Abstract
We compared outcomes of adult patients with secondary acute myeloid leukemia (sAML) versus de novo AML after non-T-depleted haploidentical stem cell transplant (HaploSCT) with post-transplant cyclophosphamide (PTCy). Seventeen hundred and eleven AML patients (sAML-231, de novo-1480) in first complete remission transplanted from 2010 to 2021, were included. Patients with de novo AML were younger, median age 55.8 versus 60.8 years, p < 0.0001, had better transplantation comorbidity index (HCT-CI) ≥ 3 21.3% versus 40.8%, p < 0.0001 and Karnofsky performance status (KPS) with KPS ≥ 90 in 78% versus 68.5%, respectively, p = 0.002. The two patient groups did not differ with respect to gender, cytomegalovirus serostatus, and cell source. Median time from diagnosis to HaploSCT was 5.2 versus 4.9 months, respectively, p = 0.005. Fewer sAML patients received myeloablative conditioning 35.1% versus 50.1%, p < 0.0001. Two hundred and eleven sAML and 410 de novo AML patients were included in the matched-pair analysis matching two de novo AML with each sAML. No significant difference was observed in any transplantation outcome parameter between the sAML versus de novo AML groups. Two-year non-relapse mortality and relapse incidence did not differ with HaploSCT for de novo versus sAML; 21.4% versus 21%, hazard ratio (HR) = 0.98, p = 0.9 and 23.4% versus 20.6%, HR = 0.92, p = 0.67, respectively. Two-year leukemia-free survival, overall survival, and graft-versus-host disease (GVHD)-free, relapse-free survival were also not different between the de novo AML and sAML groups 55.2% versus 58.4%, HR = 0.95, p = 0.67; 61.4% versus 66.4%, HR = 0.91, p = 0.51 and 46.3% versus 48.2%, HR = 0.92, p = 0.48, respectively. Similarly, the incidence of engraftment as well as acute and chronic GVHD was similar between the 2 cohorts. In conclusion, HaploSCT with PTCy may be able to overcome the bad prognosis of sAML as results are not significantly different to those of HaploSCT in de novo AML.
Similar content being viewed by others
Introduction
Secondary acute myeloid leukemia (sAML) is a distinct type of acute myeloid leukemia (AML) evolving from an antecedent hematological disorder or as a complication of prior cytotoxic chemotherapy or radiation therapy [1, 2]. Patients with sAML have inferior outcomes compared to de novo AML, mainly due to a higher frequency of adverse molecular mutations and high-risk cytogenetic abnormalities in addition to typically being older and having an antecedent hematological disease [3,4,5,6,7]. Allogeneic hematopoietic cell transplantation (HSCT) represents a potentially curative therapy in this setting, rescuing up to 40% of the patients [8,9,10,11,12]. Despite some improvement in matched sibling and unrelated transplantation for sAML in the last few decades, as we have recently demonstrated on behalf of the Acute Leukemia Working Party (ALWP) of the European Society for Blood and Marrow Transplantation (EBMT) with a study of sAML patients comparing 1337 that were transplanted in 2000 to 2010 with 2887 transplanted in 2011 to 2020. We demonstrated a significant reduction in 2-year non-relapse mortality (NRM) and a significant improvement in the 2-year graft-versus-host disease (GVHD)-free, relapse-free survival (GRFS) but the 2-year leukemia-free (LFS) and overall survival (OS) were similar [13] with somewhat better results with myeloablative (MAC) versus reduced intensity conditioning (RIC) [9, 14]. These results are better than those reported in 2010 by the Center for International Blood and Marrow Transplant Research (CIBMTR) in 868 patients with therapy-related AML or myelodysplastic syndrome (MDS) transplanted between 1990 and 2004 mainly from matched sibling donors (MSD) or matched unrelated donors (MUD) and MAC with 5-year disease-free survival (DFS) and OS of 21% and 22%, respectively, with the caveat that the CIBMTR study included also patients in second CR and more advance disease [8], or our previous results evaluating transplantation outcome in close to 5000 patients with sAML transplanted between 2000 and 2016 mainly from MSD and MUD, where we observed 2-year OS, LFS and GRFS of 44.5%, 38.8% and 27.2%, respectively [9]. Notably, transplantation outcomes with MSD and MUD in sAML are significantly inferior to those typically achieved in de novo AML with a lower OS, LFS, and GRFS due to higher NRM and relapse incidence (RI) [10]. However, the picture may differ with non-T depleted haploidentical stem cell transplantation (HaploSCT) with post-transplant cyclophosphamide (PTCy) which has been increasingly used for AML and proven to be highly effective in preventing GVHD and reducing NRM thus improving transplantation results [15, 16]. HaploSCT for sAML has been performed in recent years [15, 16] with a 2-year LFS of 49% and OS of 57% in patients transplanted in complete response (CR) from 2006 to 2016 [15]. Furthermore, some reports indicate a stronger graft-versus-leukemia (GVL) effect with Haplo grafts due to the broad human leukocyte antigen (HLA) disparity [19, 20] which may be of special importance in sAML being a high-risk leukemia category carrying a high post-transplantation RI [8]. Indeed, relapse is the most frequent cause of transplant failure in sAML with a poor prognosis, a median OS of about 8 months, and limited therapeutic options [8,9,10, 21, 22]. It is conceivable therefore that the results of HaploSCT in sAML will not differ from those in de novo AML. Such a comparison has not yet been performed. Therefore, the goal of the current study was to compare the outcomes of HaploSCT in patients with sAML with those of HaploSCT in de novo AML.
