Abstract
The traditional prehospital management of trauma victims with potential spinal injury has become increasingly questioned as authors and clinicians have raised concerns about over-triage and harm. In order to address these concerns, the Norwegian National Competence Service for Traumatology commissioned a faculty to provide a national guideline for pre-hospital spinal stabilisation. This work is based on a systematic review of available literature and a standardised consensus process. The faculty recommends a selective approach to spinal stabilisation as well as the implementation of triaging tools based on clinical findings. A strategy of minimal handling should be observed.
Similar content being viewed by others
Background
Traumatic injury to the spinal cord (SCI) or cauda equina is uncommon but may have devastating consequences [1, 2]. Spinal instability occurs when the integrity of the spinal column is compromised by fractures and/or joint dislocations so that it no longer can maintain it’s protective configuration under normal physiologic loading, predisposing to further injury [3, 4]. Since the 1960s, mishandling of the traumatised spine has been thought to cause neurological deterioration and field spinal stabilisation has been considered pivotal for preventing such secondary injury [5–15]. Through adding external supports to the victim’s body before extrication, treatment and transport to hospital, clinicians aim to reduce spinal movement and prevent further secondary injury [16–19]. The spine is to be stabilised in a neutral position. While this position is poorly defined and subject to controversy and individual variation, it is similar to the position one assumes when standing and looking ahead [20–24]. For decades, the dominant strategy has been to generously assume the presence of unstable spinal injury in all patients with a relevant mechanism of injury or clinical findings and then to stabilise using a combination of a rigid cervical collar, head-blocks, straps and a rigid stretcher system [25–32]. While numerous other devices exist, this combination is widely implemented [33–39].
Many authors have raised concerns over this strategy and have questioned its efficacy, over-triage, costs and potential harmful effects [40–45]. Consequently, several organisations and authors have promoted a more selective strategy [2, 44, 46]. This controversy has generated regional variations in stabilisation strategies within the Emergency Medical Services (EMS) [44]. In order to address these concerns from a national perspective, the Norwegian National Competence Service for Traumatology (NKT-T) in collaboration with The Norwegian Knowledge Centre for the Health Services (NOKC) commissioned a multi-disciplinary faculty to provide a national guideline designed to facilitate the prehospital management of adult trauma victims with potential spinal injury. The GRADE system (grading of recommendations, assessment, development and evaluation) has been combined with standards for clinical practice guidelines and best available evidence to improve pre-hospital management of adult patients with potential spinal injury.
Methods
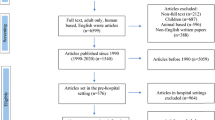
The multi-disciplinary faculty included members from all Norwegian health trusts representing the medical specialties of neurosurgery (1), trauma surgery (1), prehospital care (3), anesthesiology (1) and EMS (1), all with expert knowledge of trauma management. In addition, one methodologist directed the systematic evidence work, including evidence appraisal and synthesis. The standards for developing clinical practice guidelines using The Appraisal of Guidelines for Research and Evaluation (AGREE) tool were followed [47]. Key clinical questions were created in accordance with the PICO format (Population, Intervention, Comparison, Outcome) (Table 1). In December 2014, a research librarian performed a scoping search for existing international guidelines and systematic reviews [48–52].
In March 2015, a systematic literature search for primary studies was performed on core databases Medline, Embase The Cochrane Library and the Cochrane Central Register of Controlled Trials (CENTRAL). Medical Subject Headings (MeSH) search terms are listed in Additional file 1 that is available as a supplementary on-line material. Search was further limited to human studies published in English language.
Two reviewers independently screened titles and abstracts of all records identified in the searches for inclusion. Any discrepancy was resolved through discussion and consensus in the faculty. For completeness, additional records were identified by scanning reference lists and the authors contributing papers known to them. Full text records were critically appraised using the PRISMA checklist for systematic reviews, the CASP checklist for observational studies and the AGREE tool for guidelines [47, 53]. The quality of evidence and strength of recommendations were described using the GRADE tool. In line with the principles of the GRADE methodology, we downgraded the quality of evidence of an intervention for identified risks of bias (methodological quality), inconsistency, indirectness, imprecision or publication bias. Evidence was rated as one of four levels of quality (high, moderate, low and very low). When agreeing on strength of recommendations, three factors were considered and integrated in a group consensus process: benefits and harms, quality of evidence and the preferences of patients and clinicians. The strength of recommendations were graded as strong or conditional. A strong recommendation indicates that the benefits of an intervention far outweigh the harms (or vice versa). A conditional recommendation denotes uncertainty over the balance of benefits and harms. Finally, the faculty opted to use the term ‘good clinical practice’ in instances where a recommendation was considered obviously rational, but where the literature was found too heterogeneous for meta-analysis.
Results
Six guidelines were identified in the scoping stage [2, 19, 46, 54–56]. One publication was of particularly high methodological quality. In 2013, A joint committee from The American Association of Neurological Surgeons (AANS) and the Congress of Neurological Surgeons (CNS) issued updated guidelines for the management of acute cervical spine and spinal cord injuries [46]. These comprehensive guidelines are based on systematic literature searches between 1966 and 2011 and was considered to be both relevant and complete by our faculty. Therefore, we limited our further searches to papers published after 2010 overlapping the AANS/CNS joint committees’ searches by 1 year. In their guideline, Theodore et al. relied on 109 records for their literature review of which one was excluded as it was found as a duplicate amongst our search results. Of the remaining 108, 93 were available in full text format for inclusion into our literature review. The 15 records that were not available were non-peer-reviewed magazine articles, meeting proceedings, local EMS protocols and chapters in textbooks no longer in print or otherwise not available.
Our core database search generated 9.441 abstracts and titles. After independent author review, 9372 were excluded by title or abstract for unrelated topics or for not being primary studies or systematic reviews. A total of 69 original papers were selected for full text reading of which 16 were considered eligible for inclusion into our literature base (Additional file 2). In addition, six systematic reviews were identified and included (Additional file 3) [42, 44, 45, 57–59].
During guideline preparation, another 16 original studies were identified from screening bibliographies and from the authors contributing articles known to them. In total, we identified 63 original studies and 6 systematic reviews that generated and supported 10 recommendations.
