Abstract
Background
In the state of Victoria, Australia, the 111-day lockdown due to the COVID-19 pandemic exacerbated the population’s prevailing state of poor mental health. Of the 87% of Australians who visit their GP annually, 71% of health problems they discussed related to psychological issues. This review had two objectives: (1) To describe models of mental health integrated care within primary care settings that demonstrated improved mental health outcomes that were transferable to Australian settings, and (2) To outline the factors that contributed to the effective implementation of these models into routine practice.
Methods
A scoping review was undertaken to synthesise the evidence in order to inform practice, policymaking, and research. Data were obtained from PubMed, CINAHL and APA PsycINFO.
Results
Key elements of effective mental health integrated care models in primary care are: Co-location of mental health and substance abuse services in the primary care setting, presence of licensed mental health clinicians, a case management approach to patient care, ongoing depression monitoring for up to 24 months and other miscellaneous elements. Key factors that contributed to the effective implementation of mental health integrated care in routine practice are the willingness to accept and promote system change, integrated physical and mental clinical records, the presence of a care manager, adequate staff training, a healthy organisational culture, regular supervision and support, a standardised workflow plan and care pathways that included clear role boundaries and the use of outcome measures. The need to develop sustainable funding mechanisms has also been emphasized.
Conclusion
Integrated mental health care models typically have a co-located mental health clinician who works closely with the GP and the rest of the primary care team. Implementing mental health integrated care models in Australia requires a ‘whole of system’ change. Lessons learned from the Mental Health Nurse Incentive Program could form the foundation on which this model is implemented in Australia.
Similar content being viewed by others
Background
Mental disorders are among the most important public health problems in Australia. According to the Productivity Commission [1], over 23% of the population (5.9M) are at risk of developing a mental health problem. Persons with mental disorders also have a high rate of comorbidity, including psychological, social and physical problems [2]. In most developed countries, the first point of contact for individuals seeking healthcare is the general practitioner [GP].
More than 87% of the Australian population visit their GP every year [3]. The Royal Australian College of General Practitioners reports that 71% of the health problems discussed with GPs relate to psychological issues [4]. GPs also report that they are concerned about successfully managing patients’ mental health problems into the future [4]. Considering the burden of mental health problems encountered by GPs and the need to also manage co-morbidities in patients, an integrated approach to treatment is required. This approach needs collaboration between different health care specialists, health and community workers and agencies [5].
In the state of Victoria, Australia, mental health services have been reported to be fragmented and not fit for purpose thereby leaving a large group of individuals with an unmet need for services [6]. The COVID-19 pandemic exacerbated the poor state of mental health in the population when the state went into a 111-day lockdown [7]. The Royal Commission into Victoria's Mental Health System recommended that the system needed to be adaptive so that it ‘can identify and test new ideas, gather evidence about what works, and translate this into effective treatment, care and support’ [6]. The Commission envisaged that collaboration and communication occur between services within and beyond the mental health system and that continuing research, evaluation and innovation be used to respond to community needs [6]. As a response to the recommendations of the Royal Commission and the importance of general practitioners in primary mental health care, it is worth exploring mental health service models that involve general practitioners.
Collaborative care [CC]
Over two decades ago, Michael Von Korff and David Goldberg argued that efforts to improve primary care of depression needed to focus on low cost case management dovetailed with accessible working relationships between the primary care doctor, the case manager and a mental health specialist [8]. The concept of multidisciplinary teams in primary care came to be referred to as a collaborative care model [CCM] and typically consisted of a multi-professional approach to patient care, a structured management plan, pharmacological and non-pharmacological interventions, scheduled patient follow-ups and enhanced inter-professional communication [9]. A systematic review in 2012 showed that CCMs could improve mental and physical outcomes for individuals with mental disorders and they provide a robust clinical and policy framework for care integration [10]. There have since been increased calls for this evidence to be translated into practice [11, 12].
The evidence for effective models of care for substance use disorders continues to be developed. For instance, the Washington State Hub and Spoke Model that incorporates primary care and substance use treatment programs, as well as outreach and referral has shown promise [13]. However, a systematic review of the effectiveness of models of care for the management of Alcohol Use Disorder in primary health care settings found that outcomes were mixed and that further research on the types and components of models was necessary [14].
