Abstract
Background
Care for injured patients in England is provided by inclusive regional trauma networks. Ambulance services use triage tools to identify patients with major trauma who would benefit from expedited Major Trauma Centre (MTC) care. However, there has been no investigation of triage performance, despite its role in ensuring effective and efficient MTC care. This study aimed to investigate the accuracy of prehospital major trauma triage in representative English trauma networks.
Methods
A diagnostic case-cohort study was performed between November 2019 and February 2020 in 4 English regional trauma networks as part of the Major Trauma Triage Study (MATTS). Consecutive patients with acute injury presenting to participating ambulance services were included, together with all reference standard positive cases, and matched to data from the English national major trauma database. The index test was prehospital provider triage decision making, with a positive result defined as patient transport with a pre-alert call to the MTC. The primary reference standard was a consensus definition of serious injury that would benefit from expedited major trauma centre care. Secondary analyses explored different reference standards and compared theoretical triage tool accuracy to real-life triage decisions.
Results
The complete-case case-cohort sample consisted of 2,757 patients, including 959 primary reference standard positive patients. The prevalence of major trauma meeting the primary reference standard definition was 3.1% (n=54/1,722, 95% CI 2.3 – 4.0). Observed prehospital provider triage decisions demonstrated overall sensitivity of 46.7% (n=446/959, 95% CI 43.5-49.9) and specificity of 94.5% (n=1,703/1,798, 95% CI 93.4-95.6) for the primary reference standard. There was a clear trend of decreasing sensitivity and increasing specificity from younger to older age groups. Prehospital provider triage decisions commonly differed from the theoretical triage tool result, with ambulance service clinician judgement resulting in higher specificity.
Conclusions
Prehospital decision making for injured patients in English trauma networks demonstrated high specificity and low sensitivity, consistent with the targets for cost-effective triage defined in previous economic evaluations. Actual triage decisions differed from theoretical triage tool results, with a decreasing sensitivity and increasing specificity from younger to older ages.
Similar content being viewed by others
Introduction
The care of seriously injured patients in England was noted to be sub-optimal in a 2007 report by the National Confidential Enquiry into Patient Outcome and Death, where 60% of cases demonstrated deficiencies in organisational or clinical aspects of care [1]. A subsequent 2010 National Audit Office enquiry confirmed these findings, highlighting the ad hoc organisation of trauma care, with unacceptable variations in mortality rates, depending on where and when a patient received treatment [2].
In response, trauma care in England was reconfigured with the introduction of inclusive regional trauma networks in 2011 [3]. These systems of care consist of a central major trauma centre (MTC) hospital providing specialist resuscitation, definitive care, and rehabilitation to the highest acuity and most seriously injured patients. Non-specialist general hospitals, termed trauma units, manage less seriously injured patients and can provide stabilisation and transfer of the more seriously injured to MTCs when needed. Other acute hospitals, which would not routinely manage injured patients, are designated Local Emergency Hospitals. Management, training, and governance structures are incorporated to coordinate patient management and ensure high quality care is delivered [4].
English ambulance services use triage tools to identify patients with major trauma who would benefit from expedited MTC care. Developed from the American College of Surgeons Committee on Trauma Field Triage Guidelines, these consist of a checklist of physiological and injury variables [5]. Their primary purpose is to identify appropriate patients for direct transportation to MTCs, potentially bypassing other hospitals that may be closer to the location of injury. A second purpose, relevant to patients regardless of injury location, is to guide pre-alert calls to the MTC emergency department to allow activation of a hospital trauma team and rapid resuscitation. Triage tools must balance under- and over-triage, to ensure patients with major trauma are appropriately treated, but MTC resources are not wasted unnecessarily.
Introduction of trauma systems has been associated with improved outcomes for patients with major trauma [6]. However, there has been no investigation of triage tool performance, despite their pivotal role in ensuring effective and efficient MTC care. Each English ambulance service uses a different triage tool, varying in structure and content. This study aimed to characterise major trauma triage tool performance in representative English trauma networks. Specific objectives were to describe the characteristics of patients presenting to ambulance services with non-trivial injury, to evaluate the accuracy of real-life triage decisions, and to investigate the theoretical accuracy of triage tools.
