Abstract
Background
Ingrown toenails are a common nail pathology. When conservative treatments are ineffective, a surgical approach is often utilised. Despite recent narrative reviews, there is a need for an up-to-date and rigorous systematic review of surgical methods for treating ingrown toenails.
Methods
Five databases (MEDLINE, Embase, CINAHL, Web of Science and CENTRAL) and two registers (Clinicaltrials.gov and ISRCTN) were searched to January 2022 for randomised trials evaluating the effects of a surgical intervention(s) for ingrown toenails with a follow-up of at least 1 month. Two independent reviewers screened records, extracted data, assessed risk of bias and certainty of evidence.
Results
Of 3,928 records identified, 36 (3,756 participants; 62.7% males) surgical interventions were included in the systematic review and 31 studies in the meta-analysis. There was very low quality evidence that using phenol with nail avulsion vs nail avulsion without phenol reduces the risk of recurrence (risk ratio [RR] 0.13 [95% CI 0.06 to 0.27], p < 0.001). No favourable effect was observed between chemical or surgical vs conservative management (0.55 [0.19 to 1.61], p = 0.280; 0.72 [0.33 to 1.56], p = 0.410), chemical or surgical vs other (e.g., CO2 laser, electrocautery) (1.61 [0.88 to 2.95], p = 0.120; 0.58 [0.25 to 1.37], p = 0.220), chemical vs surgical (0.75 [0.46 to 1.21], p = 0.230), surgical vs surgical (0.42 [0.21 to 0.85]), chemical vs chemical (0.19 [0.01 to 3.80], p = 0.280), surgical vs surgical + chemical (3.68 [0.20 to 67.35], p = 0.380), chemical vs surgical + chemical (1.92 [0.06 to 62.30], p = 0.710), local anaesthetic vs local anaesthetic + adrenaline (1.03 [0.22 to 4.86], p = 0.970), chemical timings 30 s vs 60 s (2.00 [0.19 to 21.41]) or antibiotics vs no antibiotics (0.54 [0.12 to 2.52], p = 0.430). Central toenail resection was the only procedure to significantly relieve symptoms (p = 0.001) but data were only available up to 8 weeks post-surgery.
Conclusion
Despite the high number of publications, the quality of research was poor and the conclusions that can be inferred from existing trials is limited. Phenolisation of the nail matrix appears to reduce the risk of recurrence following nail ablation, and with less certainty 1 min appears to be the optimum time for application. Despite this being a widely performed procedure there remains a lack of good quality evidence to guide practice.
Similar content being viewed by others
Introduction
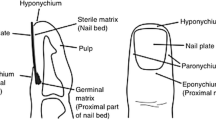
An ingrown toenail, or onychocryptosis, is a common problem that occurs when the nail plate punctures the periungual skin causing substantial pain, inflammation, discomfort and increased risk of infection if left untreated [1]. Most cases occur in the hallux and typically present in teenagers and young adults, although may present at any age [2, 3]. Several factors have been proposed as contributory to the occurrence or worsening of ingrown toenails with varying degrees of evidence. These include poor nail cutting technique, hyperhidrosis, ill-fitting footwear, nail deformity, trauma, obesity, and peripheral oedema [4, 5].
Multiple semi-quantitative classification systems have been developed to classify ingrown toenails. Most focus on the severity of ingrown toenails, and generally have three stages: mild (stage I), moderate (stage II) and severe (stage III) [6,7,8]. Although, more recently an alternative approach has been suggested that focusses on the shape of the nail plate and aetiology of the pathology [8]. The performance of these classification systems has not been evaluated but have been proposed as a basis upon which to base treatment decisions.
Conservative approaches in the form of appropriate nail cutting and spicule removal, soaking in warm water, guttering, and orthonyxia (nail bracing) have all been advocated in the literature for use in mild to moderate stages (stage I and II) with varying success rates and quality of evidence [5, 8]. However, when conservative treatment fails, where there is nail deformity, or in more severe cases (stage II and III), a surgical approach is often recommended aiming to remove the problem part of the nail and destroy the underlying matrix to avoid recurrence [8,9,10].
Multiple surgical interventions have previously been described with most including either partial or total avulsion of the nail plate, that is often combined with ablation of the nail matrix to stop regrowth. Nail surgery is performed by a range of health professionals including GPs (general practitioners), orthopaedic surgeons, dermatologists, and podiatrists. Indeed nail surgery forms a substantial part of the workload of podiatrists, having been identified as the tenth most commonly performed procedure performed by the profession [11]. Whilst there is little published data to describe how this common nail pathology is treated in practice, it is clear that a large number of small studies have been published on the topic. Systematically searching for and reviewing these studies, pooling estimates of effectiveness, and providing recommendations for practice and future research is essential to enable evidence-based practice.
A Cochrane review published 10 years ago suggested that use of phenol reduced the likelihood of recurrence but did not differentiate between regrowth of the nail plate (which may be asymptomatic) with recurrence of symptoms [4]. The authors also found that there was insufficient evidence to make recommendations on whether more radical surgery was more effective in cases of more severe disease, or how key patient reported outcomes such as relief of symptoms, patient satisfaction, and post-operative pain were affected by nail surgery. More recent narrative reviews have been written [8, 12], and a systematic review specific to the use of phenol used a very limited search strategy, and did not adhere to key methodological principles such as prospective registration of their review [13]. Accordingly, there is a need for an up-to-date and rigorous systematic review of surgical methods for treating ingrown toenails. The aim of this study, therefore, was to systematically search and synthesise the literature relating to the effectiveness/efficacy of surgical methods for treating ingrown toenails.
Methods
The Cochrane Handbook for Systematic Reviews of Interventions [14] was used to guide the conduct of this review. The review was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [15], This review was prospectively registered at https://www.crd.york.ac.uk/prospero/ [CRD42021251938].
