Abstract
Background
Canadians endured unprecedented mental health (MH) and support access challenges during the first COVID-19 wave. Identifying groups of individuals who remain at risk beyond the acute pandemic phase is key to guiding systemic intervention efforts and policy. We hypothesized that determinants of three complementary, clinically actionable psychiatric outcomes would differ across Canadian age groups.
Methods
The Personal Impacts of COVID-19 Survey (PICS) was iteratively developed with stakeholder feedback, incorporating validated, age-appropriate measures. Baseline, cross-sectional online data collected between November 2020-July 2021 was used in analyses. Age group-specific determinants were sought for three key baseline MH outcomes: (1) current probable depression, generalized anxiety disorder, obsessive–compulsive disorder and/or suicide attempt during COVID-19, (2) increased severity of any lifetime psychiatric diagnosis, and (3) inadequate MH support access during COVID-19. Multivariable logistic regression models were constructed for children, youth (self- and parent-report), young adults (19–29 years) and adults over 29 years, using survey type as a covariate. Statistical significance was defined by 95% confidence interval excluding an odds ratio of one.
Results
Data from 3140 baseline surveys were analyzed. Late adolescence and early adulthood were identified as life phases with the worst MH outcomes. Poverty, limited education, home maker/caregiver roles, female and non-binary gender, LGBTQ2S + status and special educational, psychiatric and medical conditions were differentially identified as determinants across age groups.
Interpretation
Negative psychiatric impacts of COVID-19 on Canadians that include poor access to MH support clearly persisted beyond the first wave, widening pre-existing inequity gaps. This should guide policy makers and clinicians in current and future prioritization efforts.
Similar content being viewed by others
Introduction
Pre-Pandemic mental health (mh) and support access across the lifespan
One in five Canadians are affected by mental illness [64], with difficulties typically emerging during adolescence and early adulthood [65]. Across age groups, depression and generalized anxiety are particularly common [21, 42]. Vulnerability to mental illness is influenced by a combination of genetic risk factors and socio-environmental determinants including, for Canadian children and youth, low family/neighborhood income, limited education/employment opportunities, housing/food insecurity, and early life stressors [65]; and for Canadian adults, low socioeconomic status and educational attainment, unemployment, female and non-binary gender, lesbian/gay/bisexual orientation, and chronic physical disease/disability, among others [3, 49, 66, 68, 69].
Fortunately, the long-term morbidity of most psychiatric illnesses can be mitigated through early intervention [8]. In fact, access to MH service mediates relationships between determinants and outcomes among young Canadians [65]. However, many Canadians have difficulty accessing MH support and those that cannot may be among the most vulnerable. As per the 2012 Canadian Community Health Survey, 20% accessed formal or informal MH support [60] and 12% reported unmet MH needs. Those with unmet needs were younger, more commonly had substance use disorders, and had fewer interactions with professionals [14, 57].
Initial pandemic impacts on MH
At this point, it is well-established that the initial wave of COVID-19 was associated with global impacts on mental health, especially anxiety and depression [10]. Our systematic review of MH data from the first COVID-19 wave identified increased depression and anxiety symptoms among children and youth, with older adolescents, females, neurodiverse and chronically ill individuals appearing most underserved [51]. Increased anxiety and depression symptoms also emerged among adults but were reportedly restricted to the early months of 2020 [2, 11]. Obsessive–compulsive disorder (OCD) symptoms increased during the pandemic, regardless of diagnostic status [26, 34]. Globally, risk appeared greatest in younger versus older adults [63], in the LGBTQ + community [45] and among adults with pre-existing psychiatric diagnoses [27]. However, Canada-specific data indicated divergent influences of pre-existing psychiatric diagnosis with deterioration in some and improvement in others [9].
Ongoing pandemic impacts on MH
Beyond the initial impact of the pandemic, Canadians have endured unprecedented impacts to daily activities across multiple COVID-19 waves. Given that the ‘incubation period’ for psychiatric problems typically exceeds that for infectious illness, it is critical to build upon literature from the first wave and identify the extent to which clinically significant psychiatric problems emerged through the pandemic, what social determinants are most predictive of these concerns, and what needs for MH support remain unmet. Further, as life experience and developmental life stage may differentially influence vulnerability and resilience [61], identification of age group-specific determinants provides an important contribution to guide policy and intervention.
This study responds to calls for examination of long-term pandemic MH impacts and service provision in different age groups [20, 28, 40, 51]. Broad, transdiagnostic MH outcomes were intentionally defined based upon their actionable and societal relevance, including expectedly common or potentially lethal psychiatric problems, increased severity of any clinically-diagnosed psychiatric condition and inadequate MH support access. GAD, depression and OCD were selected for focus based on first wave studies [10, 34, 51, 63]. Further, since increased anxiety, sadness and contamination avoidance during COVID-19 would be expected and not necessarily indicative of a need for clinical attention among Canadians, we also required the presence of symptom-related impairment, using a more conservative approach than many early pandemic studies [20]. Suicide attempts during COVID-19 were also included, given pandemic associated risk [6], interconnections with psychiatric illness [38, 70] and associated mortality risk [17].