Our recommendations, the quality of supporting evidence as well as the strength of recommendation are summarised in Table 2. The original studies supporting each recommendation are listed and described in a separate evidentiary table that is available as supplementary material (Additional file 4). The recommendations formed the framework for an algorithm designed to facilitate the prehospital management of adult trauma victims with potential spinal injury (Fig. 1). A draft version of the guideline was subjected to a national open hearing process involving stakeholders such as the ambulance services of the Norwegian hospital trusts, the air ambulance organisations, regional trauma leaders and the primary health care services. This manuscript presents the finalised version of these recommendations. The rationale and literature behind each recommendation is expanded upon below.
The guideline is now undergoing national operationalisation as it is being implemented in the individual health trusts’ ambulance operating procedures, is taught on e-learning programs and is incorporated into the training of new EMS personnel. The guideline is also widely disseminated through meeting presentations and in national care publications
Recommendation 1: Victims with potential spinal injury should have spinal stabilisation.
Recommendation 2: a minimal handling strategy should be observed.
Rationale and evidence base
Higher level evidence supporting spinal stabilisation is lacking
Despite spinal stabilisation being one of the most frequently performed prehospital interventions, higher grade evidence demonstrating beneficial effects is lacking [46]. From the 1970s to the 1980s the incidence and mortality of complete spinal injury decreased significantly. As this coincided with the introduction of modern spinal management strategies, authors have to varying extents credited stabilisation for this reduction [46, 60–63]. Other than these assumptions, the evidence directly supporting stabilisation consists of reports of low quality associating failure to reduce spinal mobility with neurological deterioration [6, 9, 64–67]. In contrast, in a controversial study comparing patients who had spinal stabilisation in New Mexico, USA with patients in Kuala Lumpur, Malaysia who had no spinal stabilisation, Hauswald et al. demonstrated no protective effect from stabilisation [68]. Nevertheless, taking into account the existing evidence, the anatomical perspective as well as decades of clinical experience, it is likely that the current paradigm of spinal stabilisation has played a part in the reduction of secondary neurological injury. The faculty found no reason to abandon the strategy of external spinal stabilisation. For the same reasons, after having restored the patient to an anatomical position, it is recommended that unnecessary patient handling and movement is minimised. Authors have opined that working in accordance with such a minimal handling strategy may not only reduce spinal movement but may also minimise pain as well as promote hemostasis [69].
Recommendation 3: Spinal stabilisation should never delay or preclude life-saving intervention in the critically injured trauma victim.
Rationale and evidence base
While the faculty recommends adhering to the prehospital stabilisation doctrine, it must also be recognised that SCI is uncommon and that spinal stabilisation is not, in itself, always a benign intervention [43, 46].
Spinal stabilisation may interfere with or delay life-saving intervention
The incidence of SCI in hospitalised trauma victims has been reported in the range of 0.5 to 3% [2]. Spinal stabilisation may preclude or delay the effective management of life-threatening reversible insults such as airway compromise, hypoxemia, tension pneumothorax, cardiac tamponade, haemorrhage or brain trauma which may require urgent prehospital or hospital interventions. Spinal stabilisation has been associated with difficult airway management, restricted thoracopulmonary function and delayed time to intervention [42, 44, 70–74]. In light of this, spinal stabilisation must be de-emphasised in the critically injured patient. While remaining important, spinal stabilisation should never interfere with or delay life-saving intervention nor be allowed to cause or worsen critical injury (Fig. 1).
Recognising time critical injury
Staging and defining time critical injury in trauma is controversial. Identifying patients with critical injury that are unlikely to tolerate prolonged extrication and spinal stabilisation is ultimately up to the attending clinician. Vital parameters may support the decision but should be interpreted cautiously. Nevertheless, we have opted to include a supporting definition of critical injury previously issued by The Norwegian Directorate of Health in a guideline for the management of mass casualty incidents. This definition is designed for individual triage, is based on readily obtainable clinical findings and is nationally recognised by our EMS [75].
Airway compromise, respiratory rate lower than 10 or above 30 breaths per minute, pulse frequency above 120 beats per minute, absent radial pulses or no motor response to verbal commands are signs suggestive of time critical injury. Patients with injuries designated as time critical should not suffer prolonged extrication or evacuation due to spinal concerns. Importantly, this does not imply that spinal precautions are entirely abandoned, but only applied to an extent and in a way that does not delay extrication nor intervention.
The lateral trauma position
Historically, first responders without advanced airway skills have placed unconscious or obtunded victims in the recovery position in order to facilitate the clearance of fluids and to maintain airway patency [45]. Unfortunately, this contradicts the principle of spinal stabilisation in trauma victims as it generates unacceptable spinal movement [76]. The lateral trauma position (LTP) is a variation of the established recovery position that is achieved using a modified two-person log-roll with manual cervical spine control and, eventually, blankets and a rigid collar for cervical stabilisation [77]. While the log-roll involved may generate spinal motion, this may be offset by the beneficial effects of gaining airway patency and clearance. Clinicians not trained in advanced airway management should be encouraged to consider the LTP when transporting obtunded patients.
Recommendation 4: Victims of isolated penetrating injury should not be immobilised.
Rationale and evidence base
Victims of isolated penetrating trauma suffer increased mortality with routine spinal stabilisation [57]. In a 2010 retrospective review of hospitalised victims of penetrating trauma, Haut et al. demonstrated how patients with penetrating injuries who had spinal stabilisation had twice the mortality (14.7%) as those who were not stabilised, likely through delaying transport to surgical intervention. Moreover, the authors found that spinal cord injury in isolated penetrating injury was extremely rare at a rate of 0.01% of victims [74].
Recommendation 5: Triaging tools based on clinical findings should be implemented.
Rationale and evidence base
Triaging tools
In order to address over-triage, authors have advocated implementing triaging tools to assist in identifying low-risk patients who do not require stabilisation [41, 78–81]. The National Emergency X-radiography Utilisation Study (NEXUS) tool and the Canadian C-Spine Rule Criteria (CCR) were originally developed to aid physicians in determining which trauma patients require imaging of the cervical spine [2, 82, 83]. Protocols similar to NEXUS have proven to be useful triaging tools for prehospital spinal stabilisation. Since the early 1990s the Fresno/Kings/Madera EMS system in California have implemented a selective stabilisation protocol similar to NEXUS. In a 2001 retrospective review, Stroh and Braude reported that this protocol had a 99% sensitivity for the correct stabilisation of patients with actual cervical injury [84]. In a prospective observational study of EMS personnel in Maine, also using a tool similar to NEXUS, Burton et al. found that the protocol sensitivity for stabilisation of any spinal fracture was 87% with a negative predictive value of 99.9% [85].
