Abstract
Background
Patients with electrical injury are considered to be at risk of cardiac arrhythmia. Assessing the risk of developing a major adverse cardiac event (MACE) is the cornerstone of patient management. The aim of this study was to assess the performance of initial troponin and troponin rise to predict Major Adverse Cardiac Events (MACEs) in all patients with electrical injuries admitted to the Emergency Department.
Methods
This is a multicentre retrospective study in which consecutive patients with electrical injuries admitted to the Emergency Departments (ED) (adult and paediatric) of five French Hospitals were included between 2005 and 2019. The threshold for troponin elevation is based on the European Society of Cardiology guidelines for patients presenting without persistent ST segment elevation. The primary endpoint was the rate of MACE.
Results
A total of 785 included patients were admitted to ED with a first diagnosis of electrical injury during the study period. Troponin assays were performed in 533 patients (67.9%), including 465 of 663 adults (70.1%) and 68 of 122 children (55.7%) and 17/533 (3.2%) of patients had an initial elevated troponin. If none of the clinical criteria for MACE were present (i.e., previous known heart disease, exposure to a high voltage of ≥ 1000 Volts, initial loss of consciousness, or an abnormal initial ECG), this defined a low-risk subgroup (n = 573, 76.0%) that could be safely discharged. The initial positive troponin assay had a sensitivity of 83.3 (95% CI 35.9–99.6%), a specificity of 97.7 (95% CI 96.1–98.8%), a positive likelihood ratio 36.6 (95% CI 18.8–71.1%) and a negative predictive value of 99.9 (95% CI 99.2–99.9%) in predicting a MACE.
Conclusions
Troponin assay appears to be a predictive marker of MACE risk and should be considered in high-risk patients.
Similar content being viewed by others
Background
Electrical injuries can cause immediate respiratory and cardiac arrest as well as heart failure, cardiomyopathy and myocardial infarction [1,2,3]. However, electrical injuries are very varied and heterogeneous, ranging from minor injuries or burns to life-threatening damage to internal organs or significant long-term morbidity [1, 4,5,6,7]. The two major cardiac complications of electrical shock are arrhythmias and myocardial tissue injuries. These cardiac events are infrequent following an electrical injury, especially in cases of low voltage (mortality rates = 0–2.6%) [8, 9]. Most cardiac events occur immediately after the accident resulting from the proarrhythmic effect of electric shock, but delayed ventricular arrhythmias have also been reported in rare cases [10]. Most studies did not report a delayed events [11,12,13,14].
The major issue in electrical accidents lies primarily in the risk stratification of developing a serious cardiac event in order to identify a large subgroup of low-risk patients where rapid discharge is safe and of those at a high-risk requiring Electrocardiogram (ECG) monitoring in an intensive care unit. ECG on admission appears to be the most predictive element of cardiac complications. Most cardiac arrhythmias in patients following electrical injury can be diagnosed by an initial ECG [1, 15]. The risk of serious cardiac arrhythmia is considered high in patients corresponding to four main criteria: previous known heart disease and/or exposure to a high voltage ≥ 1000 Volts or/and with initial loss of consciousness and/or an abnormal initial ECG [1, 15,16,17]. Troponin assays are controversial following electrical injury. In the practical algorithm of the recommendations published in Eur Heart Journal in 2018, it is suggested to perform a systematic assay of troponin and monitoring of troponin elevation. The text highlightsthat "no significant studies exist concerning the usefulness of troponin in these clinical situations" [1]. However, other authors do not recommend it in routine practice for all patients due to the lack of assessment [18, 19]. The European Resuscitation Council (ERC) guidelines do not mention the usefulness of biological markers after an electrical injury in special circumstances [20].
Study aims
The main aim of this study was to assess the performance of initial troponin and troponin elevation in order to predict Major Adverse Cardiac Events (MACEs) in all patients with electrical injuries admitted to the ED. Our population of interest did not include the most serious patients with major trauma, severe burns or direct admission to the ICU. The secondary objective was to evaluate the appropriateness of troponin assays in subgroups classified as low risk and those classified as high risk by clinical and ECG evidence. We aimed to isolate a group of low-risk patients who could be rapidly and safely discharged from the ED by clinical criteria without the need for biological testing. We hypothesised that troponin could identify patients at risk of MACE after an electrical injury.
