Abstract
Background
It is estimated that over 930 million people live in fragile and conflict-affected situations (FCAS) worldwide. These regions, characterized by violence, civil unrest, and war, are often governed by corrupt administrations who are unwilling to provide their citizens with basic human rights. Individuals living in FCAS face health inequities; however, women are disproportionally affected and face additional barriers to accessing sexual and reproductive services, including antenatal care (ANC). This systematic review aims to identify the factors that impact ANC usage in the 37 countries or regions classified as FCAS in 2020 by The World Bank.
Methods
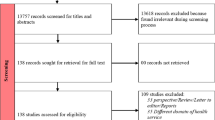
Using the PRISMA guidelines, a systematic search of five databases (SCOPUS, Web of Science, PubMed, EMBASE, and CINAHL) was conducted. Results were limited to human studies, written in English, and published between January 2002 and January 2022. Studies that identified factors affecting utilization of ANC or maternal health services were included for review and critically appraised using the National Institute of Health’s Quality Assessment Tools. Findings were summarized using a narrative synthesis approach.
Results
The database search yielded 26,527 studies. After title, abstract and full-text review, and exclusion of duplicate articles, 121 studies remained. Twenty-eight of the 37 FCAS were represented in the included studies. The studies highlighted that women in FCAS’ are still not meeting the World Health Organization’s 2002 recommendation of four ANC visits during pregnancy, a recommendation which has since been increased to eight visits. The most cited factors impacting ANC were socioeconomic status, education, and poor quality of ANC. Despite all studies being conducted in conflict-affected regions, only nine studies explicitly identified conflict as a direct barrier to accessing ANC.
Conclusion
This review demonstrated that there is a paucity in the literature examining the direct and indirect impacts of conflict on ANC utilization. Specifically, research should be conducted in the nine FCAS that are not currently represented in the literature. To mitigate the barriers that prevent utilization of maternal health services identified in this review, policy makers, women utilizing ANC, and global organizations should attempt to collaborate to enact policy change at the local level.
Similar content being viewed by others
Introduction
As of 2022, it is estimated that over 930 million people live in fragile and conflict-affected situations (FCAS) worldwide and the number of individuals affected by conflict continues to rise [1]. FCAS are countries or regions characterized by a high propensity for recurring conflict or war. FCAS often have unstable and corrupt governments who are unwilling to provide basic resources and protect the human rights of their citizens [2,3,4]. In 2020, the World Bank classified 37 countries as fragile and conflict-affected in their annual list of FCAS.
Conflict presents as one of the world’s most significant threats to health [5]. Individuals living in FCAS suffer worse health on numerous outcomes including trauma and injuries, infectious and chronic disease, mental health, child health, and malnutrition [6]. Women, in particular, are heavily affected by ongoing conflict and violence as they obtain lower levels of education, do not have the autonomy to make decisions regarding their health, and experience abhorrent gender-based violence [7, 8]. In FCAS, women face increased barriers to accessing a continuum of sexual, productive, and maternal health services, including antenatal care (ANC). This has negative impacts on maternal mortality rates (MMR) worldwide [6]. The United Nations created Sustainable Development Goal (SDG) 3.1 in 2015 to reduce the global MMR to less than 70 per 100,000 live births by 2030 [9], from an estimated rate of 211 per 100,000 live births in 2017 [10]. Although the MMR goal outlined in SDG 3.1 is considerably lower than the current global MMR, this difference is even greater when compared to the MMR of FCAS—583 per 100,000 live births as of 2017 [11]. To work towards achieving SDG 3.1, increased attention and interventions are needed to improve maternal health service utilization in FCAS, where the MMR are highest.