We hypothesized that distinct age group-specific determinants would predict: (1) common or high lethality psychiatric problems [defined by at least one of: suicide attempt during COVID-19, or probable Generalized Anxiety Disorder (GAD), Major Depressive Disorder (MDD) or Obsessive–Compulsive Disorder (OCD) at baseline]; (2) increased severity of any diagnosed lifetime psychiatric illness during COVID-19; and (3) unmet MH support needs.
Method
Study design
The online survey study protocol was approved by the UBC Children’s and Women’s Research Ethics Board (see Additional file 5). Baseline data collection transpired from November 2020- July 2021 after the first COVID-19 wave in Canada (see Additional file 2). Data from follow-up surveys are not presented in this paper. See details in the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) [12] (see Additional file 1).
Selection and description of participants
Multi-source recruitment via social media and targeted, non-random approaches [43] aimed to recruit a representative sample of 3000 Canadians for maximal result generalizability (Table 1). Canadians over 8 years (years) were eligible. Non-Canadians, suspected fraudulent respondents, those without stated age and non-completers were excluded (see Additional file 5).
Primary measurements/outcomes
The Personal Impacts of COVID-19 Survey (PICS) combines validated questionnaires and novel items, iteratively co-created with stakeholders between April and November 2020 (see acknowledgment section). Versions included self-reports for youth and adults, and parent-reports for children/youth. Items characterized individuals, pandemic impacts and pandemic-era supports.
Outcome 1: Probable GAD, depression, OCD and/or pandemic-era suicide attempt
GAD, depression and OCD symptoms were identified via validated measures: the Generalized Anxiety Disorder Scale (GAD-7) [36, 55], Patient Health Questionnaire for Depression (PHQ-9) [29, 46] and the Obsessive–Compulsive Inventory–Revised (OCI-R) and -Child Version (OCI-CV) [15, 16], with clinical threshold scores of 10, 10, 21 and 11, respectively. “How difficult have these problems made it for you to do your work, take care of things at home, or get along with other people?” queried impact required for GAD and depression. Item 2 from adult/child versions of the Yale-Brown Obsessive Compulsive Scale [24, 52] queried impact required for OCD. Above-threshold scores with concurrent impairment, or a reported COVID-19-era suicide attempt provided a dichotomous indicator of clinically relevant psychiatric problems.
Outcome 2: Increased severity of any diagnosed psychiatric illness
Those reporting one or more lifetime psychiatric diagnoses by a health professional were asked for each disorder whether its severity changed during COVID-19, using a 5-point Likert scale with item scoring from “much worse” to “much better”.
Outcome 3: unmet MH support needs
Unmet MH support needs were captured by asking respondents if they had needed but not received support for their MH, with response choices of “yes” or “no”.
Statistical analyses
Data processing and statistical models were constructed using R version 4.1.1 (r-project.org). Data were initially summarized using descriptive statistics, including mean scores and standard deviations for continuous measures and numbers and percentages for categorical variables. Data were identified as missing at the item-level. Forty missing item-level data sets were imputed using ‘mice’ (version 3.13.0) [62]. Imputed values’ quality was assured by evaluating imputed values distributions and trace plots for proper mixing and spike absence in the iterations. Subsequent analyses were conducted on each imputed data set with estimates pooled using Rubin’s rule [48] and degrees of freedom calculated using Barnard-Rubin adjustment [5].
Primary analyses involved multivariable logistic regression models, in which the binary outcome variable was regressed on primary variables of interest and covariates. Separate regression models were constructed for each age group (parent-report on children under 8 years, parent-report on youth 8–18 years, youth self-report 8–18 years, and self-reports on young adults 19–29 years, and adults over 29 years). Due to survey differences, not all included variables were identical across models. Key variables in all models included: age, gender, race (white versus other), residence (rural versus urban), poverty (income under $75,000 and/or food insecurity), lifetime psychiatric diagnosis, medical condition and assessment period (dichotomized starting March 1, 2021). Additional variables of interest were special education needs of 0–18 year old (all models except adult self-report); LGBTQ2S + status (all models except parent-report); and current employment status (adult self-report models). For adult models, survey type was included as a covariate. Model results are presented using odds ratios (OR) and 95% confidence intervals. Statistical significance was identified based on 95% confidence intervals that do not include the OR of one (equivalent to a nominal p value < 0.05).
Results
Baseline participants
Data from 3140 participant baseline surveys were included for analyses (see Additional file 3). Table 1 characterizes demographic and traditional MH determinant prevalence across age groups relative to the Canadian population (indicating degree of anticipated study result generalizability). Additional details are provided in Additional file 4. Across age groups, individuals identifying as female, non-binary, non-white, LGBTQ2S + , immigrants, urban residents, and those with medical conditions were adequately represented, as were children and youth with special educational needs. Under-represented characteristics across age groups included specific ethnicities (Metis/First Nations, east/central Asians), rural/northern residents, low educational attainment, living in poverty (except in young adults) and, among adults, male gender.
