Abstract
Complex chromosomal rearrangements (CCR) are rare chromosomal structural abnormalities. The chromosomal structural variants in CCR carriers are one of the factors contributing to a history of adverse pregnancy and childbirth. In this study, we report a patient with a history of adverse pregnancy and childbirth who exhibited complex balanced chromosomal translocations. The female patient was phenotypically and intellectually normal; in her first pregnancy, the embryo was damaged, and a histological examination of the chromosomes of the embryos revealed a deletion of approximately 4.66 Mb at 1p32.3p32.2, a duplication of approximately 1.02 Mb at 1p22.2p22.1, a duplication of approximately 1.46 Mb at 6q27 and a deletion of approximately 7.78 Mb at 9p24.3p24.1. Chromosomal examinations of the patient revealed the karyotype to be 46,XX,(1;9)(p32; p34). In the second pregnancy, the foetus was diagnosed prenatally with three or more positive ultrasound soft indicators. The patient's karyotype was re-examined and further confirmed by fluorescence in situ hybridisation as 46,XX,t(1;9;6)(p31;p22;q27), revealing this patient was a carrier of complex balanced chromosomal translocations. Carriers of CCR have a higher risk of spontaneous abortion, and genetic counselling clinicians should consider the karyotype analyses of such patients in clinical practice and recheck their chromosomes if necessary.
Similar content being viewed by others
Preface
Complex chromosomal rearrangement (CCR) is a rare structural chromosomal abnormality characterised by three or more breakpoints on two or more chromosomes accompanied by inter- or intra-chromosomal single-segment insertions or translocations, etc. [1,2,3]. As a rare structural recombination, CCR can be balanced or unbalanced [4, 5]. Individuals carrying CCR can be phenotypically normal or exhibit clinical abnormalities [6]. The degree of clinical abnormality in congenital malformations or intellectual dysfunctions in carriers of CCR ranges from normal to mild to severe [7]. Such clinical abnormalities are caused by microdeletions or microduplications near translocation breakpoints, gene disruptions and positional effects located at breakpoints or elsewhere in the genome [8]. Additionally, the likelihood of phenotypic abnormalities increases with the number of CCR-associated breakpoints [3].
Adverse pregnancy outcomes refer to the history of spontaneous miscarriage, embryonic arrest, foetal death, stillbirth, neonatal death and the birth of mentally impaired and malformed babies [9]. There are many causes of adverse pregnancy outcomes, including genetic, anatomical, immunological and biological factors [10,11,12]. Chromosomal abnormalities in parents or embryos are the most common cause of adverse pregnancy and childbirth history [13,14,15]. A statistical analysis of previous studies revealed that 3.5% of couples with a history of recurrent miscarriage have at least one partner who is a CCR carrier [16]. The most frequent type of CCR is translocations, while other rearrangement types include inversions, insertions, deletions and duplications. Additionally, it was found that about 18.4% of CCR carriers produce phenotypically abnormal offspring [16]. Thus, it is of great importance to analyse as accurately as possible whether patients with a history of adverse pregnancies are CCR carriers and to assess the risks they face.
Along with the development of molecular cytogenetics, techniques such as Giemsa banding (G-Banding), fluorescence in situ hybridisation (FISH) and copy number variation sequencing (CNV-seq) have been applied to study chromosomal structural changes [17], and hidden and complex chromosomal rearrangements are yet to be revealed. In this paper, we report the case of an adult female patient with a normal phenotype and intelligence and a history of adverse pregnancy and delivery who was found to be a carrier of complex balanced chromosomal translocations.
Materials and methods
Clinical data of study subjects
The patient was a 22-year-old female, with a normal phenotype and intelligence. She was 158 cm tall and weighed 48 kg. The patient and her husband were nonconsanguineous, and the patient had had two post-marital pregnancies and one embryonic arrest in 2020, with a chromosomal examination via embryonic histology. During the second pregnancy (20 weeks + 3 days), the patient requested a prenatal diagnosis at the Department of Reproductive Genetics at Hebei Provincial People's Hospital. The study was approved by the institutional ethics committee for sample collection, and the patient provided signed informed consent.