Methods
Study design and setting
This is a multicentre retrospective study. Consecutive patients with electrical injuries admitted to the Emergency Departments (ED) (adult and paediatric) of five French Hospitals were included. From these five centres, two EDs are University Hospital Centres (average ED admissions in 2019: 100,000 (70,000 in the adult department and 30,000 in the paediatric department), one is a High-Capacity Hospital Centre (average admissions in 2019 > 60,000) and two are Low-Capacity Hospital Centres (average admissions in 2019 < 60,000). These 5 hospitals cover a defined population in the west of France. In these ED, patients older than 16 years are referred to the adult ED managed by emergency physicians, and younger patients are referred to the paediatric department managed by paediatricians. None of the 5 centres had a well-established protocol for the management of patients suffering from electrical injuries. The STARD recommendations were followed for the reporting of diagnostic studies [21].
Firstly, we will describe the outcome of the entire cohort. Secondly, we will assess the predictive value of troponin in patients who had a troponin assay. Thirdly, we will perform a subgroup analysis according to risk factors to position troponin testing in a relevant as possible wat in the management of patients.
Participants
We extracted all discharges records of ED patients from a 15-year period (2005–2019) with the corresponding ICD-10 codes as the principal diagnosis (“Appendix”). The most affected victims (i.e., out of hospital cardiac arrest, extensive burns, severe rhythmic disorders, comatose patients or early MI) were treated outside the hospital by an Emergency Medical Service (EMS) and were not included in this study because they were referred directly to an intensive care unit (ICU) or an operating room without being admitted to the ED. Clinical data were obtained from the hospital information system and patient records. Baseline demographics, medical history, and antiarrhythmic medication were registered along with the location, time, and circumstances of the electrical injury. Furthermore, all clinical parameters which are deemed to be risk factors for cardiac arrhythmias based on the ERC criteria were summarised. We also recorded presenting symptoms, severity of burns, and other injuries.
Measurements
The threshold for troponin elevation is based on the European Society of Cardiology guidelines for patients presenting without persistent ST segment elevation as there are no specific prospective data available on this specific population affected by electrical accidents [22]. From 2005 to 2011, the laboratories of the five centres measured troponin T and the threshold was set at 0.03 μg l−1 according to the manufacturer’s guidelines; from 2011, high-sensitivity troponin T was used. We used the manufacturer’s recommended 99th percentile upper reference limit (URL) to reduce site-to-site variability when determining the cut-off point. A significant increase in troponin was defined as an increase of at least 10 ng/l within 6 h or 6 ng/l within 3 h as per the manufacturer’s guidelines.
Outcomes
The primary endpoint was the rate of Major Adverse Cardiac Events (MACEs) from admission to the ED until discharge or during hospitalisation or upon re-presentation to the ED or in another department of the referral hospital within 30 days. MACE was a composite measure defined as (i) acute myocardial infarction according to the Fourth Universal Definition of Myocardial Infarction, Myocardial Infarction with No Obstructive Coronary Arteries (MINOCA), myocarditis or Tako-Tsubo Syndrome [23], (ii) sustained Ventricular Tachycardia (VT) or Ventricular Fibrillation (VF) according to the definition provided by the American Heart Association [24], (iii) in-hospital cardiac arrest with return of spontaneous circulation (ROSC), (iv) death from any cause. Patients diagnosed with unstable angina or myocardial injuries not meeting the previously stated criteria were not considered as having suffered a MACE.
The secondary endpoint was the rate of cardiac events during in-hospital monitoring or upon re-presentation to the ED or in another department of the referral hospital within 30 days. A cardiac event includes MACE and the need for cardiac treatments (revascularisation and/or cardiac medication), non-sustained VT, arrythmias including sinus tachycardia (more than 30 min), atrial tachyarrhythmia or bradyarrhythmia requiring monitoring and/or treatment.
Ethics
Due to the non-interventional retrospective nature of the current study no informed consent was required (Deliberation no. 2016-262, 2016-263, CNIL MR-003). Ethical approval for this study was obtained from the Nantes Research Ethics Committee (Groupe Nantais d’Ethique dans le Domaine de la Santé, GNEDS).