Eligibility criteria
Randomised controlled trials (RCTs) that evaluated the effects of a surgical intervention(s) for ingrown toenails with a follow-up period of at least 1 month were included. Trials comparing one form of surgery with another form of surgery, or a non-surgical intervention, or no intervention were included. Unpublished trials and conference abstracts were only included if the methodological descriptions were adequate to determine eligibility. Where such information was missing from the abstract, it was sought through direct contact with the author. There were no restrictions on the setting, age, or gender of participants. Studies were restricted to English, pertaining to human participants, and must have reported one of the following outcomes for inclusion. Relief of symptoms, and symptomatic regrowth (nail spicules/nail spikes) were considered co-primary outcomes in advance of conducting the searches. Healing time, postoperative complications (e.g., infection and haemorrhage), pain of operation, postoperative pain (duration and intensity) and participant satisfaction were defined as secondary outcomes. After completing searches, and screening it became clear that the majority of papers did not differentiate symptomatic/asymptomatic regrowth of the nail plate, but instead frequently conflated these and considered ‘recurrence’. This was therefore adopted as a co-primary outcome rather than ‘symptomatic regrowth’.
Search strategy
Electronic databases were searched from inception to January 2022: MEDLINE (Ovid), EMBASE (Ovid), CINAHL, Web of Science and Cochrane Central Register of Controlled Trials (CENTRAL). The search strategy (Supplementary File 1) was conducted using Medical Subject Heading (MeSH), truncation and Boolean operators. Other relevant completed and ongoing studies were also sought through screening of clinicaltrials.gov, the International Clinical Trials Registry [ISRCTN] and forward and backwards citations of included studies.
All searches were carried out by the same author and search results generated by the electronic databases were exported to Rayyan, where duplicates were removed. Abstract, titles and full text screening were conducted independently by two review authors, who recorded reasons for exclusion. Discrepancies were discussed with a third author and resolved by consensus. Review authors were not blinded to the author, institution, or the publication source of the study.
Data extraction
A modified Cochrane data extraction form was piloted and then used to extract and record information. Data extracted included: (a) general information such as author(s), title, journal and study funding; (b) trial characteristics such as study aim and objectives, study design, unit of allocation and ethical approvals; (c) participant characteristics such as setting, inclusion/exclusion criteria, sample size (number of participants and nail folds), age, gender, baseline imbalances, severity of ingrown toenails; (d) intervention and comparison group(s); (e) outcome measures including as time points, unit of measurement, outcome definition, data at baseline/follow-up and statistical methods.
Two review authors independently extracted data from the included studies, with disagreements resolved through consensus of a third review author. Where data were missing or unclear, the corresponding author(s) was contacted via email and relevant information requested. If after initial request no response was forthcoming, at least one further email was sent.
Data synthesis and analysis
Meta-analyses were conducted using Review Manager (RevMan V5.3 Cochrane Collaboration, Oxford, UK). The RevMan programme is designed to allow independent data entry by different reviewers. This ensures blinded data entry and highlights any discrepancies in values entered by reviewers. Any discrepancies between entered values was rechecked and discussed. For continuous data, pooled results were expressed as mean differences (MD), 95% confidence intervals (CI) and p values, with <0.05 considered significant. For dichotomous outcomes, pooled results were expressed as risk ratios (RR) and corresponding 95% CI, generated by RevMan. Where studies used a different assessment tool to measure the same construct, the standardised mean difference (SMD) and corresponding 95% CI was calculated. Where studies had multiple assessment time points, data were extracted for the final follow-up time point from randomisation.
Statistical heterogeneity and consistency were determined by interpreting the I2 statistic, and the following thresholds were identified a priori: 0–40% may not be important, 30–60% may represent moderate heterogeneity, 50–90% may represent substantial heterogeneity, 75–100% considerable heterogeneity [14]. If statistical heterogeneity was noted (I2 > 40%) for a particular treatment comparison, a random-effects model was used for analysis to account for expected heterogeneity between studies. Where there was no or little evidence of statistical heterogeneity, a fixed-effects model was used. The fixed-effect model assumes all studies are measuring the same treatment effect and that all differences between studies are due to random (sampling) error. The Mantel-Haenszel methods [16] is the default fixed-effect method implemented in Revman. The random-effects model assumes the treatment effect varies between the studies. This model estimates the mean of the distribution of effects and is weighted for both within-study and between-study variation. This approach uses the variance within each study and adds a second measure known as Tau2. Sensitivity analysis was performed if a substantial heterogeneity (I2 > 75%) was detected. Where data aggregation was not possible due to methodological heterogeneity, these results were summarised narratively. Potential publication bias for each outcome with more than ten studies was evaluated by visual inspection of funnel plots [17].
Certainty of evidence
The Grades of Research, Assessment, Development and Evaluation (GRADE) approach was used independently by two review authors to analyse the certainty of evidence against six domains: risk of bias/ certainty, indirectness of evidence, heterogeneity or inconsistency of effect, imprecision and publication bias [18, 19]. Disagreements were resolved by a third author.
Risk of bias
The Cochrane Risk of Bias tool (RoB 2.0) was assessed independently by two review authors to determine the validity and methodological rigor [18]. Discussion between the two review authors was utilised to resolve any discrepancies, with any disagreements resolved by a third author. Included studies were assessed on the randomisation process, deviations from the intended interventions, missing outcome data, measurement of the outcome and selection of the reported result, with each domain judged as ‘low’, ‘some concerns’, or ‘high’ risk. The overall RoB judgement was derived from the highest classified domain.
In this paper we present analysis for our primary outcomes and secondary outcomes are presented in a subsequent paper.
