Abstract
Background
Prediction of the return of spontaneous circulation (ROSC) in cardiac arrest patients is a parameter for deciding when to stop cardiopulmonary resuscitation (CPR) or to start extracorporeal CPR. We investigated the change in transcutaneous PCO2 (PtcCO2) in cardiac arrest patients.
Methods
This study was carried out as a retrospective chart review. Patients with out-of-hospital cardiac arrest or in-hospital cardiac arrest within the emergency department were included. PtcCO2 monitoring with a V-Sign™ combined monitor (SenTec Inc., Therwil, Switzerland) was applied to patients at the start of CPR. We divided the included patients into the ROSC group and the no ROSC group. The ROSC group was subdivided into those achieving ROSC <15 min CPR and >15 min CPR. The change in the PtcCO2 value was analyzed at 0 min, 5 min, 10 min, and 15 min from PtcCO2 stabilization and was compared among the groups.
Results
A total of 42 patients were enrolled. Twenty-eight patients achieved ROSC; 13 patients achieved ROSC <15 min CPR and 15 patients achieved ROSC >15 min CPR. Fourteen patients expired without ROSC. The absolute values of PtcCO2 was lower in the ROSC group than in the no ROCS group. The PtcCO2 change over time had a tendency to decrease or to remain constant in the ROSC groups. In contrast, all patients in the no ROSC group experienced an increase in the PtcCO2 change during CPR except one case.
Conclusions
PtcCO2 monitoring provides non-invasive, continuous, and useful monitoring in cardiac arrest patients.
Similar content being viewed by others
Background
The return of spontaneous circulation (ROSC) in cardiac arrest patients is meaningful for several reasons. It can help in deciding when to stop cardiopulmonary resuscitation (CPR). It also provides a parameter that can help decide when to start extracorporeal CPR (ECPR) despite the fact that the indication for CPR varies across critical care settings [1]. Many factors such as etiology, witnessed or not, location, initial electrocardiogram (ECG), bystander CPR, and time to hospital, are considered to predict ROSC. End-tidal CO2 (etCO2) monitoring has been known, heretofore, as a useful tool to predict the ROSC of a cardiac arrest patient [2]. However, several factors affect etCO2, such as airway obstruction, low cardiac output, and pulmonary edema, which are frequently found in cardiac arrest patients [3].
Transcutaneous PCO2 (PtcCO2) monitoring was introduced about 30 years ago. With advances in technology, the use of PtcCO2 monitoring has been expanded to adult patients [4]-[7]. In several clinical situations, a PtcCO2 analysis is preferred to an etCO2 analysis [8]-[10].
We observed that PtcCO2 monitoring is easily applied to and gives continuous information on gas changes in critically ill patients. Some investigators have reported that PtcCO2 shows good agreement with PaCO2 under the condition of adequate cardiac output, but it becomes flow-dependent during a low-flow shock in a laboratory, intensive care unit, or operating room [11],[12]. On the basis of these findings, in this study, we investigated the change of PtcCO2 in cardiac arrest patients.
Materials and methods
This study was carried out as a retrospective chart review and approved by the institutional review board of Korea University Guro Hospital. The study was conducted in Korea University Guro Hospital Emergency Department (ED) from March 2013 to December 2013. Patients with out-of-hospital cardiac arrest (OHCA) or in-hospital cardiac arrest (IHCA) within the ED were included. We excluded cases for whom transcutaneous monitoring was not applied or that failed to provide sufficient quality of PtcCO2 monitoring data. We also excluded patients under the age of 18 years. We divided the included patients into ROSC and no ROSC. The ROSC group was again divided into the ROSC in less than 15 min of CPR and the ROSC in more than 15 min of CPR. In this study, ROSC was defined as a case in which the evidence of a palpable pulse or a measurable blood pressure was sustained for >20 min.
The PtcCO2 monitoring device was a V-Sign™ combined monitor (SenTec Inc., Therwil, Switzerland). The V-Sign™ combined monitor is composed of display device and sensor using a heated electrode membrane. When a sensor is attached to the patient’s earlobe, it is heated up to 42°C. As the heated membrane vasodilates the skin capillaries, PtcCO2 comes in agreement with arterial PCO2.The waveform of PtcCO2 is displayed on a monitor, and it stabilizes in about 5 min after attachment of the sensor.
