hyponatremia, hyperkalemia, or hypoglycemia. It represents the most severe complication of AI, which can occur in several stressful situations; its susceptibility varies among patients and unknown risk factors may potentiate the risk of occurrence [16].
The education of the pediatric patient and his family, as well as all the personnel working in the PED is essential to prevent and promptly treat this acute complication at home and upon arrival at the hospital during sick events. Previous findings suggest that physicians are the primary source for obtaining information about the disease and its complications. However, evidence show the need to improve their performances and awareness [16,17,18].
The incidence of AC in our cohort (3.2 episodes/100 patient-year) was in accordance with literature data [13, 14, 16]. Admission rates were higher among pre-school patients, as reported by previous studies, which may be explained by the frequent infections in this age group. Literature data describe a second peak of accesses to the ED in adolescents, attributable to the transition period from paediatric to adult services, to greater patient autonomy and the reduced adherence to therapy, exposing them to a greater risk of complications [17,18,19]. The same period of life is often characterized by the need for a therapy adjustment for the pubertal status.
To raise awareness of AC among healthcare professionals, consensus guidelines for patients with AI recommend that patients wear or carry medical alert devices, such as wallet cards, even though currently these alert devices are rarely used. In the present study, the patient informed the triage about the AI condition in 93.5% of accesses to the PED. Future use of a critical information note (CIN), as reported previously [15, 17], could provide details on the signs and symptoms to consider and recommendations to follow for the most appropriate management of AI patients in triage settings.
The patients described presented to the Hospital primarily for infectious diseases, mostly gastroenteritis, with no evidence of hemodynamic compromise. Of these, approximately half patients (44%) were later discharged after clinical evaluation, feeling well, without receiving additional steroid therapy during PED access, as most of them had doubled or tripled the habitual steroid dose at home prior to PED access. Literature data confirm that this could be the first approach to a patient with AI during stressful situations [11, 15].
In the cohort studied, a lower usual hydrocortisone replacement dose was observed in patients who developed AC; furthermore, home steroid therapy was not increased in 75% of cases. Based on epidemiological data, it has in fact been suggested that the increase in AC rates may be due to the current use of lower doses of glucocorticoids in patients with hypoadrenalism [5, 14, 18, 20].
Previous data report that children with PAI are at higher risk for AC than subjects affected by secondary forms [13, 14, 18,19,20], although in our cohort this difference was not significant, probably due to the low number of AC.
Eyal et al. suggested that younger age at diagnosis may be a risk factor for AC, with a higher incidence of AC in the first year of life [13]. In our cohort, age did not significantly influence the presentation of AC and there was no difference in the mean age at ED admission between primary and secondary forms.
The most common biochemical feature of AC was hyponatremia, occurring in 53.8% of the subjects, with lower mean sodium value in primary than secondary forms (p = 0.05), followed by hypoglycemia (38.5%), in accordance to previous studies on children and adults, especially on patients with PAI [10, 11, 18,19,20].
Treatment of AC is effective when given promptly. In the PED setting, steroid administration was faster in CAI than PAI patients, probably for more severe and acute presentation and the recognized underlying disease in the latter form. Findings from a previously published survey result from AI adult patients in the United Kingdom reported a time limit of 30 min from ED arrival to hydrocortison administration. Additional interventions, such as triage protocols for patients with AI, might be useful to expedite hydrocortison administration after clinical evaluation [15, 18].
The risk factors for the development of AC were dehydration at presentation and the failure to take or increase habitual steroid therapy at home.
Appropriate management requires prompt recognition of the clinical signs, symptoms and biochemical profile of AI and AC triggers [21].
To our knowledge, this is the first study that reports the clinical features of AI patients accessing a PED and evaluates risk factors for AC. The strengths of the study are that the information is based on the patients’ medical records and not on their self-reports and that the cohort includes patients with both primary and secondary AI.
Limitations are the retrospective nature of the study, with potential under- or over-reporting of AC. Certainly, further prospective and multicenter studies are needed to analyze the accesses of patients with AI in the PED, to establish guidelines for the management of these patients with potentially life-threatening events in emergency settings.
Conclusions
Children with AI may present to the PED setting with an acute life-threatening condition that requires prompt and effective recognition and management to avoid serious complications.
Our study confirms the previously observed high complexity of this disease, especially in the emergency setting, and added more information on the clinical characteristics of these patients and some red flags to consider.
While patient and family education is the key to successful prevention and treatment of AC crises at home in AI patients, it should be emphasized that raising information and awareness of this rare but potentially fatal complication in all healthcare professionals working in emergency settings is equally critical, to recognize it early and treat it adequately.
Data Availability
All data are available upon request to the corresponding author.
References
Bowden SA, Henry R. Pediatric adrenal insufficiency: diagnosis, management, and New Therapies. Int J Pediatr. 2018 Nov;2018:1.
Charmandari E, Nicolaides NC, Chrousos GP. Adrenal insufficiency. Lancet. 2014 Jun;21(9935):2152–67.
Arlt W, Allolio B. Adrenal insufficiency. Lancet. 2003 May 31;361(9372):1881-93.