Methods
Study design
A diagnostic case-cohort study was undertaken to evaluate the accuracy of major trauma triage in representative English trauma networks [7]. Study procedures and reporting followed the principles stated in STARD guidelines for performing diagnostic accuracy studies [8]. This study was conducted as a planned secondary analysis of the Major Trauma Triage Study (MATTS), described in detail elsewhere [9].
Setting
The study was undertaken in four inclusive regional trauma networks: Birmingham, West Yorkshire, North West London, and Severn. These are predominantly served by four separate NHS ambulance services: West Midlands Ambulance Service (WMAS); Yorkshire Ambulance Service (YAS); London Ambulance Service (LAS); and the South-Western Ambulance Service (SWAS) respectively. The study trauma networks represent a diverse range of localities, demographic, socioeconomic and injury profiles. Further details on the participating trauma networks are provided in the supplementary materials.
Index tests and reference standard
Participating ambulance service triage tools consisted of a checklist of variables applied in parallel. With exception of SWAS, these were grouped into domains. Physiology (‘step 1’) and anatomical injury (‘step 2’) variables are mandatory, indicating bypass and pre-alerting to MTCs when positive. Mechanism of injury (‘step 3’) and special circumstance (‘step 4’) variables are discretionary, prompting consideration of bypass and pre-alerting to MTCs. Ambulance service triage tools are presented in the supplementary materials.
The primary index test under consideration was prehospital provider triage decision making, with a positive result defined as patient transport with a pre-alert call to the MTC. This reflects the dual purposes of a major trauma tirage tool: a) to select patients for bypass to a distant MTC (relevant to patients injured closest to a non-MTC), and b) to inform emergency department pre-alert calls facilitating activation of a hospital trauma team (relevant to patients injured closest to MTC or bypassed). Initial hospital destination, MTC versus non-MTC, was investigated as a secondary index test.
The theoretical diagnostic accuracy of each ambulance service's major trauma triage tool was also examined, representing the simulated application of triage tools. Triage tool variables were assessed according to objective data present in ambulance service records, regardless of the final triage decision or hospital destination, clinical judgement, or hospital destination.
The primary reference standard against which triage decisions were assessed was injured patients who would benefit from expedited MTC care, as characterised by previously published MATTS consensus-based definition [10]. This consists of four domains, comprising: need for critical interventions, presence of significant individual anatomical injuries requiring specialist care, a burden of multiple injuries benefiting from specialist multidisciplinary management, and patient characteristics indicating a capacity to benefit from advanced specialist care. Secondary reference standards were also considered: injury severity score (ISS) ≥16; [11] the need for urgent trauma interventions (the critical interventions domain of the MATTS reference standard); [10] and the MATTS reference standard without open fractures.
Study population
The source population was all patients presenting with acute injuries to the four participating ambulance services and included trauma networks. The subsequent study population consisted of consecutive patients, irrespective of age, conveyed to a participating trauma network hospital, between 1st November 2019 and 28th February 2020 and meeting study inclusion and exclusion criteria as detailed in Table 1. A random sample of individuals from the study population were included irrespective of reference standard status (‘sub-cohort’). Furthermore, all eligible patients meeting reference standard criteria were identified from the Trauma Audit and Research Network (TARN) database, the English national trauma registry, and included as 'cases' [12]. Data linkage between a) cases meeting reference standard criteria collected by TARN, and b) Emergency medical services (EMS) identified patients with acute injuries, was conducted deterministically where possible based on a unique ambulance service patient report form number shared across both datasets. In cases where exact deterministic matching was not possible due to missing or inaccurate patient report form number, research paramedics performed probabilistic matching by manually reviewing each reference standard positive case in detail. Demographic, non-unique ambulance identifiers (e.g., ambulance call sign) and incident information was used from TARN data to search for a corresponding record in ambulance service databases. All matches were independently confirmed by a second researcher and a match was not confirmed in the presence of any uncertainty or disagreement. The final study sample included patients with complete data available allowing calculation of triage tool diagnostic accuracy.