Two investigators who were blinded to the study objectives reviewed the patient charts. The collected data were gender, age, location of cardiac arrest, bystander CPR, OHCA versus IHCA, duration of CPR in the hospital, epinephrine used in the first 15 min of in-hospital CPR, time from the EMS call to hospital arrival, sodium bicarbonate use, and initial PtcCO2. The change in PtcCO2 during CPR was investigated in the ROSC <15 minute CPR group, the ROSC >15 minute CPR group, and the no ROSC group. The PtcCO2 value was analyzed at 0 min, 5 min, 10 min, and 15 min from the PtcCO2 stabilization and was compared in three groups. When the two chart reviewers reported conflicting data for continuous variables, the mean value was used in the continuous variables. For categorical variables, a third investigator reviewed the chart and determined which data were to be used.
For statistics, the Kruskal-Wallis test was used to compare the mean value of the continuous variables, and the chi-squared analysis was used for categorical variables with the SPSS 17.0 software package (IBM, Chicago, IL, USA). Repeated measures ANOVA with a post hoc test was used to test for the significance of the change in PtcCO2 value with time. We considered a p value of less than 0.05 to be statistically significant.
Results
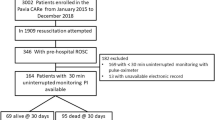
A total of 154 patients received CPR in the ED during a 10-month period. One hundred twelve patients were excluded because PtcCO2 monitoring was not applied to them; PtcCO2 monitoring failed to provide sufficient quality of data for the analysis; or they were pediatric patients under the age of 18 years. In the end, 42 patients were enrolled (Figure 1). Clinical data on the included patients are presented in Table 1. Thirteen patients achieved ROSC in less than 15 min from the start of CPR, 15 patients achieved ROSC after 15 min CPR, and 14 patients expired without ROSC. Age, gender, bystander CPR and OHCA versus IHCA did not show differences among the three groups. Time from EMS call to hospital arrival in OHCA was 25.3 ± 10.4 min in the ROSC <15 min CPR group, 31.4 ± 6.5 min in the ROSC >15 min CPR group and 27.8 ± 14.6 min in the no ROSC (p >0.05). The rate of sodium bicarbonate use was the highest in the ROSC >15 min CPR group, and the duration of CPR in the hospital was the longest in the no ROSC group. Initial PtcCO2 was 49.1 ± 22.0 mmHg in the ROSC <15 min CPR group, 78.6 ± 33.5 mmHg in the ROSC >15 min CPR group and 84.9 ± 49.1 mmHg in the no ROSC group (p <0.05). The absolute values of PtcCO2 were higher and more widely distributed widely in the no ROSC patients than in the ROSC patients (Figure 2). The change in PtcCO2 over time, relative to baseline, is shown in Figure 3. The PtcCO2 change over time had a tendency to decrease or to remain constant in the ROSC patients. In contrast, all patients in the no ROSC group experienced an increase in the PtcCO2 change during CPR except in one case.
The absolute value of PtcCO 2 over time in patients with cardiopulmonary resuscitation. PtcCO2, partial pressure of transcutaneous carbon dioxide tension; ROSC, return of spontaneous circulation; CPR, cardiopulmonary resuscitation. *p <0.05 vs. PtcCO2 in no ROSC according to a post hoc test (A. ROSC < 15 min CPR, B. ROSC > 15 min CPR, C. No ROSC).
The change in PtcCO 2 over time in patients with cardiopulmonary resuscitation. PtcCO2, partial pressure of transcutaneous carbon dioxide tension; ROSC, return of spontaneous circulation; △ PtcCO2, the change in PtcCO2 from baseline. *p <0.05 vs. PtcCO2 in no ROSC according to a post hoc test (A. ROSC < 15 min CPR, B. ROSC > 15 min CPR, C. No ROSC).
Discussion
The chance of survival from cardiac arrest cannot be accurately predicted by physicians. Decisions concerning CPR are difficult in two ways. First, it would be better to stop CPR in cases such as terminal cancer or prolonged CPR. Second, however, if ROSC does not occur, extending the resuscitative effort may be appropriate in some cases [13]. Nowadays, the increasing role of extracorporeal cardiopulmonary resuscitation (ECPR) is highlighted for patients failing conventional resuscitation [14]. Despite the fact that opinions on the indications for ECPR vary among operators, ECPR was provided to patients with witnessed cardiac arrest and a brief “no flow” time; if there was no recovery of cardiac function within 20 min of CPR [15],[16]. Thus, ROSC has a large significance in the determination of continuing CPR, while it is also meaningful for planning ECPR in a case with a low possibility of ROSC.