Speiser PW, Azziz R, Baskin LS, Ghizzoni L, Hensle TW, Merke DP, Meyer-Bahlburg HF, Miller WL et al. Congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010 Sep;95(9):4133-60. https://doi.org/10.1210/jc.2009-2631. Erratum in: J Clin Endocrinol Metab. 2021 Jun 16;106(7):e2853.
Bornstein SR, Allolio B, Arlt W, Barthel A, Don-Wauchope A, Hammer GD, et al. Diagnosis and treatment of primary adrenal insufficiency: an endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016 Feb;101(2):364–89.
Kazlauskaite R, Maghnie M. Pitfalls in the diagnosis of central adrenal insufficiency in children. Endocr Dev. 2010;17:96–107.
Kazlauskaite R, Evans AT, Villabona CV, Abdu TA, Ambrosi B, Atkinson AB et al. Consortium for evaluation of Corticotropin Test in Hypothalamic-Pituitary adrenal insufficiency. Corticotropin tests for hypothalamic-pituitary- adrenal insufficiency: a metaanalysis. J Clin Endocrinol Metab 2008 Nov;93(11):4245–53.
Shulman DI, Palmert MR, Kemp SF. Lawson Wilkins drug and therapeutics Committee. Adrenal insufficiency: still a cause of morbidity and death in childhood. Pediatrics. 2007 Feb;119(2):e484–94.
Miller BS, Spencer SP, Geffner ME, Gourgari E, Lahoti A, Kamboj MK, et al. Emergency management of adrenal insufficiency in children: advocating for treatment options in outpatient and field settings. J Investig Med. 2020 Jan;68(1):16–25.
Ishii T, Adachi M, Takasawa K, Okada S, Kamasaki H, Kubota T, et al. Incidence and characteristics of adrenal Crisis in Children younger than 7 years with 21-Hydroxylase Deficiency: a Nationwide Survey in Japan. Horm Res Paediatr. 2018;89(3):166–71.
Burger-Stritt S, Kardonski P, Pulzer A, Meyer G, Quinkler M, Hahner S. Management of adrenal emergencies in educated patients with adrenal insufficiency-A prospective study. Clin Endocrinol (Oxf). 2018 Jul;89(1):22–9.
Rushworth RL, Torpy DJ, Falhammar H. Adrenal Crisis. N Engl J Med. 2019 Aug;29(9):852–61.
Eyal O, Levin Y, Oren A, Zung A, Rachmiel M, Landau Z, et al. Adrenal crises in children with adrenal insufficiency: epidemiology and risk factors. Eur J Pediatr. 2019 May;178(5):731–8.
Ali SR, Bryce J, Haghpanahan H, Lewsey JD, Tan LE, Atapattu N et al. Real-World Estimates of Adrenal Insufficiency-Related Adverse Events in Children With Congenital Adrenal Hyperplasia. J Clin Endocrinol Metab. 2021 Jan 1;106(1):e192-e203.
Halpin KL, Paprocki EL, McDonough RJ. Utilizing health information technology to improve the recognition and management of life-threatening adrenal crisis in the pediatric emergency department: medical alert identification in the 21st century. J Pediatr Endocrinol Metab 2019 May 27;32(5):513–8.
Rushworth RL, Torpy DJ, Stratakis CA, Falhammar H. Adrenal crises in children: perspectives and research directions. Horm Res Paediatr. 2018;89(5):341–51.
Hahner S, Hemmelmann N, Quinkler M, Beuschlein F, Spinnler C, Allolio B. Timelines in the management of adrenal crisis - targets, limits and reality. Clin Endocrinol (Oxf). 2015 Apr;82(4):497–502.
Hsieh S, White PC. Presentation of primary adrenal insufficiency in childhood. J Clin Endocrinol Metab. 2011 Jun;96(6):E925–8.
Wijaya M, Huamei M, Jun Z, Du M, Li Y, Chen Q et al. Etiology of primary adrenal insufficiency in children: a 29-year single-center experience. J Pediatr Endocrinol Metab 2019 Jun 26;32(6):615–22.
Capalbo D, Moracas C, Cappa M, Balsamo A, Maghnie M, Wasniewska MG et al. Primary adrenal insufficiency in Childhood: Data from a large Nationwide Cohort. J Clin Endocrinol Metab 2021 Mar 8;106(3):762–73.
Simpson A, Ross R, Porter J, Dixon S, Whitaker MJ, Hunter A. Adrenal insufficiency in Young Children: a mixed methods study of parents’ experiences. J Genet Couns. 2018 Dec;27(6):1447–58.
Acknowledgements
Not applicable.
Funding
No funds nor grants have supported this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study design and conception. Material preparation, data collection and analysis were performed by JM and GT. The clinical management of the enrolled subjects was managed by EA, CB, EC. The first draft of the manuscript was written by EA, JM, PM and LdS and all authors have commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the principles of the Declaration of Helsinki. The approval was granted by the Ethics Committee of the City of Health and Science University Hospital of Turin (01/09/2022, 13988/A1). Written parental consent to participate was obtained.
Consent for publication
Consent to publish has been received from all partecipants.
Competing interests
All authors have nothing to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Abrigo, E., Munarin, J., Bondone, C. et al. Adrenal insufficiency management in the pediatric emergency setting and risk factors for adrenal crisis development. Ital J Pediatr 49, 63 (2023). https://doi.org/10.1186/s13052-023-01475-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13052-023-01475-y