Data collection
Patient records for patients sampled in the sub-cohort, or matched to non-sampled reference standard positive cases, were imported into a bespoke research database. Demographic, patient characteristics, physiology, incident, mechanism of injury, interventions, treatments, and clinical assessment information were collected. Relevant electronic closed field data were imported directly where possible, with free text data coded by hand after review of the patients record by research paramedics. Data abstraction was blinded, with all ambulance service data anonymised and reference standard status not available. Data collection was piloted and guided by a pre-specified coding dictionary. Weekly meetings were convened to review data collection, with any uncertainties resolved through consensus. Data was recorded as missing if not present in closed fields, or if not possible to infer from free text fields. Following data collection, range and consistency checks were performed with implausible values set to missing.
TARN data collection has been reported in detail previously [12, 13]. Each submitted TARN case from participating hospitals during the study period was coded centrally by TARN data analysts according to primary and secondary reference standard criteria. Anonymised data for reference standard positive cases were then imported into a study database for review by research paramedics. Eligibility against inclusion and exclusion criteria was confirmed manually.
Statistical analyses
The analysis proceeded in six stages. Firstly, the derivation of study population, parent cohort, sub-cohort, and reference standard positive cases were enumerated and delineated graphically using flow charts. Secondly, the study sample was characterised, with patient demographics, injury features and missing data examined using descriptive statistics. Thirdly, in the main analysis, the diagnostic accuracy of prehospital provider triage decision for all patients was investigated against the primary reference standard. Sensitivity and specificity were calculated with their 95% confidence intervals, overall and stratified by each ambulance service. Fourthly, the accuracy of triage decisions across different age groups was evaluated for the whole sample, with sensitivity and specificity calculated for children (aged <16 years) and subgroups defined by adult age deciles. Finally, in secondary analyses, the theoretical accuracy of each ambulance service triage tool was assessed. Triage tools were coded algorithmically according to their stated variable thresholds against the observed data. The first recorded vitals sign was used for physiology variables. Where triage tool variables were defined as sustained physiology values, two or more consecutive values meeting the threshold were required. Two independent statisticians undertook coding to ensure accuracy. Cumulative sensitivity and specificity of sequential triage tool steps, including discretionary steps, based on recorded data were calculated in the full study sample. Results were displayed graphically using plots of paired sensitivity/specificity and compared to the accuracy of provider triage decisions. In sensitivity analyses the main analysis was repeated for alternative index tests (MTC Vs non-MTC initial destination) and reference standards (injury severity score ≥16, the need for urgent trauma interventions, and the MATTS open reference standard without open fractures).
Analyses were conducted in R Statistical Software (v4.3.0; R Core Team 2023) and STATA version 17.0 (StataCorp. 2016. Stata Statistical Software: Release 17. College Station, TX: StataCorp LP). Unweighted summary statistics were reported separately for the case-cohort sample characteristics, diagnostic accuracy metrics, and reference standard prevalence. The unit of analysis was the individual incident. Direct patient identifiers were unavailable, and it was therefore not possible to account for clustering from recurrent incidents in the same patient.
Funding, ethical approval and data governance
This study was undertaken as part of the Major Trauma Triage Study (MATTS) project, aiming to develop a new national triage tool, funded by the National Institute of Health Research Health Technology Agency Assessment Programme (NIHR HTA ref: 17/16/04) [9]. Ethical approval was provided by Yorkshire and The Humber - Bradford Leeds Research Ethics Committee (Reference: 19/YH/0197). A study protocol and statistical analysis plan were pre-specified.