Care coordination is a related recovery-oriented service delivery model that has been found to be effective in reducing unmet needs for persons with severe mental health problems [15]. It is built on the evidence that persons with severe and complex mental illness have multiple and complex needs related to accommodation, food, physical health problems, transport, childcare, etc. [16, 17]. It involves working with individuals to first identify and prioritize their needs, then liaising with multiple service providers to develop a care plan, and finally facilitating the provision of services according to that plan to meet clients’ needs [15]. This model considers the consumer as a whole including their culture, their family and carers as well as the community in which they live [18]. As a consumer-driven and co-designed model, it is meant to empower consumers and their carers in obtaining the best available care. National guidelines on coordinated care for persons with severe and complex mental illness have been published by the Australian government [18].
Integrated care
Integrated care is different from CC. While CC refers to multiple professions working closely together in the delivery of care, in integrated care, the different professions are subsumed into a single organisational framework . Therefore, collaboration is a precondition for integration but collaboration does not require integration [19]. The literature on Integrated care for persons with mental illness is fast gaining traction [20]. According to a position paper by the American College of Physicians most integrated care models in the primary care setting fall into two major categories: the Collaborative Care Model (CCM), originally developed for the treatment of depression in primary care, and the Screening, Brief Intervention, Referral to Treatment (SBIRT) model for alcohol and substance use disorders (ASUD) [21]. Most other integrated models build on these two models. While the evidence on the effectiveness of the CCM has been demonstrated, effectiveness studies of the SBIRT have been less encouraging [22].
General practice in Australia
In Australia, general practices have traditionally been smaller, private, single or two GP practices that provide comprehensive and continuing medical care. However, of late, they have started to become more corporatized [23]. The latest available data shows that there are 8147 general practices in Australia [24]. Nationally, the average number of full-time GPs is 117.7 per 100,000 population [25], the majority of whom work in group practices (82%) [26]. Currently, a majority (91%) of practices have practice nurses, 57% have allied health professionals and 23% have other specialists [26].
Females tend to see their GP more often than males, and older people visit their GP more regularly than younger people [26]. Patients speak highly of their GPs with 90% and over reporting that their GP always or often spends enough time with them and always or often shows respect, and listens carefully [26].
Primary health care and integrated care are a beneficial match. Valentijn et al. argue that by virtue of being continuous, comprehensive, and coordinated, primary health care is inherently integrated [27]. However, despite the known potential of these models of care, integrating mental (used interchangeably with behavioural) health care within the primary care setting has been fraught with challenges at the patient, provider and system level [28, 29]. Kates et al. argue that the different models themselves are not as important as the principles that underpin integrated care, and these principles can be translated to different settings [12].
This review focused on integrated care models that can feasibly be implemented in the Australian primary care setting, although the findings might have implications for other developed countries with similar primary care structures. The findings of this review can be used to support a consultative, evidence-based approach to commissioning, program design and implementation of primary mental health integrated care models.
Method
A scoping review was undertaken since it is a method of evidence synthesis used to ‘map the literature on a particular topic or research area and provides an opportunity to identify key concepts, gaps in the research, and types and sources of evidence to inform practice, policymaking, and research’ [30]. The Joanna Briggs Institute [JBI] methodological framework for scoping reviews was adopted [31, 32]. JBI is an international organisation that promotes and supports evidence-based decisions to improve health and health service delivery.
Aims of the review
The aims of this review were twofold:
-
1.
To describe the models of integrated care including care coordination within a primary care setting that have demonstrated evidence of a positive effect on improving: mental health and wellbeing, substance abuse.
-
2.
To identify factors contributing to the effective implementation of integrated care models within primary care that are relevant to the Australian setting.
Inclusion criteria
The inclusion criteria have been categorised under the three headings of participants, concept and context as per the JBI guidelines [31, 32].
Participants
Participants in included studies were persons with mental health problems, typically common mental disorders such as depression and anxiety. No restrictions were placed on age or gender of participants since the focus was to identify effective models of integrated care in the primary care setting.
Concept
The main concept of this scoping review relates to models of integrated mental health care including care coordination models that have shown benefit in improving mental health and wellbeing and substance abuse. With a view to trialling such models, commissioning agencies are also interested in identifying the factors contributing to their effective implementation such as funding and infrastructure, service access and intake, workforce, technology, research, evaluation and performance monitoring, lived experience engagement, governance; and partnerships.