ANC has been cited by numerous studies as a type of maternal health service that, if utilized, has the potential to reduce maternal mortality [12,13,14]. ANC is care provided to pregnant women by healthcare practitioners to identify maternal risks, prevent and manage complications, encourage positive health behaviours, and build a therapeutic patient–provider relationship [15]. In 2002, the World Health Organization (WHO) created the first set of ANC recommendations, which consisted of one first trimester visit and three subsequent visits [13]. In 2016, the WHO’s ANC recommendations increased from four total visits to eight [16]. Studies conducted prior this new recommendation in FCAS have found that the majority of women in these regions are not meeting the ANC recommendations established in 2002 [17].
This systematic review is grounded in Andersen’s Model of Healthcare Utilization [18] (Fig. 1). This theoretical framework conceptualizes healthcare utilization as a function of the interaction between predisposing, enabling, and need factors that influence whether women are able to seek ANC as recommended. This model was used to create themes which were found to impact women’s ANC usage and to analyze the data extracted from included articles.
Objectives
FCAS have been previously studied, as have the numerous health outcomes of individuals living in FCAS, including maternal health. However, the common factors that prevent women living in FCAS from accessing ANC have not been well studied. Furthermore, there is a paucity in the literature on the impact of conflict on health equity in FCAS, including the intersectional effect of gender within these situations [2]. This systematic review aims to better understand the access to maternal health services in FCAS and the factors that contribute to the inequitable gap in ANC utilization. For the purposes of this study, ANC will be defined as a visit to a healthcare practitioner to receive services, such as laboratory tests, scans, or advice regarding health behaviours, while pregnant. Visits at the time of childbirth will be excluded. Our specific objectives are to (1) identify the predisposing, enabling, and need factors which prevent and/or enable women living in FCAS from utilizing ANC according to Andersen’s Model of Healthcare Utilization [18]; and (2) identify the effects of persistent conflict on women’s access to and utilization of ANC in the 37 FCAS globally.
Methods
This systematic review was carried out to examine the barriers, facilitators, and overall factors that impact ANC usage in the 37 countries or regions classified as FCAS in 2020 by The World Bank (Fig. 2). A systematic review protocol was developed using the PRISMA checklist and uploaded to the International prospective register of systematic reviews (PROSPERO) on July 10th, 2020 (ID #: CRD42020180994).
Search strategy
A literature search of peer-reviewed articles was conducted using SCOPUS, Web of Science, PubMed, EMBASE, and CINAHL. All five databases were searched on January 11, 2022 using a combination of MeSH terms and keywords (Table 1). The search strategy was created with the help of a subject-specific librarian and adapted to each database. Search results were limited to human studies, written in English, and published between January 2002 and January 2022.
All relevant studies were imported into Covidence, a web-based systematic review software, which identifies and removes duplicates, streamlines screening of citations, and facilitates the resolution of conflicts between reviewers. Two reviewers (B.Z. and K.A.) individually screened all titles, abstracts, and full texts. Disputes were resolved through general discussion with the senior author (I.L) when necessary.
Study inclusion and exclusion criteria
Studies were eligible for inclusion if they were conducted in a conflict-affected region of one of the 37 FCAS. To achieve this, the authors identified medium and high conflict zones within each FCAS, using the Humanitarian Data Exchange or the Armed Conflict Location and Event Data Project. Any studies that took place (1) in a low conflict area of an FCAS without widespread conflict or (2) in an unspecified region of an FCAS, were excluded. Studies that utilized nationwide data, such as the Demographic and Health Surveys (DHS) and Multiple Indicator Cluster Studies (MICS), and took place in FCAS where conflict was not widespread, were excluded. This was done to ensure the data analyzed was focused on conflict-affected populations within FCAS. However, studies that utilized nationwide data were included if the FCAS had widespread conflict, such as Afghanistan. Studies published between January 2002 and January 2022 were eligible for inclusion. The year 2002 was chosen as this was when the WHO released their first set of recommendations for focused and goal-oriented ANC in an attempt to extend antenatal coverage in low- and middle-income countries [15]. Studies that identified barriers or facilitators of ANC use were included in the review. Data from women who were pregnant and had received a minimum of one ANC visit were also included in the review. Regarding study design, both quantitative and qualitative studies were eligible for inclusion. Poster presentations, conference abstracts, theses, and studies for which the full text could not be located were excluded from the review. Studies that only examined skilled birth were excluded as this type of care has been more widely studied in the context of FCAS and is not an outcome of interest in this review.