Triaging tools based on clinical findings reduce over-triage
Authors have recommended implementing tools that, similar to NEXUS, are predominantly based on clinical findings [78, 86, 87]. Tools that emphasise the mechanism of injury result in over-triage without increasing accuracy. In a prospective review of 498 trauma patients, Hong et al. found that 95.4% of patients would have been immobilised if EMS personnel had stabilised in accordance with the mechanism based 7th edition PHTLS criteria. In contrast, stabilisation in accordance with protocols based on clinical findings, NEXUS or Hankins protocols, would result in stabilisation rates of 68.7% and 81.5%, respectively. All patients with actual spinal injury would have been stabilised using any of the protocols [88]. In 1999, Muhr et al. reported how the implementation of an out-of-hospital clearance protocol based on clinical findings reduced stabilisation by one third [87]. These and other reports provide evidence of how EMS successfully can implement selective prehospital stabilisation strategies given that they are coupled with training and clinical governance [89–93]. The faculty recommends applying the NEXUS criteria on the entire spine for triage in the prehospital setting. In the absence of midline tenderness, focal neurologic deficit, altered level of consciousness, intoxication, and significant distracting injury, it is safe to withhold stabilisation.
Recommendation 6: Cervical stabilisation may be achieved using manual in-line stabilisation, head-blocks, a rigid collar or combinations thereof.
Rationale and evidence base
The approach to cervical stabilisation should be informed and selective, observing the pros and cons of several techniques. The goal is to achieve stabilisation of the cervical spine. The means will vary.
The efficacy and harms of the rigid cervical collar
No high quality studies have identified the true efficacy of the rigid collar. The existing evidence is difficult to compare due to variations in methodology and types of collars tested [94]. However, numerous studies document how the application of a rigid cervical collar will limit motion in the cervical spine [34, 36, 95–101]. It is also apparent, from these same studies, that movement restriction is limited. Moreover, there is a growing body of evidence documenting harm. As rigid collars achieve cervical stabilisation through compression of the mandible, mouth opening will be reduced. Thus, application may impede breathing and airway management including the clearing of vomit or secretions [43, 102]. Rigid cervical collars can increase intracranial pressure by inducing pain or through blocking cranial venous return [103–105]. In a study on cadavers with an artificially induced unstable C1-C2 lesion, Ben-Galim et al. demonstrated how cervical traction from a collar caused separation between C1 and C2, suggesting a mechanism that could aggravate injury [106]. Severe neurological deterioration has been reported in patients with ankylosing spondylitis after receiving triple stabilisation [107, 108]. Finally, rigid collars may induce pain or discomfort that may trigger non-compliance, agitation and even increased spinal movement in some patients [109–111]. Cervical collar use has also been associated with pressure point ulceration, necrosis and mandibular nerve palsy with prolonged use [112–116].
The rigid collar should not be applied routinely
The aforementioned reports support a selective approach to rigid collar use. While collars are safe to use in the majority of patients, they should be used selectively in patients with traumatic brain injury, airway compromise, ankylosing spondylitis or agitation. In such cases the collar may be withheld or used intermittently. The collar may provide support during certain manoeuvres, such as in stretcher transfers or during evacuation from a vehicle, after which the collar may be opened or removed [99, 117]. With adequate MILS this can be achieved with minimal spinal displacement [118]. Transport may proceed using only MILS and/or head blocks. Holla et al. recently demonstrated how the addition of a rigid collar did not result in improved movement restriction in volunteers already strapped to a rigid stretcher with head blocks [102]. Patients with a kyphotic spine, such as in ankylosing spondylitis, should be stabilised in a position similar to their habitual spinal curvature [108].
Recommendation 7: Transfer from the ground or between stretchers systems should be achieved using a scoop stretcher.
Rationale and evidence base
A significant amount of spinal motion is generated as the patient is transferred from the ground onto or between stretcher systems or beds. Working in accordance with a minimal handling strategy, clinicians must take care to minimise spinal movement during these critical stages of extrication.
The log-roll may generate undue spinal motion and should be avoided in favour of alternative techniques
Log-rolling has traditionally been used to transfer the patient onto or off stretcher systems or to gain access to patients back for examination, despite authors questioning its safety [119]. The log-roll is a potentially dangerous procedure as it may cause fracture dislocation, pain, distress or clot disruption in patients with pelvic fractures or other injuries. The diagnostic value is limited [69, 120, 121]. Moreover, as the head, hips and pelvis are of different diameters, spinal motion is inherent to the technique, and several studies have demonstrated how log-rolling generates more motion than readily available alternative techniques such as lift-and-slide or scoop stretcher techniques [122–128]. The faculty believes that the potential spinal motion generated by the log-roll may be further aggravated in the prehospital setting where it is commonly performed with limited personell and under difficult working conditions. Usage of the technique in the prehospital context should therefore be minimised, if not abolished.
For transfers from the ground or between stretcher systems, we recommend employing a scoop stretcher system. As the scoop stretcher is split vertically and then reassembled underneath the patient, transfer from the ground or between stretchers requires minimal or no rolling [129]. Stabilisation and comfort has been demonstrated to be comparable or better than that of the classic backboard [122, 127, 130].
Recommendation 8: Patients with potential spinal injury should be transported strapped supine on a vacuum mattress or on an ambulance stretcher system.
Recommendation 9: Hard surface stretcher systems may be used for transports of shorter duration only.
Rationale and evidence base
We wish to differentiate between hard and soft surface stretcher systems. Hard surface systems are those where the patient is directly lying on hard plastic or metal while soft surface systems have padding designed to increase comfort and decrease point pressure.
