Abstract
Background
Providing appropriate care at birth remains a crucial strategy for reducing neonatal mortality and morbidity. We aimed to evaluate the consistency of practice and the adherence to the international guidelines on neonatal resuscitation in level-I and level-II Italian birth hospitals.
Methods
This was a cross-sectional electronic survey. A 91-item questionnaire focusing on current delivery room practices in neonatal resuscitation was sent to the directors of 418 Italian neonatal facilities.
Results
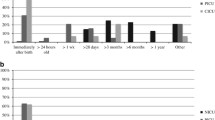
The response rate was 61.7% (258/418), comprising 95.6% (110/115) from level-II and 49.0% (148/303) from level-I centres. In 2018, approximately 300,000 births occurred at the participating hospitals, with a median of 1664 births/centre in level-II and 737 births/centre in level-I hospitals. Participating level-II hospitals provided nasal-CPAP and/or high-flow nasal cannulae (100%), mechanical ventilation (99.1%), HFOV (71.0%), inhaled nitric oxide (80.0%), therapeutic hypothermia (76.4%), and extracorporeal membrane oxygenation ECMO (8.2%). Nasal-CPAP and/or high-flow nasal cannulae and mechanical ventilation were available in 77.7 and 21.6% of the level-I centres, respectively. Multidisciplinary antenatal counselling was routinely offered to parents at 90.0% (90) of level-II hospitals, and 57.4% (85) of level-I hospitals (p < 0.001). Laryngeal masks were available in more than 90% of participating hospitals while an end-tidal CO2 detector was available in only 20%. Significant differences between level-II and level-I centres were found in the composition of resuscitation teams for high-risk deliveries, team briefings before resuscitation, providers qualified with full resuscitation skills, self-confidence, and use of sodium bicarbonate.
Conclusions
This survey provides insight into neonatal resuscitation practices in a large sample of Italian hospitals. Overall, adherence to international guidelines on neonatal resuscitation was high, but differences in practice between the participating centres and the guidelines exist. Clinicians and stakeholders should consider this information when allocating resources and planning perinatal programs in Italy.
Similar content being viewed by others
Introduction
Approximately 5–10% of all newborns need support for transition to initiate breathing and aerate the lungs, while less than 1% require advanced resuscitation at birth, including tracheal intubation, chest compressions, and medications [1,2,3]. Inadequate cardiorespiratory support at birth may result in pulmonary damage and worsen ongoing hypoxia or ischemia, with the risk of aggravating patient outcomes [2, 3]. To improve resuscitation practices worldwide, the International Liaison Committee on Resuscitation (ILCOR) promulgates and regularly updates through rigorous and continuous review of scientific literature the consensus on both the science of neonatal resuscitation and recommendations for treatment. These updates have formed a basis from which individual countries drew up their own guidelines. Of these, the guidelines drawn up by the American Academy of Pediatrics (AAP)/American Heart Association (AHA) are notable and were adopted by the Italian Society of Neonatology (SIN) and its Task Force on Neonatal Resuscitation since 1994. To improve compliance with the guidelines and to promote adequate knowledge of newborn life support, SIN has invested heavily in neonatal resuscitation training sessions for national instructors, national and on-site neonatal resuscitation courses for practitioners and meetings and congresses on the topic.
Issuing and disseminating recommendations is, however, not sufficient, so we set out to evaluate the degree of uptake of these recommendations. Therefore, the aim of our study was to assess the adherence to Neonatal Resuscitation Guidelines in Italian centres, and to compare the consistency of practice between level-I and level-II centres with the hope that the results of our study would help to shape the strategies for diffusion of the current guidelines according to actual needs.
Methods
This cross-sectional study was conducted as an electronic, web-based survey involving all Italian birth centres. According to the 2021 Italian standards of perinatal care [4], level-I centres take care of low- and medium-risk pregnancies and assist both healthy newborns and infants with intermediate diseases. Centres with 500–999 births/year can admit infants with GA ≥36 weeks and BW ≥1900 g, while centres with ≥1000 births/year can admit infants with GA ≥34 weeks and BW ≥1750 g, if the weight is adequate for GA (> 10° centile and < 90° centile). However, at the time of the survey, Italian level-I units admitted infants with GA ≥34 weeks, and some of them infants with GA ≥32 weeks. Level-II centres, in addition to the first level of care, are responsible for high-risk pregnancies and assist newborn infants with complex pathologies in neonatal intensive-care beds.
This Italian survey is part of a European survey on delivery room practices endorsed by the Union of European Neonatal and Perinatal Societies (UENPS) and SIN [5]. The study was approved by the Padua Provincial Institutional Review Board and was declared not to be human subject research.