Results
Search results
A total of 3,928 records were identified, with 1,641 remaining after de-duplication, 70 studies were retrieved and examined for full-text screening leaving 36 studies eligible for inclusion (Fig. 1 and Supplementary Table 1). Of these, 31 were included in the meta-analysis for recurrence and 5 were reported narratively. In accordance with Cochrane Handbook guidance [Section 23.3], the study by Tatlican and colleagues [20] was not included in the meta-analysis for the following reasons: 1) groups could not be combined due to the similarity in groups, comparison of the same chemical at different application timepoints, 2) all groups were relevant therefore it was not possible to include only relevant groups, and 3) as all groups were being compared there was no single comparator to spilt the ‘shared’ group into two or more groups. Other reasons for exclusion from the meta-analysis included not assessing the outcome measure [21], heterogeneity in terminology reporting [22,23,24] and three trial arms [20].
PRISMA flow diagram of literature search and study selection phases. n, number; WoS, Web Of Science; CENTRAL, Cochrane Central Register of Controlled Trials; WHO ICTRP, World Health Organisation International Clinical Trials Registry Platform; ISRCTN, International Standard Randomised Controlled Trial Number Registry
In addition, synthesis of evidence for relief of symptoms was reported narratively due to the small number of studies reporting this outcome.
Study characteristics
Characteristics of included studies are summarised in Table 1. Of the 36 RCTs, published between 1979 to 2021, studies were conducted across 14 countries with Turkey being the most frequent (16.6%). Included studies comprised of 3,756 participants, with a sample size ranging from 10 to 125 per study. Five studies [22,23,24,25,26] did not report gender. Of the remaining 31 studies, 62.7% of participants were male.
Interventions
Of the 36 included studies, 5 compared a conservative intervention: orthonyxia [46], nail tube splinting [29], nail elevation and flexible tubing [36], or gutter method [24, 52] to either chemical or surgical matrixectomy. Eleven studies [26, 28, 35, 38, 41, 45, 47, 49, 50, 53, 55] compared chemical matrixectomy to surgical matrixectomy, using various techniques. Two studies [39, 43] compared chemical matrixectomy to avulsion only, and two studies [31, 41] compared chemical matrixectomy to a combination of surgical and chemical matrixectomy.
One study compared a surgical intervention to another surgical intervention [40], two added the use of phenol to a surgical intervention [32, 41]. Three studies compared the same surgical intervention, one adding phenol alongside partial nail avulsion [43], another compared nail avulsion with phenol or trichloroacetic acid [33] and one introduced a new suturing technique alongside a Winograd procedure [54]. One study compared chemical matrixectomy with phenol or trichloroacetic acid [27]. Four studies compared the same surgical intervention and introduced a chemical matrixectomy at different application timings [20, 22, 23, 51].
Five compared an alternative intervention: CO2 laser [42] or electrocautery [25, 34, 44, 48] to either chemical or surgical matrixectomy. There were 2 studies [30, 37] comparing local anaesthetics (4 mL solution of 2% mepivacaine; 2% plain lidocaine, respectively), with or without epinephrine and 2 studies [21, 35] looked at pre- and postoperative use of antibiotics following a surgical intervention.
Recurrence
Recurrence was reported in all but one study [21]. The definition of recurrence varied between studies (Table 2) and two studies were unclear and reported the ‘number of successes/number of failures’ [24] and ‘number symptom-free’ [22, 23], respectively. Therefore, these studies were reported narratively. Follow-up ranged from 1 to 24 months.
Chemical matrixectomy vs conservative management
Two studies [29, 36] found that phenol matrixectomy did not significantly decrease the rate of recurrence when compared to a conservative approach such as nail tube splinting or nail elevation and flexible tubing (RR 0.55 [95% CI 0.19 to 1.61], I2 0%; p = 0.280) (Fig. 2).
Surgical matrixectomy vs conservative management
Two studies [46, 52] compared surgical matrixectomy to a conservative approach, however neither method was significantly more effective at preventing recurrence (RR 0.72 [95% CI 0.33 to 1.56] I2 34%; p = 0.410) (Fig. 2). Conversely, one study [24] that could not be included in this meta-analysis reported the wedge resection (27/32, 84%) to be superior to the gutter treatment (20/36, 56%) in terms of ‘number of successes’ (p < 0.05).
Chemical matrixectomy vs surgical matrixectomy
Combining the eleven studies [26, 28, 35, 38, 41, 45, 47, 49, 50, 53, 55] where chemical matrixectomy was compared to surgical matrixectomy, found no significant difference in their ability to prevent recurrence (RR 0.75 [95% CI 0.46 to 1.21] I2 55%; p = 0.230) (Fig. 3). In addition, funnel plots suggest an absence of publication bias (Supplementary File 2) as these data are symmetrically distributed.
Chemical matrixectomy vs chemical matrixectomy
Two studies [27, 33] compared phenol to trichloroacetic acid, however neither chemical proved to be more effective at preventing recurrence (RR 0.19 [95% CI 0.01 to 3.80] p = 0.280) (Supplementary Fig. 1).
Surgical matrixectomy vs other (e.g., CO2 laser, electrocautery)
In three studies [34, 42, 44], a surgical intervention (partial nail matrixectomy or curettage) did not significantly decrease the rate of recurrence when compared to an alternative method of matrixectomy such as electrocautery or CO2 laser (RR 1.61 [95% CI 0.88 to 2.95] I2 37%; p = 0.120) (Supplementary Fig. 2).
Chemical matrixectomy vs other (e.g., CO2 laser, electrocautery)
Similarly, when comparing chemical matrixectomy to an alternative method of matrixectomy in two studies [25, 48], there was no significant difference in prevention of recurrence (RR 0.58 [95% CI 0.25 to 1.37] I2 0%; p = 0.220) (Supplementary Fig. 3).
Avulsion vs avulsion + chemical matrixectomy
Avulsion with phenol matrixectomy was compared with nail avulsion alone in two studies [39, 43]. There was a significant reduction of recurrence in favour of phenol matrixectomy (RR 0.13 [95% CI 0.06 to 0.27] I2 0%; p < 0.001) (Supplementary Fig. 4). Although Greig and colleagues [39] called their procedure ‘Nail edge excision’ the procedure described was the same as partial avulsion.
