Abstract
Background
Neonatal sepsis is one of the leading causes of neonatal morbidity and mortality. Despite implementing of different preventive interventions, the burden of neonatal sepsis is reporting in different areas of Ethiopia. For further interventions, identifying its determinants is found to be crucial.
Objective
This study aimed to identify determinants of neonatal sepsis in the Northwest part of Ethiopia.
Methods
Unmatched case-control study was conducted among 246 neonates admitted in neonatal intensive care unit, Northwest Ethiopia. Study participants were selected from February 1st to March 30th 2018. Data was collected through face to face interview and review of neonates’ medical records using pretested structured questionnaire. Data was entered into Epi Data version 4.2.0.0 and further transferred to SPSS statistical software version 25 for analysis. All independent variables with p-value < 0.25 in Bivariable analysis were entered into multivariable logistic regression analysis. Finally, variables with p-value < 0.05 were considered as determinants of neonatal sepsis.
Results
A total of 82 cases and 164 controls were included in this study. Neonates with gestational age < 37 weeks [AOR = 6.90; 95% CI (2.76, 17.28)], premature rupture of membrane [AOR = 2.81; 95% CI (1.01, 7.79)], not crying immediately at birth and have received resuscitation at birth [AOR = 2.85; 95% CI (1.09, 7.47)] were found to be predictors of neonatal sepsis.
Conclusions and recommendations
Premature rupture of membrane was found to be obstetric-related determinant of neonatal sepsis. Gestational age < 37 weeks, not crying immediately at birth, and have received resuscitation at birth were found to be neonatal-related risk factors of neonatal sepsis. Infection prevention strategies need to be strengthening and/or implementing by providing especial attention for the specified determinants.
Similar content being viewed by others
Background
Globally, each year over 2.5 million neonates died within the first month of life in 2017. It accounts for two-thirds of deaths of infants and nearly two-fifths of all deaths in under-five children. Most of the neonatal deaths occur in low-and middle-income countries [1]. Neonatal sepsis is a major cause of neonatal morbidity and mortality in developing countries [2]. It is highly prevalent in sub-Saharan Africa, south Asia, and Latin America with case fatality risk of 9.8% in the first month of life [3]. Septicemia, meningitis, pneumonia, arthritis, osteomyelitis, and urinary tract infections [4, 5] are some of the prior causes of sepsis.
Improving maternal health and nutrition [6], maternal immunization [7], clean delivery, intra-partum antibiotic prophylaxis, intravenous central line management, clean umbilical cord cutting, early detection and treatment of infectious disease, closed medication system [8,9,10], improvements perinatal care services, and producing trained health professionals, like skill birth attendants and neonatal nurses [11, 12] are implementing approaches to prevent neonatal sepsis.
In spite of those approaches, premature rupture of membrane (PROM), medical and surgical problems of mothers [13,14,15], history of maternal urinary tract infection or sexually transmitted infection, presence of intra-partum fever, gestational age < 37 weeks, APGAR score < 7 at 5th minute, need for artificial ventilation, not crying immediately at birth [16, 17], delay in care seeking, and lack of access to well-trained health workers [18, 19] are identified to be contributing factors of neonatal sepsis from previous studies. In the involvement of different determinants, the prevalence of neonatal sepsis from primary studies is reported frequently in different countries, including Ethiopia. Notably, in Shashemene Ethiopia showed 77.9% [20]; 29.3% in Kenya [21], 24% in Dar es SalaamTanzania [22], and 35.1% in Mandya, Karnataka, India [23].
To prevent further this neonatal problem and to achieve sustainable development goal by reducing neonatal mortality, data from different geographical area of Ethiopia is required. Therefore, identifying the predictors of neonatal sepsis is indicated which is helpful in designing strategies to prevent and/or treat neonatal sepsis.
Objective
This study aimed to identify determinants of neonatal sepsis in the Northwest part of Ethiopia.