The survey was anonymous and sent to the directors of all Italian birth centres between January and September 2020 by e-mail link (www.surveymonkey.com). A reminder was sent to non-responders every 2 weeks for a maximum of three times; if no answer was received, we contacted the participant by phone. The participant was considered a non-responder if no response was obtained after the phone call.
The survey consisted of a 91-item questionnaire focusing on current Delivery Room (DR) practices of neonatal resuscitation [6]. It was broken down into the following sections: a) epidemiological data, b) perinatal organization, c) equipment, d) procedures, e) ethics, and f) education. The questionnaire was prepared by a committee of experts in neonatal resuscitation and members of the SIN Task Force on Neonatal Resuscitation. The questions included multiple-choice, fill-in, and yes/no questions (the complete questionnaire can be consulted in the supplementary materials).
Statistical analysis
All returned questionnaires were reviewed by two researchers working separately to avoid duplication of data. Data were examined with descriptive analyses. Categorical data were expressed as numbers and percentages and continuous data as median and interquartile ranges (IQR). In the analysis, level-I and level-II centres were compared using χ2 tests. Statistical analysis was performed using Stata 15 Statistical Package (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC).
Results
In total, 418 neonatologists and paediatricians identified as directors of birth centres were invited to participate in the survey. The overall response rate to the questionnaire was 61.7% (258/418), 95.6% (110/115) for level-II centres and 49.0% (148/303) for level-I centres. Missing values to individual questions were always < 10%, except in 1 question (see text and tables). Of the participating centres, 49 (11.7%) were academic hospitals. Among these, 43 (39.1%) were level-II centres and 6 (4.0%) were level-I centres.
In 2018, approximately 300,000 births occurred at the participating hospitals (about 70% of all Italian births). The median of births/centre was 1664 (IQR: 1250-2391) at level-II and 737 (IQR: 525–1035) at level-I centres. The main results of the survey are reported in Tables 1, 2, 3, 4 and 5, broken down by questionnaire section. Participating level-II hospitals were able to provide nasal-CPAP and/or high-flow nasal cannulae (100%), mechanical ventilation (99.1%), HFOV (71.0%), inhaled nitric oxide (80.0%), therapeutic hypothermia (76.4%), and ECMO (8.2%). Nasal-CPAP and/or high-flow nasal cannulae and mechanical ventilation were available in 77.7 and 21.6% of the level-I centres, respectively. In 74.5% of the level-II centres, the lowest GA of assisted infants was 22–23 weeks, while among level-I centres the lowest GA of assisted infants was 32 weeks in 20.6% and 34 weeks in 53.9%.
Multidisciplinary antenatal counselling was routinely offered to parents at 90.0% (90) of level-II hospitals, and 57.4% (85) of level-I hospitals (p < 0.001). A neonatologist or paediatrician was required to attend all deliveries in about 60% of centres at each level.
Significant differences between level-II and level-I centres were found mainly in antenatal counselling, composition of the resuscitation team for high-risk deliveries, team briefings before resuscitation, providers qualified with full resuscitation skills and role of the anaesthesiologist (Table 1), lack of awareness about temperature (Table 3), routine tracheal suction for non-vigorous neonates born through meconium-stained amniotic fluid, self-confidence, sodium bicarbonate use (Table 4) and frequency of neonatal resuscitation courses (Table 5).
Discussion
Overall, our survey documents good compliance with international guidelines on neonatal resuscitation in most Italian level-II and level-I centres. However, as expected, there are some differences, mostly in perinatal care.
Before birth
A lower number of births/centre and less complexity in the assisted cases account for the differences in how the levels approach the period ‘before birth’. Indeed, before delivering a very preterm infant or an infant with anticipated problems, counselling with parents is routinely performed more often at level-II centres, which expect to assist the most vulnerable newborn infants. For the same reason, paediatricians and neonatologists working in level-I hospitals are less trained for emergencies, so an anaesthesiologist is more frequently needed on the resuscitation team.
Umbilical cord management
Delaying cord clamping (DCC) at birth is associated with increased haemoglobin levels and better iron stores in newborn infants [7]; it favours the cardiovascular transition that occurs in the first minutes of life [8, 9] and decreases mortality among infants with GA < 37 weeks [10]. Delayed or physiologically based cord clamping (i.e. aerating the lung before removing placental support) is provided to most vaginally delivered term infants, suggesting that these interventions were introduced in Italy after umbilical cord management recommendations were disseminated [11]. However, in term elective caesarean section, delayed strategies decrease to 67.2% in level-II and 52.7% in level-I hospitals, indicating the need to implement umbilical cord management for these otherwise healthy newborn infants. As suggested by recent evidence, delaying cord clamping does not affect maternal blood losses [12, 13].