Context
The context of this review includes primary care settings in developed countries that are comparable to the Australian setting. Dates for the search were customised from 1st January 2000 to 7th June 2023 since some of the early publications of collaborative care were after year 2000 [8]. Language was restricted to English for convenience. Inclusion and exclusion criteria are given in Table 1.
Search strategy
The search strategy was organised around the three concepts of Primary health care, Integrated care models/care coordination and Mental disorders. MeSH terms and keywords were chosen and piloted in PubMed. Articles identified through this process were assessed to further refine the search strategy. Search terms and keywords within each concept were combined using the Boolean operator ‘OR’ and across components using ‘AND’. The master search was designed and finalised in PubMed. The searches were then converted and executed in CINAHL and APA PsycINFO databases as described in Box 1.
Study selection
All references were imported to Covidence for screening and study selection. Duplicates were then removed.
Title and abstract screening
Following discussions on screening protocols, title and abstract screening was performed independently by two reviewers [AI and EM] and conflicts were resolved following discussion.
Full-text screening
Full text screening was also undertaken independently by two reviewers. The lead author reviewed the excluded papers a second time. We excluded reports from Veteran’s Affairs settings in the USA because they are typically large clinics with multiple professionals working under a single roof, whereas Australia has smaller practices with one or more GPs assisted by one or two nurses and administrative staff.
Data extraction
Reports were forwarded for data extraction following full text reviews. Only those that reported on effective mental health integrated care models in primary care settings or factors that contributed to their effectiveness were included.
Data collation and synthesis
Studies identified in the review were divided into two groups. Experimental studies (RCTs) and systematic reviews of experimental studies that reported on effective mental health integrated care models in primary care settings were included in Group 1. Group 2 included reviews of characteristics of organisations that have achieved mental health integrated care mechanisms in primary care, facilitators and barriers for implementing this integration as well as recent advances on how to establish such models in routine care. Findings from group 1 and group 2 studies were then extracted separately into tables and synthesised as follows.
-
1.
Elements of mental health integrated care models in primary care settings that have shown improvement in patient outcomes
-
2.
Key factors that contribute to the effective implementation of such models that are relevant to the Australian primary care setting.
Results
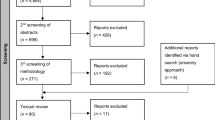
One thousand three hundred and eighty-seven studies were identified in the search. Twelve papers were selected for the review. They included 2 randomised controlled trials, 2 cluster randomised controlled trails, one systematic review of randomised controlled trials, 2 systematic reviews, one systematic review of interviews with service providers, 2 integrative reviews, one narrative review and one site specific analysis. Six studies were based in the USA, 2 in the UK and one each in Australia, Netherlands, Germany and China. The report from China was included because it reviewed models from around the world rather than from low- and middle-income countries. Figure 1 shows the PRISMA flowchart for selection of reports for this review.
Elements of mental health integrated care models in primary care (Group 1)
Six studies described mental health integrated care models in primary care settings that showed improvement in patient outcomes [33,34,35,36,37,38]. Characteristics of each model studied and their reported outcomes are given in Table 2. Outcomes reported by these studies primarily include better engagement of patients with mental health and substance abuse services [33, 34] and better clinical and functional outcomes [35, 36]. Key elements of effective mental health integrated care models in primary care are given below.
Co-location: Mental health and substance abuse services were co-located in the primary care setting (including assessment, care planning, counselling, case management, psychotherapy, and pharmacological treatment), with no distinction in terms of signage or clinic names [33,34,35].
Licensed mental health clinicians: Mental health and substance abuse services were provided by licensed mental health/substance abuse providers (including social workers, psychologists, psychiatric nurses, psychiatrists, and master’s-level counsellors) [33, 34] although in one study, trained health care assistants (HCA) provided case management [36]. In addition to having a licensed mental health practitioner on site, some models had visiting or liaison psychiatrists particularly when patients presented with complex conditions [35, 37, 38].
Case management: A case management approach where proactive support was provided for the patient by the entire practice team was evident. This required communication between mental health and substance abuse clinician and primary care provider about the clinical evaluation and treatment plan [33, 34] or between the case manager and general practitioner [36]. It also required regular cross appointments [33, 34].