Statistical analysis
Continuous variables are presented with their median, first and third quartiles (Q1–Q3). Categorical variables are summarised with the number of patients and percentage with a 95% confidence interval (95% CI). The Chi-squared test, Fisher’s exact test, Student’s t-test and the Mann–Whitney U test were used when appropriate (two-tailed; level of significance p < 0.05).
To assess the performances of the initial troponin aim 7 say and the second troponin assay for predicting the primary endpoint, we assessed diagnostic performances (sensitivity, specificity, negative and positive predictive values, negative and positive likelihood ratio and accuracy).
Performances of the 4 high-risk clinical items combined (with prior known heart disease and/or exposure to a high voltage of ≥ 1000 Volts and/or with initial loss of consciousness or/and an abnormal initial ECG) were assessed to predict MACE. This item is considered as positive if one or more item was present. The aim is to identify simple clinical criteria to isolate a group of patients who will not have MACE (i.e., < 1%) without the need for a bioassay, for a safe ED rule out.
A subgroup analysis was performed in low-risk patients and in high-risk patients using the same endpoint. Patients without ECG at baseline were excluded from this analysis.
All statistical analyses were 2-tailed, and a p value less than 0.05 was required for statistical significance. No imputation of missing data was performed. Since occurrences of electrical injuries are rare, we did not determine a necessary sample size. All statistical analysis was performed using R Statistical Software (version 4.0.3; R Foundation for Statistical Computing, Vienna, Austria) (URL https://www.R-project.org/).
Results
A total of 875 patients were admitted to hospitals with a first diagnosis of electrical injuries during the study period. Ninety were excluded for various reasons which are summarised in Fig. 1. The population incidence for patients severely injured admitted directly to ICU was 0.21 per 100,000 person-years (95% CI 0.17–0.26) and of 1.87 per 100,000 person-years (95% CI 1.74–2.00) for moderate or less injured patients admitted to the ED. The final analysis assessed 785 patients (663 adults (84.5%) and 122 children (15.5%)) (Table 1). The sex ratio was 0.33 (193 women/59 men2) and the median age was 30 years.
Flow diagram. *According to the 4 high-risk clinical items combined (previous known heart disease, exposure to a high voltage of ≥ 1000 V, initial loss of consciousness, abnormal initial ECG); if ≥ 1 items = high risk patients. Missing data, n = 31. **Initial elevated troponin and/or significant rise on the 2nd essay. MACE Major Adverse Cardiac Even
An ECG was performed in 756 patients (96.3%) and results were abnormal in 99 cases (12.6%) with the occasional association of several anomalies (Table 1). The most frequent electrocardiographic observations were non-specific ST-T changes (n = 47/99, 47.5%), incomplete right bundle branch block (n = 27/99, 27.3%), sinus tachycardia (> 100 bpm) (n = 16/99, 16.2%), first-degree atrioventricular block (n = 6/99, 6.1%), ventricular extrasystole (n = 5/99, 5.1%), significant ST-elevation (n = 4/99, 4.0%), sinus bradycardia (< 60 bpm) (n = 3/99, 3.0%), ventricular pre-excitation syndrome (n = 1), non-sustained VT (n = 1).
Troponin assays were performed in 533 patients (67.9%), of which 465 of 663 were adults (70.1%) and 68 of 122 were children (55.7%). An initial elevated troponin was observed in 17/533 (3.2%) of patients. In total, 197/533 patients (37.0%) received a new troponin assay at a median of 6 [4,5,6,7,8,9,10,11] hours after the first assay. Eight presented an increase of the initial troponin (including 6 patients with initial positive troponin).
Six patients suffered a MACE (6/785, 0.76% (95% CI 0.04–1.66%) (Additional file 1: Table S1). Among them, 3 suffered VF/VT with subsequent fatal cardiorespiratory arrest (one had a STEMI on the initial ECG), 2 had sustained VT and one patient had a Tako-Tsubo diagnosis according to the International Takotsubo Diagnostic Criteria [25]. The overall patient mortality was 0.38% (95% CI 0.13–1.12%) consisting of which 2 adults n = 2/663 (0.30%, 95% CI 0.08–1.09%) and one child n = 1/122 (0.82%, 95% CI 0.14–4.5%). All MACE or deaths occurred during the initial ED work-up (< 24 h) and none during hospitalisation. A total of 13 patients suffered a cardiac event, including patients with MACE (Additional file 2: Table S2).