Methods
Study design, period, setting, and population
An institution based unmatched case-control study was conducted at Debre Markos Referral Hospital, Northwest Ethiopia from February 1st to March 30th 2018. The town is 299 km far from Addis Ababa, capital city of Ethiopia. This hospital has more than 193 bed capacity and it serves to more than 2,153,937 populations in its catchment area in the Northwest part of Ethiopia. All neonates who were admitted in neonatal intensive care unit (NICU) were the source population. Besides, all neonates who were admitted in NICU during the study period were the study population. Mothers who had hearing impairments or unable to talk, abandoned neonates who were admitted in the hospital, and neonates whose cards had incomplete information were excluded from the study in both controls and cases.
Variables
Dependent variable: Neonatal sepsis.
Independent Variables: Socio-demographic characteristics of neonates and parents (age of the neonate, sex of the neonate, religion, ethnicity, maternal age, marital status of the parents, family educational status, family occupation, family size, and place of residence), maternal factors (gravidity, parity, complication during pregnancy and delivery, place of delivery, mode of delivery, PROM, duration of labour, and ANC follow-up) and neonatal factors (birth weight, gestational age, birth asphyxia, APGAR score) were the hypothesized determinants.
Operational definitions
Case (Neonatal sepsis): The established Integrated Management of Neonatal and Childhood Illness (IMNCI) clinical features, includes the presence of two or more of persistent fever (≥37.5 °C) or persistent hypothermia (≤35.5 °C) for more than one hour, fast breathing (≥60 breath per minute), severe chest in drawing, grunting, not feeding well, movement only when stimulated, bulged fontanel, convulsion, lethargic or unconsciousness along with ≥2 of the hematological criteria such as total leukocyte count (< 4000 or > 12,000 cells/mm3), absolute neutrophil count (< 1500 cells/mm3 or > 7500 cells/mm3), platelet count (< 150 or > 450 cells/mm3), and random blood sugar (< 40 mg/dl or > 125 mg/dl) were used to diagnose neonatal sepsis cases.
Control: neonates with the diagnosis of non-sepsis case with their index mother.
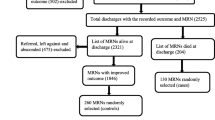
Sample size determination and sampling procedure
Sample size was determined using the Epi Info Version 3.5.1 software with the following assumptions: Two-sided confidence level (CI) =95%, Power = 80%, Ratio of controls to cases = 2:1, and from a case-control study conducted on risk factors for neonatal sepsis in public hospitals, Northern Ethiopia [16]. Then, the final sample size was 246 (82 Cases and 164 Controls).
Both cases (diagnosed with sepsis) and controls (not diagnosed with sepsis) were selected through consecutive sampling technique from the neonates who were admitted in NICU until the required sample size was reached.
Data collection method and procedure
Data were collected through interviewing mothers and reviewing neonates’ medical records using checklist and structured data abstraction sheet. The abstraction sheet includes maternal sociodemographic, maternal obstetric and gynecological, prenatal, intranatal, and neonatal variables. The data was from February 1st to March 30th 2018. The data was collected by 3 BSc nurses and 1 BSc nurse supervisor.
Data quality control
Pretest was done on 5% of the sample size. Training was given for data collectors and supervisor about data collection tool and data collection procedure. Data collection tool was prepared in English and translated to the national language (Amharic) and then back to English. Completeness of each abstraction sheet had been checked by the principal investigator and the supervisor in a daily base. Double data entry was done by two data clerks and consistency of the entered data was cross-checked.
Data processing and analysis
Data was coded and entered into Epi-data Version 4.2.0.0 and then exported into SPSS version 25 for analysis. Descriptive statistics were carried out in texts and tables. Bivariable analysis was done and all variables with p-value < 0.25 were entered into the multivariable logistic regression. Variables with p-value < 0.05 were considered as determinants of neonatal sepsis.
Ethical considerations
The study protocol was approved by research ethics and approval committee of Debre Markos University Health Science College. Official letter was written to Debre Markos Referral Hospital. Respondents/guardians had got information on the purpose of the study, its procedures, and their right to refuse or decline participation in the study at any time. Both written and verbal consent were obtained from the study participants/guardians. Confidentiality was also assured.