Ongoing depression monitoring: Patients were typically monitored every 2 weeks during the acute phase of treatment and then monthly for 1 year after stabilization of depression as per the Agency for Health Care Policy and Research guidelines for the treatment of depression in primary care [35]. In the study by Gensichen, and colleagues [36] HCAs contacted their patients by telephone twice a week in the first month and then once a month for the following 11 months. They monitored depression symptoms and adherence to medication by using the Depression Monitoring List. In other studies, patients received proactive depression treatment in primary care for 12 months and were followed up for 12 or 24 months [38].
Miscellaneous: There were other elements that were part of individual studies such as patient education in the form of video and written information [35], encouragement to take part in self-management activities, such as medication adherence and pleasant or social activities [36], adopting a standard treatment intervention such as the Problem Solving Treatment [37] or the use of a web-based patient tracking system with stepwise algorithm to monitor medication adherence and patient progress [37].
Factors that contributed to the effective implementation of mental health integrated care in primary care settings (Group 2)
Six reports explored factors that contributed to the effectiveness of mental health integrated care models in primary care settings [22, 39,40,41,42,43]. Characteristics and findings of each study are given in Table 3. Key factors that contributed to the effective implementation of mental health integrated care are described below.
Willingness to accept and promote system change
General practices need to be willing to accept and promote system change [41, 44]. It is important for GPs to recognize the benefits of the model [36, 41] and have shared values with staff [42]. This is possible when there are individuals with deep institutional vision such as influential supporters of general practices (e.g. political and other leaders) [40]. Such individuals can serve as champions to encourage GPs to refer their patients with depression to the care manager [41, 45] or facilitate integration and address any confusion, thus benefiting the organization [40, 43, 46]. Higher-level agencies can also provide practices with strong support for system change [40].
Presence of a care manager
Having a care manager on site and who is easily accessible was significantly correlated with activating patients into the program [41, 45].
Adequate training
Adequate staff training, specifically in mental health, is crucial for caring for patients with mental illnesses [42, 43]. Cross-training between the primary care and the behavioural staff was found to be beneficial in preparing staff and increasing empathy towards patients [43, 46].
Standardised workflow plan and care pathways
Clinics that developed a protocol for mental health screening and followed a standardized work flow plan, including a plan for transitioning between different care groups, managed to better engage in the care of mentally ill patients [22, 41, 43, 47]. In addition, clear role boundaries where the mental health clinician was not perceived as taking over the patient's depression care (e.g. GP decided when to change the dosage or type of medication) [41, 48], scheduled follow-up appointments for continuing engagement [41, 44] and the use of outcome measures such as the Patient Health Questionnaire-9 were found to enable the implementation of mental health integrated care. The PHQ-9 is a validated and widely used screening tool for depression in primary care [49]. It is the most accepted outcome measure by GPs, which gives them confidence in their ability to provide high quality depression care [41, 50].
Consolidated physical and mental clinical records
Integrated electronic health records showed potential to expand patient care beyond the traditional primary care setting by integrating medical and mental health information streams with telehealth, social services, etc. [22].
The ability to share electronic medical records was also found to contribute to effectiveness of the model [41, 42, 47].
Healthy organisational culture
A good relationship between the medical and the mental health care providers is vital to promote collaboration between the disciplines. This often took the form of ‘interdisciplinary huddles’ or daily catch-ups to discuss new patients and issues from the previous day [43]. Effective communication between service providers which was either written, verbal, formal or informal contributed to the healthy environment and smooth running of the model of care [42]. Similarly, organisational culture was enhanced when staff had the ability to step outside of their prescribed roles and work creatively [42] but at the same time had role clarity and accountability [42].
Regular supervision and support
Regular and ongoing supervision and support is considered to maintain morale and motivation [41, 51]. Support and supervision could be in the form of regular site visits and addressing implementation challenges [41, 52]. However, this required a good relationship between the leadership and the clinicians and staff [43].
Discussion
This review sought to first describe the models of integrated care within a primary care setting that have demonstrated evidence of a positive effect on improving mental health and wellbeing, and substance abuse challenges and second to identify the factors contributing to their effective implementation. Integrated care models typically have a co-located mental health clinician who works closely with the GP and the rest of the primary care team. Factors that enabled these models to be translated to routine care included, a willingness to accept and promote system change, consolidated physical and mental health records and regular supervision and support.