Determinants of current GAD, depression or OCD and/or pandemic-era suicide attempt
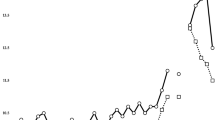
Prevalence of components of outcome #1 as reported at baseline across age groups are detailed in Table 2. Associated factors differed across age groups (Fig. 1).
Predictors of selected psychiatric problems (any of suicide attempt during COVID-19 or GAD/depression/OCD with impairment) by age groups. Note. * p < .05. Panel A: children (0–7 year) by parent-report and youth (8–18 year) by parent- and self-reports Panel B: young adults (19–29 year) and adults over 30 year by self-report
Figure 1A presents results of multivariable logistic regression models pertaining to selected psychiatric problems (with binary dependent variable indicating the presence of one or more of probable GAD, depression, OCD or suicide attempt) in children (0–7 years) and youth (8–18 years). Figure 1B presents associated factors among young adults (19–29 years) and adults over 29 years.
Determinants of Worsening Severity of Any Lifetime Psychiatric Diagnoses during COVID-19
Data on lifetime psychiatric diagnoses, rates of increased severity since the onset of COVID-19, and attribution of increased severity to COVID-19 is provided in Table 3.
Regression models for increased diagnostic severity were not constructed for children or youth due to limited sample sizes of those with lifetime diagnoses. Figure 2 shows regression results for the young adult and adults over 30 years age groups.
Table 4 provides descriptive data on pandemic-era MH support across age groups as reported following the first wave.
Determinants of unmet MH support needs during the COVID-19-era are shown in Fig. 3a (for children and youth) and Fig. 3b (for young adults and adults 30 years and older.
Discussion
Key findings
This study adds to pre-pandemic and first wave evidence, with findings that negative MH impacts of COVID-19 persist, and that these impacts and their predictors differ across age groups (Table 5). While COVID-19 infection has not spared any sector of society, MH sequelae of the pandemic appear to have disproportionately impacted Canadians transitioning from childhood to adulthood. Moreover, pre-existing MH disparities have been amplified, with ongoing or increasing influence of determinants such as poverty, limited education, LGBTQ2S + status, female and non-binary gender, medical and psychiatric illness.
Prevalence
Rates of GAD, depression, OCD and unmet MH support needs were multiple-fold of those reported by Canadian pre-pandemic studies including the 2014 Ontario Child Health Survey [21, 42] and the 2012 Canadian Community Health Survey [57] (see Additional file 3). As noted, feelings of sadness and worry and washing behaviors are all expected during an infectious pandemic, and as such, caution was required to not pathologize or label individuals based upon these singular symptoms. The use of validated psychiatric measures and the requirement for associated impairment add confidence to our conclusion that prevalence remained markedly amplified compared to pre-pandemic Canadian rates. Moreover, while Aknin et al. [2] reported on resolution of anxiety and depression symptoms beyond early 2020, our study found that these continued Aknin at least until mid-2021.
Age
The age-specific patterns parallel separate results of Canadian child [9, 51] and adult [11, 41] studies and those from other countries [10, 19]. Specifically, older adolescents and young adults report highest levels of common or high lethality psychiatric problems. Emergence of mental illness generally occurs between 14 and 25 years [54], representing a sensitive period of development into mature adulthood. As such, it follows that pandemic impacts on social isolation, educational environments, job loss and MH service availability disproportionately affected youth and young adults [59]. Amplifying challenges, this life phase also aligns with lapse of service between child and adult MH systems that exist in Canada and globally [39, 53].
Gender and orientation
Relative to males, female youth and non-binary young adult participants were at increased risk for poor MH outcomes. This generally tracks with risk for mental illness outside the pandemic experience [21, 49]. Given that gender-specific expectations and stressors have disproportionately affected females during the pandemic [4], it is clear why female gender was predictive in youth but less clear why it was not a determinant among adults in our study.
Non-binary individuals had greater risk for increased severity of psychiatric diagnoses in this study. Unfortunately, this group has been particularly avoidant of healthcare professional contact during the pandemic [58]. As such, MH care systems should optimally provide multiple options such as digital, telehealth and in-person sessions to accommodate individual preference and needs [37].
LGBTQ2S + status was a determinant of poor MH among Canadian youth and young adults. Potential explanations include exacerbated isolation in a previously socially isolated group [32], being quarantined with unsupportive parents [13] or in abusive environments [18] and increased peer victimization [22]. As such, targeted resources and support for Canadians in the LGBTQ + community are warranted. This may include provision of LGBTQ-affirming virtual extracurricular activities [25], social media MH resources such as the Trevor Project [18] and safe spaces [56]. It is advised to be particularly aware of intersectionally marginalized LGBTQ + groups such as those living in poverty who may not have access to digital technology [50].