Hard surface stretcher systems
The backboard was designed to facilitate extrication but has since its inception been used as a transportation device and quickly became the gold standard for spinal stabilisation during transport [131, 132]. The literature, on the contrary, suggests that it is not appropriate for transports of longer duration. Within short time, patients will develop significant discomfort and moderate to severe pain [133–135]. Prolonged exposure may result in pressure ulcers [136, 137]. Pain and discomfort may also result in undue voluntary spinal movement [133]. The scoop stretcher, like the backboard, has hard surfaces that could induce pain, discomfort or pressure point injury. While it is an excellent extrication device and an appropriate transportation device for short distances, for longer duration transport the scoop stretcher, like the backboard, should be removed after transferring the victim onto a vacuum splint mattress or onto a standard ambulance trolley.
Soft surface stretcher systems
The vacuum mattress, while not rigid enough for extrication, is a useful transportation device. As vacuum is applied, the mattress moulds to the patient’s contours, minimising point pressure, making it more comfortable, less painful and, arguably, less likely to produce ulceration [73, 138–141]. The vacuum mattress has been shown to provide a similar, or superior, degree of stabilisation when compared to that of the backboard [132, 139, 140, 142].
Recommendation 10: Patients should under some circumstances be invited to self-extricate from vehicles.
Rationale and evidence base
The traditional approach to extrication of victims with potential spine injury from vehicles or other settings has been to stabilise the victim with a cervical collar and then to carefully transfer the passive victim onto a backboard for extrication [143].
Self-extrication
Over the years, authors have argued that this practice often is unnecessary, resulting in prolonged extrication times and avoidable complications related to spinal stabilisation. Authors have argued that spinal movement within the normal range of motion requires so little energy, of many magnitudes less than the energy at the initial impact, that it is highly unlikely to cause further injury. Furthermore, the alert victim’s own muscular tone will suffice to protect the spine from further injury [41, 68, 144]. In 2013, the British Faculty of Pre-Hospital care acknowledged this in a statement recommending that the fully alert patient a potential spinal injury who is without distracting injury, should be allowed to self-extricate without external stabilisation [2]. Unfortunately, such a position is supported by very few studies. Shafer and Naunheim, in 2009, demonstrated how volunteers stabilised only with a rigid collar who exited a vehicle on their own volition, generated less spinal motion than when extricated using traditional assisted longboard techniques [145]. More recently, Dixon et al., in a biomechanical study on healthy volunteers found that controlled self-extrication without collar generated less movement in the cervical spine when compared to equipment aided extrication techniques [146].
A generous approach to self-extrication
Despite the scant evidence, we recommend self-extrication in some circumstances. As long as patients with back or neck pain are not obtunded, not under the influence of any drug, and without significant distracting injury, they should be invited to self-extricate to a nearby stretcher system. The prerequisite for self-extrication is that it is done under safe conditions. Should there be concerns about safety, then strategy defaults back to traditional extrication techniques. The patients should, after lying down on a stretcher system, have full external stabilisation for final evacuation and transport as they may then be subject to external force that may overwhelm their muscular protection.
Summary
This guideline, based on consensus and the best available evidence, is an attempt to address concerns about over-triage, harms and costs associated with the traditional management of potential spinal injury. The faculty found no reason to abandon the current doctrine of spinal immobilisation in patients with potential spinal injury. We do, however, recommend implementing pre-hospital triaging tools as well as maintaining a selective approach to the use of the various stabilisation devices.
Abbreviations
- EMS:
-
Emergency medical services
- MILS:
-
(Manual In-Line Stabilisation)
- PHTLS:
-
Pre-Hospital Trauma Life Support
- SCI:
-
Spinal Cord Injury
References
Prasad VS, Schwartz A, Bhutani R, Sharkey PW, Schwartz ML. Characteristics of injuries to the cervical spine and spinal cord in polytrauma patient population: experience from a regional trauma unit. Spinal Cord. 1999;37:560–8.
Connor D, Greaves I, Porter K, Bloch M, consensus group FoP-HC. Pre-hospital spinal immobilisation: an initial consensus statement. Emerg Med J. 2013;30:1067–9.
Brunette DD, Rockswold GL. Neurologic recovery following rapid spinal realignment for complete cervical spinal cord injury. J Trauma. 1987;27:445–7.
Burney RE, Waggoner R, Maynard FM. Stabilization of spinal injury for early transfer. J Trauma. 1989;29:1497–9.
Kossuth LC. The removal of injured personnel from wrecked vehicles. J Trauma. 1965;5:703–8.
Geisler WO, Wynne-Jones M, Jousse AT. Early management of the patient with trauma to the spinal cord. Med Serv J Can. 1966;22:512–23.
Kossuth LC. The initial movement of the injured. Mil Med. 1967;132:18–21.
Farrington JD. Extrication of victims--surgical principles. J Trauma. 1968;8:493–512.
Bohlman HH. Acute fractures and dislocations of the cervical spine. An analysis of three hundred hospitalized patients and review of the literature. J Bone Joint Surg Am. 1979;61:1119–42.
Rimel RW, Jane JA, Edlich RF. An educational training program for the care at the site of injury of trauma to the central nervous system. Resuscitation. 1981;9:23–8.
Wagner Jr FC, Johnson RM. Cervical bracing after trauma. Med Instrum. 1982;16:287–8.
Cline JR, Scheidel E, Bigsby EF. A comparison of methods of cervical immobilization used in patient extrication and transport. J Trauma. 1985;25:649–53.
Moylan JA. Trauma injuries. Triage and stabilization for safe transfer. Postgrad Med. 1985;78:166–71. 174–165, 177.
Jeanneret B, Magerl F, Ward JC. Overdistraction: a hazard of skull traction in the management of acute injuries of the cervical spine. Arch Orthop Trauma Surg. 1991;110:242–5.
Farrington JD. Death in a Ditch. 1967. Bull Am Coll Surg. 2013;98:44–53. discussion 43.
Stauffer ES. Orthotics for spinal cord injuries. Clin Orthop Relat Res. 1974;102:92–9.
Fenstermaker RA. Acute neurologic management of the patient with spinal cord injury. Urol Clin North Am. 1993;20:413–21.
Frohna WJ. Emergency department evaluation and treatment of the neck and cervical spine injuries. Emerg Med Clin North Am. 1999;17:739–91. v.
White CC, Domeier RM, Millin MG, Standards, Clinical Practice Committee NAoEMSP. EMS spinal precautions and the use of the long backboard - resource document to the position statement of the National Association of EMS Physicians and the American College of Surgeons Committee on Trauma. Prehosp Emerg Care. 2014;18:306–14.
