Abstract
Background
To reduce the possibility of secondary deterioration of spinal injuries, it is desirable to maintain the spinal immobilisation that is applied in the prehospital setting throughout computed tomography (CT) scanning. A previous study found that metallic components within the inflation valve of the vacuum mattresses caused CT artefacts. The aim of our study was to investigate the effect of vacuum mattresses with plastic valves on CT artefacts, the radiation dose, and noise compared to a trauma transfer board and the spine boards currently used in our trauma system.
Methods
We scanned an anthropomorphic whole body phantom with different immobilisation devices on a 128-slice CT scanner using the standard polytrauma CT-protocol at our institution. The phantom was scanned without any immobilisation device and with three different vacuum mattresses, two spine boards, and one trauma transfer board. Two radiologists independently assessed the artefacts. Agreement between the two radiologists was measured using the kappa coefficient. The radiation dose and noise were assessed.
Results
One spine board produced major artefacts due to its metal components. One of the vacuum mattresses resulted in artefacts that impaired clinical judgement. Otherwise, the artefacts predominantly did not impede clinical judgement and were mainly subtle. One of the vacuum mattresses resulted in no artefacts that affected clinical judgement. The overall inter-rater agreement was substantial (0.86, kappa 0.77). We did not observe any artefacts due to plastic valves. The mean CT radiation dose was slightly higher for two of the devices in the head series than that for the trauma transfer board, used as the standard in our system. Only marginal differences were noted for the other devices and series. Small differences in image noise were found between the devices.
Conclusions
Our results indicate that it is feasible to maintain some vacuum mattresses with plastic valves on trauma patients during CT scanning. The tested mattresses did not result in a considerably increased radiation dose or artefacts that hampered clinical judgement. One of the tested vacuum mattresses produced no artefacts that hampered clinical judgement whatsoever.
Similar content being viewed by others
Background
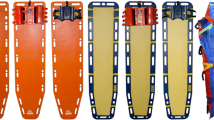
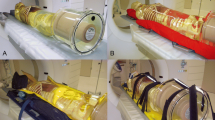
In trauma care, different devices are used to restrain motion in possible spinal injury cases to prevent secondary deterioration [1, 2]. Some examples include semi-rigid cervical collars and spine boards. However, a growing concern exists that these devices may harm the patient [3, 4]. A vacuum mattress is a deflatable whole body mattress containing small plastic beads. The mattress is moulded around the patient and deflated, leaving the device hardened to reduce spinal motion (Fig. 1). The vacuum mattress is gaining popularity in emergency medical services systems in Europe and is thought to offer equal or superior support and comfort compared to spine boards [5,6,7]. In our trauma system, spine boards and vacuum mattresses are normally removed in the emergency department, and patients are transferred for computed tomography (CT) scanning on a trauma transfer board. To reduce the possibility of secondary deterioration in spinal injury, it is desirable to maintain proper spinal immobilisation applied before hospital arrival through CT scanning. We propose to deactivate (inflate) the vacuum mattress upon arrival in the trauma bay, perform the needed survey and treatment, and reactivate (deflate) the vacuum mattress prior to transfer for CT scanning.
However, personal reports have indicated that a vacuum mattress may considerably reduce diagnostic quality. Recent studies indicate that immobilising head blocks both increase radiation and produce noise and artefacts that to some extent impair clinical judgement [8, 9]. Euler et al. recently demonstrated that whole body CT could be performed on trauma patients who are immobilised in vacuum mattresses without a relevant effect on the radiation dose or image quality, provided that the metallic valve in the vacuum mattress is not placed centrally, which is often the case [10]. In most of these cases, the device typically must be removed. Our theory was that modern immobilisations devices without metal parts may cause less artefacts and noise at acceptable radiation doses, and thereby facilitate the use of these devices through a CT scanning. The aim of our study was to investigate the effect of vacuum mattresses with plastic valves on CT artefacts, the radiation dose, and noise compared to a trauma transfer board and the spine boards currently used in our trauma system. As some immobilisation devices has large metal components that might generate artefacts on CT images, we also wanted to investigate the possibility of minimizing these during CT image reconstruction using metal artefact reduction algorithm currently available to us.
Methods
To cover all technical and practical issues, the study group included members covering the treatment chain from the trauma site (paramedic), emergency department (anaesthesiologist and Head of Trauma), trauma CT-acquisition (radiographer), interpretation (radiologists), and radiation dose/quality control (physicist).