Results
Socio-demographic characteristics of the mothers and neonates
A total of 82 neonates who had sepsis (cases) with their index mothers and 164 neonates who had no sepsis (controls) with their index mothers were included. The median age of mothers of neonates with sepsis was 25 years and 28 years for controls. More than half (58.5%) of cases and 39% controls were living in rural area. Regarding to marital status, 95.1% cases’ mothers and 98.2% of controls’ mothers were married. Nearly half (48.8%) of cases’ and 40.2% of controls’ mothers were farmers by occupation and 48.8% cases’ and 38.4% of controls’ mothers had not attended formal education. About neonates’ socio-demographic characteristics, 90.2% of the cases and 92.7% controls were found under the age of 07 days and the median age at admission was 12 h for both cases and controls. The proportions of male neonates were 43.9% in cases and 40.9% in controls. Almost all (99.2%) of respondents were Amhara by their ethnic group (Table 1).
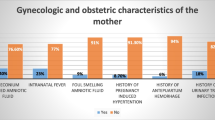
Maternal-related variables
The median parity of mothers for both cases and controls was 2 and ranges from 1 to 9 live births for cases and 1 to 6 for controls. Majority of the respondents (80.5%) cases and 89.6% controls had single pregnancy status at the index pregnancy. Most of the study participants (96.7%) have received antenatal care (ANC) service at least once during the index pregnancy. More than two thirds (70.7%) of cases and 79.9% controls were delivered by spontaneous vaginal delivery. The proportion of mothers who had history of urinary tract infections (UTI) during the index pregnancy were 19.5% in cases and 2.4% in controls. Nearly one-third (35.4%) of cases’ mother gave birth after 18 h of rupture of membrane (PROM) and 8.5% in controls group (Table 2).
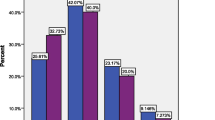
Neonatal-related variables
Two-third (67.1%) of controls and 29.3% of cases were term neonates. Majorities (62.2%) of cases and 37.1% of controls were born with below normal birth weight. More than half (53.7%) of cases and only 5.5% controls had APGAR score of < 7 at fifth minute. Besides, 53.7% of cases and 10.4% of controls have received resuscitation at birth (Table 3).
Determinants of neonatal sepsis
In multivariable logistic regression analysis, preterm neonates (gestational age < 37 weeks) had 6.9 times [AOR = 6.903; 95% CI (2.79, 17.28)] higher odds of developing sepsis compared to term neonates. The odds of neonatal sepsis among neonates born from mothers who had history of PROM was 2.8 times [AOR =2.81; 95% CI (1.01, 7.79)] as compared to their counterparts. Similarly, the odds of neonatal sepsis among neonates who were not crying immediately at birth and have received resuscitation at birth was 2.85 [AOR = 2.85; 95% CI (1.09, 7.47)] times higher compared to neonates who were crying immediately and did not received resuscitation at birth (Table 4).
Discussion
The finding of this study showed that both maternal and neonatal-related factor had a significant effect on the risk of neonatal sepsis. The result of this study showed that history of maternal PROM, being preterm neonate, those neonate who are not crying immediately at birth and have received resuscitation at birth were predictors of neonatal sepsis.
This study revealed that preterm delivery as one of the significant risk factors of neonatal sepsis which is 6.9 times more likely as compared to term delivery. This finding is in agreement with the findings from the study conducted in referral hospitals of Addis Ababa Ethiopia, Ghana, and Tanzania [13, 15, 19, 24, 25]. Explained that preterm neonates tend to have poor host defenses and more likely to suffer sepsis. Moreover, preterm neonates are also more likely to receive parenteral nutrition through insertion of needle to vein, which might expose neonates to infections.
Not crying immediately at birth showed a significant association with neonatal sepsis. The present study indicated that the odds of neonatal sepsis among neonates who were not crying immediately at birth were 2.85 times more likely as compared to those who were crying at birth. This finding was in line with the previous finding reported in Ghana and Mekele, Ethiopia [13, 16]. This might be crying at birth is the most critical part of the physiological adjustment procedure for a newborn to survive the extra uterine life following cutting of the umbilical cord when the newborn undergoes a series of cardiopulmonary changes with the first breath of air. Initial breathing is the result of a reflex triggered by pressure and temperature changes, noise, light, and other sensations related to the birth process. Neonate might be unable to cry due to interference of respiration. The absence of breathing and/or crying might leads health care professionals to do resuscitation. Resuscitation at birth was significantly associated with neonatal sepsis. Doing resuscitation to a newborn is also found to be a significant determinant of neonatal sepsis in the current and in the previous studies in Ghana and Tanzania [13, 15]. This happened because the lumen of the peripheral airway of the newborn is narrow and respiratory secretions are plentiful which could predispose the newborn to atelectasis. For the collapsed of lungs, performing vigorous procedures is may cause bruises to the delicate and fragile mucous membrane of the neonate and further serve as an entry point for microbial agents. Moreover, resuscitation might be done with unsterile equipment, which could introduce microbes into the lungs of the neonate whose immune system is not yet well developed.