Schriger DL, Larmon B, LeGassick T, Blinman T. Spinal immobilization on a flat backboard: does it result in neutral position of the cervical spine? Ann Emerg Med. 1991;20:878–81.
Nypaver M, Treloar D. Neutral cervical spine positioning in children. Ann Emerg Med. 1994;23:208–11.
Curran C, Dietrich AM, Bowman MJ, Ginn-Pease ME, King DR, Kosnik E. Pediatric cervical-spine immobilization: achieving neutral position? J Trauma. 1995;39:729–32.
Schriger DL. Immobilizing the cervical spine in trauma: should we seek an optimal position or an adequate one? Ann Emerg Med. 1996;28:351–3.
Del Rossi G, Rechtine GR, Conrad BP, Horodyski M. Is sub-occipital padding necessary to maintain optimal alignment of the unstable spine in the prehospital setting? A preliminary report. J Emerg Med. 2013;45:366–71.
Worsing Jr RA. Principles of prehospital care of musculoskeletal injuries. Emerg Med Clin North Am. 1984;2:205–17.
Swain A, Dove J, Baker H. ABC of major trauma. Trauma of the spine and spinal cord--I. BMJ. 1990;301:34–8.
McGuire Jr RA. Protection of the unstable spine during transport and early hospitalization. J Miss State Med Assoc. 1991;32:305–8.
Alexander RH, Proctor HJ, American College of Surgeons, Committee on Trauma. Advanced trauma life support program for physicians : ATLS. 5th edn. Chicago, IL: American College of Surgeons; 1993.
Mazolewski P, Manix TH. The effectiveness of strapping techniques in spinal immobilization. Ann Emerg Med. 1994;23:1290–5.
De Lorenzo RA. A review of spinal immobilization techniques. J Emerg Med. 1996;14:603–13.
Perry SD, McLellan B, McIlroy WE, Maki BE, Schwartz M, Fernie GR. The efficacy of head immobilization techniques during simulated vehicle motion. Spine (Phila Pa 1976). 1999;24:1839–44.
Cervical spine immobilization before admission to the hospital. Neurosurgery 2002, 50:S7-17.
Jones SL. Spinal trauma board. Phys Ther. 1977;57:921–2.
Graziano AF, Scheidel EA, Cline JR, Baer LJ. A radiographic comparison of prehospital cervical immobilization methods. Ann Emerg Med. 1987;16:1127–31.
Cohen J. A new device for the care of acute spinal injuries: the Russel extrication device. Aeromedical J. 1988;3:41.
Chandler DR, Nemejc C, Adkins RH, Waters RL. Emergency cervical-spine immobilization. Ann Emerg Med. 1992;21:1185–8.
Carter VM, Fasen JA, Roman Jr JM, Hayes KW, Petersen CM. The effect of a soft collar, used as normally recommended or reversed, on three planes of cervical range of motion. J Orthop Sports Phys Ther. 1996;23:209–15.
Tuite GF, Veres R, Crockard HA, Peterson D, Hayward RD. Use of an adjustable, transportable, radiolucent spinal immobilization device in the comprehensive management of cervical spine instability: Technical note. J Neurosurg. 1996;85:1177–80.
Markenson D, Foltin G, Tunik M, Cooper A, Giordano L, Fitton A, Lanotte T. The Kendrick extrication device used for pediatric spinal immobilization. Prehosp Emerg Care. 1999;3:66–9.
McHugh TP, Taylor JP. Unnecessary out-of-hospital use of full spinal immobilization. Acad Emerg Med. 1998;5:278–80.
Orledge JD, Pepe PE. Out-of-hospital spinal immobilization: is it really necessary? Acad Emerg Med. 1998;5:203–4.
Kwan I, Bunn F. Effects of prehospital spinal immobilization: a systematic review of randomized trials on healthy subjects. Prehosp Disaster Med. 2005;20:47–53.
Abram S, Bulstrode C. Routine spinal immobilization in trauma patients: what are the advantages and disadvantages? Surgeon. 2010;8:218–22.
Sundstrom T, Asbjornsen H, Habiba S, Sunde GA, Wester K. Prehospital use of cervical collars in trauma patients: a critical review. J Neurotrauma. 2014;31:531–40.
Hyldmo PK, Vist GE, Feyling AC, Rognas L, Magnusson V, Sandberg M, Soreide E. Is the supine position associated with loss of airway patency in unconscious trauma patients? A systematic review and meta-analysis. Scand J Trauma Resusc Emerg Med. 2015;23:50.
Theodore N, Hadley MN, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, Rozzelle CJ, Ryken TC, Walters BC. Prehospital cervical spinal immobilization after trauma. Neurosurgery. 2013;72 Suppl 2:22–34.
AGREE [http://www.agreetrust.org]
U.S. Department of Health and Human Services, National Guideline Clearinghouse [http://www.guideline.gov]
BMJ Best Practice [http://bestpractice.bmj.com]
UpToDate [http://www.uptodate.com]
National Institute for Health and Care Excellence [http://www.nice.org.uk]
Guidelines International Network [http://www.g-i-n.net]
Critical Appraisal Skills Programme (CASP) [http://www.casp-uk.net]
Ahn H, Singh J, Nathens A, MacDonald RD, Travers A, Tallon J, Fehlings MG, Yee A. Pre-hospital care management of a potential spinal cord injured patient: a systematic review of the literature and evidence-based guidelines. J Neurotrauma. 2011;28:1341–61.
Oteir AO, Smith K, Jennings PA, Stoelwinder JU. The prehospital management of suspected spinal cord injury: an update. Prehosp Disaster Med. 2014;29:399–402.
Prehospital care of the adult trauma patient [http://www.uptodate.com/contents/prehospital-care-of-the-adult-trauma-patient?source=search_result&search=prehospital+trauma&selectedTitle=1%7E106]
Stuke LE, Pons PT, Guy JS, Chapleau WP, Butler FK, McSwain NE. Prehospital spine immobilization for penetrating trauma--review and recommendations from the Prehospital Trauma Life Support Executive Committee. J Trauma. 2011;71:763–9. discussion 769–770.