In the univariate model, age, cardiac history, initial loss of consciousness, transthoracic current, abnormal initial ECG, positive initial troponin assay and troponin elevation were significantly associated with MACE occurrence (Table 2).
Troponin performances
Prognostic performances of the initial positive troponin assay to predict MACE are summarised in Table 3. Among the patients with initial positive troponin (n = 17), 5 suffered a MACE (29.4%) and among them two had abnormal ECG on admission (significant ST-elevation). To predict a MACE, the initial positive troponin assay had a sensitivity of 83.3 (95% CI 35.9–99.6%), a specificity of 97.7 (95% CI 96.1–98.8), a positive likelihood ratio of 36.6 (95% CI 18.8–71.1%) and a negative predictive value of 99.9 (95% CI 99.2–99.9%) (Table 4). The troponin rise had a sensitivity of 33.3 (95% CI 4.3–77.7%), a specificity of 99.2 (95% CI 98.3–99.7%), a positive likelihood ratio of 43.3 (95% CI 10.8–172.7%) and a negative predictive value of 99.5 (95% CI 99.1–99.7%). Of the patients with an initially elevated troponin, only one was asymptomatic. The patient did not receive troponin monitoring and was monitored for 24 h without the occurrence of a MACE.
Subgroup analysis
The 4 high-risk clinical items combined separated the low-risk patients (n = 573, 76.0%) from the high-risk patients (n = 181, 24.0%) (Table 4 and Additional file 1: Table S1).
In the low-risk group, no patient had a MACE or died and 4 patients had a cardiac event (3 sinus bradycardia and 1 sinus tachycardia). A total of 65 patients without any symptoms were hospitalised for monitoring. In the whole population the 4 high-risk clinical items combined had a sensitivity of 100 (95% CI 54.1–100.0%), a specificity of 76.6 (95% CI 73.4–79.6%) and a negative predictive value of 100 (95% CI 99.9–100%) to predict or exclude a MACE (Table 3).
In the high-risk group, 6 patients had a MACE (prevalence of 3.3% (95% CI 1.5–7.0%), of which 3 died (prevalence of 1.6% [95% CI 0.6–4.7%]) (i.e., one patient died in the ED and two patients during hospitalisation), and 9 had cardiac events. In the high-risk group, the initial positive troponin assay had a sensitivity of 83.3 (95% CI 35.9–99.6%), a specificity of 95.2 (95% CI 90.4–98.1%) a negative predictive value of 99.3 (95% CI 95.9–99.9%) and a positive likelihood ratio of 17.5 (95% CI 7.8–39.2%).
Discussion
The occurrence of MACE is rare following an electrical accident. Troponins could be a relevant marker in electrical accidents for predicting MACE. However, the excellent sensitivity and negative predictive value of the “4-high-risk clinical items combined” represent it the first step in risk stratification.
In this study, the troponin assay was performed in 68% of all patients in the ED and in 55.7% of children. Although there are no clear recommendations for adults, some authors do not recommend the use of troponin assays for children, except for victims of high-voltage electrical exposure, lightning strikes, and severe burns [26]. In the absence of clear guidelines, actual practices differ. Indeed, Searle et al. found that troponin assays were being used in 94% in adults and 55% in children, while Bailey et al. found a rate of 64% in high-risk patients [27, 28]. We observed that the patient’s initial risk assessment had little impact on troponin assay with a rate of 66.3% in the low-risk subgroup.
Here, we found elevated troponin in only 2.2% of patients admitted to the emergency department. In a retrospective study, Choi et al., found elevated troponin in 72.9% of patients with cardiac complications (n = 78/107) [29]. Only one child had an elevated troponin level. Searle et al. also reported that the troponin was rarely elevated, with only 2 out of 144 adults and no children exhibiting troponin elevation [27]. Even in high-risk patients, Bailey et al. found that all were at or below the detection limit [28]. However, Gokdemir et al. found 3 children out of 36 with elevated troponin after a low-voltage electrical injury, but this did not affect mortality [30].