Socioeconomic factors
Living in poverty increased risk for selected mental illness and for unmet support needs across youth and adult groups, doubling risks among adults over 30 years. Association between financial difficulties and poor MH was noted in Canadian first wave COVID-19 studies of children and adolescents [9, 47] and adults [44]. Exacerbation of negative impacts of poverty on MH have also been demonstrated globally [30], with amplification in those living with food insecurity [67]. However, to our knowledge, the link between poverty and failure to access MH support among Canadians during COVID-19 is novel. While this result may be unsurprising given pre-COVID-19 patterns, it is also particularly concerning given that Canada’s healthcare system aims to be universal. These results may reflect challenges in the system's capacity to either adapt to increased needs or maintain prior level of services in the context of the pandemic (particularly given inequities at baseline). Other identified socioeconomic determinants include limited educational attainment in adults, which relates to income potential, and ‘homemaker/caregiver’ occupational status among adults over 30 years old, which may limit financial autonomy and/or opportunities for social interaction. Regardless, it appears that COVID-19 exacerbated the role of poverty as a pre-existing disparity and action is needed to improve the availability and delivery of MH services to low-income populations.
Diagnosed conditions
Across all age groups, the lifetime diagnosis of a psychiatric illness was a determinant for current psychiatric problems and/or unmet MH support needs during the pandemic. This is generally consistent with the conceptualization that psychiatric illness can be exacerbated by stressful events [18]. Other conditions selectively conferred risk for current psychiatric problems and unmet MH support needs in either the youngest or oldest age group.
Children with special educational needs were significantly more vulnerable to negative outcomes. This may reflect the general vulnerability of these populations to stressful events or relate more specifically to the impacts of COVID-19 related changes (e.g, youth with special needs were less able to adapt to changes in school delivery). A Canadian study by Gonzalez et al. [23] found that while children with special educational needs received fewer clinical services during COVID-19, those who were also living in poverty, or who had parents with limited education or less than a full-time job were especially unlikely to receive services. As such, it is critical that these multiply disadvantaged families be targeted to receive tailored and individualized services to enable continuity of care throughout this and future pandemics. Moreover, support for their parents and caregivers is necessary to prevent burnout and their own MH challenges [1].
Medical illness was found to be a determinant of poor MH and unmet support needs in adults. These individuals were likely most directly impacted by delays or changes to health service provision as the system pivoted to prioritize COVID-19 patients. Indeed, McElroy-Heltzel et al. [35] found that among adults with illness, COVID-related loss of services was associated with mental distress, which was only partially buffered by the presence of social support. Maintenance of usual daily activities including exercise and social contacts is a recommended mitigation strategy to build psychological resilience and prevent mental illness onset among the medically ill during COVID-19 [31].
Limitations
Despite recruitment efforts, our sample under-represented Canadians of Indigenous and East/Central Asian ethnicity, street-involved individuals and rural/northern residents, limiting the ability to examine these as possible determinants. Moreover, limitations inherent to online survey research including potential selection bias and volunteer effects may have had an impact on outcomes [12]. While increased severity of any psychiatric diagnosis was considered as an outcome, the presence of potentially new onset disorders other than depression, GAD and OCD were not systematically examined via diagnostic screens. In hindsight, for example, inclusion of an eating disorder screen would have been advisable, given emergent findings in youth [54].
However, the decision to include only three diagnostic screens was made in an effort to minimize participant burden and data validity impacts due to subject fatigue. In addition, diagnostic interviews were not conducted, although checklists may offer comparable results [7, 33]. Future research would benefit from the consideration of intersectionality (e.g, individuals with multiple determinants may be at disproportionately elevated risk for poor outcomes) while mixed-methods studies are also warranted to gain in-depth appreciation of individual narratives.
Conclusion
Extending beyond the first wave, the COVID-19 pandemic has resulted in an ongoing and detrimental impact on the MH of Canadians, especially in young adults. Sadly, increasing disparities were observed in those already at risk for poor MH according to poverty/food insecurity, sex and gender minority status and prior psychiatric and health conditions. It is crucial that these findings be considered in optimizing interventions and policies to close the gap on pandemic-era and post-pandemic era MH inequities among Canadians.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- GAD:
-
Generalized anxiety disorder
- CHERRIES:
-
Checklist for reporting results of internet E-surveys
- GAD-7:
-
Generalized anxiety disorder scale
- LGBTQ2S+:
-
Lesbian/gay/Bisexual/transsexual/queer/2 spirit
- MDD:
-
Major depressive disorder
- MH:
-
Mental health
- OCD:
-
Obsessive–compulsive disorder
- OCI-CV:
-
Obsessive–compulsive inventory – revised (OCI-R) and -child version
- OR:
-
Odds ratio
- PICS:
-
Personal impacts of COVID-19 Survey
- PHQ-9:
-
Patient health questionnaire for depression
- YA:
-
Young adults
References
Aishworiya R, Kang YQ. Including children with developmental disabilities in the equation during this covid-19 pandemic. J Autism Dev Disord. 2021;51(6):2155–8.