Cytogenetic analysis of dominant bands
The patient underwent a metaphase chromosome analysis by G-Banding at a resolution level of 400 bands, and karyotyping was performed on her husband. The karyotype description was based on the recommendations of the International System for Human Cytogenetic or Cytogenomic Nomenclature [18].
Molecular cytogenetic analysis
A combination of Tel1p (green), Tel1q (red), CEP1 (red), Tel6q (red), CEP6 (white), Tel9p (green) and CEP9 (white) probes were used during FISH for high-resolution molecular cytogenetic analysis.
Chromosome karyotype analysis
The cell division phase was first observed under a 10 × microscope before being transferred to a 100 × oil immersion lens for detailed observation. Thirty division phases were counted, and those with abnormalities were doubled for counting and analysis. Three of the division phases with appropriate length, clear bands and good dispersion were analysed and diagnosed, and karyotype maps were drawn and printed. The karyotype description was based on the recommendations of the International System for Human Cytogenetic Nomenclature [18].
Results
In 2020, the patient experienced embryonic suspension, and chromosomal examination via embryonic histology revealed a deletion of about 4.66 Mb at 1p32.3p32.2, a duplication of about 1.02 Mb at 1p22.2p22.1, a duplication of about 1.46 Mb at 6q27 and a deletion of about 7.78 Mb at 9p24.3p24.1. The chromosomes of both husband and wife were examined, and the husband’s chromosomes were normal. However, the chromosomal examination of the female partner showed 46,XX,t(1;9)(p32;p34), i.e. a translocation of short arm 3 of chromosome 1 at band 2 to short arm 3 of chromosome 9 at band 4.
The patient came to our department for prenatal diagnosis in her second pregnancy at 20 weeks + 3 days of gestation. She denied any history of exposure to toxic or harmful substances or radiation during her pregnancy. Foetal ultrasonography was performed in our department and indicated that the foetal cerebellum was slightly small, with a strong light spot in the left ventricle, enhanced echogenicity in both kidneys and localised echogenicity in the lower abdomen. Amniocentesis and amniotic fluid karyotype analyses were performed, and the results showed no numerical or structural chromosomal abnormalities. However, the amniotic fluid CNV-seq revealed a deletion of about 1.6 Mb in the 6q27q27 region (a pathogenic variant) and a duplication of 4.68 Mb in the 1p32.3p32.2 region (a suspected pathogenic variant).
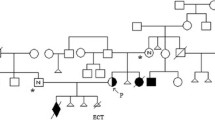
Given the presence of approximately 1.46 Mb of duplication of chromosome 6q27 in the embryo examined at the time of foetal arrest in the first pregnancy and the results of the amniotic fluid in the second pregnancy, which suggested a deletion of approximately 1.6 Mb in the 6q27q27 region, the female's chromosome was re-examined at the genetics centre of the Reproductive and Genetic Hospital of CITIC Xiangya. The karyotype analysis revealed 46,XX,t(1;9;6)(p31;p22;q27), and a balanced translocation of complex chromosomes 1, 9 and 6 was observed in this patient (Fig. 1). The results were confirmed by FISH. A Tel 9p (green)/Tel 6q (red) /CEP6 (white) probe combination was applied for FISH using the peripheral blood metaphases of the subject. Thirty division phases were observed, and one derived chromosome 6 and one derived chromosome 1 were observed in each division phase (Fig. 2A). The probe combination of Tel 1p (green)/Tel 1q (red)/CEP1 (red)/CEP9 (white) was applied for FISH using the peripheral blood metaphases of the subject. Thirty division phases were observed, and one derived chromosome 1 and one derived chromosome 9 were observed in each division phase (Fig. 2B). The female was reconfirmed via FISH as a carrier of complex translocations of chromosomes 1, 6 and 9.