Surgical matrixectomy vs surgical matrixectomy
One study [54], compared the Winograd procedure using a new suturing technique, compared to the same surgical intervention and a traditional suturing technique. After 12 months, participants were asked to report any recurrence via telephone. The new suturing technique was more effective at preventing recurrence compared to the traditional technique (RR 0.42 [95% CI 0.21 to 0.85]) (Supplementary Fig. 5).
Another compared central toenail resection to wedge toenail resection [40]. After 6 months, the central toenail resection was considered more effective at preventing recurrence compared with the wedge toenail resection (RR 0.05 [95% CI 0.0 to 0.79]) (Supplementary Fig. 6).
Surgical matrixectomy vs surgical + chemical matrixectomy
Two studies compared a surgical intervention, either nail bed excision or wedge resection, with the same surgical intervention plus the addition of phenol [32, 41]. However, addition of phenol was not significantly more effective at preventing recurrence (RR 3.68 [95% CI 0.20 to 67.35] I2 76%; p = 0.380) (Supplementary Fig. 7).
Chemical matrixectomy vs surgical + chemical matrixectomy
In two studies [31, 41], surgical matrixectomy plus phenolisation did not significantly decrease the rate of recurrence when compared to phenolisation alone (RR 1.92 [95% CI 0.06 to 62.30] I2 62%; p = 0.710) (Supplementary Fig. 8).
Local anaesthetic vs local anaesthetic + adrenaline (epinephrine)
Two studies [30, 37] compared local anaesthetic (4 mL solution of 2% mepivacaine; 2% lidocaine, respectively), with a combination of the same local anaesthetic plus adrenaline (epinephrine). The use of adrenaline did not significantly decrease the rate of recurrence (RR 1.03 [95% CI 0.22 to 4.86] I2 0%; p = 0.970) (Supplementary Fig. 9).
Chemical application time: 30 vs 60 s
Four studies used the same surgical intervention but varied the duration that the chemical was applied during the matrixectomy [20, 22, 23, 51]. Of these, three studies [20, 22, 23] could not be included in the meta-analysis, and none reported significant differences in chemical timing applications. The study by Gem and colleagues [22] compared chemical ablation with either 3 min of 80% phenol or 2 min of 10% sodium hydroxide and the second [23] compared either 1 or 2 min with 10% sodium hydroxide. Of the 422 procedures, 148 were lost to follow up, leaving 248/274 (study 1 n = 140/157; study 2 n = 108/118) who were completely asymptomatic at 18 months. No significant differences were found between the interventions. The numerical data was reproduced faithfully from the publication. There is an arithmetical error, but this has not been corrected due to uncertainty where it occurs. Lastly, Tatlican and colleagues [20] compared phenol with partial nail avulsion at 1, 2 and 3 min on rates of recurrence, assessed every 6 months over 24 months, and found no significant difference between the three groups (p = 0.092).
Of the one study [51] that was included in the meta-analysis, Muriel-Sanchez and colleagues compared the recurrence rate between phenol applications of 30 or 60 s, finding the 60-s application was more effective at preventing recurrence compared to the 30-s phenol application (RR 2.00 [95% CI 0.19 to 21.41]) (Supplementary Fig. 10).
Antibiotics vs no antibiotics
Bos and colleagues explored the use of topical antibiotics (5.3 mg soluble tablet of gentamicin applied locally) on recurrence, with and without matrix excision and phenol [35]. After 12 months the use of topical antibiotics alongside a chemical or surgical matrixectomy did not significantly decrease the rate of recurrence (RR 0.54 [95% CI 0.12 to 2.52] I2 58%; p = 0.430) (Supplementary Fig. 11).
Relief of symptoms
Five studies assessed relief of symptoms [22, 23, 38, 40, 46]. Two studies assessed symptoms using a visual analogue scale ranging from 0 to 10 [38, 46], the remaining three studies did not specify the instrument used [22, 23, 40]. No definitions were provided for relief of symptoms.
Chemical procedures
In two studies [22, 23], no statistically significant differences were identified between patients receiving 3 min application of 80% phenol, 2 min of 10% sodium hydroxide and 1 min of 10% sodium hydroxide. However, Gem and colleagues did report 91% of all participants were asymptomatic after a minimum follow up time of 12 months (study 1) [22] and 18 months (study 2) [23].
Chemical and surgical procedures
Despite a tendency in the matrix group to have fewer persisting symptoms, the study by Gerritsma-Bleeker and colleagues [38] found no significant differences between partial nail extraction with phenolisation and partial nail extraction with matrix excision at 1, 3 or 12 months (p = 0.130, p = 0.270, p = 0.290, respectively).
Surgical procedures
Habeeb and colleagues [40] showed central toenail resection was significantly better in relieving symptoms compared to wedge toenail resection after 4 and 8 weeks (both p = 0.001).
Surgical and conservative procedures
Following receipt of either partial nail extraction with partial matrix excision or orthonyxia, no differences were noted in Kruijff and colleagues [46] study after 12 months.
Ongoing studies
One ongoing clinical trial (CTRI/2017/09/009951) of interest was identified. Registered in 2017, this study remains classified as ‘Not yet recruiting’. Attempts were made to obtain an update on progress from the listed investigators but with no success. Three trial registries of interest were also identified (NCT03732313; IRCT201604176403N6; ACTRN12619001719123), however results were already included in this review [40, 42, 51].
Risk of bias
We used the used the Cochrane RoB 2.0 tool and assessed six domains for each study. No study was rated as low risk, for reasons such as not or providing information surrounding the randomisation process, not including all participants in the final analysis and failing to provide information on blinding of participants or the outcome assessor. Risk of bias summaries are presented in Fig. 4 and risk of bias table in Supplementary Table 2.