Results
Sample derivation and characteristics
Between 1st November 2019 and 28th February 2020, 47,513 patients with non-trivial injury working impression codes were conveyed to included trauma network hospitals by participating ambulance services, forming the source population. Overall, 1,853 eligible patients with complete data were sampled into the sub-cohort, comprising 55 patients (54 adults, 1 child) meeting primary reference standard criteria, and 1,798 patients (1,679 adults, 119 children) who were primary reference standard negative. During the same study period 959 TARN cases (928 adults, 31 children) met inclusion criteria, were successfully matched to a corresponding ambulance service record, and had complete data. Derivation of the parent cohort, sub-cohort, and study samples for primary reference standard positive and negative patients are detailed in Figs. 1 and 2.
The overall prevalence of major trauma meeting the primary reference standard definition in eligible sub-cohort patients with complete data was 3.1% (n=54/1,798, 95% CI 2.3 – 4.0). Included patients presenting to ambulance services with non-trivial injury were predominantly elderly (median age 73 years), female (52.6%), and sustained accidental (88.1%) blunt trauma (97.7%) from ground level falls (70.0% of injury mechanisms). Characteristics of the included complete case study sample are detailed in Table 2.
Accuracy of prehospital provider triage decisions
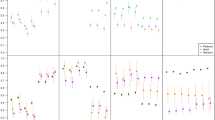
Observed prehospital provider triage decisions (i.e., whether the patient was pre-alerted to the MTC, regardless of the indicated triage tool result) demonstrated overall pooled sensitivity of 46.7% (95% CI 43.5-49.9) and specificity of 94.5% (95% CI 93.4-95.6) for the MATTS reference standard. However, there was a marked variation in triage decisions across ambulance services, ranging from low sensitivity (26%) and high specificity (98%) in SWAS, to higher sensitivity (67%) and lower specificity (89%) in LAS, as shown in Table 3 and Fig. 3. There was a clear trend of decreasing sensitivity and increasing specificity from younger to older ages. Sensitivity was 80.6% in under 16 years falling to 22.7% in over 90 years. Corresponding specificity was 92.4% in under 16 years, increasing to 98.4% in patients over 90 years (Fig. 3). Of note, a small proportion (<1% across all age groups) of patients not conveyed to a MTC with a pre-alert underwent an urgent trauma intervention.
Theoretical accuracy of ambulance service triage tools
There was variation in sensitivity and specificity across ambulance service triage tools following theoretical application of mandatory steps: SWAS (0.32/0.95), WMAS (0.46/0.88), YAS (0.51/0.86), LAS (0.56/0.86). Where relevant, theoretical application of discretionary mechanism of injury (step 3) variables appeared to provide a small increase in sensitivity, with a compensatory small reduction in specificity. Adding special circumstances (step 4) variables resulted in much higher sensitivity, but a very large fall in specificity (Fig. 3). Prehospital provider triage decisions differed from the indicated triage tool result across all ambulance services, with ambulance service clinician judgement resulting in higher specificity than mandatory triage tool steps (Table 3, Fig. 3).
Top panel: Sensitivity and specificity of observed triage decisions across different patient age groups; Bottom panel: Receiver operating characteristic curves for participating ambulance services observed triage decisions and theoretical triage tool results evaluated against the primary MATTS reference standard in patients aged over 16 years
Sensitivity analyses
Results were largely unchanged in sensitivity analyses examining the secondary ISS≥16 reference standard and omitting open fractures from the primary reference standard. A large increase in sensitivity was seen for both the theoretical application of triage tools, and actual triage decisions (80.0%), when evaluated against the urgent trauma interventions reference standard. Specificity was not materially changed and remained high (94.0%). Sensitivity was slightly increased (57.5%), and specificity decreased (78.6%) for the primary reference standard when prehospital triage decisions were evaluated according to initial hospital destination (MTC Vs non-MTC), regardless of whether a pre-alert was provided. Full details are provided in the supplementary materials.
