Abstract
Background
Accidental hypothermia designates an unintentional drop in body temperature below 35 °C. There is a major risk of ventricular fibrillation below 28 °C and cardiac arrest is almost inevitable below 24 °C. In such cases, conventional cardiopulmonary resuscitation is often inefficient. In urban areas with temperate climates, characterized by mild year-round temperatures, the outcome of patients with refractory hypothermic out-of-hospital cardiac arrest (OHCA) treated with extracorporeal cardiopulmonary resuscitation (ECPR) remains uncertain.
Methods
We conducted a retrospective monocentric observational study involving patients admitted to a university hospital in Paris, France. We reviewed patients admitted between January 1, 2011 and April 30, 2022. The primary outcome was survival at 28 days with good neurological outcomes, defined as Cerebral Performance Category 1 or 2. We performed a subgroup analysis distinguishing hypothermic refractory OHCA as either asphyxic or non-asphyxic.
Results
A total of 36 patients were analysed, 15 of whom (42%) survived at 28 days, including 13 (36%) with good neurological outcomes. Within the asphyxic subgroup, only 1 (10%) patient survived at 28 days, with poor neurological outcomes. A low-flow time of less than 60 min was not significantly associated with good neurological outcomes (P = 0.25). Prehospital ECPR demonstrated no statistically significant difference in terms of survival with good neurological outcomes compared with inhospital ECPR (P = 0.55). Among patients treated with inhospital ECPR, the HOPE score predicted a 30% survival rate and the observed survival was 6/19 (32%).
Conclusion
Hypothermic refractory OHCA occurred even in urban areas with temperate climates, and survival with good neurological outcomes at 28 days stood at 36% for all patients treated with ECPR. We found no survivors with good neurological outcomes at 28 days in submersed patients.
Similar content being viewed by others
Background
Accidental hypothermia designates an unintentional drop in body temperature below 35 °C. Such an event carries the risk of ventricular fibrillation; the risk is major below 28 °C and cardiac arrest is almost inevitable below 24 °C [1] [2]. In such cases, conventional cardiopulmonary resuscitation is often inefficient to obtain return of spontaneous circulation (ROSC).
According to the latest international guidelines, extracorporeal cardiopulmonary resuscitation (ECPR) is considered a potential second line of therapy for hypothermic refractory out-of-hospital cardiac arrest (OHCA) [3]. Refractory cardiac arrest is defined as a failure to obtain ROSC after 20 to 30 min of cardio-pulmonary resuscitation [4]. The Hypothermia Outcome Prediction after ECPR (HOPE) score provides a prediction of the probability of survival in hypothermic OHCA undergoing inhospital ECPR [5] [6]. In Paris’s emergency medical system, ECPR can be implemented in both prehospital or inhospital settings [7]. No study has described patients who have been treated with prehospital ECPR for hypothermic refractory OHCA.
A temperate urban area is characterized by a moderate and mild climate. According to the historical Köppen-Geiger climate classification system [8], these regions generally experience moderate temperature fluctuations between seasons, maintaining relatively comfortable temperatures throughout the year. Temperate climates are not subject to extreme heat or cold, making them less common settings for studies on hypothermia, which is often associated with colder environments. The significance of this study lies in investigating hypothermia in an atypical setting and demonstrating that prognostic outcomes may diverge from those observed in colder regions. Several studies have described the characteristics of patients with hypothermic cardiac arrest in urban areas [9], of patients with hypothermic OHCA treated with ECPR in cold climate settings [10], and of those admitted to a near-alpine-resort trauma center [11]. Because a poor prognosis had already been observed in submersed patients with hypothermic OHCA treated with ECPR [12] [13], we performed a subgroup analysis distinguishing hypothermic refractory OHCA as either asphyxic or non-asphyxic.