From obstetrics related variables, premature rupture of membrane (≥18 h) is found to be a significant determinants of neonatal sepsis. The odds of neonatal sepsis among neonates born from mothers who had history of PROM was 2.8 times more likely as compared to those neonates born before 18 h of rupture of membrane. This finding is similar with the findings in Mekelle, Ethiopia and Pakistan [16, 26]. However, the study in Ghana [13] did not identify premature rupture of membrane as a significant risk factor. The contradiction may be due to appropriate interventions put in place to manage such cases in Ghana. Early rupture of membrane increases the chance of ascending microorganisms from the birth canal into the amniotic sac causing Chorioamnionitis and fetal compromise as well as asphyxia which frequently leads the new born to infection in utero. Cervical incompetence, cord prolapse, and mal-presentation associated with prematurity could causes PROM and further neonatal sepsis is happened [27].
Limitation of the study
Since the study was done on admitted neonates, thus results might lack generalizability to the entire population.
Conclusions
PROM was found to be obstetric-related determinant of neonatal sepsis, Gestational age < 37 weeks, not crying immediately at birth, and have received resuscitation at birth were found to be neonatal-related risk factors of neonatal sepsis. Infection prevention strategies need to be strengthening and/or implementing by providing especial attention for the specified determinants.
Availability of data and materials
All the data are available in the manuscript.
Abbreviations
- ANC:
-
Antenatal care
- AOR:
-
Adjusted odds ratio
- APGAR:
-
Activity, pulse, grimace, appearance, respiration
- BW:
-
Birth weight
- CI:
-
Confidence interval
- EONS:
-
Early Onset Neonatal Sepsis; Integrated Management of Neonatal and Childhood Illness
- LONS:
-
Late onset neonatal sepsis
- NICU:
-
Neonatal intensive care unit
- OR:
-
Crude odds ratio
- PROM:
-
Premature rupture of membrane
- SPSS:
-
Statistical package for social science
- UTI:
-
Urinary tract infection
References
UNICEF, The neonatal period is the most vulnerable time for a child. March 2018. https://data.unicef.org/topic/child-survival/neonatal-mortality/; Accessed date 11 June 2019.
Giannoni E, et al. Neonatal Sepsis of early onset, and hospital-acquired and community-acquired late onset: a prospective population-based cohort study. J Pediatr. 2018.
Seale AC, et al. Estimates of possible severe bacterial infection in neonates in sub-Saharan Africa, South Asia, and Latin America for 2012: a systematic review and meta-analysis. Lancet Infect Dis. 2014;14(8):731–41.
Wynn JL, et al. Time for a neonatal–specific consensus definition for sepsis. Pediatr Crit Care Med. 2014;15(6):523.
Shane AL, Sánchez PJ, Stoll BJ. Neonatal sepsis. Lancet. 2017.
Darmstadt GL, et al. Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet. 2005;365(9463):977–88.
Healy CM. Vaccines in pregnant women and research initiatives. Clin Obstet Gynecol. 2012;55(2):474–86.
Silva NB, Menezes RP, Brito MO, Alves PG, Pedroso RS, Röder DV. Sepsis Neonatal: Epidemiology, Etiology and Risk Factors. Adv Biotechnol Microbiol. 2017;4(2):1–2.
Bhutta ZA, et al. Community-based interventions for improving perinatal and neonatal health outcomes in developing countries: a review of the evidence. Pediatrics. 2005;115(2):519–617.
Meegan ME, et al. Effect on neonatal tetanus mortality after a culturally-based health promotion programme. Lancet. 2001;358(9282):640–1.
de Bernis L, et al. Skilled attendants for pregnancy, childbirth and postnatal care. Br Med Bull. 2003;67(1):39–57.