Phantom and immobilisation devices
To avoid irradiation of live patients, we used an anthropomorphic whole body phantom (PBU-60, Kyoto Kagaku Co. LTD, Kyoto, Japan). With a weight of 50 kg and height of 165 cm, the phantom resembles a small European adult patient with a synthetic skeleton, soft tissue, liver, kidneys, and vessels (Fig. 2). We performed scans using three different vacuum mattresses, two spine boards, and one trauma transfer board (Table 1). For these scans we also applied a standard semi-rigid cervical collar (Ambu Perfit Ace; Ambu, Ballerup, Denmark). In addition the phantom was scanned without any immobilisation device as a reference examination. All vacuum mattresses had a plastic valve placed in the chest/abdomen area. One spine board was made entirely of polyethylene plastic (Ambu Najo, Ferno, Brendale, Australia), while the other had metal connections (CombiCarrier II, Hartwell Medical, Carlsbad, California, USA). All vacuum mattresses were moulded around the phantom and activated (deflated) prior to CT scanning.
CT protocol
We performed the scans on a 128-slice CT scanner (SOMATOM Definition Flash, Siemens Healthcare, Forchheim, Germany) with automatic exposure control (CAREDOSE 4D, Siemens) and automatic tube potential selection (CAREkV, Siemens). For head, neck, chest, and abdomen protocols, the reference tube current values were 390, 180, 75, and 206 mAs, respectively. For this phantom, the automatic programme chose 100 kV for the abdominal series and 120 kV for all other series. We positioned the arms along the trunk during the head and neck series and above the head during the chest and abdomen series. A metal artefact reduction algorithm (IMAR, Siemens) was available on our machine. IMAR is shown to reduce large metal artefacts in reconstruction of CT images [11]. We limited testing of IMAR to Spine board 1 (case 8, Table 1), being the only immobilisation device with large metal components.
As we were not accustomed to working with CT scans of phantoms, a reference scan was acquired and made available during the evaluation for comparison. We applied both soft tissue and bone reconstruction filters as well as iterative reconstruction (SAFIR, Siemens) for all series.
Assessments
Two specialists in radiology independently reviewed all CT scans regarding artefacts and were blinded to the type of device. The order of the CT scans was randomised before reviewing.
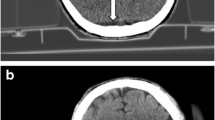
The artefacts were categorised as no artefacts (category 1), artefacts not impeding clinical judgement (category 2), artefacts impeding clinical judgement (category 3), and artefacts rendering the investigation unsuitable for clinical judgement (category 4) (see examples of artefacts in Fig. 3a-d). Artefacts not visualised inside the phantom were classified as category 2. In the head series, however, even minor artefacts visualised inside the phantom were regarded as category 3, as they could obscure small but significant injuries. Agreement between the two radiologists was assessed using the kappa coefficient.
To assess the radiation dose, we used the Computed Tomography Dose Index Volume (CTDIvol) and dose length product (DLP). The effective dose for all CT series per device was estimated based on conversion factors from American Association Physicists in Medicine (AAPM) report 96 [12]. The effective dose for each scan was compared to the dose for the trauma transfer board which is the standard devise used in our trauma system.
To allow for noise evaluation, we performed each acquisition twice, as we exclusively used an anthropomorphic phantom. We estimated noise using the standard deviation of the difference in density (CT numbers) between the two acquisitions as follows:
\( Noise=\frac{SD\left({I}_1-{I}_2\right)}{\sqrt{2}} \)
where I1 and I2 are the image intensities of series 1 and 2, respectively, and SD is the standard deviation.
Results
The two radiologists agreed on 24 of 28 evaluations regarding artefacts (Table 2). The observed agreement was 0.86 with a kappa of 0.77. Fig. 3a-d shows examples of artefacts. Spine board 1 produced major artefacts due to its metal components. Vacuum mattress 3 also resulted in a category 3 artefact in the head series. Otherwise, the artefacts predominantly did not impair clinical judgement. We mainly observed subtle artefacts. The more prominent artefacts were primarily beam-hardening artefacts due to the folding of the mattress surface. The plastic valves in the vacuum mattresses did not create artefacts.
There is a small increase in CT radiation dose output (CTDIvol) for scans acquired with an immobilization device compared to no device. Most notable increase in CTDIvol was in the head and chest series. For the head series, the dose output increased with 14 and 10% for spine board 1 and vacuum mattress 3 respectively. For the chest series, the two largest increases in dose output was 19 and 14% for vacuum mattress 2 and vacuum mattress 3 respectively (Table 3). The impact on the automatic exposure control from the devices is shown in Fig. 4.
