Abstract
Background
Although pain management is a fundamental aspect of care in emergency departments (EDs), inadequate treatment of pain is unfortunately common. There are multiple local protocols for pain assessment in the ED. This study evaluated whether the initial assessment and treatment of pain in the ED are in accordance with the in-hospital protocol of the ED at a Norwegian University Hospital.
Materials and methods
Prospective data on pain assessment and initial treatment in the ED were collected from nursing and physician documentation. The patients’ perceptions of subjective pain were recorded using a numerical rating scale (NRS) that ranged from 0 to 10.
Results
Seventy-seven percent of the 764 enrolled patients were evaluated for pain at arrival. Female patients had a higher probability of not being asked about pain, but there was no difference in the percentage of patients asked about pain with respect to age. Additionally, patients with low oxygen saturation and systolic blood pressure were less likely to be asked about pain. Of those with moderate and severe pain (58 %), only 14 % received pain relief.
Discussion
Assessment and treatment of pain in the ED are inadequate and not in line with the local protocols. A focus on strategies to improve pain treatment in the ED is a necessary aspect of developing optimal acute patient care in Norway in the future.
Similar content being viewed by others
Introduction
Pain is often referred to as the fifth vital sign [1] and is one of the most common problems in patients who arrive at emergency departments (EDs) [2]. Patients usually expect that their pain will be addressed and treated [3]; however, despite patients’ expectations, there is suboptimal pain management in the ED. Pain is used as a quality indicator [3–5], and there are multiple guidelines for pain management [6, 7]. Acute pain may have adverse physiological and psychological effects [8, 9], but there is still inadequate treatment of pain in EDs [10, 11]. Of the patients who arrive at the ED with a painful condition, more than 50 % indicate that the pain is moderate to severe [12, 13]. Despite strategies to ensure safe and effective pain treatment in the ED, nurses rarely give analgesics before a physician sees the patient [14]. Previous studies have shown that even when nurses have local pain protocols, an unacceptable proportion of patients receive an inadequate assessment and pain treatment [15]. Health care workers in the ED often have limited knowledge of pain [16], and pain assessment is poorly documented in patient records [17]. Published guidelines for pain treatment recommend initial pain assessment of all ED patients [18], and if the patient indicates moderate to severe pain, treatment should be initiated [19]. Local ED protocol at St. Olav’s hospital was implemented in 2012 to ensure adequate pain assessment and treatment of all patients who arrive at the ED, but the performance in relation to the guidelines has not been evaluated. All patients should be asked to rate their subjective pain with a numerical rating scale (NRS) [20, 21], and patients with moderate to severe pain should be offered pain medications or appropriate intervention. Multiple studies have looked at assessment and management in the ED [22]. This prospective study evaluated whether the assessment and management of pain in a Norwegian ED was in line with the local protocols. A similar study has not previously been conducted in Norway.
Materials and methods
In November 2012, a 20-day prospective study was conducted at St. Olav’s Hospital in Trondheim, Norway, where ED patient data were collected daily during the period of highest patient influx (noon-10 p.m.) [23]. Relevant quality indicators and data were chosen and included in the study design prior to collecting the data (including chief complaints, acuity level, vital signs, and pain score). Data was obtained from the regular nursing triage forms during or immediately after the initial assessment of the ED patients. All data were collected before the patient left the ED. Research assistants were constantly observing the patient care and activity in the ED while obtaining data immediately when available during the study period. The research assistants did not interfere with patient care or the nurses’ work, and there were no patient involvements. The physicians and nurses were aware of the ongoing study, but were not informed about what data that was obtained. St. Olav’s Hospital is a university hospital that serves approximately 280,000 local residents as a community hospital. In addition, the hospital has a regional function as a tertiary center for approximately 680,000 inhabitants. The ED primarily receives patients over 16 years of age and has an annual patient population of approximately 21,000 [23]. Data on all patients who arrived at the ED in the specified time period were manually recorded. Prospective data on the pain assessment and initial treatment in the ED were collected from nursing and physician documentation. The triage system, RETTS, is used to determine the acuity level (triage) in the ED (http://www.predicare.se) [24].
