Abstract
Background
Rapid and accurate identification of pathogens is very important for the treatment of Severe community-acquired pneumonia (SCAP) in children. Metagenomic Next-generation sequencing (mNGS) has been applied in the detection of pathogenic bacteria in recent years, while the overall evaluation the application of SCAP in children is lacking.
Methods
In our study, 84 cases of SCAP were enrolled. Bronchoalveolar lavage fluid (BALF) samples were analysed using mNGS; and sputum, blood, and BALF samples were analysed using conventional technology (CT).
Results
Among the 84 children, 41 were boys, and 43 were girls, with an average age ranging from 2 months to 14 years. The pathogen detection rate of mNGS was higher than that of CT (83.3% [70/84] vs. 63.1% [53/84], P = 0.003). The mNGS was much greater than that of the CT in detecting Streptococcus pneumoniae (89.2% [25/29] vs. 44.8% [13/29], P = 0.001) and Haemophilus influenzae (91.7% [11/12] vs. 33.3% [4/12], P < 0.005). The mNGS also showed superior fungal detection performance compared with that of the CT (81.8% [9/11] vs. 18.2% [2/11], P = 0.004). The mNGS test can detect viruses, such as bocavirus, rhinovirus, and human metapneumovirus, which are not frequently recognised using CT. However, the mNGS detection rate was lower than that of the CT (52.4% [11/21] vs. 95.2% [20/21], P = 0.004) for Mycoplasma pneumoniae (MP). The detection rate of mNGS for mixed infection was greater than that of the CT, although statistical significance was not observed (26.3% [20/39] vs. 21.1% [16/39], P > 0.005). Treatment for 26 (31.0%) children was changed based on mNGS results, and their symptoms were reduced; nine patients had their antibiotic modified, five had antibiotics added, nine had their antifungal medication, and seven had their antiviral medication.
Conclusion
mNGS has unique advantages in the detection of SCAP pathogens in children, especially S. pneumoniae, H. influenzae, and fungi. However, the detection rate of MP using mNGS was lower than that of the CT. Additionally, mNGS can detect pathogens that are not generally covered by CT, which is extremely important for the modification of the treatment strategy.
Similar content being viewed by others
Background
Community-acquired pneumonia (CAP) is a common respiratory disease in children with significantly higher morbidity and mortality rates in developing countries than that in developed countries [1]. According to the World Health Organization (WHO) report, the incidence of CAP in children under 5 years of age in developing countries is 0.28 times/child/year, accounting for 95% of all cases of CAP in children worldwide, and the mortality rate is 1.3–2.6% [2]. In North America and Europe, the incidence rate among pre-schoolers is 36 per 1,000 children per year [3], placing a significant economic burden on families and society. Children with CAP are prone to develop pleural effusion, lung abscess, pericarditis, meningitis, and other pulmonary and external complications [4], which eventually lead to severe community-acquired pneumonia (SCAP), respiratory and circulatory failure, or even life-threatening complications. For the pathogen diagnosis of CAP, clinical work is carried out in various microorganisms, including viruses, bacteria, and atypical pathogen combination detection to avoid missed diagnosis and mixed infection, although pathogens cannot be identified or detected in 22–57% of children [5,6,7] and 13–62% of adult with pneumonia [8, 9]. Culture, the gold standard for bacterial and fungal infection diagnosis, has high accuracy but a long detection time and low detection rate and is not suitable for the identification of pathogens that are difficult to cultivate. Viruses and atypical pathogens can be detected by polymerase chain reaction (PCR) and antigen detection, but the positive rate varies greatly and suitable for detecting only the known, limited target pathogens. In addition, some unknown pathogens in nature cannot be detected. Therefore, there is an urgent need for rapid and accurate diagnostic methods to identify pathogens in children with SCAP [10].
Metagenomic next-generation sequencing (mNGS) is a method for whole nucleic acid detection using patient samples directly [11], which can simultaneously detect various microorganisms. It has the characteristics of being less affected by antibiotics, taking a wide range of samples, and does not need to set gene sequences in advance. Therefore, it greatly applicable in diagnosis of new and rare infectious diseases [10, 12,13,14]. Currently, mNGS has been applied in the diagnosis of infectious diseases of the lungs, blood system, and central nervous system in adults [15,16,17]. Sepsis, encephalitis, and bone and joint infections have also been reported in children [18,19,20]. However, no study has been conducted on bronchoalveolar lavage fluid (BALF) in children with SCAP. In this study, 84 children with SCAP were enrolled for bronchoscopic lavage. BALF was used as the sample source to evaluate the value of mNGS in the diagnosis of SCAP in children by comparing it with conventional technology (CT).
Methods
Patient Inclusions
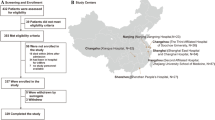
In this retrospective analysis, 84 children diagnosed with SCAP were enrolled in Tianjin Children's Hospital from January 2019 to December 2021. After admission, a fiberoptic bronchoscopy was done within 48 h. bronchoalveolar lavage fluid (BALF) was taken for mNGS detection and CT was performed simultaneously.
Inclusion criteria were as follows: (I) all patients met the SCAP diagnostic criteria; (II) pediatric patients under 14 years of age were selected; (III) BALF obtained by bronchoscopy in patients who met the bronchoscopy indications. The following conditions will be excluded from the study: (I) mNGS was not performed; (II) incomplete clinical data; (III) loss to follow up. The study was approved by The Tianjin Children’s Hospital Ethics Committee (No. L2020-02) and was in line with the Declaration of Helsinki (as revised in 2013) (Fig. 1).
SCAP definition (Includes one of the following): (I) oxygen saturation < 92%, cyanosis; (II) respiratory rate > 50 breaths/min, Infant respiratory rate > 70 breaths/min; (III) significant tachycardia for level of fever (values to define tachycardia vary with age and with temperature); (IV) prolonged central capillary refill time > 2 s; (V) difficulty in breathing; (VI) intermittent apnoea, grunting; (VII) signs of dehydration; (VIII) Infant feeding difficulties [21].