Data extraction
Two reviewers (B.Z and K.A.) independently extracted data from all included studies. Data extracted included: list of authors, year of publication, study design, methodology employed, geographic setting, patient demographics (i.e., age, marital status), type of care provided (i.e., ANC, skilled birth), factors affecting ANC (i.e., distance, education), outcomes of interest (i.e., number of ANC visits), overall conclusions, limitations, and future recommendations. Data was extracted into a standardized extraction form developed by one of the study authors (B.Z.) using Qualtrics, an online survey platform. All bibliographic information was imported into a reference manager, Zotero, to generate citations.
Quality assessment
Each source was critically appraised using the National Institutes of Health (NIH) Study Quality Assessment Tools [19]. The NIH tool utilized was specific to the study design of the article being reviewed. Studies were evaluated on the clarity of the research question, described eligibility criteria, choice of study population, sample size, outcomes measured, and type of statistical analysis employed. After the assessment, articles rated as either “good”, or “fair” were deemed to have high internal validity and were included in the review. Eight studies were classified as “poor” quality which would have caused them to be excluded, however, they were also excluded for other reasons including wrong geographic location. Discrepancies between reviewers were resolved through general discussion with the senior author (I.L.) when necessary.
Data synthesis
A narrative synthesis approach was employed to analyze the data extracted from all included articles. The factors that were found to affect ANC utilization across all included studies were inductively coded [20] by two independent authors (B.Z and K.A) according to Andersen’s Model of healthcare utilization. Factors were coded as either predisposing, enabling, need or other factor type. To gain cross-study synthesis, the geographic distribution of the studies, participant demographics, and primary outcomes measured were analyzed and the percentage of women who met the ANC recommendations were calculated whenever possible. Due to the inclusion of qualitative studies and of studies with varied designs and methodologies, the data collected was heterogenous and a meta-analysis could not be carried out.
Results
The database search yielded 26,527 studies. After exclusion of 11,029 duplicate articles, and completion of title and abstract screening, a total of 739 studies were included for full text review. After applying inclusion and exclusion criteria, 121 studies were retained for inclusion in the final dataset (Fig. 3). Due to the large number of full-text studies included in this review and the heterogeneity in the designs of the included studies, a thematic description of the results is presented. A description of each article is outlined in the Additional file 1: Table S1.
The geographical spread of the studies included in this systematic review and the number of articles per country is outlined in Fig. 4. The number of articles represented within Fig. 4 exceeds the total number of studies included as some articles examined ANC in multiple countries. Among the 121 articles included, ANC usage was examined in 123 settings: 77 articles in Africa, 15 articles in the Middle East, six articles in Southeast Asia, 11 articles in Central Asia, nine articles in Oceania, three articles in the Caribbean, one article in Palestine, and one article in Europe. Specifically, ANC was examined in 28 of the 37 regions identified as FCAS in 2020 by The World Bank. The nine FCAS for which no relevant studies were found include: Congo (Rep), Liberia, Central African Republic, Comoros, Venezuela, Kiribati, Marshall Islands, Federated States of Micronesia, and Tuvalu. Thirty-two studies analyzed utilization of care in Nigeria, which highlights that ANC has been extensively studied in this country.
The studies included were published between 2002 and 2022, with most articles being published in 2014 or later (Fig. 5). The increasing number of studies over time indicates that research on ANC has been of interest since the Millennium Development Goals and SDGs targets on maternal mortality were established in 2000 and 2015, respectively.