A scoping review similar to ours was published after our review was completed. The findings of which were broadly similar to ours and included themes related to funding, health practitioner workforce/training, and relationships with initiatives, organizations, and communities [53].
A key finding of this review was that despite integrated care models showing clear evidence of effectiveness in research settings, there continues to be challenges in translating them into routine practice [22, 54]. The services that have succeeded in doing so had the rather unique characteristics of a positive organisational culture and vision [40]. In Australia, integrating mental health care into primary care could work better for larger practices where a business case for this model might prevail. Primary Health Networks, which are agencies that aim to strengthen the primary health care system in Australia, are best placed to lead this change [55].
In countries such as the UK and Australia, the CC model was translated as the Mental Health Nurse Incentive Program [MHNIP], where mental health nurses were co-located at general practices to facilitate access to mental health services [56,57,58,59].
The model had several promising outcomes such as symptom reduction, improved coping and relationships, and enhanced community participation [56, 60]. However, there were challenges with the funding models [61] and in some countries, nurse burnout [62] and retention issues [63]. Nonetheless, this type of model resulted in improvements in integration, clinical effectiveness, patient-centred care, access and efficiency [63]. Mental health nurses continue to be excited about working in primary care, have more autonomy and flexibility in their role and have more time for health promotion [64].
A case has been made for new payment models to be developed that enable implementation of mental health integrated care because effectiveness of these models has thus far been demonstrated mostly with research funding [22]. In Australia, the mainstream mental health system is ‘block funded’ by state governments while primary care is mostly paid for by the Australian Government through fees for service, and medication subsidies [56]. Bringing mental health care into the primary health setting will therefore require a new funding model.
There are several barriers to seeking help for problems related to substance abuse [65]. These include the lack of awareness of the problem, inadequate social support, fear of treatment, privacy concerns, and lack of treatment availability [65]. In addition to these barriers, stigma attached to substance abuse problems and seeking help for it is experienced more intensely by disadvantaged communities [66]. By encapsulating mental health care within the primary care service, integrated care models overcome these barriers [40].
There are a few instances where organisations have included peer workers in their integrated health care service models [67], although how and where they fit into the care model is not yet clear and their effectiveness in improving mental health outcomes in the primary care setting is yet to be proven [68]. Patient-Centered Medical Homes (PCMH) are an improved version of general practices that focus on patient needs rather than just their medical issues [69]. However, this model is a work in progress and has yet to demonstrate effectiveness in managing persons with mental health challenges [70]. Stepped care has been trialled in integrated care settings and has shown to be cost effective [71]. However, this intervention is also in the early stages of development.
Conclusions
Integrated mental health care models typically have a co-located mental health clinician who works closely with the GP and the rest of the primary care team. Implementing mental health integrated care models in Australia requires a ‘whole of system’ change. Lessons learned from the MHNIP could form the foundation on which this model is implemented in Australia.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Productivity Commission. Mental Health, Report no.95. Canberra; 2020.
Mitchell PB, Loo CK, Gould BM. Diagnosis and monitoring of bipolar disorder in general practice. Med J Aust. 2010;193(S4):S10–3.
Department of Health. Annual Medicare statistics: Financial year 1984–85 to 2017–18. Canberra: DoH; 2018. www.health.gov.au/internet/main/publishing.nsf/content/annual-medicare-statistics.
Royal Australian College of General Practitioners. General practice: health of the nation 2022. East Melbourne: RACGP; 2022.
Minkman MMN. The current state of integrated care: an overview. J Integr Care Manag J. 2012;20(6):346–58.
Royal Commission into Victoria's Mental Health System. Royal Commission into Victoria's Mental Health System. Final Report - Summary and Recommendations. Melbourne: RCVMHS; 2021.
Gurvich C, Thomas N, Thomas EH, Hudaib AR, Sood L, Fabiatos K, et al. Coping styles and mental health in response to societal changes during the COVID-19 pandemic. Int J Soc Psychiatry. 2021;67(5):540–9.
Von Korff M, Goldberg D. Improving outcomes in depression. BMJ. 2001;323(7319):948–9.
Gunn J, Diggens J, Hegarty K, Blashki G. A systematic review of complex system interventions designed to increase recovery from depression in primary care. BMC Health Serv Res. 2006;6(1):88.