Indications for fiberoptic bronchoscopy: (I) repeated or persistent wheezing; (II) limited wheezing; (III) recurrent respiratory tract infections; (IV) hemoptysis; (V) Difficulty in withdrawing from the ventilator; (VI) Abnormal chest imaging: ① atelectasis, ② emphysema, ③ mediastinal emphysema, ④ pulmonary mass lesion, ⑤ pleural cavity lesion requiring differential diagnosis; (VII) Etiological diagnosis and treatment of pulmonary infectious diseases [22].
The study was approved by the ethics committee of Tianjin Children's Hospital, and patient data were analyzed anonymously.
Conventional technology (CT)
For hospitalized children with SCAP, blood and sputum were collected within 24 h of admission, and alveolar lavage fluid was collected within 48 h of admission. The sample source for the CT technique is mostly the BALF because it is challenging to obtain sputum from children and blood infection is quite uncommon in this study. Bacteria was detected by culture method and commercial PCR-based kits for the detection eight common respiratory bacteria (Streptococcus pneumoniae, Staphylococcus aureus, methicillin resistant Staphylococcus aureus, Klebsiella pneumoniae, Pseudomonas aeruginosa,Acinetobacter baumannii, Stenostomonas maltophilia, and Haemophilus influenzae) (Capitalbio Jinxin Bio- Technology Co., Ltd., Chengdu, China). The virus was detected by PCR (Epstein–Barr virus (EBV), cytomegalovirus (CMV), influenza A/B (Da’an Gene Technology Co., 96 Ltd., Guangzhou, China); and adenoviruses (Puruikang Biotech Co., Ltd., Shenzhen, China)). Fungi (Candida albicans, Pneumocystis vulgaris, Cryptococcus neoformans) was detected by culture method. Mycobacterium tuberculosis was detected by culture, PCR and MTB-Xpert. PCR was used to detect chlamydia and Legionella. Mycoplasma pneumoniae was detected by particle agglutination (PA) (serum MP-Ab ≥ 1:160 or MP-Ab increased or decreased by 4 times or more in recovery and acute stages), immune colloidal gold technigue (GICT) (single MP-IgM positive) [23] and PCR.
mNGS testing
Sample processing and nucleic acid extraction
The BALF sample, which is viscous and contains particles in suspension, is liquefied. Utilized a DTT reagent with a concentration of 80 mM. According to the viscosity of the sample, 1 ~ 3 times of the sample volume of DTT was added, and the sample was shaken and left at room temperature for five minutes. Non-viscous samples were directly enriched by centrifugation and the samples were stored at -20 °C. DNA was extracted from all samples using a QIAamp® UCP Pathogen DNA Kit (Qiagen) following the manufacturer’s instructions. Human DNA was removed using Benzonase (Qiagen) and Tween20 (Sigma). Total RNA was extracted with a QIAamp® Viral RNA Kit (Qiagen) and ribosomal RNA was removed by a Ribo-Zero rRNA Removal Kit (Illumina). cDNA was generated using reverse transcriptase and dNTPs (Thermo Fisher).
Library construction and sequencing
Libraries were constructed for the DNA and cDNA samples using a Nextera XT DNA Library Prep Kit (Illumina, San Diego, CA). DNA library construction includes fragmentation, end repair, ligation and purification of connectors, PCR amplification and purification, library concentration, and fragment quality monitoring. For effective libraries, the Qubit concentration was at least 1 ng/L, and the primary peak of the library fragment was between 280 and 320 bp. Library was quality assessed by Qubit dsDNA HS Assay kit followed by High Sensitivity DNA kit (Agilent) on an Agilent 2100 Bioanalyzer. Library pools were then loaded onto an Illumina Nextseq CN500 sequencer for 75 cycles of single-end sequencing to generate approximately 20 million reads for each library. For negative controls, we also prepared PBMC samples with 105 cells/mL from healthy donors in parallel with each batch, using the same protocol, and sterile deionized water was extracted alongside the specimens to serve as non-template controls (NTC).
Bioinformatics analyses
Trimmomatic was used to remove low quality reads, adapter contamination, and duplicate reads, as well as those shorter than 50 bp. Low complexity reads were removed by Kcomplexity with default parameters. Human sequence data were identified and excluded by mapping to a human reference genome (hg38) using Burrows-Wheeler Aligner software. We designed a set of criteria similar to the National Center for Biotechnology Information (NCBI) criteria for selecting representative assembly for microorganisms (bacteria, viruses, fungi, protozoa, and other multicellular eukaryotic pathogens) from the NCBI Nucleotide and Genome databases. The final database consisted of about 13,000 genomes. Microbial reads were aligned to database with SNAP v1.0beta.18. The database performance (a certain number of clinical validation samples) has a specificity of 96.2% and a sensitivity of 100%.
Interpretation of mNGS results
Currently, there is a lack of unified interpretation standards for mNGS. This study formulated the following standards based on previous literature [15, 24,25,26].
1) When the relative abundance of an organism at the species level is greater than 30% and there is supporting literature evidence of lung pathogenicity, regardless of the results of the CT method.
2) mNGS detected the same pathogenic bacteria as CT and more than 50 single microbe reads.
3) Mycobacterium tuberculosis and Legionella pneumophila are considered positive when at least one read is mapped to the species or genus level.
4) Oral and respiratory custom bacteria are not considered pathogenic bacteria, regardless of their relative abundance, unless otherwise proved or they are considered pathogenic bacteria.
CT and NGS alone could not determine whether the microorganism was infected. Finally, two senior attending physicians determined the pathogen based on clinical characteristics and reached a consensus.
Statistical analysis
Data were processed using SPSS 26.0. Continuous variables were expressed as mean ± standard deviation (SD) and assessed by independent group t tests. Categorical variables were expressed as percentage (%) and assessed by Chi-squared tests or Fisher’s exact test. A two-sided α less than 0.05 were considered as statistically significant.