Overall, the studies suggest that booking the first ANC visit late in pregnancy is very common in FCAS [21,22,23,24,25]. Many studies also indicate that while progress has been made, women in FCAS are not meeting the WHO 2002 recommendation of four ANC visits and are therefore not meeting the 2016 recommendation of eight ANC visits [26, 27]. Table 2 identifies the factors that impact use of ANC in the 121 included articles. Seeing that many studies identified multiple factors that impact ANC utilization, the total number of factors highlighted in Table 2 exceeds 121. In accordance with Andersen’s model, predisposing factors include demographic, social, and contextual items such as education, employment, marital status, gender dynamics, religion, and culture [28, 29]. Enabling factors include financial and organizational items such as conflict, structural resources, safety, distance from ANC resources, perceived poor quality of ANC, and socioeconomic status [28, 29]. Additionally, need factors, which indicate a woman’s perceived need for ANC, include parity and previous complications. Finally, factors such as unwanted pregnancies, interventions (i.e., performance-based financing, home visits, mobile phone support and health education), and a husband’s education or employment were categorized as other. The most cited factors impacting ANC were socioeconomic status, poor quality of ANC, and education. Table 2 presents the 20 factors impacting ANC identified in the 121 included articles.
Predisposing
Demographic characteristics
Demographic factors, including level of education, region of residence, marital status, age, religion, and ethnicity were cited 115 times as factors that impact ANC utilization. Education was the second most commonly cited factor that influenced ANC use in 49 studies (Table 2). Generally, women with no education or lower levels of education had decreased awareness and utilization of ANC during the first trimester and were less likely to receive the recommended number of ANC visits [30]. In contrast, women with higher levels of education were significantly more likely to book ANC early in pregnancy and to attend the recommended number of ANC visits [31]. Numerous studies also demonstrated that a husband’s level of education impacted a woman’s ANC usage [30]. It should be noted that this effect was smaller than the impact of a women’s educational attainment.
Region of residence and rurality were found to impact women’s utilization of ANC in 15 articles. The majority of studies found that, when compared to women living in rural areas, women living in urban areas within an FCAS were more likely to receive the recommended number of ANC visits and to have increased uptake of ANC overall [32].
Marital status was reported as a factor that influenced ANC utilization in 14 studies. In general, married women were more likely to use ANC as recommended compared to single women [33, 34]. Specifically, the studies found that being married increased the likelihood of early initiation of ANC [33]. The type of marital union also impacted ANC usage, where women in polygamous marriages were more likely to utilize ANC services [34].
Maternal age was shown to be a factor influencing the timing and frequency of ANC utilization in 14 studies. Most studies, with the exception of Benage et al. [27] and Bashour et al. [35], found that younger women were less likely to seek ANC early in pregnancy, receive the four recommended ANC visits, and use ANC overall [36].
Religion was reported to be a factor influencing ANC utilization in nine studies, however, its impact was context dependent. De Allegri et al. [34], found a negative association between traditional African religions and ANC uptake. Conversely, a study by Nwakamma et al. [37], found that introducing and connecting women to ANC services through faith-based communities and leaders was an important factor in promoting ANC.
Finally, an individual’s employment status was reported to be both a facilitator and barrier to ANC uptake in eight studies. Failing et al. [38], found that women’s employment negatively impacted use of ANC, where women placed more importance on completing work responsibilities to survive financially than on take time off to receiving ANC. According to other studies, using ANC four times, as previously recommended by the WHO, was generally positively associated with women’s employment [17, 39, 40]. Additionally, numerous studies found that a husband’s occupation or employment status (categorized as other) positively influenced women’s maternal healthcare utilization. To illustrate, Abimbola 2016 [30], found that a man’s occupation determines their wife’s socioeconomic status, which is an enabling factor that impacts ANC utilization [26, 38, 41].