Discussion
Summary
Patients presenting to four English trauma networks by ambulance with non-trivial injury were most commonly elderly females with blunt trauma from ground level falls. The overall prevalence of major trauma was low (3.1%). Observed prehospital provider triage decisions demonstrated overall pooled sensitivity of 46.7% (95% CI 43.5-49.9) and specificity of 94.5% (95% CI 93.4-95.6) for the primary reference standard. However, accuracy was heterogenous with SWAS demonstrating lower sensitivity and higher specificity than other ambulance services. There was a clear trend of decreasing sensitivity and increasing specificity from younger to older ages. Prehospital provider triage decisions did not always follow theoretical triage tool results, with ambulance service triage decisions demonstrating higher specificity. Sensitivity of triage decisions was increased for urgent trauma interventions (80%, 95%CI 75.0-84.0), with specificity remaining high (94%, 95%CI 93.0-95.0).
Interpretation
Statistical measures of diagnostic accuracy are typically reported in terms of sensitivity and specificity [14]. These metrics may be counterintuitive as they are defined retrospectively by disease status, rather than the clinically relevant probability of a condition being present when the test result in known [15]. There is evidence that graphical representations, predictive values, natural frequencies, or using likelihood ratios, promotes better understanding [15,16,17]. A range of visual interpretations of the main study findings are therefore presented in the supplementary materials. Taking a Bayesian system-level approach, on average there is a 3.1% chance of major trauma when an acutely injured patient presents to ambulance services. After a positive triage decision for bypassing/pre-alerting the MTC there will be a 22% chance that patient will turn out to have major trauma. Conversely, if the triage decision is negative then there will be a 98% chance that the patient does not have major trauma [18].
For triage tools structured as a 'checklist', diagnostic accuracy could be manipulated by changing the number, type, and thresholds of included variables. This results in an inevitable trade-off between sensitivity and specificity, where the number of false positive cases increases as false negatives are reduced. Sensitivity is often prioritised, for example the ACS-COT has published a target of >95% for field triage, with a consequent penalty of reduced specificity (ASC-COT targets 65-70%) [19]. However, in low prevalence settings this approach would lead to poor positive predictive values and many false positives [20]. Economic modelling has confirmed that prioritising sensitivity is not cost-effective, and specificity should be favoured [21,22,23,24]. It is interesting that real-life prehospital triage decisions are closely aligned to these empirical cost-effectiveness targets.
The index test definition for positive prehospital triage is open to debate. Our primary definition of a pre-alert call to the MTC, reflects the dual purposes of a major trauma triage tool of selecting patients for bypass to a distant MTC and facilitating emergency department pre-alert calls. It could be argued that transport to a MTC is the most important factor. However, this would not account for delayed resuscitation and treatment in cases not pre-alerted to the ED. It could also be misleadingly influenced by the proportion of patients injured within the MTC catchment area, as these patients' destination is fixed. Alternatively, from a system perspective, the final common pathway for major trauma patients' is reception into a MTC resuscitation area with hospital trauma team activation. However, full hospital trauma team assessment may not be required in stable patients, activation criteria may differ from triage tool variables, and deployment is outside the control of prehospital providers.
The reference standard against which triage decisions should be assessed is also arguable. The traditionally used Injury Severity Score has many limitations, not least its focus on the degree of anatomical trauma per se, rather than the potential to benefit from MTC care [11]. Intervention based reference standards, such as the US consensus definition, may better reflect the need for MTC care, but do not account for benefit arising from MTC supportive care and rehabilitation [10, 25]. Operationalisation in triage research is also potentially challenged by the absence of counterfactual information, and cases may be incorrectly classified as false negatives if they did not receive an intervention that was indicated due to lack of availability or expertise outside the MTC. Evaluation of multiple reference standards will provide a comprehensive and holistic assessment of triage performance.
Differences were apparent in observed prehospital triage, and calculated theoretical triage tool accuracy, across participating trauma networks. The overall pooled accuracy results should therefore be interpreted judiciously. The heterogeneity of results may reflect the use of different ambulance service triage tools. Theoretical accuracy of mandatory triage tool steps (SWAS most specific, LAS most sensitive, WMAS/YAS intermediate), appeared to correlate with real-life triage decision making (SWAS most specific, LAS most sensitive, WMAS/YAS intermediate). Alternatively, the variation could reflect differences in philosophies (inclusive versus exclusive focus), geographies (more urban Vs more rural), or network organisation (e.g., extent of remote decision support available from trauma desks).