Woltmann E, Grogan-Kaylor A, Perron B, Georges H, Kilbourne AM, Bauer MS. Comparative effectiveness of collaborative chronic care models for mental health conditions across primary, specialty, and behavioral health care settings: systematic review and meta-analysis. Am J Psychiatry. 2012;169(8):790–804.
Delaney KR, Naegle MA, Valentine NM, Antai-Otong D, Groh CJ, Brennaman L. The effective use of psychiatric mental health nurses in integrated care: policy implications for increasing quality and access to care. J Behav Health Serv Res. 2018;45(2):300–9.
Kates N, Arroll B, Currie E, Hanlon C, Gask L, Klasen H, et al. Improving collaboration between primary care and mental health services. World J Biol Psychiatry. 2019;20(10):748–65.
Reif S, Brolin MF, Stewart MT, Fuchs TJ, Speaker E, Mazel SB. The Washington State Hub and Spoke Model to increase access to medication treatment for opioid use disorders. J Subst Abuse Treat. 2020;108:33–9.
Rombouts SA, Conigrave JH, Saitz R, Louie E, Haber P, Morley KC. Evidence based models of care for the treatment of alcohol use disorder in primary health care settings: a systematic review. BMC Fam Pract. 2020;21(1):260.
Isaacs A, Beauchamp A, Sutton K, Kocaali N. Care coordination can reduce unmet needs of persons with severe and persistent mental illness. Front Psychiatry. 2019;10:563.
Isaacs AN, Beauchamp A, Sutton K, Maybery D. Unmet needs of persons with a severe and persistent mental illness and their relationship to unmet accommodation needs. Health Soc Care Community. 2019;27(4):e246–56.
Isaacs AN, Sutton K, Beauchamp A. Perspectives: recovery oriented services for persons with severe mental illness can focus on meeting needs through care coordination. J Ment Health Policy Econ. 2020;23(2):55–60.
Australian Government Department of Health. National Guidelines to improve coordination of treatment and supports for people with severe and complex mental illness. Canberra: Australian Government; 2022.
Boon HS, Mior SA, Barnsley J, Ashbury FD, Haig R. The difference between integration and collaboration in patient care: results from key informant interviews working in multiprofessional health care teams. J Manip Physiol Ther. 2009;32(9):715–22.
Ee C, Lake J, Firth J, Hargraves F, de Manincor M, Meade T, et al. An integrative collaborative care model for people with mental illness and physical comorbidities. Int J Ment Heal Syst. 2020;14(1):83.
Crowley RA, Kirschner N. The integration of care for mental health, substance abuse, and other behavioral health conditions into primary care: executive summary of an American College of Physicians position paper. Ann Intern Med. 2015;163(4):298–9.
Ramanuj P, Ferenchik E, Docherty M, Spaeth-Rublee B, Pincus HA. Evolving models of integrated behavioral health and primary care. Curr Psychiatry Rep. 2019;21(1):4.
Erny-Albrecht K, Bywood P. Corporatisation of general practice – impact and implications PHCRIS Policy Issue Review. Adelaide: Primary Health Care Research & Information Service; 2016.
Productivity Commission. Report on government services. Canberra; 2020.
Department of Health Australian Government. GP workforce statistics 2014 to 2019. Canberra: Department of Health; 2020.
Royal Australian College of General Practitioners. General Practice: Health of the Nation 2020. East Melbourne: RACGP; 2020.
Valentijn PP, Schepman SM, Opheij W, Bruijnzeels MA. Understanding integrated care: a comprehensive conceptual framework based on the integrative functions of primary care. Int J Integr Care. 2013;13: e010.
Miller BF, Mendenhall TJ, Malik AD. Integrated primary care: an inclusive three-world view through process metrics and empirical discrimination. J Clin Psychol Med Settings. 2009;16(1):21–30.
Thielke S, Vannoy S, Unützer J. Integrating mental health and primary care. Prim Care. 2007;34(3):571–92.
Daudt HM, van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med Res Methodol. 2013;13:48.
Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Implement. 2020;19(1):3–10.
Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141–6.
Ayalon L, Arean PA, Linkins K, Lynch M, Estes CL. Integration of mental health services into primary care overcomes ethnic disparities in access to mental health services between black and white elderly. Am J Geriatr Psychiatry. 2007;15(10):906–12.