Ashish K, et al. Scaling up quality improvement intervention for perinatal care in Nepal (NePeriQIP); study protocol of a cluster randomised trial. BMJ Glob Health. 2017;2(3):e000497.
Siakwa, M., M.D. Kpikpitse, and S. Mohamed, Neonatal sepsis in rural Ghana: A case control study of risk factors in a birth cohort. IJRMHS & KAJ, 2014: p. 77–88.
Lim WH, Lien R, Huang YC, Chiang MC, Fu RH, Chu SM, Hsu JF, Yang PH. Prevalence and Pathogen Distribution of Neonatal Sepsis Among Very-Low-Birth-Weight Infants; 2011.
Jabiri, A., et al., Prevalence and factors associated with neonatal sepsis among neonates in Temeke and Mwananyamala Hospitals in Dar es Salaam, Tanzania. Tanzania J Health Res, 2016. 18(4).
Gebremedhin D, Berhe H, Gebrekirstos K. Risk factors for neonatal sepsis in public hospitals of Mekelle City, North Ethiopia, 2015: unmatched case control study. PLoS One. 2016;11(5):e0154798.
Murthy S, et al. Risk factors of neonatal sepsis in India: a systematic review and meta-analysis. PLoS One. 2019;14(4):e0215683.
Shehab El-Din EMR, et al. Epidemiology of neonatal sepsis and implicated pathogens: a study from Egypt. Biomed Res Int. 2015;2015.
Aamir MM, et al. Prevalence of multidrug resistant bacteria causing late-onset neonatal sepsis. Int J Curr Microbiol App Sci. 2015;4(5):172–90.
Getabelew A, et al. Prevalence of neonatal sepsis and associated factors among neonates in neonatal intensive care unit at selected governmental hospitals in Shashemene town, Oromia regional state, Ethiopia, 2017. Int J Pediatr. 2018;2018.
Le Geyt, J. and S. Hauck, G272 Epidemiological trends of neonatal sepsis in a county referral hospital in central Kenya. 2016, BMJ Publishing Group Ltd.
Mhada TV, et al. Neonatal sepsis at Muhimbili National Hospital, Dar Es Salaam, Tanzania; aetiology, antimicrobial sensitivity pattern and clinical outcome. BMC Public Health. 2012;12(1):904.
Samaga MP. Prevalence of neonatal septicaemia in a tertiary care hospital in Mandya, Karnataka, India. Int J Res Med Sci. 2016;4(7):2812.
Girma T. Prevalence and associated factors of neonatal sepsis among neonates in neonatal intensive care unitat selected governmental hospitals in Addis Ababa, Ethiopia, vol. 21; 2016. p. 59.
Worku B, et al. Predictors of early neonatal mortality at a neonatal intensive care unit of a specialized referral teaching hospital in Ethiopia. Ethiop J Health Dev. 2012;26(3):200–7.
Alam MM, et al. Neonatal sepsis following prolonged rupture of membranes in a tertiary care hospital in Karachi, Pakistan. J Infect Dev Countries. 2014;8(01):067–73.
Jiang J-H, et al. Neonatal sepsis in the neonatal intensive care unit: characteristics of early versus late onset. J Microbiol Immunol Infect. 2004;37(5):301–6.
Acknowledgments
The authors acknowledged Debre Markos University, Debre Markos Referral Hospital, and data collectors.
Funding
Not applicable
Author information
Authors and Affiliations
Contributions
MA worked on designing the study, provide training the data collectors, supervising the data collectors, interpreting the result, preparing the manuscript. MA1, MA, HA, BM, WA, and AE analyzed and interpreted the result and wrote the manuscript. All authors involved starting from design, data interpretation, to critically review the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was obtained from Debre Markos University, College of Health sciences, Institutional Health Research Ethics Review Committee (IHRERC). Informed consent was taken from each participant.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no any competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Alemu, M., Ayana, M., Abiy, H. et al. Determinants of neonatal sepsis among neonates in the northwest part of Ethiopia: case-control study. Ital J Pediatr 45, 150 (2019). https://doi.org/10.1186/s13052-019-0739-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13052-019-0739-2