Results
General characteristics of selected children
Among the 84 patients, 41 were boys, and 43 were girls, with age ranging from 2 months to 14 years and an average of 4.4 years. There were 18 (21.4%) children with basic diseases, 6 (7.1%) had congenital heart disease; 4 (4.8%) had bronchial asthma; and primary ciliary dyskinesia, hepatoblastic carcinoma, renal malformation, giant gyri malformation, diabetes, chronic granuloma, pelvic tumour, and congenital cleft palate was each reported in 1 child. The most common symptoms were cough (92.9%), fever (73.8%), and dyspnoea (35.7%), followed by poor mental health (27.4%), stridor (26.2%), and chest pain (11.9%), and the last was haemoptysis (2.4%). A total of 65 cases (77.4%) reported moist rales, and 26 (31%) had diminished respiratory sounds. In addition, 54 (62.3%) children exhibited severe lung imaging, including 36 with pleurisy (42.9%), 28 with inflammatory consolidation (33.3%), 24 with (28.6%), 20 with pleural effusion (23.8%), 20 with atelectasis (23.8%), 11 with necrosis (13.1%), and 7 with interstitial abnormalities (8.3%). The white blood cell (WBC) count (12.57 ± 6.46 × 109/L) was calculated, as was the neutrophil ratio (77.06 ± 11.96%), the lymphocyte ratio (13.98 ± 6.30%), the C-reactive protein (CRP) (77.13 ± 59.58 mg/L), and the procalcitonin (PCT) (11.03 ± 17.57 ng/mL). Before admission, 72 (85.7%) patients had been treated with antibiotics and 20 (23.8%) with glucocorticoids (Table 1).
The pathogen detection of SCAP
The most common pathogen detected using mNGS was Streptococcus pneumoniae (25 strains), human herpesvirus type 5 (12 strains), Haemophilus influenzae (11 strains), and Mycoplasma pneumoniae (MP) (11 strains). Pathogens, such as oral Streptococcus, Bifidobacterium brevis, Bacteroides fragilis, and Candida proximalis, were also detected. Combined with clinical manifestations, the bacteria were considered as respiratory colonising bacteria, not pathogenic ones (Fig. 2).
The most common pathogens detected using CT were MP (20 strains), S. pneumoniae (13 strains), and Staphylococcus aureus (10 strains).
Finally, 76 cases (90.5%) were diagnosed with determinate pathogen infection, and 18 (23.7%) were bacterial infections. Six patients (7.9%) were infected with a virus, and there were 10 (13.2%) cases of atypical bacterial infection. In addition, there were three (3.9%) cases of Mycobacterium tuberculosis (MTB) infection and 39 (51.3%) of mixed infection (Fig. 3A).
The detection rate of mNGS and CT
The sensitivity, specificity, positive predictive value and negative predictive value of mNGS were 92.1% (70/76), 62.5% (5/8), 95.9% (70/73) and 45.5% (5/11), respectively. mNGS detection rate was 83.3% (70/84), which was higher than that of the CT at 63.1% (53/84) (P = 0.003).
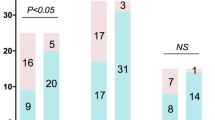
The bacterial detection rate of mNGS was higher than that of the CT (80.8% [42/52] vs. 44.2% [23/52], P < 0.001) (Fig. 4A). The detection rate of Gram-negative bacteria was significantly higher in mNGS than that in the CT (90.1% [20/22] vs. 22.7% [5/22], P < 0.001), while there was no significant difference in Gram-positive bacteria (75% [30/40] vs. 57.5% [23/40], P = 0.098). S. pneumoniae was the most detected bacteria in 29 cases, in which the detection rate of mNGS was higher than that of the CT (89.2% [25/29] vs. 44.8% (13/29), P = 0.001). A total of nine cases were detected using mNGS and CT, sixteen were only positive for mNGS, and four were only positive for CT. The second most detected bacteria were H. influenzae (12 cases), in which the detection rate of mNGS was higher than that of the CT (91.7% [11/12] vs. 33.3% [4/12], P < 0.005). mNGS alone detected eight cases, CT alone detected one, and common method detected three. There were 12 cases of S. aureus, three were detected using mNGS and CT, two were only positive for mNGS, and seven were positive for CT. Among the three children with Enterococcus faecalis infection, two were detected using CT and one using mNGS. E. faecium and Micrococcus gamboge were identified by culture but not by mNGS in patient 59. There were three cases of Klebsiella pneumoniae, one in patient 11, one in patient 44, detected using mNGS, and one in patient 64, detected using CT. There were two cases of Pseudomonas aeruginosa, one of which was detected using both mNGS and CT and the other using mNGS alone. Additionally, mNGS detected Prevotella melanogenes in patient 26, Enterobacter cloacae in patients 43 and 44, Escherichia coli in patient 50, and Acinetobacter baumannii in patient 65, all of which were not detected on CT.
Comparison of pathogens detected by Metagenomic Next-generation sequencing (mNGS) and Conventional technology (CT). A Bateria detected by mNGS and CT methods. B Virus detected by mNGS and CT methods. C Fungus detected by mNGS and CT methods. D Atypical pathogen detected by mNGS and CT methods. ADV, adenovirus; CMV, human herpes virus; EBV, Epstein-Barr virus,; RSV, Respiratory syncytial virus
For virus detection, the detection rate of mNGS was higher than that of the CT, but there was no statistical significance (76% [19/25] vs. 56% [14/25], P = 0.136) (Fig. 4B). Respiratory syncytial virus (RSV) and Epstein-Barr virus (EBV) were the most frequently detected viruses, with seven cases each. mNGS alone identified five cases of RSV, while CT alone identified one case; however in patient 79, RSV was detected using both mNGS and CT. EBV was detected by CT in six cases (patients 9,10, 13, 53, 63, and 65), and by mNGS in four cases (patients 13, 36, 63, and 65). Boca virus (HBoV) was detected in four cases, all of which were detected by mNGS. In three cases of CMV infection, both mNGS and CT were positive. Two cases of adenovirus (ADV) and one case of influenza A virus were detected using CT. However, mNGS detected bocavirus in patients 39, 42, 68, and 76, rhinovirus in patient 58, and human metapulmonary virus in patient 66.