Hyldmo PK, Vist GE, Feyling AC, Rognas L, Magnusson V, Sandberg M, Soreide E. Does turning trauma patients with an unstable spinal injury from the supine to a lateral position increase the risk of neurological deterioration?--A systematic review. Scand J Trauma Resusc Emerg Med. 2015;23:65.
Oteir AO, Smith K, Stoelwinder JU, Middleton J, Jennings PA. Should suspected cervical spinal cord injury be immobilised?: a systematic review. Injury. 2015;46:528–35.
Green BA, Eismont FJ. Acute spinal cord injury: a systems approach. Cent Nerv Syst Trauma. 1984;1:173–95.
Olson CM, Jastremski MS, Vilogi JP, Madden CM, Beney KM. Stabilization of patients prior to interhospital transfer. Am J Emerg Med. 1987;5:33–9.
Garfin SR, Shackford SR, Marshall LF, Drummond JC: Care of the multiply injured patient with cervical spine injury. Clin Orthop Relat Res 1989;(239):19–29.
Waters RL, Meyer Jr PR, Adkins RH, Felton D. Emergency, acute, and surgical management of spine trauma. Arch Phys Med Rehabil. 1999;80:1383–90.
Gunby I. New focus on spinal cord injury. JAMA. 1981;245:1201–6.
Marshall LF, Knowlton S, Garfin SR, Klauber MR, Eisenberg HM, Kopaniky D, Miner ME, Tabbador K, Clifton GL. Deterioration following spinal cord injury. A multicenter study. J Neurosurg. 1987;66:400–4.
Toscano J. Prevention of neurological deterioration before admission to a spinal cord injury unit. Paraplegia. 1988;26:143–50.
Todd NV, Skinner D, Wilson-MacDonald J. Secondary neurological deterioration in traumatic spinal injury: data from medicolegal cases. Bone Joint J. 2015;97-B:527–31.
Hauswald M, Ong G, Tandberg D, Omar Z. Out-of-hospital spinal immobilization: its effect on neurologic injury. Acad Emerg Med. 1998;5:214–9.
Moss R, Greaves I. consensus g: Minimal patient handling: a faculty of prehospital care consensus statement. Emerg Med J. 2013;30:1065–6.
Bauer D, Kowalski R. Effect of spinal immobilization devices on pulmonary function in the healthy, nonsmoking man. Ann Emerg Med. 1988;17:915–8.
Walsh M, Grant T, Mickey S. Lung function compromised by spinal immobilization. Ann Emerg Med. 1990;19:615–6.
Schafermeyer RW, Ribbeck BM, Gaskins J, Thomason S, Harlan M, Attkisson A. Respiratory effects of spinal immobilization in children. Ann Emerg Med. 1991;20:1017–9.
Totten VY, Sugarman DB. Respiratory effects of spinal immobilization. Prehosp Emerg Care. 1999;3:347–52.
Haut ER, Kalish BT, Efron DT, Haider AH, Stevens KA, Kieninger AN, Cornwell 3rd EE, Chang DC. Spine immobilization in penetrating trauma: more harm than good? J Trauma. 2010;68:115–20. discussion 120–111.
Masseskadetriage [https://helsedirektoratet.no/retningslinjer/nasjonal-veileder-for-masseskadetriage]
Gunn BD, Eizenberg N, Silberstein M, McMeeken JM, Tully EA, Stillman BC, Brown DJ, Gutteridge GA. How should an unconscious person with a suspected neck injury be positioned? Prehosp Disaster Med. 1995;10:239–44.
Fattah S, Ekas GR, Hyldmo PK, Wisborg T. The lateral trauma position: what do we know about it and how do we use it? A cross-sectional survey of all Norwegian emergency medical services. Scand J Trauma Resusc Emerg Med. 2011;19:45.
Domeier RM, Evans RW, Swor RA, Rivera-Rivera EJ, Frederiksen SM. Prehospital clinical findings associated with spinal injury. Prehosp Emerg Care. 1997;1:11–5.
Lin HL, Lee WC, Chen CW, Lin TY, Cheng YC, Yeh YS, Lin YK, Kuo LC. Neck collar used in treatment of victims of urban motorcycle accidents: over- or underprotection? Am J Emerg Med. 2011;29:1028–33.
Boland LL, Satterlee PA, Jansen PR. Cervical spine fractures in elderly patients with hip fracture after low-level fall: an opportunity to refine prehospital spinal immobilization guidelines? Prehosp Disaster Med. 2014;29:96–9.
Morrison J, Jeanmonod R. Imaging in the NEXUS-negative patient: when we break the rule. Am J Emerg Med. 2014;32:67–70.
Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma, National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343:94–9.
Michaleff ZA, Maher CG, Verhagen AP, Rebbeck T, Lin CW. Accuracy of the Canadian C-spine rule and NEXUS to screen for clinically important cervical spine injury in patients following blunt trauma: a systematic review. CMAJ. 2012;184:E867–876.
Stroh G, Braude D. Can an out-of-hospital cervical spine clearance protocol identify all patients with injuries? An argument for selective immobilization. Ann Emerg Med. 2001;37:609–15.
Burton JH, Dunn MG, Harmon NR, Hermanson TA, Bradshaw JR. A statewide, prehospital emergency medical service selective patient spine immobilization protocol. J Trauma. 2006;61:161–7.
Domeier RM, Evans RW, Swor RA, Hancock JB, Fales W, Krohmer J, Frederiksen SM, Shork MA. The reliability of prehospital clinical evaluation for potential spinal injury is not affected by the mechanism of injury. Prehosp Emerg Care. 1999;3:332–7.
Muhr MD, Seabrook DL, Wittwer LK. Paramedic use of a spinal injury clearance algorithm reduces spinal immobilization in the out-of-hospital setting. Prehosp Emerg Care. 1999;3:1–6.
Hong R, Meenan M, Prince E, Murphy R, Tambussi C, Rohrbach R, Baumann BM. Comparison of three prehospital cervical spine protocols for missed injuries. West J Emerg Med. 2014;15:471–9.
Domeier RM, Evans RW, Swor RA, Rivera-Rivera EJ, Frederiksen SM. Prospective validation of out-of-hospital spinal clearance criteria: a preliminary report. Acad Emerg Med. 1997;4:643–6.