Prehospital providers triage decisions were observed to differ from those indicated by triage tools, apparently improving triage performance. This could result from discretionary triage tool use in selected patients, application of additional clinical judgement to over-rule indicated triage tool results, or the influence of applying discretionary triage tool steps. Previous qualitative research has demonstrated that prehospital triage making is often heuristic with triage tools used less commonly as experience increases [26]. It is perhaps not surprising that subjective real-life decisions outperformed objective triage tool accuracy, as clinical judgement has been consistently demonstrated to be superior in multiple studies across many disease areas [27, 28]. This has important implications, as to benefit from better overall triage performance achieved through subjective clinical judgement, some incorrect individual clinical decisions will need to be accepted; and clinical governance strategies to increase triage tool use and adherence may be counterproductive. Spectrum effects were apparent across different age groups with decreasing sensitivity and increasing specificity for triage decisions from younger to older ages for the primary reference standard. Interestingly, the proportion of false negatives requiring urgent trauma interventions remained negligible (<1%), perhaps reflecting provider judgement in selecting patients perceived to benefit most from MTC care.
The four included trauma networks are representative of the broader English population, including a diverse mix of urbanisation, socioeconomic status, geographies, and injury profiles. The results of this study should therefore be generalisable throughout the UK National Health Service. In response to the COVID-19 pandemic, new triage tools have been implemented in LAS and SWAS, which may influence contemporary triage. External validity to other settings is limited. Different injury patterns (e.g., higher numbers of gun-shot wounds), alternative health system models (state Vs insurance Vs private funding), trauma network organisation (level of training, inclusive Vs exclusive), medicolegal risk, and patient demographics (e.g., population age profiles) in other settings could strongly influence triage decision making.
Comparison to literature
Two recent systematic reviews have examined real-life major trauma triage decisions and compliance with theoretical triage tool results. Van Rein (2018a) evaluated prehospital triage decisions, defined by initial hospital destination, in 33 studies [29]. The findings were limited by poor methodological quality and very heterogenous results were reported with sensitivity ranging from 32% to 99% and specificity from 1% to 99%. Notwithstanding the different populations and trauma system organisation seen in the predominantly US settings, results from the better-quality studies were not disimilar to the current findings. It was also concluded, in common with the current study, that EMS provider judgment added value to triage protocols in the identification of severely injured patients. Van Rein (2018b) also investigated compliance, reviewing 11 studies comparing objective triage tool results with actual triage destinations [30]. The methodological quality of most studies was again poor, with widely disparate compliance rates between 21% and 91% reported. One study with good methodological quality showed, in common with our findings, that the triage protocol identified only a minority of severely injured patients, and a tendency to transport elderly trauma patients to lower-level trauma centres, even if the patient met one or more triage criteria.
Limitations
This study has several strengths. The risk of information bias was minimised by following recommendations for collection of routine data in retrospective studies [31, 32]. Other common sources of systematic error in diagnostic accuracy studies were avoided, including a 'two-gate' case-control study design; and test, diagnostic review, partial verification, incomplete verification, incorporation, and disease progression biases [33]. However, there are some potential limitations. The use of routine data may have resulted in index test or reference standard misclassification. Selection bias could arise from imperfect matching of ambulance service and TARN data and complete case analyses, omitting cases with missing data. However, the matching rate was high (>95%) and missing data rate was low (<10%). Furthermore, reference standard classification is dependent on encompassing TARN inclusion criteria, complete case ascertainment by TARN, and accurate matching of TARN and prehospital data.
Conclusions
Prehospital decision making for injured patients in English trauma networks demonstrated high specificity and low sensitivity, consistent with the targets for cost-effective triage defined in previous economic evaluations. Actual triage decisions differed from theoretical triage tool results, with a clear trend of decreasing sensitivity and increasing specificity from younger to older ages. Further research could usefully explore factors associated with triage tool compliance, such as included variables, mechanism of injury, injury timing and location, and patient characteristics.