Certainty of evidence
The certainty of evidence (Supplementary Table 3) for the outcome recurrence was: very low for meta-analyses comparing surgical vs conservative (2 RCTs, n = 209), chemical vs surgical (11 RCTs, n = 1041), surgical vs other (3 RCTs, n = 388), chemical vs avulsion (2 RCTs, n = 263), surgical vs surgical + chemical (2 RCTs, n = 171), chemical vs other (2 RCTs, n = 160), chemical vs surgical + chemical (2 RCTs, n = 191), epinephrine vs without epinephrine (2 RCTs, n = 114). Low for chemical vs conservative (2 RCTs, n = 173), phenol vs trichloroacetic acid (2 RCTs, n = 187) and surgical vs surgical + suturing (1 RCT, n = 128). Moderate for surgical vs surgical (1 RCT, n = 100), chemical timings (1 RCT, n = 108) and antibiotics (1 RCT, n = 117). The main reasons for downgrading the evidence were risk of bias, indirectness of evidence and imprecision.
Discussion
Ingrown toenails, or onychocryptosis is a common nail pathology. Surgical resolution is often sought when conservative measures fail, or even as a first line intervention in more severe cases. As such, nail surgery is one of the most commonly performed procedures by podiatrists in the UK [11]. Despite the high number of publications on the topic, there has been a lack of robust systematic reviews covering the spectrum of surgical options in the decade since the last Cochrane review [4].
This review followed Cochrane methodology and conducted a prospectively registered systematic review with meta-analysis of surgical treatments for ingrown toenails. This paper includes a detailed description of our methodology and presents findings from our predefined primary outcomes: recurrence and relief of symptoms. Analysis of secondary outcomes will follow in a subsequent publication.
The systematic, search identified 1,641 potential publications which, after screening, enabled 36 studies with 3,756 participants covering a range of techniques that were included in the review. This is a substantial increase on the 24 and 18 studies in the previous Cochrane review [4], and the review by Vinay and colleagues [13], respectively. Recurrence was reported in all but one study, although there were variations in how this was defined and captured. Meta-analysis did not demonstrate a difference in risk of regrowth for most comparisons. Perhaps unsurprisingly, phenolisation was a notable exception to this pattern and when compared to nail avulsion alone, there was a very low certainty of evidence that use of phenol significantly reduced the risk of recurrence [39, 43]. However, use of phenol combined with surgical excision offered no benefit over phenolisation alone [31, 41]. In terms of how long to apply the phenol for, there was a moderate certainty of evidence that application of 1 min had lower risk of regrowth compared to 30 s [51], but there was no additional benefit when it was applied for 2 or 3 min [20]. Studies of peri-operative factors beyond the actual procedure such as use of different local anaesthetic with / without adrenaline [30, 37] and topical antibiotics [35] did not affect rates of regrowth even with such an atypical application technique.
Surprisingly, symptom relief was only reported in five [22, 23, 38, 40, 46] of the 36 studies and in three of those, it was not clear whether this was patient reported, or determined by the clinicians [22, 23, 40]. Even in these studies, exactly what ‘symptoms’ refers to is often unclear. Ingrown toenails are intensely painful though, and that this is rarely captured is a poor reflection on the quality of research in the field: it is no longer acceptable for studies to fail to capture key outcomes that matter to patients, and instead only focus on clinician reported outcomes. The importance of PROMs is well recognised by major national health policy and regulatory authorities [56, 57]. The authors question whether it is acceptable for future trials in ingrown toenails to continue to omit patient reported outcomes. It is important that future clinical trials differentiate between regrowth, which may be asymptomatic, and regrowth which causes pain and infection.
Clinical conclusions from this paper should be interpreted in line with our second paper that considers the secondary outcomes from our review: healing time, postoperative complications, pain of operation, postoperative pain (duration and intensity), and participant satisfaction. Only with these can a broader, more holistic, assessment of outcome be fully appreciated so these are essential for guiding practice.
All 36 studies included in the review were assessed as being either high risk or having some concerns about bias when assessed with the Cochrane RoB 2.0 tool. Similarly, out of the 15 comparisons made here, most were considered to have either very low, or low certainty of evidence when assessed with the GRADE system. Only three reached moderate, and none were considered to have high certainty. The main reasons for downgrading the evidence were risk of bias, indirectness of evidence, and imprecision. In addition, surgical technique was often poorly described, and there was large variation in the use of terms such as recurrence. It is also important that future clinical trials differentiate between regrowth that may be asymptomatic and regrowth that causes pain and infection. To put this another way, 3,756 people have taken part in research studies that do little to guide clinical practice. Some of this may be due to poor reporting, but poor design also plays a major role. Regardless, both of these reasons can, and should be avoided and this topic has been widely discussed in the literature with recommendations made to improve research across healthcare [58,59,60]. Findings from this review differ from those of previous reviews. In part, this may be explained by the publication of new research in the decade since the Cochrane review [4] and a broader focus than the review by Vinay and colleagues specific to phenol [13]. However, the risk of bias assessment was also different as was the grading of strength of recommendations that could be made. Whilst there would inevitably be some variation in these relatively subjective assessment systems the authors stand by this assessment and have discussed some of the methodological limitations in the existing evidence base that have led us to this conclusion. More, high quality clinical trials to inform clinical decision making are urgently needed in nail surgery.
This review and meta-analysis both have strengths and limitations. The authors consider the robust methodology of the search, screening, extracted data, synthesis, meta-analysis, and use of tools such as RoB 2.0 and GRADE as methodological strengths. Deliberate attempts have been made to ensure that comparisons within the meta-analysis are clinically meaningful. Whilst some readers may disagree with how these studies have been compared, or want additional comparisons, they have been made in an open and transparent way. As a further note, this process was made more difficult due to the poor procedure descriptions, with many describing more than one procedure i.e., stated as nail edge excision but partial avulsion was described. Well established reporting guidelines such as the SUPER and IDEAL frameworks should be followed in the future [61, 62].
Conclusion
This paper presents the co-primary outcomes from a systematic review with meta-analysis that should be interpreted in conjunction with its second paper. Despite the high number of publications on this topic, the quality of research was poor and the conclusions that can be inferred from existing trials is limited. Phenolisation of the nail matrix reduces the risk of recurrence following nail ablation, and 1 min appears to be the optimum time for application but there is less certainty around this recommendation. Further research is needed to explore the effectiveness of other commonly used ablative agents such as sodium hydroxide and to systematically explore the optimisation of post-operative care.