Gender dynamics
Gender dynamics, which for the purposes of this study includes autonomy, decision-making abilities, and intimate partner violence, was found to impact ANC use in 26 studies. Women with higher autonomy, specifically financial autonomy, and increased decision-making abilities had greater uptake of ANC [42, 43]. Receiving permission from the husband was cited as an additional barrier to accessing ANC in numerous studies [44,45,46]. Furthermore, women who did not experience intimate partner violence and who did not believe that wife-beating was acceptable were more likely to use ANC and meet the recommendation of four ANC visits [17].
Cultural and health beliefs
Cultural and health beliefs were reported to influence ANC uptake in 22 and 6 studies, respectively (Table 2). Culture was found to shape a woman’s beliefs about ANC and pregnancy, as well as her autonomy to make healthcare decisions [22]. For example, some women believed that their baby would be in danger or that enemies would bewitch them and cause them to miscarry if the pregnancy was disclosed too early, which resulted in late initiation of ANC [22, 47]. Furthermore, in some traditions it is customary for a woman’s mother-in-law to decide whether or not she can receive care [46, 48], which can further decrease ANC utilization. Women’s health beliefs, specifically those who believed that ANC was beneficial, were more likely to use maternal health services compared to those who believed ANC was only for curative purposes. Additionally, many women believed that pregnancy is a natural process and care should only be sought if one becomes ill or develops complications [49, 50]. Therefore, the type of health belief that a woman held regarding the utility of ANC played a role in whether or not they utilized it.
Enabling
Socioeconomic status
Socioeconomic status or financial difficulty was the most cited factor that prevented women from using ANC early and receiving the recommended number of visits. It was reported to influence ANC uptake in 68 of the 121 studies included in this review. The majority of studies found that women with higher socioeconomic status or wealth were more likely to utilize ANC in general, to initiate ANC early in pregnancy, and to receive the four recommended visits [26, 38, 41].
Distance & transport
Distance to the nearest ANC facility was the fourth most commonly cited reason for late or insufficient ANC uptake in 47 studies (Table 2). Women who lived closer to healthcare facilities or perceived the nearest healthcare facility as close to them, had higher levels of ANC usage. Unsurprisingly, those who lived further away from the nearest health facility were less likely to receive four ANC visits, initiate ANC early in their pregnancy, and use ANC overall [51, 52]. Transportation was found to be a barrier of ANC uptake in 14 studies included (Table 2). Telfer et al. found unavailability of transportation to be one of the most important barriers preventing women from accessing ANC. Pregnant women also cited having to walk to the ANC facility and having inadequate modes of transportation (i.e., rickshaws, bicycles, motorbikes) as key barriers to accessing care. The high cost of transportation was also associated with fewer ANC visits and an overall lack of ANC utilization [30, 64].
Poor quality of ANC
Poor Quality of ANC was reported to be a barrier to ANC uptake in 49 studies [53, 59]. Women who believed they received low quality care were less likely to meet the WHO ANC recommendations [42, 60]. Women cited lack of resources (e.g. ultrasound machines, providers etc.) [60,61,62,63], shortened hours of operation [27, 60], long wait times [64], and a lack of trust in providers [65, 66] as reasons for poor quality of care. Women also stated that healthcare providers were incompetent and had negative attitudes [43, 50], which may explain the distrust they experienced [65].
Infrastructure and resources
Infrastructure or lack of resources was a factor reported to impact access to ANC in 11 studies. Studies found that women who perceived operational and infrastructure problems in their community (i.e., lack of electricity, running water, destroyed building infrastructure) were deterred from accessing ANC and faced poorer health outcomes as a result [61, 67]. A study conducted by Mourtada et al. [63], found that as infrastructure destruction increased because of conflict, there was an associated decreased uptake of ANC.