In our study, the 4-high-risk clinical items combined which are prior known heart disease and/or exposure to a high voltage ≥ 1000 Volts and/or with initial loss of consciousness and/or an abnormal initial ECG obtained excellent values to exclude the occurrence of MACE (sensitivity 100% and negative predictive value 100%). Only 4 cardiac events occurred but had no negative impact on patients. Using this first step in risk stratification enables the identification of a large low-risk subgroup (76%, n = 573/754) that can be rapidly discharged from the emergency department with only an initial examination and an ECG. Indeed, this strategy would allow a rapid and safe discharge of most patients, which would limit the waiting time of these patients and others by repercussion, and avoid the overcrowding encountered in the ED [31]. These 4 items are those found in the literature and were recently proposed by Waldman [1].
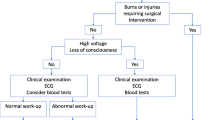
In the whole population, the sensitivity of troponin value in predicting cardiac events was intermediate (83%) but had a large confidence interval due to the low rate of MACE. The same performances were obtained in the high-risk subgroup. Given the high level of specificity, the troponin could identify MACE in all patients that suffer electrical accidents. However, it seems unnecessary to add bioassays in the subgroup of low-risk patients for the performance of the clinical items alone. It may therefore be appropriate to reserve troponin dosing and control for high-risk patients. In this study, we focused only on troponin and not on creatine kinase-MB. Cardiac troponin T has been recognised as the most sensitive and specific cardiac enzyme for the diagnosis of myocardial injury in general. Data indicate that creatine kinase-MB is an unreliable marker for electrical injuries because of an inadequate sensitivity and potential confusion with peripheral skeletal muscle injury [4]. On the basis of this study, a standardised approach is conceivable, combining the ERC recommendations with the criteria evaluated by Blackwell et al. and Waldmann et al. (Fig. 2) [1, 14]. This study does not allow this algorithm to be reliably validated, but it is clear that performing troponins in all patients presenting to the ED without having previously assessed clinical severity items for electrical injuries does not seem useful. Multiplying tests in the ED was associated with prolonged length of stay and an increase in the use of resources [32]. Various strategies for securely decreasing the number of complementary exams are being implemented to combat frequent ED overcrowding [33]. However, the risk assessment in our study was probably biased due to its retrospective design. Indeed, there was no standard of care and it is possible that patients considered at low-risk did not have troponins or ECG. For high-risk patients, a small subgroup of patients could be admitted directly to the ICU.
Flowchart for a standard protocol for patients with electrical injury (based on the paper by Waldmann et al. [1]). *No prospective data available, a procedure in line with the acute coronary syndrome is recommended: follow-up 12-channel ECG, troponin after 6 h and, if necessary, after 12–24 h (ERC)
MACEs occurred during the initial ED workup. This is consistent with previous studies that found a non-existent or low risk of developing MACE at a distance from the electrification injury [10, 12, 13]. In 1986, Purdue et al. asked whether monitoring for all patients was a “necessity or a luxury” and proposed the use of clinical history and ECG as a basis for patient selection [34]. In our study, 65 patients at low risk were hospitalised without any symptoms in order to be monitored.
In our series, we found a case of Tako-Tsubo syndrome after a low voltage electrical injury in a 65-year-old woman. This is a rare case but has already been described in the literature [35]. It is difficult to assess whether the electrical injury was an emotional trigger or a physical trigger [25].
In the context of a rare and heterogeneously managed disease leading to inconsistent guidelines, one of the strengths of this study was its multicentric design and its significant number of patients.
Limitations
First of all, there were very few cases of troponin elevation and few MACEs occurred, thus limiting the statistical power of the study. However, creating larger databases on this condition appears to be very difficult due to its low prevalence. Secondly, due to the retrospective design of the study many data could not be collected and there may be an information bias. A large-scale prospective study would be required to validate the findings of this retrospective study. The third limitation was the lack of availability of the length of stay in the ED and the delay between the accident and the occurrence of MACE, which resulted in a lack of support for our conclusions regarding the monitoring period. Lastly, it is possible that early discharge patients may have had a secondary MACE but this would potentially have been accounted for in referral hospital records.
Conclusions
Patients with an electrical injury have a highly variable risk of major adverse cardiac events. It is necessary to perform risk stratification based initially on clinical items and an ECG to safely discharge a large subgroup of patients from the ED. This will also likely help reserve troponin assays, control and patient monitoring for those at high risk.
Availability of data and materials
Available upon reasonable request.