All scans with an immobilization device had an increased effective dose compared to trauma transfer board, except spine board 1 that was marginally lower (Table 4).
The noise profile across the CT series for each device (Fig. 5) shows only minor variations in image noise for each device. Mean image noise varied slightly. Compared to trauma transfer board the most notable difference was a 9 % increase in noise for vacuum mattress 2 and 6 % decrease for vacuum mattress 1 (Table 4).
The artefacts were categorised independently by the two radiologists as no artefacts (category 1), artefacts not impeding clinical judgement (category 2), artefacts impeding clinical judgement (category 3), and artefacts rendering the investigation unsuitable for clinical judgement (category 4).
Discussion
We found substantial agreement between the two radiologists regarding artefact assessment. We did not observe any artefacts due to plastic valves. We observed beam hardening artefact (streak artefact) from the mattress canvas and combined beam hardening and metal artefacts from the metal components restricted to spine board 1.
Vacuum mattress 1 caused no artefacts that impeded clinical judgement.
Artefacts in head were subtle for vacuum mattress 2. Category 2 artefacts in the head series automatically became category 3 artefacts by definition. This can explain the difference in assessments between radiologist 1 and 2. Radiologist 1 specifically commented that the artefacts were minor. Apart from this finding, category 3 and 4 artefacts were limited to spine board 1 and vacuum mattress 3. Spine board 1 had metal components and produced significant beam-hardening artefacts, rendering the investigation unsuitable for clinical judgement. We were not able to correct this effect using metal artefact reduction.
Overall a slight increase in radiation dose was observed for almost all of the devices compared to the trauma transfer board. The largest increase in radiation dose output (CTDIvol) was 19% for vacuum mattress 2. The increase in dose output is most likely due to higher photon attenuation since the tested devices are larger and denser than the trauma transfer board, causing the automatic exposure control to increase the dose output. In our opinion, the increased radiation dose due to denser devices is small. The image noise profiles (Fig. 5) shows small variations across the devices. The variation in mean image noise is also small.
Overall, our results confirm those of Euler et al. [10] and indicate that plastic valves resolve the problem of artefacts produced by metallic valves.
We have not been able to identify any publications of neurological deterioration of spinal cord injuries, caused by emergency room handling. Indeed, a recent systematic review found no evidence for harm during the log roll manoeuvre, which may represent one of the situations with the greatest potential for spinal motion [13]. However, leading teaching systems like Advanced Trauma Life Support and Pre Hospital Trauma Life Support demand efforts to restrict spinal movement until a spinal injury has been ruled out [1, 2]. Therefore, such efforts will be made in most trauma systems aiming to provide maximum protection with minimum discomfort to the patient.
To prevent secondary deterioration in a possible spinal injury, it is desirable to maintain immobilisation throughout CT scanning. Furthermore, refraining from removing the immobilisation equipment may reduce the time consumption from arrival in the hospital to CT scans completed. Vacuum mattress 2 and 3 had to be deflated to free the arms (and then re-inflated in the new position) prior to chest/abdomen image acquisition. This adjustment, however, was not necessary with vacuum mattress 1. In addition to producing more artefacts than vacuum mattress 1, vacuum mattress 2 is broad and may not be able to pass into the CT gantry when applied to a large patient.
There are several limitations to our study. First, all scans were performed exclusively using one advanced CT scanner. Thus, we do not know the extent to which immobilisation devices would produce artefacts when older and less advanced machines are used. Second, our phantom represents a small adult patient. Automatic tube current modulation and automatic tube potential selection may make different choices with an average or large patient. The automatic tube potential selection was 100 kV for our phantom abdomen. For large patients, this value would normally be 120 kV or higher. Increasing tube potential is a technique to reduce artefacts from metal objects and will in similar fashion reduce streak artefacts from a dense mattress canvas. CT exposure is also increased for larger patients and may contribute to reduce streak artefacts. We therefore assume that an average or large patient would have less prominent CT artefacts. However, the reverse reasoning may imply more artefacts for smaller children. Third, we assessed only one scan per device. Different folding of the same device may theoretically induce differences in artefacts. Fourth: Although it was not possible to blind the interpreters completely to the generic type of device, they were blinded to manufacture type. Radiologists are not familiar to immobilisation devices in daily practise and we have assumed they therefore do not carry any bias on device type. Finally, our radiologists were not accustomed to evaluating CT scans of a phantom. Although it is realistic, the phantom still is not identical to a living patient, which may have affected the assessments.
Our results are based on a phantom study and may be viewed as an explorative feasibility study. A possible next step would be to conduct a prospective population-based study.