Temperature
A high incidence of postnatal hypothermia has been reported in high- and low-resource countries. It remains an independent predictor of neonatal morbidity and mortality, especially in very preterm infants in all settings. The International Guidelines suggest that the temperature of newly born infants should be maintained between 36.5 and 37.5 °C after birth through admission and stabilization [2, 3]. Effective interventions to achieve this may include environmental temperature 23–25 °C, use of radiant warmers, exothermic mattresses, woollen or plastic caps, plastic wraps, humidified and heated gases [14]. According to our survey, neonatologists in level-I centres are less aware than those in level-II of the importance of keeping the delivery room and operating room temperatures within the suggested ranges as part of the effective interventions to prevent thermal losses at birth.
It is well known that therapeutic hypothermia should be started within the first 6 h of life for newborn infants at risk of hypoxic-ischemic encephalopathy [15]. We observed good compliance with this practice in all Italian birth centres, in most of which ‘passive cooling’ is started within 1 h of life.
Airways, ventilation, circulation and medications
Since 2015, the International Guidelines have recommended against routine endotracheal suctioning of meconium-stained non-vigorous newborns, instead suggesting resuscitation with positive pressure ventilation. Our survey showed that both level-II and level-I centres had changed their practice accordingly; however, in level-II centres, routine tracheal suction is still performed more often, reflecting a greater confidence with the intubation manoeuvre.
Effective ventilation is considered the most critical intervention for successful delivery room resuscitation [16]. Most perinatal management of this aspect is comparable between birth centres, especially in the use of a ‘gentle’ approach to ventilation. In both level-II and level-I hospitals, a T-piece is preferred to a self-inflating bag to administer positive pressure ventilation (PPV), predominantly using a face mask as the first interface. However, in 12% of level-II centres, short binasal prongs are the first choice. This solution seems to offer some advantages over face masks in terms of reducing intubation in the delivery room [17,18,19].
An air-oxygen blender and a pulse oximeter to guide oxygen titration are available in almost all Italian delivery rooms. Moreover, as recommended by the International Guidelines, a laryngeal mask is part of the equipment in more than 90% of the participating hospitals, to be used in the event of failure of face mask ventilation or intubation [2, 3]. On the other hand, an end-tidal CO2 detector, which is considered the most reliable tool to identify the correct placement of the endotracheal tube [20], is only available in about 20% of the responding birth centres. This device could potentially decrease the number of intubation attempts and improve outcomes [21, 22]. Among technical aspects, fewer level-I neonatal resuscitation teams self-evaluated as excellent or good at performing the endotracheal intubation manoeuvre. By contrast, this is a well-acquired skill by level-II teams, who are expected to assist the most vulnerable newborn infants routinely.
Since 2015, electrocardiography is recognized as an important adjunct for babies requiring resuscitation. Nevertheless, a 3-lead ECG Monitor is only available in a quarter of responding centres, showing limited adherence to the latest version of the guidelines, which recommend its use in infants needing advanced resuscitation [2, 3].
Finally, although sodium bicarbonate is no longer considered helpful during acute resuscitation [23], it is still used on occasion, especially in level-I centres.
Ethics and education
Our survey shows that awareness of ethical issues should be reinforced in Italy. Indeed, a difficult decision like the time-limit before stopping full resuscitation in severely asphyxiated infants is not supported by shared guidelines in about 50% of responding hospitals. Moreover, parents are involved in the decision-making process of resuscitation in only one third of Italian centres. These findings are in line with previous European studies [24, 25]. Ethics remains a delicate field that needs further research to help neonatal staff and parents deal with difficult situations.
Courses on neonatal resuscitation are routinely held in more than 80% of Italian birth centres, and most of these follow the American or European guidelines. Frequency of retraining is also optimal in about 80% of centres, according to the 2020 recommendations, suggesting that among participants who have been trained in neonatal resuscitation, individual or team booster-training should occur more frequently than every 2 years in order to support retention of knowledge, skills, and behaviour.
Strengths and limitations
The strengths of the present study include the structured questionnaire prepared by a group of experts; the assessment of several areas of neonatal resuscitation; the high representativity of the sample, which accounts for about 70% of all Italian deliveries in 2018; and finally, the use of an online survey.