Patients and methods
Study design and data collection
This was a retrospective, multicenter analysis using the dataset of the ALWP of the EBMT. The EBMT is a voluntary working group of more than 600 transplant centers that are required to report all consecutive stem cell transplantations and follow-ups once a year. EBMT minimum essential data forms are submitted to the registry by transplant center personnel following written informed consent from patients in accordance with the centers’ ethical research guidelines. Data accuracy is assured by the individual transplant centers and by quality control measures such as regular internal and external audits. In addition, the study protocol was approved by each site and complied with country-specific regulatory requirements. The results of disease assessments at HSCT were also submitted and form the basis of this report. Eligibility criteria for this analysis included adult patients ≥ 18 years of age with de novo or sAML in CR1 who underwent the first HSCT from a non-T-cell depleted Haplo donor with PTCy as part of GVHD prophylaxis between 2010 and 2021. A Haplo donor was defined as ≥ 2 HLA mismatches between donor and recipient. The exclusion criteria were HSCT from other donor types (sibling, unrelated, or cord blood donor); previous history of HSCT, T cell-depleted hematopoietic cell graft, unknown or favorable cytogenetic risk and unknown antecedent hematological disorder. Data collected included recipient and donor characteristics (age, gender, cytomegalovirus (CMV) serostatus, Karnofsky performance status (KPS) and hematopoietic cell transplantation specific comorbidity index (HCT-CI), disease characteristics, antecedent hematological disorder, year of transplant, type of conditioning regimen, stem cell source, and GVHD prophylaxis regimen. The conditioning regimen was defined as MAC when containing total body irradiation (TBI) with a dose > 6 Gray or a total dose of busulfan (Bu) > 8 mg/kg or > 6.4 mg/kg when administered orally or intravenously, respectively. All other regimens were defined as RIC [23]. Grading of aGVHD was performed using established criteria [24]. Chronic (c) GVHD was classified as limited or extensive according to published criteria [25]. For this study, all necessary data were collected according to the EBMT guidelines, using the EBMT minimum essential data forms. The list of institutions contributing data to this study is provided in the Additional file 1: Appendix.
Statistical analysis
The median, interquartile range (IQR), and range were used for quantitative variables, and frequency and percentage for categorical variables. The study endpoints were OS, LFS, RI, NRM, engraftment, aGVHD, cGVHD, and GRFS. All endpoints were measured from the time of transplantation. Engraftment was defined as achieving an absolute neutrophil count of 0.5 × 109/L for three consecutive days. OS was defined as time to death from any cause. LFS was defined as survival with no evidence of relapse or progression. NRM was defined as death from any cause without previous relapse or progression. We used modified GRFS criteria. GRFS events were defined as the first event among grade III-IV aGVHD, extensive cGVHD, relapse, or death from any other cause [26]. Patient, disease, and transplant-related characteristics for the two cohorts (de novo and secondary AML) were compared using the Mann–Whitney U test for numerical variables, and the chi-squared or Fisher’s exact test for categorical variables. The probabilities of OS, LFS, and GRFS were calculated using the Kaplan–Meier estimate. The RI and NRM were calculated using cumulative incidence (CI) functions in a competing risk setting, with death in remission being treated as a competing event for relapse. Early death was considered as a competing event for engraftment. To estimate the CI of acute or cGVHD, relapse and death were considered as competing events. Univariate analyses were performed using the log-rank test for LFS and OS while Gray’s test was used for CI. Multivariate analyses were performed using the Cox proportional-hazards regression model [27]. All variables differing significantly between the two groups, and potential risk factors were included in the model. In order to take into account, the heterogeneity in the effect of a characteristic or a treatment across centers, we introduce a random effect (also named frailty effect) in Cox multivariate models. Then, the same random effect is shared by all patients within the same center [28].
For each patient with secondary AML, two separate matched controls with de novo AML were identified using exact and propensity-score matched criteria. Exact matching was used for cytogenetics risk group, conditioning intensity, source of stem cells and sex matching (female to male vs all others), and nearest neighbor for recipient age, and Karnofsky score (90–100 vs < 90) [29]. HCT-CI was not included in the propensity score because of the high number of missing values.
Comparisons were performed using a Cox model and cluster-robust standard errors were used to account for dependence between observations within matched pairs. Results were expressed as the hazard ratio (HR) with a 95% confidence interval (95% CI). All p values were two-sided with a type 1 error rate fixed at 0.05. Statistical analyses were performed with SPSS 25.0 (SPSS Inc., Chicago, IL, USA) and R 4.0.2 (R Core Team Fifty (2020). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/) [30].