Availability of data and materials
All data are available from the corresponding author on reasonable request.
Abbreviations
- CENTRAL:
-
Cochrane Central Register of Controlled Trials
- CI:
-
Confidence Interval
- GRADE:
-
Grades of Research, Assessment, Development and Evaluation
- ISRCTN:
-
International Clinical Trials Registry
- MD:
-
Mean Differences
- MESH:
-
Medical Subject Heading
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROMs:
-
Patient Reported Outcome Measures
- RCT:
-
Randomised Controlled Trial
- ROB:
-
Risk of Bias
- RR:
-
Risk Ratio
References
Bryant A, Knox A. Ingrown toenails: the role of the GP. Aust Fam Physician. 2015;44(3):102–5.
Khunger N, Kandhari R. Ingrown toenails. Indian J Dermatol Venereol Leprol. 2012;78(3):279–89. https://doi.org/10.4103/0378-6323.95442.
Chabchoub I, Litaiem N. Ingrown toenails. Treasure Island: StatPearls; 2022.
Eekhof JA, Van Wijk B, Knuistingh Neven A, van der Wouden JC. Interventions for ingrowing toenails. Cochrane Database Syst Rev. 2012;(4):CD001541. https://doi.org/10.1002/14651858.CD001541.pub3.
Heidelbaugh JJ, Lee H. Management of the ingrown toenail. Am Fam Physician. 2009;79(4):303–8.
Zuber TJ, Pfenninger JL. Management of ingrown toenails. Am Fam Physician. 1995;52(1):181–90.
Heifetz CJ. Ingrown toe-nail: aclinical study. Am J Surg. 1937;38(2):298–315. https://doi.org/10.1016/S0002-9610(37)90439-2.
Park DH, Singh D. The management of ingrowing toenails. BMJ. 2012;344:e2089. https://doi.org/10.1136/bmj.e2089.
Reilly I, Blandford T. An update for UK podiatrists performing toenail surgery on patients who are taking antithrombotic medications: it’s about bleeding time. Preprints. 2021;(2021050559). https://doi.org/10.20944/preprints202105.0559.v1.
Gohil K. Nail surgery guidelines. London: The College of Podiatry; 2019.
Podiatry Co. A demographic evaluation of UK podiatry services. 2016. Accessed 11 Sept 2019.
Reilly I. Toenail surgery: indications, opions and techniques. Dermatol Nurs. 2021;20(2):10–8.
Vinay K, Narayan Ravivarma V, Thakur V, Choudhary R, Narang T, Dogra S, et al. Efficacy and safety of phenol-based partial matricectomy in treatment of onychocryptosis: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2022;36(4):526–35. https://doi.org/10.1111/jdv.17871.
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane handbook for systematic reviews of interventions version 6.3 (Updated February 2022). Cochrane; 2022. Available from www.training.cochrane.org/handbook.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22(4):719–48.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101.
Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. https://doi.org/10.1136/bmj.l4898.
Schunemann H, Brozek J, Guyatt G, Oxman A, editors. GRADE handbook for grading the quality of evidence and the strength of recommendations. Updated 2013. The GRADE Working Group, 2013. Available from https://gdt.gradepro.org/app/handbook/handbook.html. Accessed 9 June 2023.
Tatlican S, Yamangokturk B, Eren C, Eskioglu F, Adiyaman S. Comparison of phenol applications of different durations for the cauterization of the germinal matrix: an efficacy and safety study. Acta Orthop Traumatol Turc. 2009;43(4):298–302.
Reyzelman AM, Trombello KA, Vayser DJ, Armstrong DG, Harkless LB. Are antibiotics necessary in the treatment of locally infected ingrown toenails? Arch Fam Med. 2000;9(9):930–2. https://doi.org/10.1001/archfami.9.9.930.
Gem M, Sykes P. Ingrowing toenails: studies of segmental chemical ablation (study 1). Br J Clin Pract. 1990;44(12):562–3.
Gem M, Sykes P. Ingrowing toenails: studies of segmental chemical ablation (study 2). Br J Clin Pract. 1990;44(12):562–3.
Wallace WA, Milne DD, Andrew T. Gutter treatment for ingrowing toenails. Br Med J. 1979;2(6183):168–71. https://doi.org/10.1136/bmj.2.6183.168.
Hamid T, Qadir MR, Nsar AR, Saleem R, Rehman A, Ali M. Outcome of partial nail avulsion followed by matricectomy either with phenol (80–88%) or with electro cautery for stage 2 & 3 ingrown toenails. Pak J Med Health Sci. 2021;15(8):2043–5.
Varma JS, Kinninmonth AW, Hamer-Hodges DW. Surgical wedge excision versus phenol wedge cauterisation for ingrowing toenail. A controlled study. J R Coll Surg Edinb. 1983;28(5):331–2.
Ahsan M, Irshad A, Asif M, Zafar M, Shah SA. Comparison of trichloroacetic acid and phenol application after partial nail extraction in the treatment of ingrown toe nails. Pak J Med Health Sci. 2019;13(4):982–4.
Akkus A, Demirseren DD, Demirseren ME, Aktas A. The treatment of ingrown nail: chemical matricectomy with NAOH versus wedge resection. Dermatol Ther. 2018;31(5). https://doi.org/10.1111/dth.12677.
AlGhamdi KM, Khurram H. Nail tube splinting method versus lateral nail avulsion with phenol matricectomy: a prospective randomized comparative clinical trial for ingrown toenail treatment. Dermatol Surg. 2014;40(11):1214–20. https://doi.org/10.1097/DSS.0000000000000154.
Altinyazar HC, Demirel CB, Koca R, Hosnuter M. Digital block with and without epinephrine during chemical matricectomy with phenol. Dermatol Surg. 2010;36(10):1568–71.