Aknin LB, Andretti B, Goldszmidt R, Helliwell JF, Petherick A, De Neve JE, Dunn EW, Fancourt D, Goldberg E, Jones SP, Karadag O. Policy stringency and mental health during the COVID-19 pandemic: a longitudinal analysis of data from 15 countries. Lancet Public Health. 2022;7(5):e417–26.
Allen J, Balfour R, Bell R, Marmot M. Social determinants of mental health. Int Rev Psychiatry. 2014;26(4):392–407.
Almeida M, Shrestha AD, Stojanac D, Miller LJ. The impact of the COVID-19 pandemic on women’s mental health. Arch Womens Ment Health. 2020;23(6):741–8. https://doi.org/10.1007/s00737-020-01092-2.
Barnard J, Miscellanea RDB. Small-sample degrees of freedom with multiple imputation. Biometrika. 1999;86(4):948–55.
Bersia M, Koumantakis E, Berchialla P, Charrier L, Ricotti A, Grimaldi P, Dalmasso P, Comoretto RI. Suicide spectrum among young people during the COVID-19 pandemic: a systematic review and meta-analysis. EClinicalMedicine. 2022;54: 101705.
Boyle MH, Duncan L, Georgiades K, Bennett K, Gonzalez A, Van Lieshout RJ, Szatmari P, MacMillan HL, Kata A, Ferro MA, Lipman EL. Classifying child and adolescent psychiatric disorder by problem checklists and standardized interviews. Int J Methods Psychiatr Res. 2017;26(4): e1544.
Carver J, Cappelli M, Davidson S, Caldwell W, Belair MA. Vloet M. Taking the next step forward: building a responsive mental health and addictions system for emerging adults. Ottawa: Mental Health Commission of Canada; 2015.
Cost KT, Crosbie J, Anagnostou E, Birken CS, Charach A, Monga S, Kelley E, Nicolson R, Maguire JL, Burton CL, Schachar RJ. Mostly worse, occasionally better: impact of COVID-19 pandemic on the mental health of Canadian children and adolescents. Eur Child Adolesc Psychiatry. 2022;31(4):671–84.
COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–12.
Czeisler MÉ, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, Weaver MD, Robbins R, Facer-Childs ER, Barger LK, Czeisler CA, Howard ME, Rajaratnam SMW. Mental health, substance use, and suicidal ideation during the COVID-19 Pandemic—United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(32):1049–57.
Eysenbach G. Improving the quality of Web surveys: the checklist for reporting results of internet e-surveys (CHERRIES). J Med Internet Res. 2004;6(3): e132.
Fish JN, McInroy LB, Paceley MS, Williams ND, Henderson S, Levine DS, Edsall RN. “I’m kinda stuck at home with unsupportive parents right now”: LGBTQ youths’ experiences with COVID-19 and the importance of online support. J Adolesc Health. 2020;67(3):450–2.
Fleury MJ, Grenier G, Vallée C, Aubé D, Farand L, Bamvita JM, Cyr G. Implementation of the quebec mental health reform (2005–2015). BMC Health Serv Res. 2016;16(1):1–5.
Foa EB, Kozak MJ, Salkovskis PM, Coles ME, Amir N. The validation of a new obsessive–compulsive disorder scale: The obsessive-compulsive inventory. Psychol Assess. 1998;10(3):206.
Foa EB, Coles M, Huppert JD, Pasupuleti RV, Franklin ME, March J. Development and validation of a child version of the obsessive compulsive inventory. Behav Ther. 2010;41(1):121–32.
Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, Musacchio KM, Jaroszewski AC, Chang BP, Nock MK. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychol Bull. 2017;143(2):187–232.
Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. J Am Med Assoc Int Med. 2020;180:817.
Gambin M, Sękowski M, Woźniak-Prus M, Wnuk A, Oleksy T, Cudo A, Hansen K, Huflejt-Łukasik M, Kubicka K, Łyś AE, Gorgol J, Holas P, Kmita G, Łojek E, Maison D. Generalized anxiety and depressive symptoms in various age groups during the COVID-19 lockdown in Poland specific predictors and differences in symptoms severity. Compr Psychiatry. 2021;105:152222.
Georgiades K. Expanding the evidence for population mental health in Canada: a call to action for evidence-informed policy and practice. Health Promot Chron Dis Prev Canada: Res Policy Pract. 2021;41(11):321.
Georgiades K, Duncan L, Wang L, Comeau J, Boyle MH. Ontario child health study team. six-month prevalence of mental disorders and service contacts among children and youth in ontario: evidence from the ontario child health study. Can J Psychiatry. 2019;64(4):246–55.