Bartels SJ, Coakley EH, Zubritsky C, Ware JH, Miles KM, Arean PA, et al. Improving access to geriatric mental health services: a randomized trial comparing treatment engagement with integrated versus enhanced referral care for depression, anxiety, and at-risk alcohol use. Am J Psychiatry. 2004;161(8):1455–62.
Areán PA, Ayalon L, Hunkeler E, Lin EH, Tang L, Harpole L, et al. Improving depression care for older, minority patients in primary care. Med Care. 2005;43(4):381–90.
Gensichen J, von Korff M, Peitz M, Muth C, Beyer M, Guthlin C, et al. Case management for depression by health care assistants in small primary care practices: a cluster randomized trial. Ann Intern Med. 2009;151(6):369–78.
Huijbregts KM, de Jong FJ, van Marwijk HW, Beekman AT, Adèr HJ, Hakkaart-van Roijen L, et al. A target-driven collaborative care model for Major Depressive Disorder is effective in primary care in the Netherlands. A randomized clinical trial from the depression initiative. J Affect Disord. 2013;146(3):328–37.
Chang-Quan H, Bi-Rong D, Zhen-Chan L, Yuan Z, Yu-Sheng P, Qing-Xiu L. Collaborative care interventions for depression in the elderly: a systematic review of randomized controlled trials. J Investig Med. 2009;57(2):446–55.
Martin MP, White MB, Hodgson JL, Lamson AL, Irons TG. Integrated primary care: a systematic review of program characteristics. Fam Syst Health. 2014;32(1):101–15.
Grazier KL, Smiley ML, Bondalapati KS. Overcoming barriers to integrating behavioral health and primary care services. J Prim Care Community Health. 2016;7(4):242–8.
Wood E, Ohlsen S, Ricketts T. What are the barriers and facilitators to implementing Collaborative Care for depression? A systematic review. J Affect Disord. 2017;214:26–43.
Coates D, Coppleson D, Travaglia J. Factors supporting the implementation of integrated care between physical and mental health services: an integrative review. J Interprof Care. 2022;36(2):245–58.
Peer Y, Koren A. Facilitators and barriers for implementing the integrated behavioural health care model in the USA: an integrative review. Int J Ment Health Nurs. 2022;31(6):1300–14.
Blasinsky M, Goldman HH, Unützer J. Project IMPACT: a report on barriers and facilitators to sustainability. Adm Policy Ment Health Ment Health Serv Res. 2006;33(6):718–29.
Whitebird RR, Solberg LI, Jaeckels NA, Pietruszewski PB, Hadzic S, Unützer J, et al. Effective Implementation of collaborative care for depression: what is needed? Am J Manag Care. 2014;20(9):699–707.
Anastas T, Waddell EN, Howk S, Remiker M, Horton-Dunbar G, Fagnan LJ. Building behavioral health homes: clinician and staff perspectives on creating integrated care teams. J Behav Health Serv Res. 2019;46(3):475–86.
Knowles SE, Chew-Graham C, Coupe N, Adeyemi I, Keyworth C, Thampy H, et al. Better together? A naturalistic qualitative study of inter-professional working in collaborative care for co-morbid depression and physical health problems. Implement Sci. 2013;8:110.
Oishi SM, Shoai R, Katon W, Callahan C, Unützer J, Arean P, et al. Impacting late life depression: integrating a depression intervention into primary care. Psychiatr Q. 2003;74(1):75–89.
Costantini L, Pasquarella C, Odone A, Colucci ME, Costanza A, Serafini G, et al. Screening for depression in primary care with Patient Health Questionnaire-9 (PHQ-9): a systematic review. J Affect Disord. 2021;279:473–83.
Nutting PA, Gallagher KM, Riley K, White S, Dietrich AJ, Dickinson WP. Implementing a depression improvement intervention in five health care organizations: experience from the RESPECT-Depression trial. Adm Policy Ment Health. 2007;34(2):127–37.
Coupe N, Anderson E, Gask L, Sykes P, Richards DA, Chew-Graham C. Facilitating professional liaison in collaborative care for depression in UK primary care; a qualitative study utilising normalisation process theory. BMC Fam Pract. 2014;15(1):78.
Wozniak L, Soprovich A, Rees S, Al Sayah F, Majumdar SR, Johnson JA. Contextualizing the effectiveness of a collaborative care model for primary care patients with diabetes and depression (Teamcare): a qualitative assessment using RE-AIM. Can J Diabetes. 2015;39:S83–91.