Álvarez-Jiménez J, Córdoba-Fernández A, Munuera PV. Effect of curettage after segmental phenolization in the treatment of onychocryptosis: a randomized double-blind clinical trial. Dermatol Surg. 2012;38(3):454–61.
Anderson JH, Greig JD, Ireland AJ, Anderson JR. Randomized, prospective study of nail bed ablation for recurrent ingrowing toenails. J R Coll Surg Edinb. 1990;35(4):240–2.
Andre MS, Caucanas M, Andre J, Richert B. Treatment of ingrowing toenails with phenol 88% or trichloroacetic acid 100%: a comparative, prospective, randomized, double-blind study. Dermatol Surg. 2018;44(5):645–50. https://doi.org/10.1097/DSS.0000000000001499.
Awad S, Althobaiti W, Alghamdi S, Alsubaie K, Ghedan S, Shetiwy M. Electrocautery with partial matrixectomy in comparison with partial matrixectomy alone in treatment of ingrown toenail. Egypt J Surg. 2020;39:1095–102.
Bos AM, van Tilburg MW, van Sorge AA, Klinkenbijl JH. Randomized clinical trial of surgical technique and local antibiotics for ingrowing toenail. Br J Surg. 2007;94(3):292–6. https://doi.org/10.1002/bjs.5691.
Ceren E, Gokdemir G, Arikan Y, Purisa S. Comparison of phenol matricectomy and nail-splinting with a flexible tube for the treatment of ingrown toenails. Dermatol Surg. 2013;39(8):1264–9. https://doi.org/10.1111/dsu.12230.
Córdoba-Fernández A, Rodríguez-Delgado F. Anaesthetic digital block with epinephrine vs. tourniquet in ingrown toenail surgery: a clinical trial on efficacy. J Eur Acad Dermatol Venereol. 2015;29(5):985–90.
Gerritsma-Bleeker CL, Klaase JM, Geelkerken RH, Hermans J, van Det RJ. Partial matrix excision or segmental phenolization for ingrowing toenails. Arch Surg. 2002;137(3):320–5. https://doi.org/10.1001/archsurg.137.3.320.
Grieg J, Anderson J, Ireland A, Anderson J. The surgical treatment of ingrowing toenails. J Bone Joint Surg Br. 1991;73(1):131–3.
Habeeb TAAM, Elaidy MM, Mawla WA. Altering toenail biomechanic in managing ingrown toenail. Randomized controlled study. Int J Surg Open. 2020;24:96–9. https://doi.org/10.1016/j.ijso.2020.03.008.
Issa M, Tanner W. Approach to ingrowing toenails: the wedge resection/segmental phenolization combination treatment. J Br Surg. 1988;75(2):181–3.
Kavoussi H, Ebrahimi A, Rezaei M, Salimi E, Rashidian H, Kavoussi R. A comparison of effectiveness and cosmetic outcome of two methods for ingrown toenail: partial nail matricectomy using CO2 laser versus lateral nail fold excision. Acta Dermatovenerol Alp Pannonica Adriat. 2020;29(2):51–4.
Khan IA, Shah SF, Waqar SH, Abdullali MT, Malik Z, Zahid MA. Treatment of ingrown toe nail-comparison of phenolization after partial nail avulsion and partial nail avulsion alone. J Ayub Med Coll Abbottabad. 2014;26(4):522–5.
Kim YJ, Ko JH, Choi KC, Lee CG, Lim KJ. Nail-splinting technique for ingrown nails: the therapeutic effects and the proper removal time of the splint. Dermatol Surg. 2003;29(7):745–8.
Korkmaz M, Colgecen E, Erdogan Y, Bal A, Ozyurt K. Teenage patients with ingrown toenails: treatment with partial matrix excision or segmental phenolization. Indian J Dermatol. 2013;58(4):327. https://doi.org/10.4103/0019-5154.113970.
Kruijff S, van Det RJ, van der Meer GT, van den Berg IC, van der Palen J, Geelkerken RH. Partial matrix excision or orthonyxia for ingrowing toenails. J Am Coll Surg. 2008;206(1):148–53. https://doi.org/10.1016/j.jamcollsurg.2007.06.296.
Leahy AL, Timon CI, Craig A, Stephens RB. Ingrowing toenails: improving treatment. Surgery. 1990;107(5):566–7.
Misiak P, Terlecki A, Rzepkowska-Misiak B, Wcisło S, Brocki M. Comparison of effectiveness of electrocautery and phenol application in partial matricectomy after partial nail extraction in the treatment of ingrown nails. Pol J Surg. 2014;86(2):89–93.
Morkane AJ, Robertson RW, Inglis GS. Segmental phenolization of ingrowing toenails: a randomized controlled study. Br J Surg. 1984;71(7):526–7. https://doi.org/10.1002/bjs.1800710718.
Muriel-Sánchez JM, Becerro-de-Bengoa-Vallejo R, Montaño-Jiménez P, Coheña-Jiménez M. The treatment of ingrown nail: chemical matricectomy with phenol versus aesthetic reconstruction. A single blinded randomized clinical trial. J Clin Med. 2020;9(3). https://doi.org/10.3390/jcm9030845.
Muriel-Sánchez JM, Coheña-Jiménez M, Montaño-Jiménez P. Effect of phenol application time in the treatment of onychocryptosis: a randomized double-blind clinical trial. Int J Environ Res Public Health. 2021;18(19). https://doi.org/10.3390/ijerph181910478.
Peyvandi H, Robati RM, Yegane RA, Hajinasrollah E, Toossi P, Peyvandi AA, et al. Comparison of two surgical methods (Winograd and sleeve method) in the treatment of ingrown toenail. Dermatol Surg. 2011;37(3):331–5. https://doi.org/10.1111/j.1524-4725.2011.01880.x.