Evaluation of pain
Patient perception of subjective pain should be evaluated at arrival according to local procedures at St. Olav’s Hospital. The pain is evaluated using a numeric rating scale (NRS), which measures the degree of pain on an 11-point scale from 0 to 10 [20, 21], where 0 indicates no pain and 10 indicates the worst imaginable pain. A score of 1–3 is defined as mild pain, 4–6 moderate pain, and 7–10 severe pain. The local protocol at St. Olav’s Hospital intends to ensure adequate pain assessment and treatment of all patients in the ED. The protocol is used for all adult patients who are awake (Glasgow Coma Scale ≥14) and do not have signs of threatened circulation or respiration (systolic blood pressure > 100 mmHg and SpO2 > 95 %). An ED nurse should evaluate all patients according to the NRS and then take action to relieve pain within 15 min. The treatment target is achievement of a NRS < 4 or patient pain tolerance.
Statistical analysis
The statistics software SPSS version 22.0 (IBM, New York, USA) was used to analyze the data. The paired t-test was used for normally distributed data, and statistical significance was set at p < 0.05. The chi-square test was used to assess significant differences between the different patient groups. When more than 20 % of the squares in the chi-square calculation had an expected value less than 5, Fisher’s exact test was used. Unless otherwise specified, the percentage was calculated for the patients for whom the relevant variable was obtained.
Ethics
The Regional Committee for Medical and Health Research Ethics (REK) in Norway and the Data Protection Officer at St. Olav’s Hospital, Trondheim, approved the study.
Results
In the study, 764 patients were included (n = 764). The average age was 58.5 years (SD 26.7 years), and the proportion of women was 52.1 %. The patient distribution was characteristic of the general patient population distribution at our ED for all of 2012 with respect to age, gender, chief complaints (Emergency Symptoms and Signs (ESS) in RETTS), and acuity level. The proportion of patients who were asked about pain upon arrival at the ED was 77 % (n = 586), and the group was not significantly different from the group that was not asked about pain with respect to age, gender, and acuity level. In the group that was not asked about pain (23 %, n = 178), 10.5 % of the patients had a systolic blood pressure below 100 mmHg (average 132 mmHg, SD 26 mmHg), whereas in the group that was asked about pain, 2.6 % (average 137 mmHg, SD 23 mmHg) had a lower blood pressure (p = 0.000). There was also a significant difference in the average blood pressure between the two groups (p = 0.022). At the same time, significantly more patients with oxygen saturation below 95 % were not asked about pain (25.8 % versus 12.0 %, χ2 = 15.772, df = 1, p = 0,000). The difference in the mean oxygen saturation was relatively small but significant, with values of 97.5 % and 95.8 %, respectively, among the patients asked about pain and those not asked about pain (p = 0.011). The most common chief complaints in both groups were abdominal pain, chest pain, breathing difficulties, and neurological and infectious conditions. The differences between the patients who were and were not asked about pain are shown in Table 1.
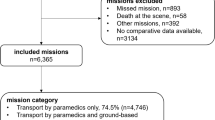
Of the patients who were asked about pain (n = 586), 58 % (n = 340) stated that they were in pain (Fig. 1) and 66.5 % (n = 226) indicated that they had pain that was more severe than mild (NRS > 3). There was no significant age difference between the patients who were asked about pain and those who were not asked about pain; however, there were significantly more women than men who were not asked about pain (80.5 and 73.8 %, respectively; χ2 = 4.733, df = 1, p = 0.03).
According to the local ED procedures, the goal is to treat all patients with moderate and severe pain. The average pain scores in patients who reported pain on arrival to the ED was 4.9 (median 5.0). There was no significant difference in the pain scores between those who were and were not treated for their pain (4.59 versus 4.91). Of the group of patients with moderate and severe pain (NRS > 3; n = 226), 14.2 % (n = 32) were treated with pain medications. There was no difference in age (p = 0.544) or gender (p = 0.188) between the patients who did or did not receive analgesia. The study was not designed to identify the drugs or interventions that were used for pain management.