The detection rate of fungi using mNGS was higher than that of the CT (81.8% [9/11] vs. 18.2% [2/11], P = 0.004) (Fig. 4C). Pneumocystis vulgaris (four cases) was the most frequently detected fungus, followed by C. albicans (three cases). There was one case of Cryptococcus neoformans, Aspergillus aspergillus, and Aspergillus niger. Only two instances of C. albicans were discovered using CT in patients 62 and 83. However, mNGS missed only patient 83. In patient 26, mNGS and CT were both negative, but the serum G test (1, 3-D glucan test) was positive (301 pg/mL), which matched the clinical symptoms and imaging diagnosis of fungal infection.
There was no significant difference in the detection rate of MTB between mNGS and CT (60% [3/5] vs. 80% [4/5], P > 0.005). A total of two cases were detected using mNGS and CT, one case was detected using mNGS alone, two cases were detected using CT, three were detected using MTB-Xpert in CT, and one by culture method (Table 2).
Among atypical bacterial infections, mNGS detection rate was lower than that of the CT (50.0% [12/24] vs. 91.7% [22/24], P = 0.003) (Fig. 4D). CT found one case of Legionella pneumophila and one of Chlamydia trachomatis alone. The detection rate of MP using mNGS was lower than that of the CT (52.4% [11/21] vs. 95.2% [20/21], P = 0.004). In addition, 10 cases were positive for both mNGS and CT, one for mNGS alone, and 10 for CT alone. CT included MP-polymerase chain reaction (PCR) detection in 57.1% (12/21), PA detection in 52.4% (11/21), and GICT detection in 14.3% (3/21) (Table 3).
The mixed infection of SCAP
There were 39 (51.3%) cases of mixed infection. CT alone detected 16 (21.1%) cases of mixed infection, and mNGS alone detected 20 (26.3%) cases of mixed infection. However, this difference was not statistically significant (P > 0.005).
Mixed bacterial and viral infections were the most common type, with 12 (30.8%) cases. Eight (20.5%) patients had mixed bacterial and fungal infections and five (12.8%) cases of mixed bacterial and atypical pathogens (Fig. 3B).
Diagnosis consistency between mNGS and CT
A total of 49 (58.3%) cases were positive for both mNGS and CT, 22 (26.2%) for only mNGS, 5 (6.0%) for only CT, and 8 (9.5%) were negative for both CT and mNGS.
Among 49 double-positive cases, mNGS and CT results were completely consistent in 16 (19.0%) patients and completely inconsistent in 14 (16.7%) cases. Nineteen (22.6%) cases were partially consistent, indicating that at least one detected pathogen overlapped between CT and mNGS (Fig. 5).
Changes after the detection of mNGS
There were 26 (31.0%) patients who changed their treatment based on mNGS results, and their symptoms were reduced. Antibiotics were changed in nine patients, antibiotics were added in five patients, antifungal drugs in nine, antivirals in seven, and antituberculosis drugs in one (Table 4).
Discussion
Our study comprehensively evaluated the application of mNGS in children with SCAP. In this study, pathogen detection rate of mNGS was higher than that of the CT (83.3% vs. 63.1%, P = 0.003), especially for S. pneumoniae, H. influenzae, and fungi. There was no significant difference between mNGS and CT in the detection of tuberculosis and virus. However, MP detection rate was lower for mNGS than that for CT (52.4% [11/21] vs. 95.2% [20/21], P = 0.004). In addition, mNGS can detect pathogens that cannot be detected using CT, which is of great significance for the adjustment of antimicrobial therapy.
BALF was used as the sample source in this study because it was collected from infected sites and was less contaminated by oral colonisation bacteria [27, 28]. Regarding bacterial detection, our study found that mNGS had a higher detection rate for S. pneumoniae than that of the CT (89.2% vs. 44.8%, P = 0.001). In a study on children with CAP by Farnaes et al., 6.7% (1/15) of S. pneumoniae were detected by culture and cell-free plasma next-generation sequencing (CFPNGS); pneumococcus was only detected using CFPNGS in the other eight cases [29]. There was another study on invasive pneumococcal disease in 96 children; positive rate of culture method was 27.1% (n = 26), while that of mNGS test was 62.5% (n = 60) (blood, cerebrospinal fluid, and pleural effusion samples) [30]. These findings suggest that when considering S. pneumoniae infection in children with SCAP, mNGS should be actively performed to clarify the aetiology and guide anti-infection treatment. In this study, the detection of S. aureus using mNGS was lower than that of traditional methods (41.7% vs. 83.3%). However, Ren et al.'s study collected noted that mNGS (blood, cerebrospinal fluid, and BALF) was more sensitive than that of the culture method (77.8% vs. 44.4%) in adult patients with sepsis [24]. We utilised both culture and PCR, which may have enhanced the rate of S. aureus identification by conventional methods. This may also be associated with the different immune systems of children and adults.
For Gram-negative bacteria, our study found that the mNGS detection rate was significantly higher than that of the CT, especially for H. influenzae (91.7% vs. 33.3%, P < 0.005). mNGS also had a greater detection rate for P. aeruginosa, K. pneumoniae, and E. coli than that of the CT in our study. The study by Wu et al. on adult SCAP also revealed that the rate of H. influenzae identification using mNGS was higher than that of the conventional detection techniques (100% vs. 33.3%) in BALF [31]. In a study on adult sepsis, Ren et al. discovered that mNGS had a greater detection, n rate of P. aeruginosa and K. pneumoniae than that of the culture method (75.4% vs. 43.5%, 81.6% vs. 26.3%, respectively), using blood, cerebrospinal fluid, and BALF samples [24]. According to the aforementioned study, mNGS should be actively performed whenever Gram-negative bacterial infection is considered. However, a previous study revealed that after paediatric haematopoietic stem cell transplantation, the detection rate of P. aeruginosa and K. pneumoniae using conventional methods is comparable to that of the mNGS using BALF [32]. These differences may be due to the different specimen sources and immune functions.