In the case of cardiac arrest, with the assumption that the CO2 production is constant, CO2 accumulates within the blood in the arrest patient as it cannot be washed out through ventilation. If systemic blood and pulmonary blood flow are recovered by CPR, the PCO2 value will drop while increasing the chance of ROSC. However, continuous gas monitoring is difficult during CPR. Invasive monitoring such as arterial blood gas analysis or central ScvO2 can be performed after patient stabilization. Several studies confirmed that the etCO2 is correlated with the cardiac output produced by CPR. In recent years, etCO2 monitoring by capnography has been recognized as a useful procedure in monitoring cardiac arrest patients [17]-[19]. It has the advantage of easy application and non-invasiveness. Nevertheless, it has some limitations in a CPR situation as noted in the introduction.
As shown in Figure 2, the absolute values of PtcCO2 were higher and more widely distributed in the no ROSC patients than in the ROSC patients; PtcCO2 becomes flow-dependent during a low-flow shock [11],[12]. Figure 3 represents the change in PtcCO2 in each patient during CPR. In the no ROSC patients, the PtcCO2 value was high and its change increased over time except in one patient. In contrast, these findings were not observed in the ROSC patients. We presumed that the decreased systemic blood flow with the decreased wash-out of CO2 from the lung contributes to these results in the no ROSC group, which indicates that PtcCO2 reflects changes in the systemic blood flow and the pulmonary blood flow. While end-tidal CO2 monitoring provides an indirect inference for the systemic blood flow change, PtcCO2 monitoring has the merit of allowing for the direct assessment of the systemic blood flow change.
As shown in Table 1, clinical characteristics were not different among three groups except for the frequency of sodium bicarbonate use, epinephrine used in the first 15 min in-hospital, and the duration of CPR in the hospital. The difference in epinephrine used in the first 15 min in-hospital and the duration of CPR in the hospital were due to dividing the groups by duration criteria. The higher rate of sodium bicarbonate use in the ROSC >15 min CPR group than in the ROSC <15 min may be due to the relatively more unstable clinical condition of the ROSC >15 min CPR group. The higher rate of sodium bicarbonate use in the ROSC >15 min CPR group than in the no ROSC group may be due to the increased success rate of arterial puncture upon recovering the pulse pressure after ROSC. The physicians might have decided to use sodium bicarbonate after confirming acidosis by an arterial blood gas analysis. Therefore, it is likely that sodium bicarbonate was used in a fair number of cases in the ROSC >15 min CPR group after CPR had been administered for at least 15 min. Even if sodium bicarbonate was administrated during the first 15 min of CPR in the ROSC >15 min CPR group, the difference in the PtcCO2 change between the ROSC >15 min CPR group and the no ROSC group would have been much greater.
As shown in Table 1, the duration of CPR was understandably longer in the no ROSC group than in the ROSC >15 min CPR group. The results of PtcCO2 in the no ROSC group and in the ROSC >15 min CPR group were not influenced by the CPR time because the analysis of the PtcCO2 change was done within the first 20 min of CPR.
This study has another limitation. Our observations were limited to a small sample. This study was done by retrospective chart review and there was no intervention for applying PtcCO2 monitoring during study period. As a result, only 33.8% of the cardiac arrest patients underwent PtcCO2 monitoring. Therefore, although this study result seems plausible, further research should be done to confirm this result.
Conclusion
PtcCO2 monitoring provides non-invasive, continuous, and useful monitoring in cardiac arrest patients. Further study is warranted to confirm the use of PtcCO2 monitoring for ROSC.
Provenance and peer review
Not commissioned; externally peer reviewed.
References
Wang CH, Chen YS, Ma MH: Extracorporeal life support. Curr Opin Crit Care. 2013, 19: 202-207. 10.1097/MCC.0b013e32836092a1.
Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW, Kudenchuk PJ, Ornato JP, McNally B, Silvers SM, Passman RS, White RD, Hess EP, Tang W, Davis D, Sinz E, Morrison LJ: Adult advanced cardiovascular life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010, 122: S729-S767. 10.1161/CIRCULATIONAHA.110.970988.
Lucangelo U, Blanch L: Dead space. Intensive Care Med. 2004, 30: 576-579. 10.1007/s00134-004-2194-8.
Eberhard P: The design, use, and results of transcutaneous carbon dioxide analysis: current and future directions. Anesth Analg. 2007, 105: S48-S52. 10.1213/01.ane.0000278642.16117.f8.