Methods
Study design
We conducted a retrospective observational monocentric study of patients admitted to Necker University Hospital, a tertiary-care center in Paris, France. We received approval from the ethics committee of the French Society of Anesthesia and Intensive Care Medicine (#IRB 00010254 - 2023–015). Data were collected by a single dedicated individual stationed within the intensive care unit (ICU), responsible for tending to patients throughout the study duration. Research data were obtained from secure medical record sources using computerized and non-computerized databases covering the period of January 1, 2011, to April 30, 2022. The same methodology was consistently employed throughout the study in compliance with French data protection legislation (French Data Protection Authority #MR004_2228701). The inclusion criteria were: an ICD-10 (International Classification Disease, 10th revision) diagnosis of accidental hypothermia (T68); adults aged 18 years or more; prehospital core temperature of 32 °C or less; accidental hypothermia being the primary cause of cardiac arrest, and extracorporeal cardiopulmonary resuscitation with prehospital or inhospital ECPR.
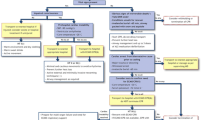
ECPR protocol
Since 2011, the Service d’Aide Médicale Urgente (SAMU) of Paris has been running an ECPR program [14] [15]. When faced with refractory OHCA cases, the ECMO Team was promptly dispatched to the field. Depending on the estimated duration required to reach the hospital, an on-field decision was taken to either proceed with prehospital or inhospital ECPR. This decision strictly followed a single protocol based on both French [16] and more recent international guidelines [17]. A comprehensive visualization of the ECMO implementation protocol, extracted from French recommendations [16], can be found in the supplemental section of the present study (Figure S1). The protocol remained unchanged throughout the study period.
Data collection
Water temperatures of the Seine River were collected through the Public Sanitation Service of Paris and were derived from the daily mean obtained from five distinct sanitation stations across the Paris area. They included yearly mean minimum and maximum temperature values from 2011 to 2022 and daily mean temperatures on the specific days when patients were submersed.
Prehospital data collection adhered to the Utstein criteria [18] and included the following variables: age; sex; prehospital external temperature measured using an external thermometer; medical history encompassing alcohol intoxication, drug intoxication, attempted suicide, social precariousness, chronic alcoholism, psychosis, depression and cognitive disorders; assessment of simplified acute physiology score (SAPS II) [19]; HOPE score assessment for patients who underwent inhospital ECPR [5]; initial heart rhythm at the time of OHCA identification; no-flow time defined as the interval spanning from OHCA identification to the initiation of chest compressions, if the precise onset of symptoms could not be determined when the patient was found in OHCA, no-flow time was considered to be greater than 10 min; low-flow time was defined as the interval spanning from the initiation of chest compressions to the initiation of ECPR pumping; epinephrine administration; amiodarone administration and external cardioversion during advanced life support; medical indication for ECPR; and selection of prehospital ECPR implementation or inhospital ECPR implementation.
Inhospital data collection included: central body temperature, which was measured using an oesophageal thermal probe or a urinary catheter equipped with a thermal sensor; pH level upon ICU arrival; serum lactate level upon ICU arrival; serum potassium level upon ICU arrival; administration of norepinephrine and/or administration of dobutamine upon ICU arrival; presence of a disseminated intravascular coagulopathy during hospital stay; use of renal replacement therapy during hospital stay; occurrence of haemorrhagic events during hospital stay meeting the BARC (Bleeding Academy Research Consensus) criterion of overt bleeding associated with a drop in haemoglobin levels of at least 3 to 5 g/dL [20]; incidence of infectious events during hospital stay defined by acute fever associated with an increase in procalcitonin serum levels, necessitating antibiotic treatment with or without microbiological documentation; refractory shock during hospital stay defined as the persistence of haemodynamic shock after ECPR implementation and rewarming; gastrointestinal bleeding; complications attributed to ECPR during hospital stay defined as: scarpa infections requiring surgical intervention, acute limb ischemia, haemorrhagic shock arising from cannulation site bleeding, anoxic encephalopathy, vessel damage requiring surgery; all the above complications occurring before or after 24 h of ICU arrival; length of hospital stay; survival at 28 days; neurological assessment at 28 days according to the Glasgow-Pittsburgh Cerebral Performance Category scale, defined as follows: (1) good cerebral performance, (2) moderate cerebral disability, (3) severe cerebral disability, (4) coma or vegetative state, (5) brain death [21]. The primary outcome was survival at 28 days with good neurological outcome defined as CPC 1 or 2.