Regarding virus detection, mNGS showed no difference compared with that of the CT in the detection of ADV, EBV, and influenza A viruses in this study. When children with SCAP caused by the above pathogens are clinically suspected, traditional methods should be considered first for pathogen detection. A previous study showed that mNGS has a low sensitivity for influenza A viruses [33]. Real-time fluorescence quantitative PCR is more sensitive than mNGS for the detection of influenza virus infection in adult SCAP [34]. In another study, mNGS (RNA-SEQ) did not detect any of the eight positive ADV samples for paediatric pneumonia but had high sensitivity to rhinovirus and RSV (100% and 96%, respectively) [35]. The potential of mNGS to identify additional viruses and subtypes that cannot be detected by conventional methods has also been confirmed in previous studies [33, 36]. In contrast, mNGS assisted in identifying cytomegalovirus (CMV) infection and not merely colonisation. In our study, mNGS and CT eventually detected three children with CMV infection, including one patient with congenital heart disease. Based on the findings of the mNGS, two cases were treated with antiviral medications, and the patients were cured. In a study, one child with leukaemia received antiviral treatment after CMV was detected using mNGS, and their symptoms improved [37]. This demonstrates that CMV should be appraised not only based on colonisation but also on the child’s underlying illness and clinical characteristics.
The fungal detection rate of mNGS was significantly higher than that of CT alone. In a study on the detection of fungal pneumonia in adults, the culture method was only used in 1/21 samples, while mNGS was used in 19/21 samples [38]. In a study of children after haematopoietic stem cell transplantation, mNGS (BALF) detected nine cases of fungal pneumonia (Pneumocystis jiroi [n = 6], Aspergillus [n = 2], and mucor [n = 1]), while none was detected using traditional methods [32]. In this study, the positive rate of fungal pneumonia detected using mNGS was 81.8% (9/11), while only 18.2% (2/11) used the traditional pathogen detection method. Among them, 54.5% (6/11) had underlying diseases, including congenital heart disease, primary ciliary dyskinesia, chronic granuloma, pelvic mass, diabetes, and congenital cleft palate. Two kinds of Aspergillus, Aspergillus aspergillus and Aspergillus niger, were also detected using mNGS, but not by traditional methods. Huang et al. also reported that mNGS detected various A. fumigatus, A. niger, A. flavus, and A. oryzae in immunosuppressed adult patients diagnosed with fungal pneumonia [39]. Therefore, mNGS should be actively applied to children with severe pneumonia and underlying diseases or immunodeficiency. In our study, three cases of C. albicans infection were confirmed, and the detection rates of mNGS and CT were similar, among which two cases had underlying diseases. Liu et al. also reported that C. albicans was one of the fungi most frequently detected in BALF cultures [40]. However, another study found that the mNGS detection rate of C. albicans was lower than that of the traditional method (70.6% vs. 82.4%) in ventilators-associated pneumonia in adults [25]. Therefore, traditional methods should be used for pathogen detection in children with C. albicans infection. Interestingly, patient 26 tested negative on mNGS and CT but positive on the 1,3-D glucan test, which combined clinical symptoms and imaging to diagnose fungal infection. Therefore, culture, mNGS, galactomannan (GM) test, and 1, 3-D glucan test should be combined in the diagnosis of fungal pneumonia to avoid missing positive samples.
The detection sensitivity of mNGS for MTB was similar to that of CT in our study. Previous studies have also confirmed that the diagnostic ability of mNGS for MTB is similar to that of the traditional detection methods [41, 42]. Therefore, when clinically considering the presence of MTB infection, traditional methods rather than mNGS should be considered first. MTB, a type of intracellular bacteria, releases less nucleic acid into the extracellular environment, and insufficient wall fracture can also affect the extraction of DNA; therefore, fewer sequences can be detected [43, 44]. mNGS combined with MTB-Xpert can be used to improve diagnostic rates [11, 43].
Surprisingly, we found that mNGS was inferior to CT in the detection of atypical pathogens (50.0% vs. 91.7%), especially for MP (52.4% vs. 95.2%). This has never been mentioned in previous studies. Only studies on children with severe unresponsive pneumonia indicated that mycoplasma detection rates of mNGS and PCR were equal (15.6% vs. 18.8%) [37]. In this study, the detection rate of MP-PCR was 57.1% (12/21), which was similar to that by mNGS. The possible reasons are the combination of PCR and two immunological methods, which increased the sensitivity of the traditional method in this study. Therefore, when considering MP infections in children with SCAP, it is not necessary to conduct mNGS examinations.
The patient received empirical anti-infective medication in the absence of knowledge of its precise aetiology. After identifying the illness' pathogenic microorganisms, 26 people (31.0%) modified their course of treatment according to the mNGS results, and their symptoms improved. In a study of adults with severe respiratory diseases, mNGS led to a change in treatment in 34.4% (11/32) of patients [13]. Combining mNGS with conventional detection technologies can improve the ability to target drug use. On the other hand, the culture process takes at least 3 days [45], while mNGS can obtain test results within 24–48 h [36]. Although PCR is quick, its reach is constrained and may not even detect the causal agent [33]. These results suggest that mNGS is important for the detection and treatment of SCAP in children.
Our study has several limitations. First, the sample size of our study was modest; hence, the number of pathogens identified was limited. Second, because of the high sensitivity of mNGS, pathogens of colonisation and contamination will also be discovered; therefore, there is no universal standard for the report's issuance and interpretation. Finally, because this was a single-centre observational study, a case selection bias may have occurred. Further prospective, multicentre, randomised controlled studies are needed to confirm the sensitivity, specificity, and clinical value of mNGS.
Conclusion
In conclusion, mNGS has its unique advantages in the detection of pathogenic agents of SCAP in children, especially Streptococcus pneumoniae, Haemophilus influenzae and fungi. In addition, mNGS can detect pathogens that cannot be detected by CT, which is of great significance for adjusting antimicrobial therapy.
Availability of data and materials
The raw sequence data reported in this paper have been deposited in the Genome Sequence Archive (Genomics, Proteomics & Bioinformatics 2021) in National Genomics Data Center (Nucleic Acids Res 2022), China National Center for Bioinformation / Beijing Institute of Genomics, Chinese Academy Sciences (GSA: CRA008578) that are publicly accessible at https://ngdc.cncb.ac.cn/gsa.