Discussion
This study reveals a known phenomenon; specifically, patients do not receive optimal assessment and treatment of pain in the ED. Twenty-three percent of patients were not asked about their pain, and only 14.3 % of the patients who reported moderate to severe pain received treatment for their pain. A study by Barletta and colleagues showed a significant difference in the pain scores between patients who received pain treatment and those who did not [25], but there was no such trend in our study. Additionally, the average pain score of 4.9 is somewhat lower than that found in other studies [26].
Other hospitals that also have guidelines for pain management additionally struggle with low compliance with pain level documentation. Only 49.2 % of the patients were asked about their pain in triage [27], and, of these patients, 41.3 % had severe pain, 38.8 % had moderate pain, and 19.8 % had mild pain. Although pain management is a fundamental aspect of emergency care, there are several attitudinal and structural barriers to efficient and adequate pain management in the ED [28]. Interestingly, some of the nurses had written explanations for the lack of assessment of pain or treatment on the patient assessment form. These reasons included communication barriers and language problems, altered mental status and intoxication, dementia or difficulty in describing pain, intermittent or occasional nature of the pain, patient received prehospital treatment or analgesia at home, and patient refusal. It is worth noticing that there are significant inter-rater differences in pain score on ED arrival between patients and emergency health care providers [29], and nurses tend to underestimate pain often than physicians [30, 31]. It is known that the subjective experience of pain, provider gender, misapprehension, prejudice among health care providers, stress, work pressure, and relatively short and intense patient interaction in the ED may affect the quality of pain management [32–38]. Additionally, a patient’s age, gender, race, and ethnicity may be of significance [39, 40]. Young age and female gender are factors that increase the likelihood of pain [26, 41], but we found no difference between the gender and age of patients who experienced pain. However, we found that female patients were less likely to be assessed for pain. Emergency signs and symptoms (ESS) coincided with previous studies in our ED [42], and patients who were not asked about pain presented with similar issues and priorities compared with the group that was asked about pain.
Pain in the elderly is a common problem in the ED [43], and pain management in the elderly can be challenging because these patients are at an increased risk for adverse effects of analgesics [44]. Older patients are less likely to experience pain in the ED, and increasing age predicts inadequate analgesia administration [45]. Nevertheless, we found no significant difference in the proportion of patients over 64 years of age who were and were not asked about pain.
Of the patients with moderate to severe pain, few received pain management in the ED. There was no difference in age or gender between the patients who did or did not receive analgesics. In one study [46], approximately 50 % of the patients were asked about pain, which is lower than the percentage in our study. Forty-three percent stated that they had moderate to severe pain, but only 25 % of these patients received pain medication. In comparison, only 14.3 % of similar patients in our ED received any treatment for pain. Other studies reveal that 50–60 % of patients who report pain in the ED receive pain management [26].
Adequate pain management should be a primary goal of health care professionals in the ED, but the pain assessment and treatment performed by nurses have been shown to be suboptimal [36]. The documentation of pain during triage and protocols that give nurses the opportunity to initiate treatment are associated with better pain management [27]. However, guidelines and protocols have little effect on the improvement of pain treatment as a single initiative [47]. Current local protocol does not require pain assessment in all patients in our ED. A series of interventions intended to improve pain treatment in the ED has been suggested, but there is no currently accepted universal model [48]. Other countries have accepted pain management in the ED as a quality indicator [49] and this will likely be adapted in Norway [50]. The first step in improving the pain assessment and management in the ED is to accurately and systematically assess every patient. To improve the assessment and treatment of pain in patients in the ED, a local framework focusing on knowledge, communication, emergency organization, and patient flow must be established [51, 52]. This approach requires a change in attitude among health workers and frequent evaluation and feedback [47, 53]. The ED staff needs to have knowledge of the patient population and to continuously measure the quality of pain management. Adapting a local protocol alone seems to give suboptimal pain assessment in the ED.