Brown LH, Gough JE, Simonds WB. Can EMS providers adequately assess trauma patients for cervical spinal injury? Prehosp Emerg Care. 1998;2:33–6.
Meldon SW, Brant TA, Cydulka RK, Collins TE, Shade BR. Out-of-hospital cervical spine clearance: agreement between emergency medical technicians and emergency physicians. J Trauma. 1998;45:1058–61.
Domeier RM, Swor RA, Evans RW, Hancock JB, Fales W, Krohmer J, Frederiksen SM, Rivera-Rivera EJ, Schork MA. Multicenter prospective validation of prehospital clinical spinal clearance criteria. J Trauma. 2002;53:744–50.
Tello RR, Braude D, Fullerton L, Froman P. Outcome of trauma patients immobilized by emergency department staff, but not by emergency medical services providers: a quality assurance initiative. Prehosp Emerg Care. 2014;18:544–9.
Roozmon P, Gracovetsky SA, Gouw GJ, Newman N. Examining motion in the cervical spine. I: Imaging systems and measurement techniques. J Biomed Eng. 1993;15:5–12.
Podolsky S, Baraff LJ, Simon RR, Hoffman JR, Larmon B, Ablon W. Efficacy of cervical spine immobilization methods. J Trauma. 1983;23:461–5.
McCabe JB, Nolan DJ. Comparison of the effectiveness of different cervical immobilization collars. Ann Emerg Med. 1986;15:50–3.
McGuire RA, Degnan G, Amundson GM. Evaluation of current extrication orthoses in immobilization of the unstable cervical spine. Spine (Phila Pa 1976). 1990;15:1064–7.
Rosen PB, McSwain Jr NE, Arata M, Stahl S, Mercer D. Comparison of two new immobilization collars. Ann Emerg Med. 1992;21:1189–95.
Del Rossi G, Heffernan TP, Horodyski M, Rechtine GR. The effectiveness of extrication collars tested during the execution of spine-board transfer techniques. Spine J. 2004;4:619–23.
Horodyski M, DiPaola CP, Conrad BP, Rechtine 2nd GR. Cervical collars are insufficient for immobilizing an unstable cervical spine injury. J Emerg Med. 2011;41:513–9.
Ivancic PC. Do cervical collars and cervicothoracic orthoses effectively stabilize the injured cervical spine? A biomechanical investigation. Spine (Phila Pa 1976). 2013;38:E767–774.
Holla M. Value of a rigid collar in addition to head blocks: a proof of principle study. Emerg Med J. 2012;29:104–7.
Raphael JH, Chotai R. Effects of the cervical collar on cerebrospinal fluid pressure. Anaesthesia. 1994;49:437–9.
Davies G, Deakin C, Wilson A. The effect of a rigid collar on intracranial pressure. Injury. 1996;27:647–9.
Kolb JC, Summers RL, Galli RL. Cervical collar-induced changes in intracranial pressure. Am J Emerg Med. 1999;17:135–7.
Ben-Galim P, Dreiangel N, Mattox KL, Reitman CA, Kalantar SB, Hipp JA. Extrication collars can result in abnormal separation between vertebrae in the presence of a dissociative injury. J Trauma. 2010;69:447–50.
Podolsky SM, Hoffman JR, Pietrafesa CA. Neurologic complications following immobilization of cervical spine fracture in a patient with ankylosing spondylitis. Ann Emerg Med. 1983;12:578–80.
Thumbikat P, Hariharan RP, Ravichandran G, McClelland MR, Mathew KM. Spinal cord injury in patients with ankylosing spondylitis: a 10-year review. Spine (Phila Pa 1976). 2007;32:2989–95.
Plaisier B, Gabram SG, Schwartz RJ, Jacobs LM. Prospective evaluation of craniofacial pressure in four different cervical orthoses. J Trauma. 1994;37:714–20.
Lerner EB, Billittier AJ, Moscati RM. The effects of neutral positioning with and without padding on spinal immobilization of healthy subjects. Prehosp Emerg Care. 1998;2:112–6.
Bruijns SR, Guly HR, Wallis LA. Effect of spinal immobilization on heart rate, blood pressure and respiratory rate. Prehosp Disaster Med. 2013;28:210–4.
Hewitt S. Skin necrosis caused by a semi-rigid cervical collar in a ventilated patient with multiple injuries. Injury. 1994;25:323–4.
Liew SC, Hill DA. Complication of hard cervical collars in multi-trauma patients. Aust N Z J Surg. 1994;64:139–40.
Rodgers JA, Rodgers WB. Marginal mandibular nerve palsy due to compression by a cervical hard collar. J Orthop Trauma. 1995;9:177–9.
Blaylock B. Solving the problem of pressure ulcers resulting from cervical collars. Ostomy Wound Manage. 1996;42:26–8. 30, 32–23.
Black CA, Buderer NM, Blaylock B, Hogan BJ. Comparative study of risk factors for skin breakdown with cervical orthotic devices: Philadelphia and Aspen. J Trauma Nurs. 1998;5:62–6.
Conrad BP, Rechtine G, Weight M, Clarke J, Horodyski M. Motion in the unstable cervical spine during hospital bed transfers. J Trauma. 2010;69:432–6.
Prasarn ML, Conrad B, Del Rossi G, Horodyski M, Rechtine GR. Motion generated in the unstable cervical spine during the application and removal of cervical immobilization collars. J Trauma Acute Care Surg. 2012;72:1609–13.
Conrad BP, Rossi GD, Horodyski MB, Prasarn ML, Alemi Y, Rechtine GR. Eliminating log rolling as a spine trauma order. Surg Neurol Int. 2012;3:S188–197.
Lee C, Porter K. The prehospital management of pelvic fractures. Emerg Med J. 2007;24:130–3.
Leech C, Porter K, Bosanko C. Log-rolling a blunt major trauma patient is inappropriate in the primary survey. Emerg Med J. 2014;31:86.
McGuire RA, Neville S, Green BA, Watts C. Spinal instability and the log-rolling maneuver. J Trauma. 1987;27:525–31.
Suter RE, Tighe TV, Sartori J, Reed K. Thoraco-Lumbar Spinal Instability during Variations of the Log-Roll Maneuver. Prehosp Disaster Med. 1992;7:133–8.