This study has some limitations, starting from the consideration that conducting surveys in an online format runs the risk of selection bias [26]. The response rate is at the same time a strength for level-II hospitals and a limitation for those at level-I. The limited response rate (49.0%) of level-I centres may restrict the generalizability of our findings. Finally, as only the directors of neonatal wards were involved, the results may mirror the opinions of this very restricted group of clinicians; nevertheless, the questionnaire was structured to limit this risk.
Conclusions
This survey provides insight into neonatal resuscitation practices in a large sample of Italian hospitals. Overall, adherence to the International Guidelines on neonatal resuscitation was high, but we also saw some divergences in practice, ethical choices, and training among the participating centres. Clinicians and stakeholders should consider this information when allocating resources and planning Italian perinatal programmes. The areas of the current guidelines that require further implementation include aspects of perinatal care, respiratory support, ethics and training. This goal can be achieved by defining new educational strategies, including quality improvement projects, simulation-based training and interventions in communication technology.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SIN:
-
Società Italiana di Neonatologia (Italian Society of Neonatology)
- UENPS:
-
Union of European Neonatal and Perinatal Societies
- HFOV:
-
High-frequency oscillatory ventilation
- ECMO:
-
Extracorporeal membrane oxygenation
- ILCOR:
-
International Liaison Committee on Resuscitation
- AAP:
-
American Academy of Pediatrics
- AHA:
-
American Heart Association
- GA:
-
Gestational Age
- BW:
-
Birth Weight
- IQR:
-
Interquartile Range
- PPV:
-
Positive pressure ventilation
References
Aziz K, Lee HC, Escobedo MB, Hoover AV, Kamath-Rayne BD, Kapadia VS, et al. Part 5: Neonatal Resuscitation: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142(16_suppl_2):S524–50.
Wyckoff MH, Wyllie J, Aziz K, de Almeida MF, Fabres JW, Fawke J, et al. International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2020;156:A156–87.
Madar J, Roehr CC, Ainsworth S, Ersdal H, Morley C, Rüdiger M, et al. European resuscitation council guidelines 2021: newborn resuscitation and support of transition of infants at birth. Resuscitation. 2021;161:291–326.
Baronciani D, Bellù R, Franchi M, et al. Obiettivi di sistema, modello organizzativo generale e standards organizzativi per la rete di assistenza alla madre ed al neonato. In: IdeaCpa Editore. Standards organizzativi per l’assistenza perinatale. Rome: Yoo Print s.r.l. - Gessate (MI); 2021. p. 46–102.
Trevisanuto D, Gizzi C, Gagliardi L, et al. Neonatal Resuscitation Practices in Europe: A Survey of the Union of European Neonatal and Perinatal Societies. Neonatology. 2022;20:1–9.
Trevisanuto D, Satariano I, Doglioni N, Criscoli G, Cavallin F, Gizzi C, et al. Neonatal resuscitation study group, Italian Society of Neonatology. Changes over time in delivery room management of extremely low birth weight infants in Italy. Resuscitation. 2014;85:1072–6.
McDonald SJ, Middleton P, Dowswell T, Morris PS. Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes. Cochrane Database Syst Rev. 2013;11:CD004074.
Hooper SB, Te Pas AB, Lang J, van Vonderen JJ, Roehr CC, Kluckow M, et al. Cardiovascular transition at birth: a physiological sequence. Pediatr Res. 2015;77:608–14.
Bhatt S, Alison BJ, Wallace EM, Crossley KJ, Gill AW, Kluckow M, et al. Delaying cord clamping until ventilation onset improves cardiovascular function at birth in preterm lambs. J Physiol. 2013;591:2113–26.
Fogarty M, Osborn DA, Askie L, Seidler AL, Hunter K, Lui K, et al. Delayed vs early umbilical cord clamping for preterm infants: a systematic review and meta-analysis. Am J Obstet Gynecol. 2018;218:1–18.
Ghirardello S, Cinotti A, Di Tommaso M, et al. Raccomandazioni italiane per la gestione del clampaggio ed il milking del cordone ombelicale nel neonato a termine e pretermine. www.neonatologia.it/Raccomandazioni
Cavallin F, Galeazzo B, Loretelli V, Madella S, et al. Delayed cord clamping versus early cord clamping in elective cesarean section: A randomized controlled trial. Neonatology. 2019;116:252–9.
Purisch SE, Ananth CV, Arditi B, Mauney L, Ajemian B, et al. Effect of delayed vs immediate umbilical cord clamping on maternal blood loss in term cesarean delivery: A randomized clinical trial. JAMA. 2019;322:1869–76.
Trevisanuto D, Testoni D, de Almeida MFB. Maintaining normothermia: why and how? Semin Fetal Neonatal Med. 2018;23:333–9.