Conclusion
Pain is one of the most common reasons for seeking emergency medical care; thus, it is important for healthcare professionals to focus on effectively assessing and treating pain. Despite guidelines and in-service educational programs, the assessment and treatment of pain in our ED are inadequate. This prospective study reveals that the management of pain is not in accordance with internal procedures. Pain management is accepted as a quality indicator of care, and additional focus on strategies to improve pain management in the ED is necessary to ensure that all patients receive optimal pain assessment and treatment.
References
Lanser P, Gesell S. Pain management: the fifth vital sign. Healthc Benchmarks. 2001;8(6):68–70. 62.
McCaig LF, Nawar EW. National Hospital Ambulatory Medical Care Survey: 2004 emergency department summary. Adv Data. 2006;23(372):1–29.
Fosnocht DE, Heaps ND, Swanson ER. Patient expectations for pain relief in the ED. Am J Emerg Med. 2004;22(4):286–8.
Lecky F, Benger J, Mason S, Cameron P, Walsh C, On behalf of the IQSWG. The International Federation for Emergency Medicine framework for quality and safety in the emergency department. Emerg Med J. 2013. doi:10.1136/emermed-2013-203000.
Schull MJ, Guttmann A, Leaver CA, Vermeulen M, Hatcher CM, Rowe BH, et al. Prioritizing performance measurement for emergency department care: consensus on evidence-based quality of care indicators. CJEM. 2011;13(5):300–9. E28-43.
Gueant S, Taleb A, Borel-Kuhner J, Cauterman M, Raphael M, Nathan G, et al. Quality of pain management in the emergency department: results of a multicentre prospective study. Eur J Anaesthesiol. 2011;28(2):97–105. doi:10.1097/EJA.0b013e3283418fb0.
Gordon DB, Dahl JL, Miaskowski C, McCarberg B, Todd KH, Paice JA, et al. American pain society recommendations for improving the quality of acute and cancer pain management: American Pain Society Quality of Care Task Force. Arch Intern Med. 2005;165(14):1574–80. doi:10.1001/archinte.165.14.1574.
Holleran RS. The problem of pain in emergency care. Nurs Clin North Am. 2002;37(1):67–78. vi-vii.
Macintyre PE, Walker SM. The scientific evidence for acute pain treatment. Curr Opin Anaesthesiol. 2010;23(5):623–8. doi:10.1097/ACO.0b013e32833c33ed.
Arendts G, Fry M. Factors associated with delay to opiate analgesia in emergency departments. J Pain. 2006;7(9):682–6. doi:10.1016/j.jpain.2006.03.003.
Rupp T, Delaney KA. Inadequate analgesia in emergency medicine. Ann Emerg Med. 2004;43(4):494–503. doi:10.1016/S0196064403012265.
Niska R, Bhuiya F, Xu J. National Hospital Ambulatory Medical Care Survey: 2007 emergency department summary. Natl Health Stat Report. 2010;6(26):1–31.
Guru V, Dubinsky I. The patient vs. caregiver perception of acute pain in the emergency department. J Emerg Med. 2000;18(1):7–12.
Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52(2):126–36. doi:10.1016/j.annemergmed.2008.03.014.
Finn JC, Rae A, Gibson N, Swift R, Watters T, Jacobs IG. Reducing time to analgesia in the emergency department using a nurse-initiated pain protocol: a before-and-after study. Contemp Nurse. 2012;43(1):29–37. doi:10.5172/conu.2012.43.1.29.
Augarten A, Zaslansky R, Matok Pharm I, Minuskin T, Lerner-Geva L, Hirsh-Yechezkel G, et al. The impact of educational intervention programs on pain management in a pediatric emergency department. Biomed Pharmacother. 2006;60(7):299–302. doi:10.1016/j.biopha.2006.06.013.
Holdgate A, Shepherd SA, Huckson S. Patterns of analgesia for fractured neck of femur in Australian emergency departments. Emerg Med Australas. 2010;22(1):3–8. doi:10.1111/j.1742-6723.2009.01246.x.
Dahl JL. MSJAMA: improving the practice of pain management. JAMA. 2000;284(21):2785.