Abbreviations
- CAP:
-
Community-acquired pneumonia
- SCAP:
-
Severe community-acquired pneumonia
- mNGS:
-
Metagenomic next-generation sequencing
- BALF:
-
Bronchoalveolar lavage fluid
- CT:
-
Conventional technology
- MP:
-
Mycoplasma pneumoniae
- EBV:
-
Epstein–Barr virus
- CMV:
-
Cytomegalovirus
- RSV:
-
Respiratory syncytial virus
- ADV:
-
Adenovirus
- MRSA:
-
Methicillin resistant Staphylococcus aureus
- MTB:
-
Mycobacterium tuberculosis
- PCR:
-
Polymerase chain reaction
- PA:
-
Particle agglutination
- GICT:
-
Immune colloidal gold technigue
References
Principi N, Esposito S. Management of Severe Community-Acquired Pneumonia of Children in Developing and Developed Countries. Thorax (2011) 66(9):815–22. Epub 2010/10/23. doi: https://doi.org/10.1136/thx.2010.142604.
Igor Rudan, Lana Tomaskovic, Cynthia Boschi-Pinto, Harry Campbell on behalf of WHO Child Health Epidemiology Reference Group. Global estimate of the incidence of clinical pneumonia among children under five years of age. Bull World Health Organ (2004) 82(12): 895–903. Epub 2005/01/05.
Cardinale F, Cappiello AR, Mastrototaro MF, Pignatelli M, Esposito S. Community-Acquired Pneumonia in Children. Early Hum Dev (2013) 89 Suppl 3:S49–52. Epub 2013/08/22. doi: https://doi.org/10.1016/j.earlhumdev.2013.07.023.
Bradley JS, Byington CL, Shah SS, Alverson B, Carter ER, Harrison C, et al. The Management of Community-Acquired Pneumonia in Infants and Children Older Than 3 Months of Age: Clinical Practice Guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis (2011) 53(7):e25–76. Epub 2011/09/02. doi: https://doi.org/10.1093/cid/cir531.
Mani CS, Murray DL. Acute Pneumonia and Its Complications. Principles Prac Pediatr Infect Dis. (2012). p. 235–45.e4.
Guo YL, Yang YX, Dong PP. [Pathogens in Bronchoalveolar Lavage Fluid of Children with Lower Respiratory Tract Infection]. Zhongguo Dang Dai Er Ke Za Zhi (2019) 21(2):144–9. Epub 2019/02/21.
Yonghong W, Yajie G, Yuying C, Qi M, Jieqiong L. Evaluation of thermostatic amplification chip in children with lower respiratory tract infectious diseases. Chin J Evid Based Pediatr. 2018;13(3):176–9. https://doi.org/10.3969/j.issn.1673-5501.2018.03.004.
Jain S, Self WH, Wunderink RG, Fakhran S, Balk R, Bramley AM, et al. Community-Acquired Pneumonia Requiring Hospitalization among U.S. Adults. N Engl J Med (2015) 373(5):415–27. Epub 2015/07/15. doi: https://doi.org/10.1056/NEJMoa1500245.
Naomi J Gadsby, Clark D. Russell, Martin P. McHugh, Harriet Mark et al: Comprehensive molecular testing for respiratory pathogens in community acquired pneumonia. Clin Infect Dis (2016) 62(7): 817–823. Epub 2016/01/07. doi: https://doi.org/10.1093/cid/civ1214.
Chen J, Zhao Y, Shang Y, Lin Z, Xu G, Bai B, et al. The Clinical Significance of Simultaneous Detection of Pathogens from Bronchoalveolar Lavage Fluid and Blood Samples by Metagenomic Next-Generation Sequencing in Patients with Severe Pneumonia. J Med Microbiol (2021) 70(1). Epub 2020/11/25. doi: https://doi.org/10.1099/jmm.0.001259.
Zheng Y, Qiu X, Wang T, Zhang J. The Diagnostic Value of Metagenomic Next-Generation Sequencing in Lower Respiratory Tract Infection. Front Cell Infect Microbiol (2021) 11:694756. Epub 2021/09/28. doi: https://doi.org/10.3389/fcimb.2021.694756.
Sun T, Wu X, Cai Y, Zhai T, Huang L, Zhang Y, et al. Metagenomic Next-Generation Sequencing for Pathogenic Diagnosis and Antibiotic Management of Severe Community-Acquired Pneumonia in Immunocompromised Adults. Front Cell Infect Microbiol (2021) 11:661589. Epub 2021/06/19. doi: https://doi.org/10.3389/fcimb.2021.661589.
Li Y, Sun B, Tang X, Liu YL, He HY, Li XY, et al. Application of Metagenomic Next-Generation Sequencing for Bronchoalveolar Lavage Diagnostics in Critically Ill Patients. Eur J Clin Microbiol Infect Dis (2020) 39(2):369–74. Epub 2019/12/10. doi: https://doi.org/10.1007/s10096-019-03734-5.
Simner PJ, Miller S, Carroll KC. Understanding the Promises and Hurdles of Metagenomic Next-Generation Sequencing as a Diagnostic Tool for Infectious Diseases. Clin Infect Dis. 2018;66(5):778–88. https://doi.org/10.1093/cid/cix881.
Peng JM, Du B, Qin HY, Wang Q, Shi Y. Metagenomic Next-Generation Sequencing for the Diagnosis of Suspected Pneumonia in Immunocompromised Patients. J Infect (2021) 82(4):22–7. Epub 2021/02/21. doi: https://doi.org/10.1016/j.jinf.2021.01.029.
Geng S, Mei Q, Zhu C, Fang X, Yang T, Zhang L, et al. Metagenomic Next-Generation Sequencing Technology for Detection of Pathogens in Blood of Critically Ill Patients. Int J Infect Dis. 2021;103:81–7. https://doi.org/10.1016/j.ijid.2020.11.166.
Zhang Y, Cui P, Zhang HC, Wu HL, Ye MZ, Zhu YM, et al. Clinical Application and Evaluation of Metagenomic Next-Generation Sequencing in Suspected Adult Central Nervous System Infection. J Transl Med (2020) 18(1):199. Epub 2020/05/15. doi: https://doi.org/10.1186/s12967-020-02360-6.