Mauer-Vakil DS, Sunderji N, Webb D, Rudoler D, Allin S. Approaches to integrate mental health services in primary care: a scoping review of system-level barriers and enablers to implementation. Can J Community Ment Health. 2023;42(3):29–45.
Grazier KL, Smith JE, Song J, Smiley ML. Integration of depression and primary care: barriers to adoption. J Prim Care Community Health. 2014;5(1):67–73.
Australian government Department of Health. Primary Health Networks Canberra, ACT: Department of Health; 2023. https://www.health.gov.au/initiatives-and-programs/phn.
Lakeman R. Mental health nurses in primary care: qualitative outcomes of the Mental Health Nurse Incentive Program. Int J Ment Health Nurs. 2013;22(5):391–8.
Australian Government Department of Health. Mental Health Nurse Incentive Program guidelines. Canberra: Department of Health; 2016. https://www.semphn.org.au/images/downloads/MHNIP%20The%20National%20MHNIP%20Guidelines.pdf.
Australian Government Departmetn of Health. Mental health nurse incentive program: case studies project report. Canberra: Department of Health; 2010.
Meehan T, Robertson S. Clinical profile of people referred to mental health nurses under the Mental Health Nurse Incentive Program. Int J Ment Health Nurs. 2013;22(5):384–90.
Meehan T, Robertson S. Impact of the mental health nurse incentive programme on patient functioning. Int J Ment Health Nurs. 2015;24(1):75–81.
Lakeman R, Cashin A, Hurley J. Values and valuing mental health nursing in primary care: what is wrong with the ‘before and on behalf of’ model? J Psychiatr Ment Health Nurs. 2014;21(6):526–35.
Duhoux A, Menear M, Charron M, Lavoie-Tremblay M, Alderson M. Interventions to promote or improve the mental health of primary care nurses: a systematic review. J Nurs Manag. 2017;25(8):597–607.
McLeod K, Simpson A. Exploring the value of mental health nurses working in primary care in England: a qualitative study. J Psychiatr Ment Health Nurs. 2017;24(6):387–95.
Olasoji M, Maude P, Cross W. Experiences of mental health nurses working in general practice: a qualitative study. Contemp Nurse. 2020;56(3):266–79.
Rapp RC, Xu J, Carr CA, Lane DT, Wang J, Carlson R. Treatment barriers identified by substance abusers assessed at a centralized intake unit. J Subst Abuse Treat. 2006;30(3):227–35.
Eylem O, de Wit L, van Straten A, Steubl L, Melissourgaki Z, Danışman GT, et al. Stigma for common mental disorders in racial minorities and majorities a systematic review and meta-analysis. BMC Public Health. 2020;20(1):879.
Siantz E, Henwood B, Gilmer T. Implementation of peer providers in integratedmental health and primary care settings. J Soc Soc Work Res. 2016;7(2):231–46.
Gagne CA, Finch WL, Myrick KJ, Davis LM. Peer workers in the behavioral and integrated health workforce: opportunities and future directions. Am J Prev Med. 2018;54(6, Supplement 3):S258–66.
Metusela C, Dijkmans-Hadley B, Mullan J, Gow A, Bonney A. Implementation of a patient centred medical home (PCMH) initiative in general practices in New South Wales, Australia. BMC Fam Pract. 2021;22(1):120.
True A, Janamian T, Dawda P, Johnson T, Smith G. Lessons from the implementation of the Health Care Homes program. Med J Aust. 2022;216(Suppl 10):S19-s21.
Yan C, Rittenbach K, Souri S, Silverstone PH. Cost-effectiveness analysis of a randomized study of depression treatment options in primary care suggests stepped-care treatment may have economic benefits. BMC Psychiatry. 2019;19(1):240.
Acknowledgements
Not applicable.
Funding
This research was funded by the North Western Primary Health Network, Melbourne,
Author information
Authors and Affiliations
Contributions
AI was responsible for the methodology, formal analysis, and preparation of the original draft. EM contributed to data analysis, review and editing. Both authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Isaacs, A.N., Mitchell, E.K.L. Mental health integrated care models in primary care and factors that contribute to their effective implementation: a scoping review. Int J Ment Health Syst 18, 5 (2024). https://doi.org/10.1186/s13033-024-00625-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13033-024-00625-x