Terrell KM, Hustey FM, Hwang U, Gerson LW, Wenger NS, Miller DK, et al. Quality indicators for geriatric emergency care. Acad Emerg Med. 2009;16(5):441–9. doi:10.1111/j.1553-2712.2009.00382.x.
Jensen MP, Karoly P. Self-report svales and procedures for assessing pain in adults. Handbook for pain assessment. 2. utgave ed. New York: Guildford Press; 2001.
Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Hals EK, et al. Assessment of pain. Br J Anaesth. 2008;101(1):17–24. doi:10.1093/bja/aen103.
Stang AS, Hartling L, Fera C, Johnson D, Ali S. Quality indicators for the assessment and management of pain in the emergency department: a systematic review. Pain Res Manag. 2014;19(6):e179–90.
Bjornsen LP, Uleberg O, Dale J. Patient visits to the emergency department at a Norwegian university hospital: variations in patient gender and age, timing of visits, and patient acuity. Emerg Med J. 2013;30(6):462–6. doi:10.1136/emermed-2012-201191.
Widgren BR, Jourak M, Martinius A. New accurate triage method. METTS-A yields basis for priority level decisions. Lakartidningen. 2008;105(4):201–4.
Barletta JF, Erstad BL, Loew M, Keim SM. A prospective study of pain control in the emergency department. Am J Ther. 2000;7(4):251–5.
Todd KH, Ducharme J, Choiniere M, Crandall CS, Fosnocht DE, Homel P, et al. Pain in the emergency department: results of the pain and emergency medicine initiative (PEMI) multicenter study. J Pain. 2007;8(6):460–6. doi:10.1016/j.jpain.2006.12.005.
Fry M, Bennetts S, Huckson S. An Australian audit of ED pain management patterns. J Emerg Nurs. 2011;37(3):269–74. doi:10.1016/j.jen.2010.03.007.
Venkat A, Fromm C, Isaacs E, Ibarra J, Committee SE. An ethical framework for the management of pain in the emergency department. Acad Emerg Med. 2013;20(7):716–23. doi:10.1111/acem.12158.
Baharuddin KA, Mohamad N, Nik Abdul Rahman NH, Ahmad R, Nik Him NA. Assessing patient pain scores in the emergency department. Malays J Med Sci. 2010;17(1):17–22.
Drayer RA, Henderson J, Reidenberg M. Barriers to better pain control in hospitalized patients. J Pain Symptom Manage. 1999;17(6):434–40.
Choiniere M, Melzack R, Girard N, Rondeau J, Paquin MJ. Comparisons between patients’ and nurses’ assessment of pain and medication efficacy in severe burn injuries. Pain. 1990;40(2):143–52.
Eder SC, Sloan EP, Todd K. Documentation of ED patient pain by nurses and physicians. Am J Emerg Med. 2003;21(4):253–7.
Tanabe P, Buschmann M. Emergency nurses’ knowledge of pain management principles. J Emerg Nurs. 2000;26(4):299–305. doi:10.1067/men.2000.108402.
Hwang U, Richardson LD, Sonuyi TO, Morrison RS. The effect of emergency department crowding on the management of pain in older adults with hip fracture. J Am Geriatr Soc. 2006;54(2):270–5. doi:10.1111/j.1532-5415.2005.00587.x.
Wilsey BL, Fishman SM, Crandall M, Casamalhuapa C, Bertakis KD. A qualitative study of the barriers to chronic pain management in the ED. Am J Emerg Med. 2008;26(3):255–63. doi:10.1016/j.ajem.2007.05.005.
Rampanjato RM, Florence M, Patrick NC, Finucane BT. Factors influencing pain management by nurses in emergency departments in Central Africa. Emerg Med J. 2007;24(7):475–6. doi:10.1136/emj.2006.045815.
Pines JM, Hollander JE. Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008;51(1):1–5. doi:10.1016/j.annemergmed.2007.07.008.
Safdar B, Heins A, Homel P, Miner J, Neighbor M, DeSandre P, et al. Impact of physician and patient gender on pain management in the emergency department--a multicenter study. Pain Med. 2009;10(2):364–72. doi:10.1111/j.1526-4637.2008.00524.x.