Rosner V, Hannhart B, Chabot F, Polu JM: Validity of transcutaneous oxygen/carbon dioxide pressure measurement in the monitoring of mechanical ventilation in stable chronic respiratoryfailure. Eur Respir J. 1999, 13: 1044-1047. 10.1034/j.1399-3003.1999.13e18.x.
Sanders MH, Kern NB, Costantino JP Stiller RA, Strollo PJ, Studnicki KA, Coates JA, Richards TJ: Accuracy of end-tidal and transcutaneous PCO2 monitoring during sleep. Chest. 1994, 106: 472-483. 10.1378/chest.106.2.472.
Cuvelier A, Grigoriu B, Molano LC, Muir F: Limitations of transcutaneous carbon dioxide measurements for assessing long-term mechanical ventilation. Chest. 2005, 127: 1744-1748. 10.1378/chest.127.5.1744.
McBride DS, Johnson JO, Tobias JD: Noninvasive carbon dioxide monitoring during neurosurgical procedures in adults: end-tidal versus transcutaneous techniques. South Med J. 2002, 95: 870-874. 10.1097/00007611-200295080-00018.
Wilson J, Russo P, Russo J, Tobias JD: Noninvasive monitoring of carbon dioxide in infants and children with congenital heart disease: end-tidal versus transcutaneous techniques. J Intensive Care Med. 2005, 20: 291-295. 10.1177/0885066605278652.
Casati A, Squicciarini G, Malagutti G, Baciarello M, Putzu M, Fanelli A: Transcutaneous monitoring of partial pressure of carbon dioxide in the elderly patient: a prospective, clinical comparison with end-tidal monitoring. J Clin Anesth. 2006, 18: 436-440. 10.1016/j.jclinane.2006.02.007.
Beran AV, Tolle CD, Huxtable RF: Cutaneous blood flow and its relationship to transcutaneous O2/CO2 measurements. Crit Care Med. 1981, 9: 736-741. 10.1097/00003246-198110000-00013.
Tremper KK, Shoemaker WC, Shippy CR, Nolan LS: Transcutaneous PCO2 monitoring on adult patients in the ICU and the operating room. Crit Care Med. 1981, 9: 752-755. 10.1097/00003246-198110000-00017.
Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Part 2: Ethical aspects of CPR and ECC. Circulation. 2000, 102: I12-I21.
Dalton HJ, Tucker D: Resuscitation and extracorporeal life support during cardiopulmonary resuscitation following the Norwood (stage 1) operation. Cardiol Young. 2011, 21 (Suppl. 2): 101-108. 10.1017/S1047951111001673.
Delmo Walter EM, Alexi-Meskishvili V, Huebler M, Redlin M, Boettcher W, Weng Y, Berger F, Hetzer R: Rescue extracorporeal membrane oxygenation in children with refractory cardiac arrest. Interact Cardiovasc Thorac Surg. 2011, 12: 929-934. 10.1510/icvts.2010.254193.
Wolf MJ, Kanter KR, Kirshbom PM, Kogon BE, Wagoner SF: Extracorporeal cardiopulmonary resuscitation for pediatric cardiac patients. Ann Thorac Surg. 2012, 94: 874-879. 10.1016/j.athoracsur.2012.04.040.
Falk JL, Rackow EC, Weil MH: End-tidal carbon dioxide concentration during cardiopulmonary resuscitation. N Engl J Med. 1988, 318: 607-611. 10.1056/NEJM198803103181005.
Callaham M, Barton C: Prediction of outcome of cardiopulmonary resuscitation from end-tidal carbon dioxide concentration. Crit Care Med. 1990, 18: 358-362. 10.1097/00003246-199004000-00002.
White RD, Asplin BR: Out-of-hospital quantitative monitoring of end-tidal carbon dioxide pressure during CPR. Ann Emerg Med. 1994, 23: 25-30. 10.1016/S0196-0644(94)70003-6.
Funding
This manuscript was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (R1009983) and was partially supported by a Korea University Grant.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
SJP, JYK and YDC managed the data and critical revisions to the manuscript. SWM made critical revisions to the manuscript. YHY and SHC conceived the research and drafted the manuscript. Each authors has read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Choi, SH., Kim, JY., Yoon, YH. et al. The use of transcutaneous CO2 monitoring in cardiac arrest patients: a feasibility study. Scand J Trauma Resusc Emerg Med 22, 70 (2014). https://doi.org/10.1186/s13049-014-0070-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13049-014-0070-2