Wassink G, Davidson JO, Dhillon SK, et al. Therapeutic hypothermia in neonatal hypoxic-ischemic encephalopathy. Curr Neurol Neurosci Rep. 2019;19:2.
Foglia EE, Te Pas AB. Effective ventilation: the most critical intervention for successful delivery room resuscitation. Semin Fetal Neonatal Med. 2018;23:340–6.
Biniwale M, Wertheimer F. Decrease in delivery room intubation rates after use of nasal intermittent positive pressure ventilation in the delivery room for resuscitation of very low birth weight infants. Resuscitation. 2017;116:33–8.
Petrillo F, Valenzano L, Franco C, et al. Pulmonary Recruitment Strategy in Preterm Neonates < 29 Weeks of Gestational Age to Reduce the Need for Intubation in the Delivery Room. Am J Perinatol. 2019;36(S 02):S115–9.
Donaldsson S, Drevhammar T, Li Y, Bartocci M, et al. Comparison of Respiratory Support After Delivery in Infants Born Before 28 Weeks’ Gestational Age: The CORSAD Randomized Clinical Trial. JAMA Pediatr. 2021. https://doi.org/10.1001/jamapediatrics.2021.1497 Online ahead of print.
Weiner GM, Zaichkin J, Kattwinkel J, Ades A. In: Weiner GM, Zaichkin J, Kattwinkel J, Ades A, editors. Textbook of neonatal resuscitation. 8th ed. Illinois: Elk Grove Village; 2021.
Sauer CW, Kong JY, Vaucher YE, et al. Intubation attempts increase the risk for severe intraventricular hemorrhage in preterm infants-A retrospective cohort study. J Pediatr. 2016;177:108–13.
Debay A, Patel S, Wintermark P, et al. Association of Delivery Room and Neonatal Intensive Care Unit Intubation, and number of tracheal intubation attempts with death or severe neurological injury among preterm infants. Am J Perinatol. 2020. https://doi.org/10.1055/s-0040-1718577 Online ahead of print.
Kapadia VS, Wyckoff MH. Drugs during delivery room resuscitation--what, when and why. Semin Fetal Neonatal Med. 2013;18:357–61.
Cuttini M, Nadai M, Kaminski M, et al. End-of-life decisions in neonatal intensive care: physicians’ self-reported practices in seven European countries. EURONIC Study Group. Lancet. 2000;355:2112–8.
Rebagliato M, Cuttini M, Broggin L, et al. EURONIC study group (European project on Parents’ information and ethical decision making in neonatal intensive care units). Neonatal end-of-life decision making: Physicians’ attitudes and relationship with self-reported practices in 10 European countries. JAMA. 2000;284:2451–9.
Blumenberg C, Barros AJD. Response rate differences between web and alternative data collection methods for public health research: a systematic review of the literature. Int J Public Health. 2018;63:765–73.
Acknowledgements
We thank the Directors of level-I and level-II Italian birth hospitals who participated in the survey (listed in Supplementary files) for their contribution. We are also grateful to David Nicholson for his English language editing service.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
CG contributed to the study concept, preparation of the survey, wrote the initial draft and critically reviewed the manuscript. DT contributed to the study concept, preparation of the survey, writing of the manuscript and critically reviewed the manuscript. LG contributed to the study concept, data analysis, writing of the manuscript and critically reviewed the manuscript. GV coordinated the contacts among participating centres, contributed to the study concept, data curation, writing the draft of the manuscript and critically reviewed the manuscript. SG contributed to the study concept, data curation, writing the draft of the manuscript and critically reviewed the manuscript. SDF contributed to the study concept, data curation, writing the draft of the manuscript and critically reviewed the manuscript. CM contributed to the study concept and to writing the draft of the manuscript, provided relevant expertise, and critically reviewed the manuscript. FM contributed to the study concept and to writing the draft of the manuscript, provided relevant expertise, and critically reviewed the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The approval for this study was obtained by the Padua Provincial Institutional Review Board (Protocol # 0035420) and was declared not to be human subject research.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interest regarding the publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary file 1.
PDF Questionnaire, complete survey questionnaire.
Additional file 2: Supplementary file 2.
List of participating centres, complete list of participating centres.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gizzi, C., Trevisanuto, D., Gagliardi, L. et al. Neonatal resuscitation practices in Italy: a survey of the Italian Society of Neonatology (SIN) and the Union of European Neonatal and Perinatal Societies (UENPS). Ital J Pediatr 48, 81 (2022). https://doi.org/10.1186/s13052-022-01260-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13052-022-01260-3