Stephenson N, Dalton JA, Carlson J, Youngblood R, Bailey D. Racial and ethnic disparities in cancer pain management. J Natl Black Nurses Assoc. 2009;20(1):11–8.
Ezenwa MO, Ameringer S, Ward SE, Serlin RC. Racial and ethnic disparities in pain management in the United States. J Nurs Scholarsh. 2006;38(3):225–33.
Karwowski-Soulie F, Lessenot-Tcherny S, Lamarche-Vadel A, Bineau S, Ginsburg C, Meyniard O, et al. Pain in an emergency department: an audit. Eur J Emerg Med. 2006;13(4):218–24. doi:10.1097/01.mej.0000217975.31342.13.
Langlo NM, Orvik AB, Dale J, Uleberg O, Bjornsen LP. The acute sick and injured patients: an overview of the emergency department patient population at a Norwegian University Hospital Emergency Department. Eur J Emerg Med. 2014;21(3):175–80. doi:10.1097/MEJ.0b013e3283629c18.
Platts-Mills TF, Esserman DA, Brown DL, Bortsov AV, Sloane PD, McLean SA. Older US emergency department patients are less likely to receive pain medication than younger patients: results from a national survey. Ann Emerg Med. 2012;60(2):199–206. doi:10.1016/j.annemergmed.2011.09.014.
Hwang U, Richardson LD, Harris B, Morrison RS. The quality of emergency department pain care for older adult patients. J Am Geriatr Soc. 2010;58(11):2122–8. doi:10.1111/j.1532-5415.2010.03152.x.
Jones JS, Johnson K, McNinch M. Age as a risk factor for inadequate emergency department analgesia. Am J Emerg Med. 1996;14(2):157–60. doi:10.1016/S0735-6757(96)90123-0.
Ware LJ, Epps CD, Clark J, Chatterjee A. Do ethnic differences still exist in pain assessment and treatment in the emergency department? Pain Manag Nurs. 2012;13(4):194–201. doi:10.1016/j.pmn.2010.06.001.
Ducharme J. Clinical guidelines and policies: can they improve emergency department pain management? J Law Med Ethics. 2005;33(4):783–90.
Sampson FC, Goodacre SW, O’Cathain A. Interventions to improve the management of pain in emergency departments: systematic review and narrative synthesis. Emerg Med J. 2014;31(e1):e9–18. doi:10.1136/emermed-2013-203079.
J. Heyworth. Emergency Department Clinical Quliaty Indicators: - A CEM guide to implementation. The College of Emergency Medicine. London. 2011. www.rcem.ac.uk/code/document.asp?ID=5832. Accessed 22 Oct 2015.
Faglige og organisatoriske kvalitetskrav for somatiske akuttmottak. “Medical and organizational requirements for somatic emergency departments”. Oslo: Directorate of Health; 2014.
Berben SA, Meijs TH, van Grunsven PM, Schoonhoven L, van Achterberg T. Facilitators and barriers in pain management for trauma patients in the chain of emergency care. Injury. 2012;43(9):1397–402. doi:10.1016/j.injury.2011.01.029.
Shaban RZ, Holzhauser K, Gillespie K, Huckson S, Bennetts S. Characteristics of effective interventions supporting quality pain management in Australian emergency departments: an exploratory study. AENJ. 2012;15(1):23–30. doi:10.1016/j.aenj.2011.11.003.
Richards CF. Establishing an emergency department pain management system. Emerg Med Clin North Am. 2005;23(2):519–27. doi:10.1016/j.emc.2004.12.014.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
JD and LPB conceived and designed this study. JD and LPB conducted the data analysis. LPB and JD drafted the manuscript. LPB prepared the figures. Both authors interpreted the data and critically revised the manuscript. Both authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Dale, J., Bjørnsen, L.P. Assessment of pain in a Norwegian Emergency Department. Scand J Trauma Resusc Emerg Med 23, 86 (2015). https://doi.org/10.1186/s13049-015-0166-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13049-015-0166-3