Gill EK, McQuillan MT. LGBTQ+ students’ peer victimization and mental health before and during the COVID-19 Pandemic. Int J Environ Res Public Health. 2022;19(18):11537.
Gonzalez M, Zeidan J, Lai J, Yusuf A, Wright N, Steiman M, Karpur A, Shih A, Elsabbagh M, Shikako K. Socio-demographic disparities in receipt of clinical health care services during the COVID-19 pandemic for Canadian children with disability. BMC Health Serv Res. 2022;22(1):1434.
Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Heninger GR, Charney DS. The yale-brown obsessive compulsive scale: i development, use, and reliability. Archiv General Psychiatry. 1989;46(11):1006.
Green A, Price-Feeney M, Dorison S. Implications of COVID-19 for LGBTQ youth mental health and suicide prevention. 2020. https://www.thetrevorproject.org/2020/04/03/implications-of-covid-19-for-lgbtq-youth-mental-health-and-suicide-prevention/.
Guzick AG, Candelari A, Wiese AD, Schneider SC, Goodman WK, Storch EA. Obsessive–compulsive disorder during the COVID-19 pandemic: a systematic review. Curr Psychiatry Rep. 2021;23(11):1.
Hao F, Tan W, Jiang LI, Zhang L, Zhao X, Zou Y, Hu Y, Luo X, Jiang X, McIntyre RS, Tran B. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. 2020;1(87):100–6.
Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, Ballard C, Christensen H, Silver RC, Everall I, Ford T. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. The Lancet Psychiatry. 2020;7(6):547–60.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Kunzler AM, Röthke N, Günthner L, Stoffers-Winterling J, Tüscher O, Coenen M, Rehfuess E, Schwarzer G, Binder H, Schmucker C, Meerpohl JJ, Lieb K. Mental burden and its risk and protective factors during the early phase of the SARS-CoV-2 pandemic: systematic review and meta-analyses. Global Health. 2021;17(1):34.
Lau BHP, Cheung MKT, Chan LTH, Chan CLW, Leung PPY. Resilience in the storm: impacts of changed daily lifestyles on mental health in persons with chronic illnesses under the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(11):5875.
Lee CM, Cadigan JM, Rhew IC. Increases in loneliness among young adults during the COVID-19 pandemic and association with increases in mental health problems. J Adolesc Health. 2020;67(5):714–7.
Levis B, Benedetti A, Thombs BD. Accuracy of patient health questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. Bmj. 2019. https://doi.org/10.1136/bmj.l1476.
Linde ES, Varga TV, Clotworthy A. Obsessive-compulsive disorder during the COVID-19 pandemic-a systematic review. Front Psychiatry. 2022;13:806872. https://doi.org/10.3389/fpsyt.2022.806872.
McElroy-Heltzel SE, Shannonhouse LR, Davis EB, Lemke AW, Mize MC, Aten J, Fullen MC, Hook JN, Van Tongeren DR, Davis DE, Miskis C. Resource loss and mental health during COVID-19: Psychosocial protective factors among US older adults and those with chronic disease. Int J Psychol. 2022;57(1):127–35.
Mossman SA, Luft MJ, Schroeder HK, Varney ST, Fleck DE, Barzman DH, Gilman R, DelBello MP, Strawn JR. The generalized anxiety disorder 7-item (GAD-7) scale in adolescents with generalized anxiety disorder: signal detection and validation. Ann Clin Psychiatry Off J Am Acade Clin Psychiatrists. 2017;29(4):227.
Nochaiwong S, Ruengorn C, Thavorn K, Hutton B, Awiphan R, Phosuya C, Ruanta Y, Wongpakaran N, Wongpakaran T. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis. Sci Rep. 2021;11(1):10173.
Nock MK, Hwang I, Sampson N, Kessler RC, Angermeyer M, Beautrais A, Borges G, Bromet E, Bruffaerts R, de Girolamo G, de Graaf R, Florescu S, Gureje O, Haro JM, Hu C, Huang Y, Karam EG, Kawakami N, Kovess V, Levinson D, Posada-Villa J, Sagar R, Tomov T, Viana MC, Williams DR. Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS Med. 2009;6(8):e1000123. https://doi.org/10.1371/journal.pmed.1000123.
Nguyen T, Embrett MG, Barr NG, Mulvale GM, Vania DK, Randall GE, DiRezze B. Preventing youth from falling through the cracks between child/adolescent and adult mental health services: a systematic review of models of care. Commun Ment Health J. 2017;53(4):375–82.
Novins DK, Stoddard J, Althoff RR, Charach A, Cortese S, Cullen KR, Frazier JA, Glatt SJ, Henderson SW, Herringa RJ, Hulvershorn L. Editors’ note and special communication: research priorities in child and adolescent mental health emerging from the COVID-19 pandemic. J Am Acad Child Adolesc Psychiatry. 2021;60(5):544–54.