Shaath N, Shea J, Whiteman I, Zarugh A. A prospective randomized comparison of the Zadik procedure and chemical ablation in the treatment of ingrown toenails. Foot Ankle Int. 2005;26(5):401–5. https://doi.org/10.1177/107110070502600511.
Uygur E, Çarkçi E, Şenel A, Kemah B, Turhan Y. A new and simple suturing technique applied after surgery to correct ingrown toenails may improve clinical outcomes: a randomized controlled trial. Int J Surg. 2016;34:1–5.
van der Ham AC, Hackeng CA, Yo TI. The treatment of ingrowing toenails. A randomised comparison of wedge excision and phenol cauterisation. J Bone Joint Surg Br. 1990;72(3):507–9. https://doi.org/10.1302/0301-620X.72B3.2341458.
Calvert M, Kyte D, Mercieca-Bebber R, Slade A, Chan A-W, King MT, et al. Guidelines for inclusion of patient-reported outcomes in clinical trial protocols: the SPIRIT-PRO extension. JAMA. 2018;319(5):483–94.
Haywood KL, Wilson R, Staniszewska S, Salek S. Using PROMs in healthcare: who should be in the driving seat—policy makers, health professionals, methodologists or patients? Patients. 2016;9(6):495–8. https://doi.org/10.1007/s40271-016-0197-5.
Pirosca S, Shiely F, Clarke M, Treweek S. Tolerating bad health research: the continuing scandal. Trials. 2022;23:458. https://doi.org/10.1186/s13063-022-06415-5.
Cook JA, Julious SA, Sones W, Hampson LV, Hewitt C, Berlin JA, et al. DELTA2 guidance on choosing the target difference and undertaking and reporting the sample size calculation for a randomised controlled trial. BMJ. 2018;363:k3750. https://doi.org/10.1136/bmj.k3750.
Cook JA, McCulloch P, Blazeby JM, Beard DJ, Marinac-Dabic D, Sedrakyan A. IDEAL framework for surgical innovation 3: randomised controlled trials in the assessment stage and evaluations in the long term study stage. BMJ. 2013;346(jun18 3):f2820. https://doi.org/10.1136/bmj.f2820.
Bilbro NA, Hirst A, Paez A, Vasey B, Pufulete M, Sedrakyan A, et al. The ideal reporting guidelines: a Delphi consensus statement stage specific recommendations for reporting the evaluation of surgical innovation. Ann Surg. 2021;273(1):82–5.
Zhang K, Ma Y, Wu J, Shi Q, Barchi LC, Scarci M, et al. The SUPER reporting guideline suggested for reporting of surgical technique. Hepatobiliary Surg Nutr. 2023. https://doi.org/10.21037/hbsn-22.
Acknowledgements
Not applicable.
Funding
MB is supported by NIHR Research Capability Funding via University Hospitals Coventry and Warwickshire NHS Trust. No specific funding was received for this work.
Author information
Authors and Affiliations
Contributions
MRB, JW and VE conceived the review. KJ and VE screened eligible studies. KJ, VE, GO extracted, summarised data and conducted the quality review. MRB and JW acted as the third reviewer to resolve discrepancies. KJ, VE and MRB wrote the manuscript. KJ is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
MB is a member of the Journal of Foot and Ankle Research Editorial Board.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Figure 1.
Chemical vs Chemical. Forest plot of risk of recurrence for chemical matrixectomy with phenol compared to matrixectomy with trichloroacetic acid.
Additional file 2: Supplementary Figure 2.
Surgical vs Other. Forrest plot of risk of recurrence for surgical matrixectomy compared to matrixectomy by other techniques.
Additional file 3: Supplementary Figure 3.
Chemical vs Other. Forrest plot of risk of recurrence for chemical matrixectomy with pheonol compared to electrocautery.
Additional file 4: Supplementary Figure 4.
Avulsion vs Avulsion + Chemical. Forrest plot of risk of recurrence for avulsion compared to avulsion plus chemical matrixextomy with phenol.
Additional file 5: Supplementary Figure 5.
Surgical vs Surgical. Forrest plot of risk of recurrence for Winograd Procedure involving a new suturing technique compared to Winograd Procedure plus traditional suturing technique.
Additional file 6: Supplementary Figure 6.
Surgical vs Surgical. Forrest plot of risk of recurrence for Central toenail resection compared to Wedge toenail resection.
Additional file 7: Supplementary Figure 7.
Surgical vs Surgical + Chemical. Forrest plot of risk of recurrence for surgical matrixectomy compared to surgical matrixectomy plus chemical ablation.
Additional file 8: Supplementary Figure 8.
Chemical vs Surgical + chemical. Forrest plot of risk of recurrence for chemical matrixectomy compared to surgical procedure plus chemical matrixectomy.
Additional file 9: Supplementary Figure 9.
Anaesthetic vs Anaesthetic + Adrenaline. Forrest plot of risk of recurrence for local anaesthetic compared to local anaesthetic plus adrenaline.
Additional file 10: Supplementary Figure 10.
Chemical timings. Forrest plot of risk of recurrence for 30 second application of phenol compared to 60 second application of phenol.
Additional file 11: Supplementary Figure 11.
Antibiotics vs No Antibiotics. Forrest plot of risk of recurrence for procedure with antibiotic compared to procedure without antibiotic.
Additional file 12: Supplementary File 1.
Full Search Strategy.
Additional file 13: Supplementary File 2.
Funnel Plot: Recurrence.
Additional file 14: Supplementary Table 1.
Table of Excluded Studies.
Additional file 15: Supplementary Table 2.
Risk of Bias Summary Table.
Additional file 16: Supplementary Table 3.
Certainty of evidence using the GRADE approach.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Exley, V., Jones, K., O’Carroll, G. et al. A systematic review and meta-analysis of randomised controlled trials on surgical treatments for ingrown toenails part I: recurrence and relief of symptoms. J Foot Ankle Res 16, 35 (2023). https://doi.org/10.1186/s13047-023-00631-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13047-023-00631-1