Conflict & safety
Conflict and safety were reported as factors that directly impacted the uptake of ANC in nine and four studies [48, 68,69,70,71,72], respectively. Women in zones of high conflict had poorer rates of ANC utilization. Due to prolonged conflict in FCAS, women felt unsafe or insecure travelling to ANC facilities, especially alone, and were therefore less likely to seek care as recommended [48, 72]. This impact is intersectional as prolonged conflict negatively impacted education, fertility rate, availability of resources (e.g. machinery and providers), quality of care, and infrastructure, which in turn further decreased ANC utilization [48, 68, 69]. Increasing severity of conflict resulted in a decreased number of women in these areas meeting the WHO’s 2016 ANC recommendations. Finally, ANC was negatively impacted by a woman’s proximity to the conflict zone [70].
Need
Parity
Parity, defined as the number of births a woman has had, was shown to be a factor that influenced ANC use in 21 studies. Women who did not have previous birth experience or who had low parity were more likely to initiate ANC early in pregnancy and to attend a greater number of ANC visits [73]. In contrast, women with higher parity were less likely to receive early ANC, attend the recommended number of visits, or meet the WHO’s ANC recommendations [17, 74, 75].
Other
In 49 studies, women’s utilization of ANC was impacted by several other factors (Table 2). One commonly cited other factor was husband’s education and employment, where women whose partners had higher levels of education or formal employment had increased usage of ANC [38]. Unwanted pregnancies [45, 73, 76], stigma from the community or family members [36, 50, 74], community members advising against using formal ANC services [21, 77], use of traditional healers [47, 77], lack of awareness and knowledge [31, 38, 78, 79] and performance-based financing interventions [80, 81] were additional factors associated with delayed and less frequent use of ANC.
Discussion
This review identified 20 factors that impacted ANC utilization across 28 of the 37 regions classified as fragile and conflict-affected by the World Bank in 2020. This is the first review, to our knowledge, that examines ANC utilization in FCAS, exclusively. Overall, the 121 studies included demonstrate that women in FCAS are not meeting the WHO recommendations for ANC use. When compared to women worldwide, those living in FCAS are significantly less likely to seek ANC early in pregnancy or attend a total of four ANC visits, which makes them even less likely to achieve the WHO’s 2016 recommendation of eight ANC visits [82].
Although all 121 studies examined ANC in FCAS, only nine studies (7.43%) identified conflict as a direct barrier to accessing care. We posit that while conflict was not a frequently cited barrier, it may largely explain women’s poor uptake of ANC. For example, in some FCAS, healthcare facilities are attacked, practitioners may be kidnapped, killed, or forced to flee to urban areas to ensure safety, and clinics often lack necessary resources [83]. These events may explain why women experience poor quality of ANC and cannot find care facilities in rural areas [6, 84, 85]. Furthermore, in regions of conflict, women may more often be raped by members of the militia. This leaves women less likely to seek ANC out of fear of experiencing violence when travelling to a healthcare facility alone [86, 87]. This discussion highlights the intersectional relationship between conflict and the four most cited factors impacting ANC [6, 88,89,90], namely education, gender dynamics, socioeconomic status, distance and quality of ANC.
Education was the most commonly cited predisposing factor affecting ANC utilization. Specifically, lack of education resulted in decreased utilization of ANC, which is consistent with literature on maternal healthcare utilization. In FCAS, students and teachers may be killed or displaced due to targeted attacks or recruitment initiatives by military groups [91]. This prevents schools from re-opening and decreases the number of students enrolled should schools reopen [91]. Women are often prematurely forced out of the education system to care for their family after their fathers and brothers are recruited into the military or because of unwanted pregnancies, secondary to rape. Women who are unable to obtain higher levels of education are less likely to know the benefits of ANC or the recommendations regarding timing and frequency of use [12, 82, 88, 92].