Availability of data and materials
The anonymised data and full reproducible analysis code is available on reasonable request, subject to ethical approvals and appropriate data sharing agreements.
Abbreviations
- MTC:
-
Major Trauma Centre
- MATTS:
-
Major Trauma Triage Study
- WMAS:
-
West Midlands Ambulance Service
- YAS:
-
Yorkshire Ambulance Service
- LAS:
-
London Ambulance Service
- SWAS:
-
South-Western Ambulance Service
- EMS:
-
Emergency medical services
- TARN:
-
Trauma Audit and Research Network
- ISS:
-
Injury severity score
References
Death NCEiPOa. NECPOD Report. Trauma Who Cares? ; 2007.
National Audit Office. Major Trauma Care in England. The Stationery Office/Tso; 2010. ISBN-13: 9780102963472, ISBN-10: 0102963479.
Vondy A, Willett K. Trauma care in England: London’s trauma system goes live. Emerg Med J. 2011;28(3):250.
McCullough AL, Haycock JC, Forward DP, Moran CG. II. Major trauma networks in England. BJA. 2014;113(2):202–6.
Sasser SM, Hunt RC, Faul M, Sugerman D, Pearson WS, Dulski T, et al. Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recomm Rep. 2012;61(Rr-1):1–20.
Moran CG, Lecky F, Bouamra O, Lawrence T, Edwards A, Woodford M, et al. Changing the system - major trauma patients and their outcomes in the NHS (England) 2008–17. EClinicalMedicine. 2018;2–3:13–21.
O’Brien KM, Lawrence KG, Keil AP. The case for case–cohort: an applied epidemiologist’s guide to reframing case-cohort studies to improve usability and flexibility. Epidemiology. 2022;33(3):354–61.
Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig L, et al. STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. BMJ. 2015;351:h5527.
GW F. ISRCTN17968752 - MATTS: Major Trauma Triage Tool Study: ISRCTN Registry; 2018. Cited 2023 8th July 2023.
Fuller G, Keating S, Turner J, Miller J, Holt C, Smith JE, et al. Injured patients who would benefit from expedited major trauma centre care: a consensus-based definition for the United Kingdom. Br Paramed J. 2021;6(3):7–14.
Baker SP, O’Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–96.
Network TAaR. Trauma Audit and Research Network 2023. Available from: www.tarn.ac.uk.
Fuller G, Hasler RM, Mealing N, Lawrence T, Woodford M, Juni P, et al. The association between admission systolic blood pressure and mortality in significant traumatic brain injury: a multi-centre cohort study. Injury. 2014;45(3):612–7.
Akobeng AK. Understanding diagnostic tests 1: sensitivity, specificity and predictive values. Acta Paediatr. 2007;96(3):338–41.
Steurer J, Fischer JE, Bachmann LM, Koller M, ter Riet G. Communicating accuracy of tests to general practitioners: a controlled study. BMJ. 2002;324(7341):824–6.
Reid MC, Lane DA, Feinstein AR. Academic calculations versus clinical judgments: practicing physicians’ use of quantitative measures of test accuracy. Am J Med. 1998;104(4):374–80.
Fanshawe TR, Power M, Graziadio S, Ordóñez-Mena JM, Simpson J, Allen J. Interactive visualisation for interpreting diagnostic test accuracy study results. BMJ Evid Based Med. 2018;23(1):13–6.
Grimes DA, Schulz KF. Refining clinical diagnosis with likelihood ratios. Lancet. 2005;365(9469):1500–5.
McCoy CE, Chakravarthy B, Lotfipour S. Guidelines for field triage of injured patients: in conjunction with the morbidity and mortality weekly report published by the center for disease control and prevention. West J Emerg Med. 2013;14(1):69–76.
Altman DG, Bland JM. Diagnostic tests 2: Predictive values. BMJ. 1994;309(6947):102.
Pollard D, Fuller G, Goodacre S, van Rein EAJ, Waalwijk JF, van Heijl M. An economic evaluation of triage tools for patients with suspected severe injuries in England. BMC Emerg Med. 2022;22(1):4.