Change history
19 October 2021
A Correction to this paper has been published: https://doi.org/10.1186/s13049-021-00968-1
Abbreviations
- 95% CI:
-
95% Confidence Interval
- ED:
-
Emergency Department
- ECG:
-
Electrocardiogram
- EMS:
-
Emergency Medical Service
- ERC:
-
European Respiratory Council
- ESC:
-
European Society of Cardiology
- ICU:
-
Intensive Care Unit
- MACE:
-
Major Cardiac Event
- MINOCA:
-
Myocardial Infarction with No Obstructive Coronary Arteries
- ROSC:
-
Return Of Spontaneous Circulation
- STEMI:
-
ST-Elevation Myocardial Infarction
- URL:
-
Upper Reference Limit
- VF:
-
Ventricular Fibrillation
- VT:
-
Ventricular Tachycardia
References
Waldmann V, Narayanan K, Combes N, Jost D, Jouven X, Marijon E. Electrical cardiac injuries: current concepts and management. Eur Heart J. 2018;39(16):1459–65.
Spies C, Trohman RG. Narrative review: Electrocution and life-threatening electrical injuries. Ann Intern Med. 2006;145(7):531–7.
Bailey B, Forget S, Gaudreault P. Prevalence of potential risk factors in victims of electrocution. Forensic Sci Int. 2001;5:58–62.
Waldmann V, Narayanan K, Combes N, Marijon E. Electrical injury. BMJ. 2017;357:j1418.
Leibovici D, Shemer J, Shapira SC. Electrical injuries: current concepts. Injury. 1995;26(9):623–7.
Biering K, Vestergaard JM, Nielsen KJ, Carstensen O, Kærgaard A. Contacts with general practitioner, sick leave and work participation after electrical injuries: a register-based, matched cohort study. Occup Environ Med. 2021;78(1):54–60.
Stockly OR, Wolfe AE, Espinoza LF, Simko LC, Kowalske K, Carrougher GJ, et al. The impact of electrical injuries on long-term outcomes: a Burn Model System National Database study. Burns. 2020;46(2):352–9.
Pawlik AM, Lampart A, Stephan FP, Bingisser R, Ummenhofer W, Nickel CH. Outcomes of electrical injuries in the emergency department: a 10-year retrospective study. Eur J Emerg Med. 2016;23(6):448–54.
Shih JG, Shahrokhi S, Jeschke MG. Review of adult electrical burn injury outcomes worldwide: an analysis of low-voltage vs high-voltage electrical injury. J Burn Care Res. 2017;38(1):e293–8.
Jensen PJ, Thomsen PE, Bagger JP, Norgaard A, Baandrup U. Electrical injury causing ventricular arrhythmias. Heart. 1987;57(3):279–83.
Ahmed J, Stenkula C, Omar S, Ghanima J, Bremtun FF, Bergan J, et al. Patient outcomes after electrical injury—a retrospective study. Scand J Trauma Resusc Emerg Med. 2021;29(1):114.
Hansen SM, Riahi S, Hjortshøj S, Mortensen R, Køber L, Søgaard P, et al. Mortality and risk of cardiac complications among immediate survivors of accidental electric shock: a Danish nationwide cohort study. BMJ Open. 2017;7(8):e015967.
Arrowsmith J, Usgaocar RP, Dickson WA. Electrical injury and the frequency of cardiac complications. Burns. 1997;23(7–8):576–8.
Blackwell N. A three year prospective audit of 212 presentations to the emergency department after electrical injury with a management protocol. Postgrad Med J. 2002;78(919):283–5.
Pilecky D, Vamos M, Bogyi P, Muk B, Stauder D, Racz H, et al. Risk of cardiac arrhythmias after electrical accident: a single-center study of 480 patients. Clin Res Cardiol. 2019;108(8):901–8.
Petroni T, Moubarak G, Varenne O, Weber S, Duboc D. Do we need to systematically hospitalize electrocuted patients in ICU? Int J Cardiol. 2011;152(3):410–1.
Cunningham PA. The need for cardiac monitoring after electrical injury. Med J Aust. 1991;154(11):765–6.
Arnoldo B, Klein M, Gibran NS. Practice guidelines for the management of electrical injuries. J Burn Care Res. 2006;27(4):439–47.
Says F. Electrical Injuries. RCEMLearning [cited 2021 Feb 2]. https://www.rcemlearning.co.uk/reference/electrical-injuries/.