Yan G, Liu J, Chen W, Chen Y, Cheng Y, Tao J, et al. Metagenomic Next-Generation Sequencing of Bloodstream Microbial Cell-Free Nucleic Acid in Children with Suspected Sepsis in Pediatric Intensive Care Unit. Front Cell Infect Microbiol (2021) 11:665226. Epub 2021/09/11. doi: https://doi.org/10.3389/fcimb.2021.665226.
Graff K, Dominguez SR, Messacar K. Metagenomic Next-Generation Sequencing for Diagnosis of Pediatric Meningitis and Encephalitis: A Review. J Pediatric Infect Dis Soc (2021) 10(Supplement_4):S78-S87. Epub 2021/12/25. doi: https://doi.org/10.1093/jpids/piab067.
Ramchandar N, Burns J, Coufal NG, Pennock A, Briggs B, Stinnett R, et al. Use of Metagenomic Next-Generation Sequencing to Identify Pathogens in Pediatric Osteoarticular Infections. Open Forum Infect Dis (2021) 8(7):ofab346. Epub 2021/07/30. doi: https://doi.org/10.1093/ofid/ofab346.
Harris M, Clark J, Coote N, Fletcher P, Harnden A, McKean M, et al. British Thoracic Society Guidelines for the Management of Community Acquired Pneumonia in Children: Update 2011. Thorax (2011) 66 Suppl 2:ii1–23. Epub 2011/10/19. doi: https://doi.org/10.1136/thoraxjnl-2011-200598.
Experts Group of Pediatric Respiratory Endoscopy, Talent Exchange Service Center of National Health Commission Endoscopy Committee, Pediatric Section of Chinese Medical Doctor Association, Pediatric Respiratory Endoscopy Committee, Endoscopists Section of Chinese Medical Doctor Association, Pediatric Interventional Respirology Group, Maternal and Pediatric Minimally Invasive Section of Chinese Maternal and Child Health Association, Bronchoscopy Collaboration Subgroup of Respirology Group, Pediatric Section of Chinese Medical Association. Guideline of pediatric flexible bronchoscopy in China. version). Chin J Appl Clin Pediatr. 2018;2018(33):983–9. https://doi.org/10.3760/cma.j.issn.2095-428X.2018.13.006.
Linchuan Laboratory Science Group. Pediatrics Society of Chinese Medical Association: Chinese expert consensus on laboratory diagnosis of mycoplasma pneumoniae respiratory tract infection in children. Chinese journal of Laboratory Medicine. 2019;42(7):507–13. https://doi.org/10.3760/cma.j.issn.1009⁃9158.2019.07.005.
Ren D, Ren C, Yao R, Zhang L, Liang X, Li G, et al. The Microbiological Diagnostic Performance of Metagenomic Next-Generation Sequencing in Patients with Sepsis. BMC Infect Dis (2021) 21(1):1257. Epub 2021/12/18. doi: https://doi.org/10.1186/s12879-021-06934-7.
Fang X, Mei Q, Fan X, Zhu C, Yang T, Zhang L, et al. Diagnostic Value of Metagenomic Next-Generation Sequencing for the Detection of Pathogens in Bronchoalveolar Lavage Fluid in Ventilator-Associated Pneumonia Patients. Front Microbiol (2020) 11:599756. Epub 2020/12/19. doi: https://doi.org/10.3389/fmicb.2020.599756.
Chen Y, Feng W, Ye K, Guo L, Xia H, Guan Y, et al. Application of Metagenomic Next-Generation Sequencing in the Diagnosis of Pulmonary Infectious Pathogens from Bronchoalveolar Lavage Samples. Front Cell Infect Microbiol (2021) 11:541092. Epub 2021/03/30. doi: https://doi.org/10.3389/fcimb.2021.541092.
Lin Y, Wang BX, Zhang NN, Zhang L, Gao ZB, Tian J, et al. Metagenomic Analysis Identified Stenotrophomonas Maltophilia Pneumonia in an Infant Suffering from Unexplained Very Severe Pneumonia. Front Pediatr (2019) 7:380. Epub 2019/10/15. doi: https://doi.org/10.3389/fped.2019.00380.
Takeuchi S, Kawada JI, Horiba K, Okuno Y, Okumura T, Suzuki T, et al. Metagenomic Analysis Using Next-Generation Sequencing of Pathogens in Bronchoalveolar Lavage Fluid from Pediatric Patients with Respiratory Failure. Sci Rep (2019) 9(1):12909. Epub 2019/09/11. doi: https://doi.org/10.1038/s41598-019-49372-x.
Farnaes L, Wilke J, Ryan Loker K, Bradley JS, Cannavino CR, Hong DK, et al. Community-Acquired Pneumonia in Children: Cell-Free Plasma Sequencing for Diagnosis and Management. Diagn Microbiol Infect Dis (2019) 94(2):188–91. Epub 2019/03/02. doi: https://doi.org/10.1016/j.diagmicrobio.2018.12.016.
Guo F, Kang L, Xu M. The Application Value of Metagenomic Next-Generation Sequencing in Children with Invasive Pneumococcal Disease. Transl Pediatr (2021) 10(12):3282–90. Epub 2022/01/25. doi: https://doi.org/10.21037/tp-21-533.
Wu X, Li Y, Zhang M, Li M, Zhang R, Lu X, et al. Etiology of Severe Community-Acquired Pneumonia in Adults Based on Metagenomic Next-Generation Sequencing: A Prospective Multicenter Study. Infect Dis Ther (2020) 9(4):1003–15. Epub 2020/11/11. doi: https://doi.org/10.1007/s40121-020-00353-y.
Qu Y, Ding W, Liu S, Wang X, Wang P, Liu H, et al. Metagenomic Next-Generation Sequencing Vs. Traditional Pathogen Detection in the Diagnosis of Infection after Allogeneic Hematopoietic Stem Cell Transplantation in Children. Front Microbiol (2022) 13:868160. Epub 2022/05/06. doi: https://doi.org/10.3389/fmicb.2022.868160.