Confirmation of fluorescence in situ hybridization (FISH) results Patient karyotype was 46,XX,t(1;9;6)(p31;p22;q27). Note: Figure on the left shows: A Tel 9p (green)/Tel 6q (red) /CEP6 (white) probe combination was applied for FISH with the peripheral blood metaphases of the subject. Thirty division phases were observed, and one derived chromosome 6 and one derived chromosome 1 were observed in each division phase. Figure on the right shows: A Tel 1p (green)/Tel 1q (red)/CEP1 (red)/CEP9 (white) probe combination was applied for FISH with the peripheral blood metaphases of the subject. Thirty division phases were observed, and one derived chromosome 1 and one derived chromosome 9 were observed in each division phase
Discussion
In the general population, CCR is rarely found. The condition is usually associated with congenital anomalies, mental impairment, recurrent spontaneous abortions and infertility [19]. For example, Sinkar and Devi [20] reported a boy who inherited a significantly balanced chromosomal translocation from his deaf–mute mother, showing mental impairment and aphasia. However, Campos et al. [21] showed that the frequency of balanced CCR in the population may be underestimated since it may not cause phenotypic effects and may not be detected by the analysis method used. This is similar to the results of the present study. The CCR patient reported herein had normal phenotyping and intelligence, but the karyotype analysis revealed that the patient was a complex chromosome translocation carrier.
There are four types of CCRs based on the combination of chromosome number and breakpoints. Type I, the simplest and most common, is inherited maternally; it is characterised by an equal number of chromosomes and breakpoints in CCRs, known as triple rearrangements (three chromosomes with one breakpoint on each chromosome), and it is the most common of all CCR cases [22]. Balanced translocations are partly inherited from the parents and partly caused by chromosomes breaking and rejoining during sperm or egg formation or fertilisation of the ovum [23, 24]. During this process, two chromosomes are exchanged after the break, and no increase or decrease of chromosomal fragments is involved. The carrier has normal intelligence and phenotyping, and the clinical manifestations may include infertility, recurrent miscarriages, embryonic arrest and embryonic developmental malformations [25].
Carriers of balanced translocations of two chromosomes form quadriradial chromosomes during meiosis; they produce 18 gametes, of which 1 is normal and 1 is a balanced translocation carrier, with the remaining 16 being unbalanced gametes [26]. The balanced translocations carried by the patient reported in this study involved a total of three chromosomes (1, 9 and 6). They were a carrier of complex translocations, which had an increased chance of chromosomal rearrangement compared with carriers involving only two chromosomes in reciprocal translocations, which are more likely to form unbalanced gametes. These complex balanced translocations were responsible for a history of adverse pregnancy and delivery [27]. In the patient's first pregnancy with foetal arrest, the embryo was examined for chromosomes 1, 6 and 9, with varying degrees of microdeletions or microduplications, and an examination of the patient's chromosomes suggested balanced translocations of chromosomes 1 and 9. In the patient's second pregnancy, the foetus exhibited three or more positive ultrasound soft indicators, which suggested an increased risk of chromosomal foetal abnormalities. The amniotic fluid CNV suggested chromosome 6 microdeletion as a pathogenic variant and chromosome 1 microduplication as a suspected pathogenic variant; both embryonic tissue and amniotic fluid suggested chromosome 6 abnormality, so the patient's chromosomes were re-examined. Finally, the patient was identified as a complex translocation carrier of chromosomes 1, 9 and 6.
The patient's gestational amniotic fluid CNV detected a deletion of approximately 1.60 Mb in the 6q27q27 region, which was a pathogenic variant containing 11 protein-coding genes, including DLL1, THBS2, ERMARD and TBP. The DLL1 gene was evaluated by ClinGen as a single-dose-sensitive gene [28]. DLL1 acts as a ligand for Notch and plays an important role in Notch signalling [29]. Studies have shown that abnormalities in the DLL1/Notch signalling pathway can lead to abnormal embryonic development, dysregulation of biological processes and malignant transformation [30]. In mammalian cells, the DLL1/Notch signalling pathway is associated with the maintenance of homeostasis in stem cells [31]. In addition, when Notch signalling is active, the Notch ligand (DLL1) binds to Notch receptors on the surface of neighbouring cells where it induces the expression of genes that inhibit neural differentiation, thereby maintaining the cell in a proliferative state. The pathogenic variant formed by the microdeletion of the 6q27q27 region detected by the CNV of this patient's pregnancy amniotic fluid may have been related to the loss of function of the protein encoded by this region of the gene.