Conrad BP, Horodyski M, Wright J, Ruetz P, Rechtine 2nd GR. Log-rolling technique producing unacceptable motion during body position changes in patients with traumatic spinal cord injury. J Neurosurg Spine. 2007;6:540–3.
Del Rossi G, Horodyski MH, Conrad BP, Di Paola CP, Di Paola MJ, Rechtine GR. The 6-plus-person lift transfer technique compared with other methods of spine boarding. J Athl Train. 2008;43:6–13.
Del Rossi G, Horodyski M, Conrad BP, Dipaola CP, Dipaola MJ, Rechtine GR. Transferring patients with thoracolumbar spinal instability: are there alternatives to the log roll maneuver? Spine (Phila Pa 1976). 2008;33:1611–5.
Del Rossi G, Rechtine GR, Conrad BP, Horodyski M. Are scoop stretchers suitable for use on spine-injured patients? Am J Emerg Med. 2010;28:751–6.
Horodyski M, Conrad BP, Del Rossi G, DiPaola CP, Rechtine 2nd GR. Removing a patient from the spine board: is the lift and slide safer than the log roll? J Trauma. 2011;70:1282–5. discussion 1285.
Hachen HJ. Emergency transportation in the event of acute spinal cord lesion. Paraplegia. 1974;12:33–7.
Krell JM, McCoy MS, Sparto PJ, Fisher GL, Stoy WA, Hostler DP. Comparison of the Ferno Scoop Stretcher with the long backboard for spinal immobilization. Prehosp Emerg Care. 2006;10:46–51.
Cooke M. Spinal boards. J Accid Emerg Med. 1996;13:433.
Luscombe MD, Williams JL. Comparison of a long spinal board and vacuum mattress for spinal immobilisation. Emerg Med J. 2003;20:476–8.
Chan D, Goldberg R, Tascone A, Harmon S, Chan L. The effect of spinal immobilization on healthy volunteers. Ann Emerg Med. 1994;23:48–51.
Cordell WH, Hollingsworth JC, Olinger ML, Stroman SJ, Nelson DR. Pain and tissue-interface pressures during spine-board immobilization. Ann Emerg Med. 1995;26:31–6.
Walton R, DeSalvo JF, Ernst AA, Shahane A. Padded vs unpadded spine board for cervical spine immobilization. Acad Emerg Med. 1995;2:725–8.
Linares HA, Mawson AR, Suarez E, Biundo JJ. Association between pressure sores and immobilization in the immediate post-injury period. Orthopedics. 1987;10:571–3.
Mawson AR, Biundo Jr JJ, Neville P, Linares HA, Winchester Y, Lopez A. Risk factors for early occurring pressure ulcers following spinal cord injury. Am J Phys Med Rehabil. 1988;67:123–7.
Chan D, Goldberg RM, Mason J, Chan L. Backboard versus mattress splint immobilization: a comparison of symptoms generated. J Emerg Med. 1996;14:293–8.
Hamilton RS, Pons PT. The efficacy and comfort of full-body vacuum splints for cervical-spine immobilization. J Emerg Med. 1996;14:553–9.
Johnson DR, Hauswald M, Stockhoff C. Comparison of a vacuum splint device to a rigid backboard for spinal immobilization. Am J Emerg Med. 1996;14:369–72.
Mok JM, Jackson KL, Fang R, Freedman BA. Effect of vacuum spine board immobilization on incidence of pressure ulcers during evacuation of military casualties from theater. Spine J. 2013;13:1801–8.
Mahshidfar B, Mofidi M, Yari AR, Mehrsorosh S. Long backboard versus vacuum mattress splint to immobilize whole spine in trauma victims in the field: a randomized clinical trial. Prehosp Disaster Med. 2013;28:462–5.
Dick T. Comparing the short-board technique. Ann Emerg Med. 1989;18:115–6.
Stevens AC, Trammell TR, Billows GL, Ladd LM, Olinger ML. Radiation exposure as a consequence of spinal immobilization and extrication. J Emerg Med. 2015;48:172–7.
Shafer JS, Naunheim RS. Cervical spine motion during extrication: a pilot study. West J Emerg Med. 2009;10:74–8.
Dixon M, O’Halloran J, Hannigan A, Keenan S, Cummins NM. Confirmation of suboptimal protocols in spinal immobilisation? Emerg Med J. 2015;32:939–45.
Acknowledgements
We are indebted to Anita Saur Haukvik, senior librarian at Sørlandet Hospital, for performing the literature search, and Hilde Strømme, senior librarian at The Norwegian Knowledge Centre for the Heath Services for peer-reviewing the literature search and their strategies.
Funding
Designing this guideline required travelling to six meetings. The Norwegian National Competence Service for Traumatology has covered travel expenses for these meetings.
Availability of data and materials
We have submitted our detailed search vocabulary and literature tables as supplementary material. There is no other data nor material.
Competing interest
PKH has been involved in the development of the Lateral Trauma Position. Other than that the faculty/authors have no competing interests to declare. PKH devised the Lateral Trauma Position method, but has gained no economic benefits thereof.
Authors’ contributions
DKK, TB, JJJ and EJ are the main authors of this manuscript. All authors (DKK, JJJ, EJ, TB, TH, TD, HA) have participated in the research and consensus process. All authors have contributed to the drafting of this manuscript and have approved this final version.
Consent for publication
This manuscript contains no individual person’s data in any form.
Ethics approval and consent to participate
Not applicable as this manuscript is a literature review and a clinical guideline.
Meetings
This guideline has been presented by PKH at the London Trauma Conference 2016.
Grant
The authors have received no financial support.
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1:
Search engine vocabulary. (DOCX 108 kb)
Additional file 2: Table S1.
Original studies identified in our search for new literature. (DOCX 24 kb)
Additional file 3: Table S2.
The systematic reviews that were identified in our search for new literature. (DOCX 23 kb)
Additional file 4: Table S3.
Original studies supporting our 10 recommendations. (DOCX 44 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kornhall, D.K., Jørgensen, J.J., Brommeland, T. et al. The Norwegian guidelines for the prehospital management of adult trauma patients with potential spinal injury. Scand J Trauma Resusc Emerg Med 25, 2 (2017). https://doi.org/10.1186/s13049-016-0345-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13049-016-0345-x