We performed a subgroup analysis distinguishing hypothermic refractory OHCA as either asphyxic or non-asphyxic. Hypothermic refractory OHCA resulting from asphyxia was defined as individuals who experienced submersion in water and subsequently developed hypothermia. Non-asphyxic hypothermic refractory OHCA was defined as individuals who developed hypothermia due to exposure to cold air or other non-water-related causes. Ice-cold water was defined as a water temperature below 7 °C. In-house hypothermia was defined as hypothermia occurring indoors, while outside hypothermia was defined as hypothermia occurring outdoors.
Statistical analysis
Continuous variables were reported as medians with interquartile ranges. Categorical variables were reported as numbers and percentages. Factors associated with favourable neurological outcomes were assessed for categorical variables using the chi-square test or Fischer’s exact test. Continuous variables were divided into categories using relevant thresholds and compared with the chi-square test or Fischer’s exact test. A two-sided p-value of less than 0.05 was considered statistically significant. The statistical analysis was performed using STATA software version v14.0 (Lakeway Drive, TX, USA). Missing data were handled using case-complete analysis.
Results
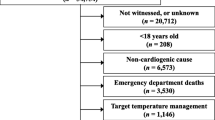
Between January 1, 2011 and April 30, 2022, a total of 36 patients were included in the study. Among them, 26 were treated with ECPR for hypothermic refractory OHCA due to non-asphyxic causes and 10 were treated for refractory hypothermic OHCA with asphyxic causes following submersion in the Seine River. Out of the 10 submersed patients, only 5 experienced exposure to ice-cold waters below 7 °C, with the lowest recorded temperature on the day of submersion being 3.3 °C (Table S2). The complete patient flow chart is depicted in Fig. 1.
Baseline patient characteristics are displayed in Table 1. The median age was 53 years (IQR 45–66) and 28/36 (78%) patients were male. Upon the arrival of the medical team, the mean external temperature stood at 24.3 °C (IQR 22.0–26.0). Overlapping consumption of various drugs, multiple psychiatric disorders, and social precariousness was observed in our patient population; each patient fulfilled at least one of these criteria. Ventricular fibrillation was the first heart rhythm observed at the scene of cardiac arrest in 23/36 (64%) patients. No-flow time was under 5 min in 14/36 (39%) patients. All 36 patients had a refractory cardiac arrest. Median low-flow time was 83 min (IQR 63–97). Prehospital implementation was carried out in 17/36 (47%) of all patients.
Patient characteristics following ICU admission are detailed in Table 2. The overall survival rate at 28 days was 15/36 (42%) of all patients, 14/26 (54%) in the non-asphyxic subgroup and 1/10 (10%) in the asphyxic subgroup. Survival at 28 days with good neurological outcomes, defined as CPC 1 or CPC 2, was observed in 13/36 (36%) of all patients. Within the non-asphyxic subgroup, 13/26 (50%) patients survived with good neurological outcomes, while no survivors were observed in the asphyxic subgroup. Among patients who received prehospital ECPR, 7/17 (41%) achieved survival with good neurological outcomes, whereas in those treated with inhospital ECPR, the rate was 6/19 (32%). Among patients treated with inhospital ECPR, the HOPE score projected a 30% survival rate and observed survival with good neurological outcomes stood at 6/19 (32%).
Table 3 presents an analysis of factors associated with good neurological outcomes at 28 days. The absence of asphyxia was significantly associated with good neurological outcomes (P < 0.01) in contrast to asphyxia. A no-flow time of less than 5 min was also significantly associated with good neurological outcomes (P < 0.01). Conversely, a low-flow time of less than 60 min was not associated with good neurological outcomes (P = 0.25). Similarly, we observed no statistically significant difference in survival rates between patients treated with prehospital ECPR 7/17 (41%) compared with patients treated with inhospital ECPR 6/19 (32%) (P = 0.55).