Results
Patient, transplant, and disease characteristics
A total of 1711 patients met the inclusion criteria, 231 with sAML and 1480 with de novo AML. Table 1 shows the baseline demographic and clinical characteristics. Median follow-up was 24.6 (IQR 19.6–31.2) and 26.3 (IQR 24.5–28.8) months for patients with sAML and de novo AML, respectively (p = 0.52). Patients with de novo AML were younger, with a median age of 55.8 (range 18.1–82.5) versus 60.8 (20.8–75.7) years, (p < 0.0001). The median year of transplant was 2019 in both groups and 57.5% and 61.9% of the patients with de novo and sAML, were male (p = 0.21), respectively.
In 64% of sAML patients, the antecedent hematological disorder was myelodysplastic syndrome/myeloproliferative neoplasm (MDS/MPN), while in 16.7% it was another hematological disorder, followed by solid tumor in 17% and nonmalignant hematological disorder in 2.3%. Cytogenetic risk was categorized as intermediate (70.1% vs 67.1%) or adverse (29.9% vs 32.9%) for patients with de novo AML and sAML, respectively (p = 0.36). Karnofsky performance status (KPS) was higher in the de novo AML group in comparison with the sAML group, with KPS ≥ 90 in 78% versus 68.5%, respectively (p = 0.002). HCT-CI was higher in the sAML group in comparison with the de novo AML group, with HCT-CI ≥ 3 in 40.8% versus 21.3%, respectively (p < 0.0001) (data were missing for 167 and 701 of the patients, respectively). There was no difference in the frequency of CMV seropositivity between the two patient groups (78.7% and 76.2%), or between the donor types (62.7% and 56.2%), respectively. Female donors to male patients were used in 23.4% and 20.2% of the cases with sAML and de novo AML, respectively (p = 0.26). Time from diagnosis to HaploSCT was longer in patients with de novo AML versus those with sAML; median 5.2 (range 1–23.9) versus 4.9 (range 1.3–20.5) months, respectively (p = 0.005). Fewer sAML patients received MAC compared to de novo AML patients, 35.1% versus 50.1%, respectively (p < 0.001). The most frequent conditioning regimen for both groups was thiotepa/busulfan/fludarabine at 50.2% and 45.9%, followed by busulfan/fludarabine in 17.6% and 16.5%, and fludarabine/low dose TBI in 16.2% and 19.9% of patients with de novo and sAML, respectively (Additional file 1: Table S1). Graft source was mainly peripheral blood stem cells in both de novo (70.7%) and sAML (78.4%) groups. In 53.9% and 53.7% of the de novo and AML patients, respectively, PTCY was combined with cyclosporine A (CSA) and mycophenolate mofetil (MMF), while in 30% and 27.7% it was combined with MMF and tacrolimus (Tacro), respectively (Additional file 1: Table S2).
Transplantation outcome
Engraftment and GVHD incidence did not differ between the sAML versus de novo AML groups as depicted in Table 2. Neutrophil recovery (ANC > 0.5 × 109/L) was achieved in 95.1% and 94.4% of the patients with de novo and sAML, respectively (p = 0.69). On day + 180, the incidence of aGVHD grades II-IV and III-IV was 27.2% (24.9–29.6%) versus 29.1% (23.1–35.3%) (p = 0.55) and 9.2% (7.7–10.8%) versus 6.6% (3.8–10.4%), respectively (p = 0.23). Two-year incidence of total and extensive cGVHD was 32.2% (29.5–34.9%) versus 33.3% (26.5–40.3%) (p = 1) and 11.9% (10.1–13.9%) versus 11.3% (7.1–16.6%), respectively (p = 0.48). Similarly, two-year NRM and RI as well as LFS, OS, and GRFS did not differ between the sAML versus de novo AML groups. Two-year NRM and RI were 21.1% (18.29–23.4%) versus 20.8% (15.4–26.7%) (p = 0.72) and 19.5% (17.2–21.8%) versus 21.3% (15.6–27.5%) (p = 0.39) in de novo versus sAML, respectively (Table 3A). The 2-year LFS, OS, and GRFS were 59.5% (56.6–62.2%) versus 58% (50.5–64.7%) (p = 0.28), 65.4% (62.5–68%) versus 66.7% (58.3–72.1%) (p = 0.35) and 49.9% (47–52.7%) versus 47% (39.5–54.1%) (p = 0.5), respectively (Table 3A). Also no difference was observed in any transplantation outcome parameter between sAML post MDS/MPN/ bone marrow failure syndrome (BMFS) versus de novo AML and sAML post other malignant hematological disorders (OMHD) /solid tumor (ST) versus de novo AML (Table 3B).