Truhlář A, Deakin CD, Soar J, Khalifa GEA, Alfonzo A, Bierens JJLM, et al. European resuscitation council guidelines for resuscitation 2015. Resuscitation. 2015;95:148–201.
Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig L, et al. STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. BMJ. 2015;351:h5527.
Thiele H, Barbato E, Barthelemy O, Bauersachs J, Bhatt DL. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation; 79.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction. J Am Coll Cardiol. 2018;72(18):2231–64.
Al-Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, Curtis AB, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: executive summary. Heart Rhythm. 2018;15(10):e190-252.
Ghadri J-R, Wittstein IS, Prasad A, Sharkey S, Dote K, Akashi YJ, et al. International expert consensus document on Takotsubo syndrome (part i): clinical characteristics, diagnostic criteria, and pathophysiology. Eur Heart J. 2018;39(22):2032–46.
Roberts S, Meltzer JA. An evidence-based approach to electrical injuries in children. Pediatr Emerg Med Pract. 2013;10(9):1–16 (quiz 16–7).
Searle J, Slagman A, Maaß W, Möckel M. Cardiac monitoring in patients with electrical injuries. Deutsches Aerzteblatt Online. 2013. https://doi.org/10.3238/arztebl.2013.0847.
Bailey B, Gaudreault P, Thivierge RL. Cardiac monitoring of high-risk patients after an electrical injury: a prospective multicentre study. Emerg Med J. 2007;24(5):348–52.
Choi JH, Han D, Kang S-H, Yoon C-H, Cho JR, Kym D. Retrospective study of prognosis and relating factors of cardiac complications associated with electrical injuries at a single centre in Korea. BMJ Open. 2019;9(7):e028741.
Gokdemir MT, Kaya H, Söğüt Ö, Cevik M. Factors affecting the clinical outcome of low-voltage electrical injuries in children. Pediatr Emerg Care. 2013;29(3):357–9.
Li L, Georgiou A, Vecellio E, Eigenstetter A, Toouli G, Wilson R, et al. The effect of laboratory testing on emergency department length of stay: a multihospital longitudinal study applying a cross-classified random-effect modeling approach. Acad Emerg Med. 2015;22(1):38–46.
Kocher KE, Meurer WJ, Desmond JS, Nallamothu BK. Effect of testing and treatment on emergency department length of stay using a national database: effect of testing and treatment on ED LOS. Acad Emerg Med. 2012; 19(5):525–34.
Nazerian P, Vanni S, Fanelli A, Fallai L, Duranti C, Ognibene A, et al. Appropriate use of laboratory test requests in the emergency department: a multilevel intervention. Eur J Emerg Med. 2019;26(3):205–11.
Purdue GF, Hunt JL. Electrocardiographic monitoring after electrical injury: necessity or luxury. J Trauma. 1986;26(2):166–7.
Hayashi M, Yamada H, Agatsuma T, Nomura H, Kitahara O. A case of takotsubo-shaped hypokinesis of the left ventricle caused by a lightning strike. Int Heart J. 2005;46(5):933–8.
Funding
None.
Author information
Authors and Affiliations
Contributions
IA, FJ, DD conceived the overarching study. KS, AY, BG collected the patients. DD, IA, FJ, SD, LBQ, KS, AY, GB made substantial contributions to the protocol and this article. All authors take responsibility for this paper as a whole. All authors contributed critical analysis, interpretation and writing within all drafts and approved the final draft for submission. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval for this study was obtained from the Nantes Research Ethics Committee (Groupe Nantais d’Ethique dans le Domaine de la Santé, GNEDS).
Consent for publication
Not applicable.
Competing interests
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised to correct the authors' given and family names, that had inadvertently been interchanged.
Supplementary Information
Additional file 1: Table S1.
Characteristics of patients who suffered from MACE.
Additional file 2: Table S2.
Management and outcomes of patients according to their risk classification*.
Appendix
Appendix
See Table 5.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Douillet, D., Kalwant, S., Amro, Y. et al. Use of troponin assay after electrical injuries: a 15-year multicentre retrospective cohort in emergency departments. Scand J Trauma Resusc Emerg Med 29, 141 (2021). https://doi.org/10.1186/s13049-021-00955-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13049-021-00955-6