Discussion
Within our study cohort, 13/36 (36%) patients achieved survival with good neurological outcomes at 28 days, including 13/26 (50%) patients in the non-asphyxic subgroup. However, we did not observe any instances of survivors with good neurological outcomes at 28 days among submersed patients. Prehospital ECPR showed no statistically significant difference in survival with good neurological outcomes when compared with inhospital ECPR (P = 0.55). Prolonged low-flow was not found to be associated with poorer neurological outcomes (P = 0.25). In patients treated with inhospital ECPR, survival predicted by the HOPE score was 30% and observed survival was 6/19 (32%).
Similar survival rates were reported in various studies across different climatic regions. These rates included a 55% survival rate in a continental climate area [9], a 26.5% survival rate in an oceanic climate area [12], a 20% survival rate in an alpine-sport-related accident setting [11], and a 100% survival rate in a high desert climate [22]. It’s important to note that our study population differed from those in these studies. Indeed, a significant portion of our patients faced social precariousness, and/or psychiatric disorders including alcoholism in 18/36 (50%) cases, drug use in 3/36 (8%) cases, psychosis in 5/36 (14%) cases and depression in 9/36 (25%) cases. A study conducted in France between 2000 and 2010, spanning 18 urban areas, attributed 3.9% of all deaths to cold exposure [23]. Notably, deaths related to hypothermia were nearly ninety times more frequent among socially precarious individuals compared with the general population [24]. Additionally, another study conducted in Paris concerning addictions and psychiatric conditions among socially distressed individuals reported that 31.5% suffered from psychiatric disorders [25]. In alignment with these findings, a substantial majority of our patients, 31 out of 36 (86%), faced social precariousness, and 29 out of 36 (81%) presented with at least one psychiatric disorder. This specific profile of accidental hypothermia patients in urban areas with temperate climates represents a significant confounding factor. Therefore, caution must be exercised when comparing hypothermia patient cohorts, and the influence of this parameter should not be overlooked.
We established a significant correlation between the occurrence of asphyxia resulting from submersion in patients experiencing hypothermic refractory OHCA and an increased mortality rate (P < 0.01). Notably, within the asphyxic subgroup, there were no survivors who achieved good neurological outcomes. These findings concur with previous research [12] [26] [27], particularly a study conducted in Paris from 2002 to 2012 that concentrated on inhospital ECPR for drowned patients. In that particular study, out of 20 drowned patients treated with ECPR, only 1 patient was discharged from the hospital with good neurological outcomes, while another patient had poor neurological outcomes [13]. In our study, which encompassed patients treated with both inhospital and prehospital ECPR, only a single patient survived to hospital discharge with poor neurological outcomes. Several hypotheses have been formulated to elucidate these findings. Firstly, certain publications have posited that the neuroprotective effect of water is exclusively conferred by ice-cold water (< 7 °C) [28]. In our investigation, we meticulously recorded the temperature of the Seine River on the day of submersion to explore this threshold. Among the 10 submersed patients, only 5 were exposed to temperatures below 7 °C. The temperatures recorded on the day of submersion in the Seine River ranged from as low as 3.3 °C to as high as 23.5 °C. When considering the comprehensive temperature data of the Seine River (as presented in Table S1 and Table S2) during submersion incidents, the often elevated water temperatures exceeding 7 °C, along with the resulting loss of their neuroprotective attributes, offer a compelling explanation for the heightened mortality observed in our study within the Paris area. Secondly, other noteworthy distinctions highlighted in Tables 1 and 2 can account for the mortality difference between our subgroups. For instance, the asphyxic subgroup exhibited an increased prevalence of asystole 7/10 (70%) compared with the non-asphyxic subgroup 6/26 (23%). Also, the duration of no-flow was more often higher than 5 min in the asphyxic subgroup 9/10 (90%) compared with the asphyxic subgroup 10/26 (39%). These outcomes warrant a reconsideration of the criteria for ECPR, whether conducted in-hospital or prehospital, for hypothermic patients with refractory OHCA following submersion within urban areas with temperate climates.