Nwachukwu I, Nkire N, Shalaby R, Hrabok M, Vuong W, Gusnowski A, Surood S, Urichuk L, Greenshaw AJ, Agyapong VI. COVID-19 pandemic: age-related differences in measures of stress, anxiety and depression in Canada. Int J Environ Res Public Health. 2020;17(17):6366.
Pearson C, Janz T, Ali J. Mental and substance use disorders in Canada. Health at a Glance. Statistics Canada Catalogue no. 82–624-X. Released September 2013. https://www150.statcan.gc.ca/n1/en/pub/82-624-x/2013001/article/11855-eng.pdf?st=KNqDHImh
Pierce M, McManus S, Jessop C, John A, Hotopf M, Ford T, Hatch S, Wessely S, Abel KM. Says who? The significance of sampling in mental health surveys during COVID-19. Lancet Psychiatry. 2020;7(7):567–8.
Polsky JY, Gilmour H. Food insecurity and mental health during the COVID-19 pandemic. Health Rep. 2020;31(12):3–11.
Prokopenko E, Kevins C. Vulnerabilities related to COVID-19 among LGBTQ2+ Canadians. Statistics Canada. 2020. https://www150.statcan.gc.ca/n1/pub/45-28-0001/2020001/article/00075-eng.htm
Richardson LP, McCauley E, Grossman DC, McCarty CA, Richards J, Russo JE, Rockhill C, Katon W. Evaluation of the patient health questionnaire-9 item for detecting major depression among adolescents. Pediatrics. 2010;126(6):1117–23.
Rizeq J, Korczak DJ, Cost KT, Anagnostou E, Charach A, Monga S, Birken CS, Kelley E, Nicolson R, Burton CL, Crosbie J. Vulnerability pathways to mental health outcomes in children and parents during COVID-19. Curr Psychol. 2021;19:1–1.
Rubin DB. The calculation of posterior distributions by data augmentation: comment: a noniterative sampling/importance resampling alternative to the data augmentation algorithm for creating a few imputations when fractions of missing information are modest: The SIR algorithm. J Am Stat Assoc. 1987;82(398):543–6.
Rutherford L, Stark A, Ablona A, Klassen BJ, Higgins R, Jacobsen H, Draenos CJ, Card KG, Lachowsky NJ. Health and well-being of trans and non-binary participants in a community-based survey of gay, bisexual, and queer men, and non-binary and Two-Spirit people across Canada. PLoS ONE. 2021;16(2): e0246525.
Salerno JP, Williams ND, Gattamorta KA. LGBTQ populations: psychologically vulnerable communities in the COVID-19 pandemic. Psychol Trauma. 2020;12(S1):S239–42.
Samji H, Wu J, Ladak A, Vossen C, Stewart E, Dove N, Long D, Snell G. Mental health impacts of the COVID-19 pandemic on children and youth–a systematic review. Child Adolesc Mental Health. 2022;27(2):173–89.
Scahill L, Riddle MA, McSwiggin-Hardin M, Ort SI, King RA, Goodman WK, Cicchetti D, Leckman JF. Children’s yale-brown obsessive compulsive scale: reliability and validity. J Am Acad Child Adolesc Psychiatry. 1997;36(6):844–52.
Signorini G, Singh SP, Marsanic VB, Dieleman G, Dodig-Ćurković K, Franic T, Gerritsen SE, Griffin J, Maras A, McNicholas F, O’Hara L, Purper-Ouakil D, Paul M, Russet F, Santosh P, Schulze U, Street C, Tremmery S, Tuomainen H, Verhulst F, Warwick J, de Girolamo G. The interface between child/adolescent and adult mental health services: results from a European 28-country survey. Eur Child Adolesc Psychiatry. 2018;27(4):501–11.
Solmi F, Downs JL, Nicholls DE. COVID-19 and eating disorders in young people. Lancet Child Adolesc Health. 2021;5:316–8.
Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Suen YT, Chan RCH, Wong EMY. Effects of general and sexual minority-specific COVID-19-related stressors on the mental health of lesbian, gay, and bisexual people in Hong Kong. Psychiatry Res. 2020;292: 113365.
Sunderland A, Findlay LC. Perceived need for mental health care in Canada: results from the 2012 Canadian Community Health Survey-Mental Health. Statistics Canada. 2015. https://www150.statcan.gc.ca/n1/pub/82-003-x/2013009/article/11863-eng.htm
Tami A, Ferguson T, Bauer GR, Scheim AI. Avoidance of primary healthcare among transgender and non-binary people in Canada during the COVID-19 pandemic. Prev Med Rep. 2022;27: 101789.
UNESCO. Education: from school closure to recovery | UNESCO. 2021.
Urbanoski K, Inglis D, Veldhuizen S. Service use and unmet needs for substance use and mental disorders in Canada. Can J Psychiatry. 2017;62(8):551–9.