Multivariate analysis
In multivariate analysis (Table 4A), no difference was observed in any transplantation outcome parameter between the sAML versus de novo AML groups; The HR for NRM was 0.87 (95% CI 0.7–1.35, p = 0.87), RI HR = 1.02(95% CI 0.72–1.45, p = 0.9), LFS HR = 1, (95% CI 0.79–1.27, p = 0.99), OS HR = 0.95 (95% CI 0.74–1.23, p = 0.72) and GRFS HR = 0.94 (95% CI 0.75–1.17, p = 0.57) (Table 4). Similarly, the incidence of a GVHD II-IV HR = 1.04 (95% CI 0.77–1.41, p = 0.8), aGVHD III-IV HR = 0.73 (95% CI 0.41–1.32, p = 0.3), cGVHD all grades HR = 0.96 (95% CI 0.71–1.29, p = 0.78) and extensive cGVHD HR = 0.65 (95% CI 0.39–1.08, p = 0.097) did not differ between the two groups (Table 4A). Also no difference was observed in any transplantation outcome parameter between sAML post MDS/MPN/BMFS versus de novo AML and sAML post OMHD/ST versus de novo AML (Table 4B). Other significant prognostic factors were adverse cytogenetics risk predicting higher RI and lower LFS, OS, and GRFS; age (per 10 years) predicted higher NRM and inferior LFS, OS, and GRFS. KPS > 90 was a prognostic factor for lower NRM and higher LFS, OS, and GRFS. RIC was associated with higher RI and worse LFS and OS. Female donor to male patient combination was associated was lower LFS, OS, GRFS and higher extensive cGVHD. A peripheral blood graft was a predictive factor for a higher incidence of grade II–IV and III–IV aGVHD as well as total cGVHD (Table 4).
Cause of death
A total of 485 (32.8%) patients with de novo AML and 79 (34.2%) with sAML died during the study period (Table 5). The original disease was the main cause of death accounting for 36.3% and 42.1% of the deaths, respectively. The second cause of death was infection at 30.5% and 26.3%, followed by GVHD with 14.6% and 9.2% of deaths, in patients with de novo and sAML, respectively (Table 5). Multi-organ failure accounted for 2.4% and 3.9% of the deaths, respectively. Other causes of death were infrequent and included veno-occlusive disease of the liver, cardiac toxicity, hemorrhage, graft failure, and central nervous system toxicity, each accounting for less than 2% of total deaths with no difference between the patient groups (Table 5).
Matched-pair analysis
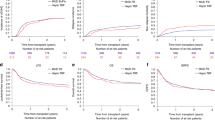
To minimize the effect of confounding factors, a matched-pair analysis (2:1 ratio) was performed. Using the criteria mentioned above, 621 well-matched pairs (de novo AML = 410; sAML = 211 were identified (Additional file 1: Tables S3–S7). In 141 of the sAML patients the antecedent hematological disorder was MDS or MPN or bone marrow failure syndrome (BMFS) while in 70 patients the antecedent disease was other malignant haematological disorder (OMHD) [10] or solid tumor (ST), respectively. The results of the matched-pair analysis were consistent with previous results for the entire population. Engraftment was 93.4% versus 94.9% in de novo and sAML, respectively (p = 0.47) (Additional file 1: Table S4). Incidence of both acute and cGVHD was similar between the 2 cohorts: aGVHD Grade II-IV 27.6% (23.2–32.1) versus 27.7% (21.6–34.1), HR = 0.99 (95% CI 0.72–1.38, p = 0.96), aGVHD Grade III-IV 9.5% (6.9–12.7) versus 6.7% (3.7–10.8), HR = 0.7 (95% CI 0.36–1.35, p = 0.29), total cGVHD 31.8% (26.7–37%) versus 32.8% (25.7–40.1%), HR = 1.03 (95% CI 0.75–1.42, p = 0.84) and extensive cGVHD 10.2% (7.2–13.8%) versus 10.6% (6.4–16.1%), HR = 0.93 (95% CI 0.53–1.61, p = 0.79), respectively (Table 6A). Two-year NRM and RI did not differ with HaploSCT for de novo versus sAML; 23.4% (19–28.1) versus 20.6% (15.1–26.8%), HR = 0.92(95% CI 0.64–1.33, p = 0.67) and 21.4% (17–26.1%) versus 21% (15.1–27.5%), HR = 0.98 (95% CI 0.672–1.42, p = 0.9), respectively (Table 6A). There was also no difference in LFS, OS, and GRFS between the de novo AML and sAML groups 55.2% (49.5–60.5%) versus 58.4% (50.6–65.4%), HR = 0.95 (95% CI 0.74–1.22, p = 0.67); 61.4% (55.7–66.5%) versus 66.4% (58.8–73%), HR = 0.91 (95% CI 0.69–1.2, p = 0.51) and 46.3% (40.7–51.6%) versus 48.2% (40.4–55.6%), HR = 0.92 (95% CI 0.73–1.16, p = 0.48), respectively (Table 6A, Fig. 1). No difference was observed in any transplantation outcome parameter between sAML post MDS/MPN/BMFS versus de novo AML and sAML post OMHD/ST versus de novo AML (Table 6B, Fig. 2). Finally, we also verified that the results are consistent when adjusting the comparison on HCT-CI (data not shown). Causes of death are listed in Additional file 1: Table S7.