In the present study, the patient had discrepancies in the results of two karyotypic analyses; the first showed translocations only of chromosomes 1 and 9, while the second showed complex balanced translocations of chromosomes 1, 6 and 9, which were further confirmed by FISH. There are various reasons for the discrepancy in the results of the two examinations, for example, the resolution (high vs low) of the G-Banding karyotype analysis may have led to variations in the results.
Conclusion
Carriers of CCR have a higher risk of having both spontaneous miscarriage and offspring with unbalanced karyotypes. Therefore, in clinical practice, genetic counsellors should accurately analyse whether patients with a history of adverse pregnancies are CCR carriers; furthermore, they should evaluate their risks and provide appropriate fertility advice.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
References
Poot M. Of simple and complex genome rearrangements, chromothripsis, chromoanasynthesis, and chromosome chaos. Mol Syndromol. 2017;8(3):115–7.
Poot M, Haaf T. Mechanisms of origin, phenotypic effects and diagnostic implications of complex chromosome rearrangements. Mol Syndromol. 2015;6(3):110–34.
Priya PK, Mishra VV, Liehr T, et al. Characterization of a complex chromosomal rearrangement involving chromosomes 1, 3, and 4 in a slightly affected male with bad obstetrics history. J Assist Reprod Genet. 2018;35(4):721–5.
Leone PE, Yumiceba V, Jijón-Vergara A, et al. Cytogenetic and genomic analysis of a patient with turner syndrome and t(2;12): a case report. Mol Cytogenet. 2020;13(1):46.
Hemmat M, Yang X, Chan P, et al. Characterization of a complex chromosomal rearrangement using chromosome, FISH, and microarray assays in a girl with multiple congenital abnormalities and developmental delay. Mol Cytogenet. 2014;7:50.
Pan Q, Hu H, Han L, et al. Mapping breakpoints of complex chromosome rearrangements involving a partial trisomy 15q23.1–q26.2 revealed by next generation sequencing and conventional techniques. PLoS ONE. 2016;11(5):0154574.
de Vree PJ, Simon ME, van Dooren MF, et al. Application of molecular cytogenetic techniques to clarify apparently balanced complex chromosomal rearrangements in two patients with an abnormal phenotype: case report. Mol Cytogenet. 2009;2:15.
Engvall M, Cahill N, Jonsson BI, et al. Detection of leukemia gene fusions by targeted RNA-sequencing in routine diagnostics. BMC Med Genomics. 2020;13(1):106.
Jenderny J. Chromosome aberrations in a large series of spontaneous miscarriages in the German population and review of the literature. Mol Cytogenet. 2014;7:38.
Ouyang F, Zhang J, Betrán AP, et al. Recurrence of adverse perinatal outcomes in developing countries. Bull World Health Organ. 2013;91(5):357–67.
Sabiri N, Kabiri M, Karboubi L, et al. Risk factors for perinatal mortality at Souissi maternity hospital, Rabat. Morocco Int J Gynaecol Obstet. 2012;119(3):285–6.
Mortensen LH. Socioeconomic inequality in birth weight and gestational age in Denmark 1996–2007: using a family-based approach to explore alternative explanations. Soc Sci Med. 2013;76(1):1–7.
Tan Y, Yin X, Zhang S, et al. Clinical outcome of preimplantation genetic diagnosis and screening using next generation sequencing. Gigascience. 2014;3(1):30.
Tucker T, Montpetit A, Chai D, et al. Comparison of genome-wide array genomic hybridization platforms for the detection of copy number variants in idiopathic mental retardation. BMC Med Genomics. 2011;4:25.
Yin L, Tang Y, Lu Q, et al. Application value of NIPT for uncommon fetal chromosomal abnormalities. Mol Cytogenet. 2020;13:39.
Ou J, Yang C, Cui X, et al. Successful pregnancy after prenatal diagnosis by NGS for a carrier of complex chromosome rearrangements. Reprod Biol Endocrinol. 2020;18(1):15.