Gender dynamics, which encompasses gender-based violence and lack of autonomy, was cited 26 times as a predisposing factor that impacts initiation and frequency of ANC. In conflict-affected areas, the gender dynamics are strained, which puts women at higher risk of experiencing sexual violence and military sexual slavery [93, 94]. Should a woman become pregnant secondary to rape, she must ask for permission and financial support from her husband before seeking out necessary maternal care [12, 96]. Lack of autonomy to make decisions about contraception use [8, 97, 98] may also increase the likelihood of unwanted pregnancies, which is an other factor negatively impacting ANC use [6, 97, 99]. Women who are granted permission to seek ANC may still be unable to access it due to safety concerns associated with transport or lack of infrastructure in regions of high conflict.
Socioeconomic status, an enabling factor, was the most cited factor impacting ANC use. In regions of conflict, employment opportunities are limited, which makes it difficult for women to obtain the financial resources to pay the service and transportation fees associated with ANC. As a result, women may accept employment opportunities that put them at risk of physical and sexual harm, which may cause prenatal complications [95]. Should these women succeed in accessing timely and cost-effective ANC, they may not be able to afford the medications needed to ensure a healthy pregnancy. Women with lower socioeconomic status are also less likely to obtain higher levels of education, have financial autonomy, or be employed [100], which are all known to impact ANC utilization.
Distance was the fourth most commonly cited factor affecting the use of ANC. Distance is commonly thought of as the geographical space between a woman’s home and the nearest health facility [43]. In FCAS, conflict results in displacement of communities and the destruction of roads, transport vehicles and healthcare facilities, which all contribute to the increased distance between residential communities and healthcare facilities [101, 102]. Interestingly, this review found that perceived distance, which is how far a woman believes the nearest ANC facility is to her, also impacted uptake of ANC. Perceived distance is influenced by weather conditions, physical terrain, lack of transportation, and fear of travelling to healthcare facilities alone [8, 103]. Overall, distance, both real and perceived, to the nearest healthcare facility was found to impact ANC utilization and these distances may be increased in regions of conflict.
Poor quality of ANC was the second most commonly cited enabling factor impacting ANC uptake during pregnancy [6, 104]. Women reported experiencing long wait times and receiving care from providers who were unfriendly and “inept” [30]. Conflict directly affects resource allocation and contributes to a lack of providers, equipment, and medical resources, which may explain the poor quality of care [83]. Pregnant women in FCAS are a vulnerable population who are often unaware of the benefits of ANC [38]. When a woman feels she received poor quality ANC, it may reinforce the idea that ANC has little benefit and deter her from seeking it in the future. As such, the shortage of healthcare resources in FCAS as a result of conflict makes it difficult to provide women with high quality care which appears to have negative impacts on ANC utilization.
In order to start addressing the predisposing barriers that women living in FCAS face when seeking ANC, policies must be changed and region-specific interventions are needed. First, policies that prioritize girls’ access to education should be implemented to ensure they can continue with their studies if they become pregnant. Second, educational curricula should be modified to teach students the importance of using contraceptives and seeking ANC. It is also an opportunity to target cultural beliefs that claim use of ANC early in pregnancy can bewitch a child and lead to miscarriage. Third, there is a need to increase the employment opportunities for women. This will allow women to have increased financial autonomy and higher socioeconomic status, which are both positively related to ANC utilization [40]. If girls are educated and women are employed, the gender dynamics that are prevalent in FCAS may also be redefined.
To mitigate enabling factors, governments should provide safe and affordable transportation, cost-effective ANC services, and incentives to ANC providers. Providing transportation will help women feel safer when travelling through regions of conflict to seek ANC. Similarly, subsidizing the costs associated with ANC will help alleviate the financial burdens that women of low socioeconomic status face when seeking care. Performance-based financing schemes, which have been implemented in some FCAS [105], may financially incentivize healthcare workers to provide high quality, patient-centered ANC. It would be important, however, to ensure that a portion of the money practitioners receive is used to hire additional personnel and purchase necessary equipment, which will further ameliorate the quality of care provided.