Conclusions
Our results indicate that it is feasible to maintain some vacuum mattresses with plastic valves on trauma patients during CT scanning. The mattresses tested did not result in a considerably increased radiation dose or artefacts that impeded clinical judgement. One of the vacuum mattresses tested produced no artefacts that impeded clinical judgement.
References
PHTLS Committee of NAEMT: Spinal Trauma. In PHTLS - Basic and Advanced Prehospital Trauma Life Support. 7th edition. Edited by McSwain NE. St. Louis, IL, USA: Mosby JEMS, Elsevier; 2011: 245-289.
American College of Surgeons Committee on Trauma: Spine and spinal cord trauma. In Advanced trauma life support for doctors - student course manual. 9th edition. Edited by Rotondo MF. Chicago, IL, USA: American College of Surgeons; 2012: 174-205.
White CC, Domeier RM, Millin MG. EMS spinal precautions and the use of the long backboard - resource document to the position statement of the National Association of EMS physicians and the American College of Surgeons Committee on trauma. Prehosp Emerg Care. 2014;18:306–14.
Sundstrom T, Asbjornsen H, Habiba S, Sunde GA, Wester K. Prehospital use of cervical collars in trauma patients: a critical review. J Neurotrauma. 2014;31:531–40.
Luscombe MD, Williams JL. Comparison of a long spinal board and vacuum mattress for spinal immobilisation. Emerg Med J. 2003;20:476–8.
Hamilton RS, Pons PT. The efficacy and comfort of full-body vacuum splints for cervical-spine immobilization. J Emerg Med. 1996;14:553–9.
Pernik MN, Seidel HH, Blalock RE, Burgess AR, Horodyski M, Rechtine GR, Prasarn ML. Comparison of tissue-interface pressure in healthy subjects lying on two trauma splinting devices: the vacuum mattress splint and long spine board. Injury. 2016;47:1801–5.
Hemmes B, Brink PR, Poeze M. Effects of unconsciousness during spinal immobilization on tissue-interface pressures: a randomized controlled trial comparing a standard rigid spineboard with a newly developed soft-layered long spineboard. Injury. 2014;45:1741–6.
Hemmes B, Jeukens CR, Al-Haidari A, Hofman PA, Vd Linden ES, Brink PR, Poeze M. Effect of spineboard and headblocks on the image quality of head CT scans. Emerg Radiol. 2016;23:263–8.
Euler A, Stieltjes B, Schindera ST. Automatic tube current modulation for whole-body polytrauma CT with immobilization devices: is there an increase in radiation dose and degradation of image quality? Emerg Radiol. 2017;24:31–37.
Morsbach F, Bickelhaupt S, Wanner GA, Krauss A, Schmidt B, Alkadhi H. Reduction of metal artifacts from hip prostheses on CT images of the pelvis: value of iterative reconstructions. Radiology. 2013;268:237–44.
American Association of Physicists in Medicine. The measurement, reporting and management of radiation dose in CT. Report No 96. AAPM Task Group 23 of the Diagnostic Imaging Council CT Committee. College Park: American Association of Physicists in Medicine; 2008.
Hyldmo PK, Vist GE, Feyling AC, Rognas L, Magnusson V, Sandberg M, Soreide E. Does turning trauma patients with an unstable spinal injury from the supine to a lateral position increase the risk of neurological deterioration?--a systematic review. Scand J Trauma Resusc Emerg Med. 2015;23:65.
Acknowledgements
We wish to thank the University of Tromsø for lending us the phantom and radiologist Jon Bache Marthinsen, SSHF, for artefact assessments.
Funding
This project was funded by Sørlandet Hospital.
Availability of data and materials
DICOM images and acquired datasets will be made available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
PKH conceived the study. PJS, EA, MMB, AMM, SA, and PKH designed the study. Data acquisition was performed by PJS, EA, MMB, AMM, SA, and PKH. PJS, EA and MMB analysed and interpreted the data. PJS drafted the manuscript. All authors contributed to revision of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
SA has served as an advisor for AB Germa, Sweden and Kohlbrat & Bunz GmbH, Austria but has gained no economic compensation or any other benefits. All other authors declare no competing interests, economic or otherwise.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Stokkeland, P.J., Andersen, E., Bjørndal, M.M. et al. Maintaining immobilisation devices on trauma patients during CT: a feasibility study. Scand J Trauma Resusc Emerg Med 25, 84 (2017). https://doi.org/10.1186/s13049-017-0428-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13049-017-0428-3