Matched-pair analysis of haploidentical transplantation outcomes in secondary AML per antecedent hematological disorder versus de novo AML: non-relapse mortality (NRM), relapse incidence (RI), leukemia-free survival (LFS), overall survival (OS), and GVHD-free, relapse-free survival (GRFS). sAML post myelodysplastic syndrome (MDS), myeloproliferative neoplasm (MPN), bone marrow failure syndrome (BMF) (MDS /MPN) (n-141); sAML post other malignant hematologic disorders(OMDS), solid tumors (ST) (OMDS/ST) (n-70)
Discussion
In this study, we have demonstrated similar transplantation outcomes for patients with sAML in comparison to those with de novo AML following non-T depleted HaploSCT and PTCy. Furthermore, no difference was observed in transplantation outcomes irrespectively of the antecedent hematological disorder. Impressively, about two thirds of the sAML patients were rescued and half of them were relapse-free and GVHD free at 2 years. These results are similar and even slightly better than the results we previously published on behalf of the ALWP of the EBMT analyzing transplantation outcomes in 154 sAML patients undergoing non-T depleted HaploSCT between 2006 to 2016, 119 of them with PTCy, and a 2-year LFS, OS, and GRFS of 37.1%, 43.3% and 42.1%, respectively [17]. In a subsequent study that included 246 HaploSCT performed in a similar period, 2-year LFS, OS, and GRFS were 32%, 41%, and 23%, respectively [18]. Schmaelter et al. from the ALWP of the EBMT compared transplantation results in 11,439 patients with de novo and 1325 with sAML (8600 of whom were in CR1) transplanted mostly from sibling and unrelated donors and observed a higher RI and also higher NRM in sAML versus de novo AML, which translated to significantly inferior LFS, OS, and GRFS in the sAML patients with HRs of 1.33, 1.32 and 1.2, respectively [10]. Historically, conventional therapeutic results in sAML are inferior to those in de novo AML due to multiple reasons including more aggressive disease biology, more unfavorable cytogenetics and mutation rates, the antecedent malignancy, and previous therapies upregulating multidrug resistance genes, and thus a poor response to chemotherapy as well as patient-related factors such as older age, and comorbidities leading to reduced tolerability to chemotherapy with increased toxicity and side effects [3,4,5,6,7, 21, 31,32,33]. These poor prognostic factors are also operating in the setting of transplantation resulting in both higher relapse rates as well as higher NRM which translate to inferior outcomes including LFS and OS, and GRFS in patients with sAML in comparison to those with de novo AML [8,9,10,11,12, 14, 34]. However, the scenario with non-T depleted HaploSCT especially with PTCy may differ due to the unique biology of the PTCy platform leading to a remarkable reduction in transplant-related mortality and GVHD, translating into improved results [15, 16, 35,36,37]. Furthermore, the Haplo procedure may be associated with enhanced anti-leukemic efficacy as was recently nicely proved by Professor Huang Xia June in a mice model which carried the human AML-ETO or MLL-AF9 fusion gene showing that cytotoxic T lymphocytes from the haploSCT group had higher cytotoxicity than those from the MSD group [38]. Although controversial, the GVL effect may be stronger with non-T cell-depleted Haplo donors with faster clearance of post-transplant measurable residual disease, reduced post-transplant disease progression, and relapse, and better results in positive MRD pre-transplantation high-risk leukemia as compared to sibling transplantation [19, 20, 38,39,40,41,42]. Furthermore, it is conceivable that the GVL effect is not the only mechanism that protects from disease relapse when using PTCy. The PTCy strategy may provide a direct immune-mediated specific anti-leukemic effect, distinct from GVHD, that is probably mediated by the release of cytokines or other molecules to which leukemic cells may be more sensitive than normal cells [43]. Altogether the reduced toxicity and potentially stronger anti-leukemic effect may be of special importance in patients with sAML and may explain the lack of difference we observed with the Haplo transplants in patients with sAML versus those with de novo AML. Furthermore, our data were analyzed using a propensity score analysis in order to balance the characteristics of the two populations. The matched-pair analysis confirmed the results that we found in the standard analysis indicating similar main outcomes post-HaploSCT in sAML and de novo AML. Our data are somewhat similar and in agreement with a recent report by our Chinese colleagues that demonstrated that the prognosis of haploSCT in patients with AML with myelodysplasia related changes (AML-MRC) in first CR is similar to that of other types of high-risk AML patients and that HaploSCT is an ideal choice for patients with AML-MRC in CR [44].
As previously reported for de novo AML and MDS, we observed a lower relapse rate with MAC as compared to RIC in agreement with a previous publication where we demonstrated lower RI and better LFS and OS by including patients with sAML post-MDS and patients with AML undergoing second transplants [14, 45, 46].
The other factors observed to be associated with HaploSCT outcomes included cytogenetic risk, age, KPS, and female donor-to-male patient combination and are in agreement with previous publications of allogeneic transplantations including HaploSCTs in de novo AML [9,10,11, 22, 45,46,47,48,49].
This study, being a retrospective and registry-based transplantation study, has several limitations including the risk of selection bias and the possibility of unavailable data that could not have been considered, such as frontline therapies as well as molecular, MRD, and CD34 cell dose data. Also, we included in our analysis only patients in CR1 that are thus with favorable outcomes, and results in more advanced stages of sAML may differ, especially as sAML is typically associated with lower and shorter CRs compared to de novo AML.
In conclusion, in this relatively large registry-based retrospective analysis of HaploSCT for sAML in comparison to HaploSCT in de novo AML, we observed similar transplantation outcomes with HaploSCT being about two-thirds of the patients with this devastating leukemia. Hopefully, the recently approved novel agents (mainly vyxeos [CPX-351]) that have been shown to enable more sAML patients to undergo HLA-matched allogeneic transplantation and hopefully also HaploSCTs, it may be possible to further improve sAML outcomes [50].