Regarding prehospital ECPR, a previous study has suggested that the implementation of ECPR in a prehospital setting might offer advantages over inhospital ECPR for OHCA [7]. However, this matter remains ambiguous, as only a few medical teams practice prehospital ECPR, and no large, randomized clinical trial has yet addressed this question. In our present study, we observed no statistically significant difference in survival rates with good neurological outcomes between prehospital ECPR 7/17 (41%) and inhospital ECPR 6/19 (32%) (P = 0.55). However, the size of our sample indicates that the analysis of this statistical result must be approached with great caution. In any case, one of the suggested explanations that could account for this outcome is the less discriminative nature of low-flow in patients with hypothermic refractory OHCA compared with those with non-hypothermic refractory OHCA [29]. Indeed, the median low-flow time in our study reached 83 min (IQR 63–97), surpassing the typical 60-minute threshold linked to survival in ECPR [15]. Surprisingly, a low-flow duration of 60 min or less did not exhibit a statistically significant correlation with favorable neurological outcomes at 28-days (P = 0.25). This outcome prompts doubts about the applicability of the 60-minute implementation guideline for the specific subset of patients encountering hypothermic refractory OHCA. In contrast, a no-flow duration of less than 5 min displayed a statistically significant association with positive neurological outcomes (P < 0.01). As a result, while the duration of no-flow remains of utmost importance, the significance of low-flow might be diminished in cases of hypothermic refractory OHCA [30], thereby reducing the advantage of prehospital ECPR compared with other indications.
The HOPE score, introduced in 2018, estimates the survival probability of patients admitted to the ICU after experiencing hypothermic OHCA and undergoing inhospital ECPR [5]. Due to the frequent absence of serum potassium levels in the prehospital setting, our score calculations were limited to patients receiving inhospital ECPR. Within this particular group, our analysis revealed a projected survival rate of 30% as predicted by the HOPE score. Similarly, the actual observed survival rate with good neurological outcomes at 28 days was recorded at 6/19 (32%). Nevertheless, the utility of the score could prove advantageous in urban areas with temperate climates for effectively prioritizing hypothermic patients in both prehospital and inhospital scenarios.
Limitations
We wish to acknowledge several limitations in our study. Firstly, the size of our participant group remained modest. Despite the rarity of the phenomenon we were exploring, having a larger number of patients in our study would have improved the statistical strength of our results. This would have been especially valuable for conducting more precise comparisons between prehospital and inhospital ECPR survival rates, as well as for facilitating more effective examinations of various subgroups.
Secondly, due to the retrospective nature of our research and our reliance on medical records, we encountered missing data, notably in relation to electroencephalography, chest computed tomography, and brain imaging. However, it is essential to consider that the patients in our study, as reflected in their prognosis, were highly critical cases following hypothermic refractory OHCA treated with ECPR and were seldom feasible for transport to the Radiology department in such conditions.
An additional constraint was the method used for measuring prehospital external temperatures, which involved an external thermometer. Unfortunately, this method’s reliability was not ideal for accurately representing the actual core temperature. Furthermore, in three cases, we faced challenges where the external thermometer failed to detect extremely low temperatures, making the prehospital external temperature data unavailable. In these situations, we relied on the clinical assessment of hypothermia, which we supplemented with central temperature measurements upon the patients’ admission to the ICU. It is worth noting that this central temperature data did not have any missing values and consistently supported the presence of significant hypothermia in all patients.
Conclusions
Hypothermic refractory OHCA occurred even in urban areas with temperate climates, and survival with good neurological outcomes at 28 days stood at 36% for all patients treated with ECPR. We found no survivors with good neurological outcomes at 28 days in submersed patients.
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ECPR:
-
Extracorporeal Cardiopulmonary Resuscitation
- ROSC:
-
return of spontaneous circulation
- HOPE:
-
Hypothermia Outcome Prediction after ECPR
- ICU:
-
Intensive Care Unit
- SAMU:
-
Service d’aide médicale Urgente
- SAPS II:
-
Simplified Acute Physiology Score II
- RRT:
-
Renal Replacement Therapy
- DIC:
-
Disseminated Intravascular Coagulopathy
- BARC:
-
Bleeding Academy Research Consensus
References
Paal P, Brugger H, Strapazzon G. Accidental hypothermia. Handb Clin Neurol. 2018;157:547–63.
Paal P, Pasquier M, Darocha T, et al. Accidental hypothermia: 2021 update. Int J Environ Res Public Health. 2022;19:501.