Vaillancourt T, Szatmari P, Georgiades K, Krygsman A. The impact of COVID-19 on the mental health of Canadian children and youth. Facets. 2021;6(1):1628–48.
Van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;12(45):1–67.
Varma P, Junge M, Meaklim H, Jackson ML. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: a global cross-sectional survey. Prog Neuropsychopharmacol Biol Psychiatry. 2021;13(109): 110236.
Waddell C, Georgiades K, Duncan L, Comeau J, Reid GJ, O’Briain W, Lampard R, Boyle MH, Ontario Child Health Study Team. Ontario child health study findings: policy implications for Canada. Can J Psychiatry. 2014;64(4):227–31.
Westwell-Roper C, Stewart E. Health Inequities Facing Children Vulnerable to Mental Health Challenge. In: Supporting Children and Their Families Facing Health Inequities in Canada. Essay, University of Toronto Press, Scholarly Publishing Division, 2021.
Wittgens C, Fischer MM, Buspavanich P, Theobald S, Schweizer K, Trautmann S. Mental health in people with minority sexual orientations: a meta-analysis of population-based studies. Acta Psychiatr Scand. 2022;145(4):357–72.
Wolfson JA, Garcia T, Leung CW. Food insecurity is associated with depression, anxiety, and stress: evidence from the early days of the COVID-19 pandemic in the United States. Health Equity. 2021;5(1):64–71.
World Health Organization. Calouste Gulbenkian Foundation (2014) Social determinants of mental health. Geneva: World Health Organization; 2007.
World Health Organization Secretariat. Risks to mental health: an overview of vulnerabilities and risk factors—Background paper by WHO secretariat for the development of a comprehensive mental health action plan. World Health Organization; 2012.
Zalsman G, Stanley B, Szanto K, Clarke DE, Carli V, Mehlum L. Suicide in the time of COVID-19: review and recommendations. Arch Suicide Res. 2020;24(4):477–82.
Acknowledgements
We gratefully acknowledge support from the multitude of organizations whose input enabled this study’s design and recruitment. These include: Anxiety Canada, British Columbia Association of Aboriginal Friendship Centres, British Columbia Centre for Disease Control, British Columbia Ministry of Children and Family Development, British Columbia Ministry of Health, British Columbia Ministry of Mental Health and Addictions, Family Support Institute of British Columbia, Inclusion British Columbia, Metis Nation British Columbia, The Responsive Intersectoral Children's Health, Education, and Research Initiative and YWCA Metro Vancouver. Specifically, we would like to thank the following individuals: Jehannine Austin, Andrea Chapman, Amrit Dhariwal, Diana Franco Yamin, Ashley Miller, Kimberly Miller, Kishore Mulpuri, Carly Parsons and Tamara Vanderwal.
Funding
This work was financially supported by the British Columbia Children’s Hospital Foundation (collection, analysis, interpretation of data and manuscript preparation), the British Columbia Ministry of Health (data collection), the British Columbia Centre for Disease Control (data collection) and the Canadian Institutes for Health Research (analysis and interpretation of data).
Author information
Authors and Affiliations
Contributions
SES and HS contributed to study oversight, design, data analysis, interpretation and manuscript preparation. JB and RS contributed to study design, data analysis and interpretation and manuscript preparation. ZN, BL, CL and AA contributed to study design and data collection. CWR contributed to study design, data analysis and interpretation and manuscript preparation. GS contributed to data analysis. TV, EE and KD contributed to study design and data interpretation. QD contributed to study design and manuscript preparation. All authors read and approved the final manuscript.
Authors’ information
SES and HS partnered to design and complete this work. SES is a Professor of Psychiatry, child and adolescent psychiatrist and researcher at UBC, medical director of clinical mental health research at the British Columbia Children’s Hospital and director of the Brain, Behaviour and Development theme at the British Columbia Children’s Hospital Research Institute. HS is an epidemiologist at British Columbia Centre for Disease Control and Assistant Professor at Simon Fraser University. JB is a biostatistician with expertise in mental health research.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the University of British Columbia Children and Women’s Research Ethics Board.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
CHERRIES Checklist.
Additional file 2: Figure S1.
Study Recruitment Relative to COVID-19 Waves in Canada.
Additional file 3: Table S2.
Detailed characteristics of participants and Canadian reference samples.
Additional file 4: Table S3.
Age-group specific rates of current GAD, depression, OCD as reported at baseline in PICS Sample and in Canadian (Cdn) pre-pandemic reference samples.
Additional file 5: Document 1.
Study Protocol.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Stewart, S.E., Best, J., Selles, R. et al. Age-specific determinants of psychiatric outcomes after the first COVID-19 wave: baseline findings from a Canadian online cohort study. Child Adolesc Psychiatry Ment Health 17, 20 (2023). https://doi.org/10.1186/s13034-023-00560-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13034-023-00560-8