Availability of data materials
A.N., M.N., M.L., and M.M. had full access to all study data (available upon data-specific request).
Change history
29 September 2023
A Correction to this paper has been published: https://doi.org/10.1186/s13045-023-01501-w
References
Granfeldt Ostgard LS, Medeiros BC, Sengelov H, Norgaard M, Andersen MK, Dufva IH, et al. Epidemiology and Clinical Significance of Secondary and Therapy-Related Acute MSecondary AML is generally associated with poor clinical outcomes compared to de novo AMLyeloid Leukemia: a National Population-Based Cohort Study. J Clin Oncol. 2015;33(31):3641–9.
Hulegårdh E, Nilsson C, Lazarevic V, Garelius H, Antunovic P, Rangert Derolf Å, et al. Characterization and prognostic features of secondary acute myeloid leukemia in a population-based setting: a report from the Swedish Acute Leukemia Registry. Am J Hematol. 2015;90(3):208–14.
Della Porta MG. Prognosis of secondary acute myeloid leukemia. Leuk Res. 2013;37(8):857–8.
Kayser S, Döhner K, Krauter J, Köhne C-H, Horst HA, Held G, et al. The impact of therapy-related acute myeloid leukemia (AML) on outcome in 2853 adult patients with newly diagnosed AML. Blood. 2011;117(7):2137–45.
Zeichner SB, Arellano ML. Secondary adult acute myeloid leukemia: a review of our evolving understanding of a complex disease process. Curr Treat Options Oncol. 2015;16(8):37.
Richardson DR, Green SD, Foster MC, Zeidner JF. Secondary AML emerging after therapy with hypomethylating agents: outcomes, prognostic factors, and treatment options. Curr Hematol Malig Rep. 2021;16(1):97–111.
Bauer M, Vaxevanis C, Heimer N, Al-Ali HK, Jaekel N, Bachmann M, et al. Expression, regulation and function of microRNA as important players in the transition of MDS to secondary AML and their cross talk to RNA-binding proteins. Int J Mol Sci. 2020;21(19):7140.
Litzow MR, Tarima S, Perez WS, Bolwell BJ, Cairo MS, Camitta BM, et al. Allogeneic transplantation for therapy-related myelodysplastic syndrome and acute myeloid leukemia. Blood. 2010;115(9):1850–7.
Sengsayadeth S, Labopin M, Boumendil A, Finke J, Ganser A, Stelljes M, et al. Transplant outcomes for secondary acute myeloid leukemia: acute leukemia working party of the european society for blood and bone marrow transplantation study. Biol Blood Marrow Transplant. 2018;24(7):1406–14.
Schmaelter A-K, Labopin M, Socié G, Itälä-Remes M, Blaise D, Yakoub-Agha I, et al. Inferior outcome of allogeneic stem cell transplantation for secondary acute myeloid leukemia in first complete remission as compared to de novo acute myeloid leukemia. Blood Cancer J. 2020;10(3):26.
Kida M, Usuki K, Uchida N, Fukuda T, Katayama Y, Kondo T, et al. Outcome and risk factors for therapy-related myeloid neoplasms treated with allogeneic stem cell transplantation in Japan. Biol Blood Marrow Transplant. 2020;26(8):1543–51.
Nilsson C, Hulegårdh E, Garelius H, Möllgård L, Brune M, Wahlin A, et al. Secondary acute myeloid leukemia and the role of allogeneic stem cell transplantation in a population-based setting. Biol Blood Marrow Transplant. 2019;25(9):1770–8.
Nagler A, Ngoya M, Galimard JE, Labopin M, Kröger N, Socié G, et al. Trends in outcome of transplantation in patients with secondary acute myeloid leukemia: an analysis from the Acute Leukemia Working Party (ALWP) of the EBMT. Bone Marrow Transplant. 2022. https://doi.org/10.1038/s41409-022-01825-0.
Nagler A, Peczynski C, Dholaria B, Labopin M, Valerius T, Dreger P, et al. Impact of conditioning regimen intensity on outcomes of second allogeneic hematopoietic cell transplantation for secondary acute myelogenous leukemia. Bone Marrow Transplant. 2022;57(7):1116–23.
McCurdy SR, Kanakry JA, Showel MM, Tsai HL, Bolaños-Meade J, Rosner GL, et al. Risk-stratified outcomes of nonmyeloablative HLA-haploidentical BMT with high-dose posttransplantation cyclophosphamide. Blood. 2015;125(19):3024–31.
Kasamon YL, Bolaños-Meade J, Prince GT, Tsai HL, McCurdy SR, Kanakry JA, et al. Outcomes of nonmyeloablative HLA-haploidentical blood or marrow transplantation with high-dose post-transplantation cyclophosphamide in older adults. J Clin Oncol. 2015;33(28):3152–61.
Li Z, Labopin M, Ciceri F, Blaise D, Tischer J, Ehninger G, et al. Haploidentical transplantation outcomes for secondary acute myeloid leukemia: acute Leukemia Working Party (ALWP) of the European Society for Blood and Marrow Transplantation (EBMT) study. Am J Hematol. 2018;93(6):769–77.