Lott C, Truhlář A, Alfonzo A, et al. European Resuscitation Council Guidelines 2021: cardiac arrest in special circumstances. Resuscitation. 2021;161:152–219.
Working group of the French Language Resuscitation Society. Expert formalized recommendations on the management of cardiac arrest. French Language Resuscitation Society (FR). 2006. https://www.srlf.org/wpcontent/uploads/2015/12/2007_recommandations_formalisees_d_experts_arret_cardiaque_texte-court.pdf. Accessed 24 Feb 2023.
Pasquier M, Hugli O, Paal P, et al. Hypothermia outcome prediction after extracorporeal life support for hypothermic cardiac arrest patients: the HOPE score. Resuscitation. 2018;126:58–64.
Pasquier M, Rousson V, Darocha T, et al. Hypothermia outcome prediciton after extracorporeal life support for hypothermic cardiac arrest patients: an external validation of the HOPE score. Resuscitation. 2019;139:321–8.
Lamhaut L, Hutin A, Puymirat E, et al. A pre-hospital extracorporeal Cardio Pulmonary Resuscitation (ECPR) strategy for treatment of refractory out hospital cardiac arrest: an observational study and propensity analysis. Resuscitation. 2017;117:109–17.
Beck HE, Zimmermann NE, McVicar TR, et al. Present and future Köppen-Geiger climate classification maps at 1-km resolution. Sci Data. 2018;5:180214.
Schober A, Sterz F, Handler C, et al. Cardiac arrest due to accidental hypothermia-A 20 year review of a rare condition in an urban area. Resuscitation. 2014;85:749–56.
Sawamoto K, Bird SB, Katayama Y, et al. Outcome from severe accidental hypothermia with cardiac arrest resuscitated with extracorporeal cardiopulmonary resuscitation. Am J Emerg Med. 2014;32:320–4.
Ruttmann E, Dietl M, Kastenberger T, et al. Characteristics and outcome of patients with hypothermic out-of-hospital cardiac arrest: experience from a european trauma center. Resuscitation. 2017;120:57–62.
Svendsen ØS, Grong K, Andersen KS, et al. Outcome after rewarming from Accidental Hypothermia by Use of extracorporeal circulation. Ann Thorac Surg. 2017;103:920–5.
Champigneulle B, Bellenfant-Zegdi F, Follin A, et al. Extracorporeal life support (ECLS) for refractory cardiac arrest after drowning: an 11-year experience. Resuscitation. 2015;88:126–31.
Lamhaut L, Jouffroy R, Kalpodjian A, et al. Successful treatment of refractory cardiac arrest by emergency physicians using pre-hospital ECLS. Resuscitation. 2012;83:177–8.
Lamhaut L, Jouffroy R, Soldan M, et al. Safety and feasibility of prehospital extra corporeal life support implementation by non-surgeons for out-of-hospital refractory cardiac arrest. Resuscitation. 2013;84:1525–9.
French Resuscitation Council; French Society of Anesthesia and Intensive Care; French Society of Cardiology; French Society of Thoracic and Cardiovascular Surgery. French society of Emergency Medicine; French Society of Pediatrics; french-speaking Group of Pediatric Resuscitation and Emergency Medicine; French Society of Perfusion; French Language Society of Resuscitation. Guidelines for indications for the use of extracorporeal life support in refractory cardiac arrest. Ann Fr Anesth Reanim. 2009;28:182–90.
Hutin A, Abu-Habsa M, Burns B, et al. Early ECPR for out-of-hospital cardiac arrest: best practice in 2018. Resuscitation. 2018;130:44–8.
Perkins GD, Jacobs IG, Nadkarni VM, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein Resuscitation Registry Templates for Out-of-hospital cardiac arrest: a Statement for Healthcare Professionals from a Task Force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, critical care, Perioperative and Resuscitation. Resuscitation. 2015;96:328–40.
Le Gall JR, Lemeshow S, Saulnier F. A new simplified Acute Physiology score (SAPS II) based on a european / north american multicenter study. JAMA. 1993;270:2957–63.
Mehran R, Rao SV, Bhatt DL, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the bleeding Academic Research Consortium. Circulation. 2011;123:2736–47.