Qian YY, Wang HY, Zhou Y, Zhang HC, Zhu YM, Zhou X, et al. Improving Pulmonary Infection Diagnosis with Metagenomic Next Generation Sequencing. Front Cell Infect Microbiol (2020) 10:567615. Epub 2021/02/16. doi: https://doi.org/10.3389/fcimb.2020.567615.
Qu J, Zhang J, Chen Y, Huang Y, Xie Y, Zhou M, et al. Aetiology of Severe Community Acquired Pneumonia in Adults Identified by Combined Detection Methods: A Multi-Centre Prospective Study in China. Emerg Microbes Infect (2022) 11(1):556–66. Epub 2022/01/28. doi: https://doi.org/10.1080/22221751.2022.2035194.
Schlaberg R, Queen K, Simmon K, Tardif K, Stockmann C, Flygare S, et al. Viral Pathogen Detection by Metagenomics and Pan-Viral Group Polymerase Chain Reaction in Children with Pneumonia Lacking Identifiable Etiology. J Infect Dis (2017) 215(9):1407–15. Epub 2017/04/04. doi: https://doi.org/10.1093/infdis/jix148.
Shen H, Shen D, Song H, Wu X, Xu C, Su G, et al. Clinical Assessment of the Utility of Metagenomic Next-Generation Sequencing in Pediatric Patients of Hematology Department. Int J Lab Hematol (2021) 43(2):244–9. Epub 2020/10/26. doi: https://doi.org/10.1111/ijlh.13370.
Wang H, Lu Z, Bao Y, Yang Y, de Groot R, Dai W, et al. Clinical Diagnostic Application of Metagenomic Next-Generation Sequencing in Children with Severe Nonresponding Pneumonia. PLoS One (2020) 15(6):e0232610. Epub 2020/06/05. doi: https://doi.org/10.1371/journal.pone.0232610.
Wang Q, Wu B, Yang D, Yang C, Jin Z, Cao J, et al. Optimal Specimen Type for Accurate Diagnosis of Infectious Peripheral Pulmonary Lesions by Mngs. BMC Pulm Med (2020) 20(1):268. Epub 2020/10/17. doi: https://doi.org/10.1186/s12890-020-01298-1.
Huang J, Jiang E, Yang D, Wei J, Zhao M, Feng J, et al. Metagenomic Next-Generation Sequencing Versus Traditional Pathogen Detection in the Diagnosis of Peripheral Pulmonary Infectious Lesions. Infect Drug Resist (2020) 13:567–76. Epub 2020/02/29. doi: https://doi.org/10.2147/IDR.S235182.
Liu H, Zhang Y, Chen G, Sun S, Wang J, Chen F, et al. Diagnostic Significance of Metagenomic Next-Generation Sequencing for Community-Acquired Pneumonia in Southern China. Front Med (Lausanne) (2022) 9:807174. Epub 2022/03/05. doi: https://doi.org/10.3389/fmed.2022.807174.
Tang W, Zhang Y, Luo C, Zhou L, Zhang Z, Tang X, et al. Clinical Application of Metagenomic Next-Generation Sequencing for Suspected Infections in Patients with Primary Immunodeficiency Disease. Front Immunol (2021) 12:696403. Epub 2021/09/07. doi: https://doi.org/10.3389/fimmu.2021.696403.
Shi CL, Han P, Tang PJ, Chen MM, Ye ZJ, Wu MY, et al. Clinical Metagenomic Sequencing for Diagnosis of Pulmonary Tuberculosis. J Infect (2020) 81(4):567–74. Epub 2020/08/10. doi: https://doi.org/10.1016/j.jinf.2020.08.004.
Ye Y, Yang N, Zhou J, Qian G, Chu J. Case Report: Metagenomic Next-Generation Sequencing in Diagnosis of Disseminated Tuberculosis of an Immunocompetent Patient. Front Med (Lausanne) (2021) 8:687984. Epub 2021/07/30. doi: https://doi.org/10.3389/fmed.2021.687984.
Chen Y, Yan X, Li N, Zhang Q, Lv Y, Ruan T. Metagenomic Next-Generation Sequencing of Radial Ultrasound Bronchoscopy-Guided "Cocktail" Specimens as an Efficient Method for the Diagnosis of Focal Pulmonary Infections: A Randomised Study. Ann Palliat Med (2021) 10(2):2080–8. Epub 2021/03/18. doi: https://doi.org/10.21037/apm-20-2578.
Miao Q, Ma Y, Wang Q, Pan J, Zhang Y, Jin W, et al. Microbiological Diagnostic Performance of Metagenomic Next-Generation Sequencing When Applied to Clinical Practice. Clin Infect Dis (2018) 67(suppl_2):S231-S40. Epub 2018/11/14. doi: https://doi.org/10.1093/cid/ciy693.
Acknowledgements
The authors wish to thank the patients and participating investigators and staff associatied with the cilinical studies discussed here.
Funding
This work was supported by The general program of Tianjin Natural Science Foundation[Grant number21JCYBJC00460], General project of Tianjin Children’s Hospital[Grant numberY2020013], Tianjin Health Commission(grant number TJWJ2021QN054), Tianjin Science and Technology Committee, China International Medical Foundation (grant number Z-2019–41-2101–04) and the Program of Tianjin Science and Technology talent cultivation [Grant number RC20020]. We are grateful for the financial support from the "Tianjin Medical Key Discipline (Specialist) Construction Project".
Author information
Authors and Affiliations
Contributions
All authors contributed to the intellectual content of this manuscript and approved the final manuscript as submitted. YW and ZT conceived the design of the article. YX and ZJ provided administrative support. ZJH provided the study patients. YM completed the data collection and assembly. JY searched the literature. All authors contributed to the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the Tianjin Children’s Hospital (No. L2020-02) and individual consent for this retrospective analysis was waived.
Consent for publication
Not applicable.
Competing interest
All authors have completed the ICMJE uniform disclosure form. The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wei, Y., Zhang, T., Ma, Y. et al. Clinical Evaluation of Metagenomic Next-Generation Sequencing for the detection of pathogens in BALF in severe community acquired pneumonia. Ital J Pediatr 49, 25 (2023). https://doi.org/10.1186/s13052-023-01431-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13052-023-01431-w