Ruggeri A, Labopin M, Savani B, Paviglianiti A, Blaise D, Volt F, et al. Hematopoietic stem cell transplantation with unrelated cord blood or haploidentical donor grafts in adult patients with secondary acute myeloid leukemia, a comparative study from Eurocord and the ALWP EBMT. Bone Marrow Transplant. 2019;54(12):1987–94.
Yu S, Huang F, Wang Y, Xu Y, Yang T, Fan Z, et al. Haploidentical transplantation might have superior graft-versus-leukemia effect than HLA-matched sibling transplantation for high-risk acute myeloid leukemia in first complete remission: a prospective multicentre cohort study. Leukemia. 2020;34(5):1433–43.
Wang Y, Liu DH, Xu LP, Liu KU, Chen H, Chen YH, et al. Superior graft-versus-leukemia effect associated with transplantation of haploidentical compared with HLA-identical sibling donor grafts for high-risk acute leukemia: an historic comparison. Biol Blood Marrow Transplant. 2011;17(6):821–30.
Yoshizato T, Nannya Y, Atsuta Y, Shiozawa Y, Iijima-Yamashita Y, Yoshida K, et al. Genetic abnormalities in myelodysplasia and secondary acute myeloid leukemia: impact on outcome of stem cell transplantation. Blood. 2017;129(17):2347–58.
Bazarbachi A, Schmid C, Labopin M, Beelen D, Wolfgang Blau I, Potter V, et al. Evaluation of trends and prognosis over time in patients with AML relapsing after allogeneic hematopoietic cell transplant reveals improved survival for young patients in recent years. Clin Cancer Res. 2020;26(24):6475–82.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant. 2009;15(12):1628–33.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 Consensus conference on acute GVHD grading. Bone Marrow Transplant. 1995;15(6):825–8.
Shulman HM, Sullivan KM, Weiden PL, McDonald GB, Striker GE, Sale GE, et al. Chronic graft-versus-host syndrome in man. A long-term clinicopathologic study of 20 Seattle patients. Am J Med. 1980;69(2):204–17.
Ruggeri A, Labopin M, Ciceri F, Mohty M, Nagler A. Definition of GvHD-free, relapse-free survival for registry-based studies: an ALWP-EBMT analysis on patients with AML in remission. Bone Marrow Transplant. 2016;51:610–1.
Kanate AS, Nagler A, Savani B. Summary of scientific and statistical methods, study endpoints and definitions for observational and registry-based studies in hematopoietic cell transplantation. Clin Hematol Int. 2019;2(1):2–4.
Andersen PK, Klein JP, Zhang MJ. Testing for center effects in multi-center survival studies: a Monte Carlo comparison of fixed and random effects tests. Stat Med. 1999;18:1489–500.
McCaffrey DF, Griffin BA, Almirall D, Slaughter ME, Ramchand R, Burgette LF. A tutorial on propensity score estimation for multiple treatments using generalized boosted models. Stat Med. 2013;32(19):3388–414.
A language and environment for statistical computing. https://www.R-project.org/. R Core Team: R Foundation for Statistical Computing, Vienna, Austria, 2020.
Boddu PC, Kantarjian HM, Ravandi F, Garcia-Manero G, Verstovsek S, Jabbour EJ, et al. Characteristics and outcomes of older patients with secondary acute myeloid leukemia according to treatment approach. Cancer. 2017;123:3050–60.
Park SH, Chi H-S, Cho Y-U, Jang S, Park C-J. Evaluation of prognostic factors in patients with therapy-related acute myeloid leukemia. Blood Res. 2013;48:185.
Christiansen DH, Andersen MK, Pedersen-Bjergaard J. Mutations with loss of heterozygosity of p53 are common in therapy-related myelodysplasia and acute myeloid leukemia after exposure to alkylating agents and significantly associated with deletion or loss of 5q, a complex karyotype, and a poor prognosis. J Clin Oncol. 2001;19:1405–13.
Schmid C, De Wreede LC, Van Biezen A, Finke J, Ehninger G, Ganser A, et al. Outcome after relapse of myelodysplastic syndrome and secondary acute myeloid leukemia following allogeneic stem cell transplantation: a retrospective registry analysis on 698 patients by the Chronic Malignancies Working Party of the European Society of B. Haematologica. 2018;103:237–45.
Ciurea SO, Zhang MJ, Bacigalupo AA, Bashey A, Appelbaum FR, Aljitawi OS, et al. Haploidentical transplant with posttransplant cyclophosphamide vs matched unrelated donor transplant for acute myeloid leukemia. Blood. 2015;126(8):1033–40.
Wachsmuth LP, Patterson MT, Eckhaus MA, Venzon DJ, Gress RE, Kanakry CG. Post-transplantation cyclophosphamide prevents graft-versus-host disease by inducing alloreactive T cell dysfunction and suppression. J Clin Investig. 2019;129(6):2357–73.
Wachsmuth LP, Patterson MT, Eckhaus MA, Venzon DJ, Kanakry CG. Optimized timing of post-transplantation cyclophosphamide in MHC-haploidentical murine hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2020;26(2):230–41.