Phelps R, Dumas F, Maynard C, et al. Cerebral Performance Category and long-term prognosis following out-of-hospital cardiac arrest. Crit Care Med. 2013;41:1252–7.
Kraai E, Wray TC, Ball E, et al. E-CPR in Cardiac arrest due to Accidental Hypothermia using Intensivist Cannulators: a Case Series of nine consecutive patients. J Intensive Care Med. 2023;38:215–9.
Corso M, Pascal M, Wagner V. Impacts de la chaleur et du froid sur la mortalité totale en France entre 2000 et 2010. Bull Epidémiol Hebd. 2017;31:634–40.
Working group of the National Observatory of Poverty and Social Exclusion (FR). Mortality of homeless individuals in France between 2008 and 2010. National Observatory of Poverty and Social Exclusion (FR). 2013. https://onpes.gouv.fr/IMG/pdf/Lettre_ONPES_sept_2013.pdf. Accessed 24 Feb 2023.
Laporte A, Vandentorren S, Détrez MA, et al. Prevalence of Mental Disorders and Addictions among Homeless People in the Greater Paris Area, France. Int J Environ Res Public Health. 2018;15:241.
Walpoth BH, Walpoth-Aslan BN, Mattle HP, et al. Outcome of survivors of accidental deep hypothermia and circulatory arrest treated with extracorporeal blood warming. N Engl J Med. 1997;337:1500–5.
Hilmo J, Naesheim T, Gilbert M. Nobody is dead until warm and dead: prolonged resuscitation is warranted in arrested hypothermic victims also in remote areas - a retrospective study from northern Norway. Resuscitation. 2014;85:1204–11.
Tipton MJ, Golden FS. A proposed decision-making guide for the search, rescue and resuscitation of submersion (head under) victims based on expert opinion. Resuscitation. 2011;82:819–24.
Pasquier M, Paal P, Blancher M, et al. Higher survival chances of hypothermic vs. nor- mothermic cardiac arrest patients with ECLS re-warming. Resuscitation. 2019;134:161–2.
Swol J, Darocha T, Paal P, Brugger H, Podsiadło P, Kosiński S, Puślecki M, Ligowski M, Pasquier M. Extracorporeal life support in Accidental Hypothermia with Cardiac Arrest-A narrative review. ASAIO J. 2022;68:153–62.
Acknowledgements
We would like to thank Necker Hospital Intensive Care Unit team and the team of the SAMU de Paris for their efforts and contributions.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Author A, TS (first author): Conceptualization, Investigation, Writing-Original Draft.
Author B, JHR: Conceptualization, Writing-Review & Editing.
Author C, WB: Methodology, Formal analysis, Writing-Review & Editing.
Author D, DV: Resources.
Author E, HA: Resources.
Author F, SY: Resources.
Author G, CD: Resources.
Author H, KA: Resources.
Author I, AM: Resources.
Author J, PC: Supervision.
Author K, AH: Writing-Review & Editing.
Author L, LL (corresponding author): Supervision, Writing-Review & Editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Registration Number : IRB 00010254 - 2023–015.
This retrospective observational study has been examined by 3 independent rapporteurs who concluded that it does not pose any particular ethical problem and does not fall within the field of application of the regulations governing research involving the human person, as defined in Articles R.1121-1 and R.1121-2.
Dr Valerie BILLARD - Head of CERAR – Comité d’Ethique pour la Recherche en Anesthésie-Réanimation.
Consent for publication
The consent for publication is available from the corresponding author on request.
Competing interests
TS, JHR, DV, HA, YS, CD, KA, AM, PC, declares no competing interests. WB, consulting activity for Withings. AH, Lecture for Getinge. LL, Lecture for Getinge, President of SAUV Life (non-profit organization).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Soumagnac, T., Raphalen, JH., Bougouin, W. et al. Extracorporeal cardiopulmonary resuscitation for hypothermic refractory cardiac arrests in urban areas with temperate climates. Scand J Trauma Resusc Emerg Med 31, 68 (2023). https://doi.org/10.1186/s13049-023-01126-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13049-023-01126-5