Luo A, Cheng D, Yuan S, et al. Maternal interchromosomal insertional translocation leading to 1q43-q44 deletion and duplication in two siblings. Mol Cytogenet. 2018;11:24.
McGowan-Jordan J, Hastings R, Moore S. Re: international system for human cytogenetic or cytogenomic nomenclature (ISCN): some thoughts, by T. Liehr Cytogenet Genome Res. 2021;161(5):225–6.
Nguyen MH, Morel F, Pennamen P, et al. Balanced complex chromosome rearrangement in male infertility: case report and literature review. Andrologia. 2015;47(2):178–85.
Sinkar P, Devi SR. Complex chromosomal rearrangement: a case report to emphasize the need for parental karyotyping and genetic counseling. J Hum Reprod Sci. 2020;13(1):68–70.
Campos AE, Rosenberg C, Krepischi A, et al. An Apparently balanced complex chromosome rearrangement involving seven breaks and four chromosomes in a healthy female and segregation/recombination in her affected son. Mol Syndromol. 2021;12(5):312–20.
Loup V, Bernicot I, Janssens P, et al. Combined FISH and PRINS sperm analysis of complex chromosome rearrangement t(1;19;13): an approach facilitating PGD. Mol Hum Reprod. 2010;16(2):111–6.
Colley E, Devall AJ, Williams H, et al. Cell-free DNA in the investigation of miscarriage. J Clin Med. 2020;9(11):3428.
Tezcan B, Bredaki FE. Prenatal diagnosis of rare familial unbalanced translocation of chromosomes 7 and 12. Case Rep Obstet Gynecol. 2015;2015: 905946.
Mitsuhashi S, Ohori S, Katoh K, Frith MC, Matsumoto N. A pipeline for complete characterization of complex germline rearrangements from long DNA reads. Genome Med. 2020;12(1):67.
Shilenkova YV, Pendina AA, Mekina ID, et al. Age and serum AMH and FSH levels as predictors of the number of oocytes retrieved from chromosomal translocation carriers after controlled ovarian hyperstimulation: applicability and limitations. Genes (Basel). 2020;12(1):18.
Vozdova M, Oracova E, Kasikova K, et al. Balanced chromosomal translocations in men: relationships among semen parameters, chromatin integrity, sperm meiotic segregation and aneuploidy. J Assist Reprod Genet. 2013;30(3):391–405.
Yamasaki M, Makino T, Khor SS, et al. Sensitivity to gene dosage and gene expression affects genes with copy number variants observed among neuropsychiatric diseases. BMC Med Genomics. 2020;13(1):55.
Varshney S, Wei HX, Batista F, et al. A modifier in the 129S2/SvPasCrl genome is responsible for the viability of Notch1[12f/12f] mice. BMC Dev Biol. 2019;19(1):19.
Huang MT, Chiu CJ, Chiang BL. Multi-faceted notch in allergic airway inflammation. Int J Mol Sci. 2019;20(14):3508.
Chillakuri CR, Sheppard D, Lea SM, Handford PA. Notch receptor-ligand binding and activation: insights from molecular studies. Semin Cell Dev Biol. 2012;23(4):421–8.
Funding
The Medical Science Research Project in Hebei Province (No.20190387; No.20211535).
Author information
Authors and Affiliations
Contributions
Yan Luo and Hezhen Lu conceived of the study, Yanshang Zhang and Zhiqiang Cui participated in its design and coordination, Pingping Zhang and Yali Li helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research was approved by the Ethics Committee of Maternity and child Care Hospital of Huaihua. All patient guardians gave informed consent to the study.
Consent for publication
Consent to Publish.
Competing of interests
All of the authors had no any personal, financial, commercial or academic conflicts of interest separately.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Luo, Y., Lu, H., Zhang, Y. et al. A case of complex balanced chromosomal translocations associated with adverse pregnancy outcomes. Mol Cytogenet 15, 37 (2022). https://doi.org/10.1186/s13039-022-00615-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13039-022-00615-z