Sanz J, Galimard JE, Labopin M, Afanasyev B, Angelucci E, Ciceri F, et al. Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation (EBMT).Post-transplant cyclophosphamide after matched sibling, unrelated and haploidentical donor transplants in patients with acute myeloid leukemia: a comparative study of the ALWP EBMT. J Hematol Oncol. 2020;13(1):46.
Guo H, Chang YJ, Hong Y, Xu LP, Wang Y, Zhang XH, Wang M, Chen H, Chen YH, Wang FR, Wei-Han SYQ, Yan CH, Tang FF, Mo XD, Liu KY, Huang XJ. Dynamic immune profiling identifies the stronger graft-versus-leukemia (GVL) effects with haploidentical allografts compared to HLA-matched stem cell transplantation. Cell Mol Immuno. 2021;18(5):1172–85.
Chang Y-J, Wang Y, Liu Y-R, Xu LP, Zhang XH, Chen H, et al. Haploidentical allograft is superior to matched sibling donor allograft in eradicating pre-transplantation minimal residual disease of AML patients as determined by multiparameter flow cytometry: a retrospective and prospective analysis. J Hematol Oncol. 2017;10(1):134.
Salvatore D, Labopin M, Ruggeri A, Battipaglia G, Ghavamzadeh A, Ciceri F, et al. Outcomes of hematopoietic stem cell transplantation from unmanipulated haploidentical versus matched sibling donor in patients with acute myeloid leukemia in first complete remission with intermediate or high-risk cytogenetics: a study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Haematologica. 2018;103(8):haematol.2018.189258.
Gorin NC, Huang XJ. A vision for the future of allogeneic hematopoietic stem cell transplantation in the next decade. Sci Bull (Beijing). 2022;67(19):1921–4.
Battipaglia G, Labopin M, Kröger N, Vitek A, Afanasyev B, Hilgendorf I, et al. Posttransplant cyclophosphamide vs antithymocyte globulin in HLA-mismatched unrelated donor transplantation. Blood. 2019;134(11):892–9.
Fei Q, Huang XJ, Liu Y, Xu LP, Zhang XH, Liu KY, Chen H, Chen YY, Wang Y. The clinical analysis of haploidentical stem cell transplantation in myelodysplastic syndrome-associated acute myeloid leukemia. Zhonghua Xue Ye Xue Za Zhi. 2018;39(7):589.
Sengsayadeth S, Gatwood KS, Boumendil A, Labopin M, Finke J, Ganser A, et al. Conditioning intensity in secondary AML with prior myelodysplastic syndrome/myeloproliferative disorders: an EBMT ALWP study. Blood Adv. 2018;2(16):2127–35.
Scott BL, Pasquini MC, Logan BR, Wu J, Devine SM, Porter DL, et al. Myeloablative versus reduced-intensity hematopoietic cell transplantation for acute myeloid leukemia and myelodysplastic syndromes.
Nagler A, Labopin M, Dholaria B, Ciceri F, Fraccaroli A, Blaise D, et al. Impact of cytogenetic risk on outcomes of non-T-cell-depleted haploidentical hematopoietic cell transplantation in patients with relapsed or refractory acute myeloid leukemia. Transplant Cell Ther. 2022;28(11):773.e1-773.e8.
Nagler A, Labopin M, Dholaria B, Angelucci E, Afanasyev B, Cornelissen JJ, et al. Comparison of haploidentical bone marrow versus matched unrelated donor peripheral blood stem cell transplantation with posttransplant cyclophosphamide in patients with acute leukemia. Clin Cancer Res. 2021;27(3):843–51.
Gorin NC, Labopin M, Blaise D, de Groot M, Socié G, Bourhis JH, et al. Stem cell transplantation from a haploidentical donor versus a genoidentical sister for adult male patients with acute myelogenous leukemia in first remission: a retrospective study from the acute leukemia working party of the European Society for Blood and Marrow Transplantation. Cancer. 2020;126(5):1004–15.
Lancet JE, Uy GL, Newell LF, Lin TL, Ritchie EK, Stuart RK, et al. Cortes JE.CPX-351 versus 7+3 cytarabine and daunorubicin chemotherapy in older adults with newly diagnosed high-risk or secondary acute myeloid leukaemia: 5-year results of a randomised, open-label, multicentre, phase 3 trial. Lancet Haematol. 2021;8:e481–91.
Acknowledgements
We thank all the EBMT centers and national registries for contributing patients to this study (Additional file 1: Appendix). We also thank the data managers for their excellent work.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
AN wrote the manuscript, designed the study, and interpreted the data. ML and MM designed the study, performed the statistical analyses, interpreted the data, and edited the manuscript. DB, ANR, LLC, SB, SS, JLDM, YK, JP, AK, AB, ABR, PR, CS, EB, JS, AB, SG, and FC reviewed the manuscript and provided clinical data. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The scientific boards of the ALWP of the EBMT approved this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no relevant conflict of interest and no competing financial interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Contributing centers and Supplemental Tables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nagler, A., Labopin, M., Blaise, D. et al. Non-T-depleted haploidentical transplantation with post-transplant cyclophosphamide in patients with secondary versus de novo AML in first complete remission: a study from the ALWP/EBMT. J Hematol Oncol 16, 58 (2023). https://doi.org/10.1186/s13045-023-01450-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13045-023-01450-4