Newgard CD, Yang Z, Nishijima D, McConnell KJ, Trent SA, Holmes JF, et al. Cost-effectiveness of field trauma triage among injured adults served by emergency medical services. J Am Coll Surg. 2016;222(6):1125–37.
Nishijima DK, Yang Z, Newgard CD. Cost-effectiveness of field trauma triage among injured children transported by emergency medical services. Am J Emerg Med. 2021;50:492–500.
Maughan BC, Lin A, Caughey AB, Bulger EM, McConnell KJ, Malveau S, et al. Field trauma triage among older adults: a cost-effectiveness analysis. J Am Coll Surg. 2022;234(2):139–54.
Lerner EB, Willenbring BD, Pirrallo RG, Brasel KJ, Cady CE, Colella MR, et al. A consensus-based criterion standard for trauma center need. J Trauma Acute Care Surg. 2014;76(4):1157–63.
Newgard CD, Nelson MJ, Kampp M, Saha S, Zive D, Schmidt T, et al. Out-of-hospital decision making and factors influencing the regional distribution of injured patients in a trauma system. J Trauma. 2011;70(6):1345–53.
Veldhuis LI, Ridderikhof ML, Bergsma L, Van Etten-Jamaludin F, Nanayakkara PWB, Hollmann M. Performance of early warning and risk stratification scores versus clinical judgement in the acute setting: a systematic review. Emerg Med J. 2022;39(12):918.
Schriger DL, Elder JW, Cooper RJ. Structured Clinical Decision Aids Are Seldom Compared With Subjective Physician Judgment, and Are Seldom Superior. Ann Emerg Med. 2017;70(3):338-44.e3.
van Rein EAJ, van der Sluijs R, Houwert RM, Gunning AC, Lichtveld RA, Leenen LPH, et al. Effectiveness of prehospital trauma triage systems in selecting severely injured patients: Is comparative analysis possible? Am J Emerg Med. 2018;36(6):1060–9.
van Rein EAJ, van der Sluijs R, Raaijmaakers AMR, Leenen LPH, van Heijl M. Compliance to prehospital trauma triage protocols worldwide: A systematic review. Injury. 2018;49(8):1373–80.
Kaji AH, Schriger D, Green S. Looking through the retrospectoscope: reducing bias in emergency medicine chart review studies. Ann Emerg Med. 2014;64(3):292–8.
Vassar M, Holzmann M. The retrospective chart review: important methodological considerations. J Educ Eval Health Prof. 2013;10:12.
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–36.
Acknowledgments
This research was supported by the Major Trauma Triage Study (MATTS) study management group, including: Ian Maconochie, Mathew Ward, Mark Millins, Emily Turton, Simon Waterhouse, Matt Stevenson, Daniel Pollard, Abdullah Pandor, Maria Robinson, Stuart Reid, and Di Charles. We are also grateful to the participating trauma networks, hospitals, and Trauma Audit and Research Network staff for their support and help.
Funding
The study was funded by the National Institute of Health Research Health Technology Agency Assessment Programme (NIHR HTA ref: 17/16/04).
Author information
Authors and Affiliations
Consortia
Contributions
GF conceived the study. All authors contributed to design the study. JB and GF performed the data management. JM, RP, KM, JB, and NK collected and coded the data. GF and JB performed the analyses. All authors made substantial contributions to data interpretation. GF drafted the article and all other authors revised it critically for important intellectual content. CC is the guarantor. All authors had full access to all the data in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was provided by Yorkshire and The Humber - Bradford Leeds Research Ethics Committee (Reference: 19/YH/0197). Approval from the Confidentiality Advisory Group was given for the analysis of anonymised routine patient data without explicit patient consent.
Consent for publication
Not applicable – no individual personal data reported.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fuller, G., Baird, J., Keating, S. et al. The accuracy of prehospital triage decisions in English trauma networks – a case-cohort study. Scand J Trauma Resusc Emerg Med 32, 47 (2024). https://doi.org/10.1186/s13049-024-01219-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13049-024-01219-9