Addressing the barriers that prevent uptake of ANC will require a grassroots approach and cooperation from several stakeholders, which may be complex, costly, and lengthy. Local policy makers, women utilizing ANC within FCAS, and global organizations, such as the WHO, should collaborate and discuss the local context, the effect of conflict on utilization of ANC, and the factors that impact its uptake. This will maximize the potential to create effective change to increase women’s access to and utilization of ANC in FCAS.
Limitations
This review has some limitations that must be considered. First, we excluded studies not published in English, conducted prior to 2002, and for which the full text could not be accessed. Considering English is not the official language in many of the FCAS analyzed, this review may be missing relevant studies. Second, our search string was created according to the World Bank’s 2020 list of FCAS; however, studies from as early as 2002 are included in this review. As such, some of the analyzed data may have been collected at a time when the region was not classified as fragile and conflict-affected and may not represent the current barriers women in these regions are facing. Third, the included studies are heterogeneous and differ in their study design, sample size, and overall quality, which ultimately prevented us from carrying out a meta-analysis. Furthermore, many studies used self-reported data, which is subject to recall and social desirability biases. Despite these limitations, we used systematic methodologies informed by the PRISMA guidelines to conduct this review and have ensured the quality of the research findings by including studies that were rated as fair or good according to the NIH’s Quality Assessment Tools. Finally, this review does not include studies that utilized nationwide data (i.e., DHS and MICS), which may identify other factors that limit use of ANC. However, elimination of those studies was done to ensure that the data analyzed was specific to conflict-affected populations.
Conclusion
The findings of this systematic review demonstrate that women living in FCAS worldwide face many barriers to accessing ANC. These women are not meeting the WHO 2016 recommendations of eight ANC visits, which is contributing to the high MMR in these regions. Although conflict was not commonly identified as a barrier to accessing maternal health services, it is likely that the frequently cited factors, namely socioeconomic status, distance, education, quality of ANC, and gender dynamics, are exacerbated by the effects of conflict.
Future research
Our findings revealed that research on the factors that affect utilization of ANC is needed in the nine FCAS that are not represented in the included studies. Additionally, it is evident that the direct and indirect impacts of conflict on women’s healthcare utilization have not been well studied. Future research is urgently needed to understand how conflict impacts ANC uptake if we hope to lower the global MMR and achieve SDG 3.1 by 2030.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- ANC:
-
Antenatal care
- FCAS:
-
Fragile and conflict-affected situations
- MMR:
-
Maternal mortality rate
- SDG:
-
Sustainable development goal
- WHO:
-
World Health Organization
References
The World Bank. Population, total—Fragile and conflict affected situations. Published online 2018. https://data.worldbank.org/indicator/SP.POP.TOTL?locations=F1.
Ranson K, Poletti T, Bornemisza O, Sondorp E. Conflict-affected fragile states. Published online 2007.
Bakrania S, Lucas B. The Impact of the financial crisis on conflict and state fragility in sub-Saharan Africa. 2009.
Bertocchi G, Guerzoni A. Growth, history, or institutions: What explains state fragility in sub-Saharan Africa? J Peace Res. 2012;49(6):769–83. https://doi.org/10.1177/0022343312452420.
Singh S, Orbinski JJ, Mills EJ. Conflict and health: a paradigm shift in global health and human rights. Confl Health. 2007;1(1):1. https://doi.org/10.1186/1752-1505-1-1.
Garry S, Checchi F. Armed conflict and public health: into the 21st century. J Public Health. 1990;2019:1–12. https://doi.org/10.1093/pubmed/fdz095.
Bafilemba F, Prendergast J. Congo stories: battling five centuries of exploitation and greed. 2018.
Ziegler BR. Pregnancy in Peril : the impact of conflict on antenatal care and skilled birth attendant utilization in the Democratic Republic of the Congo and Burundi. Published online 2020.
The United Nations. Sustainable development goal. Published online 2015. https://sustainabledevelopment.un.org/sdg3.
World Health Organization. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division: executive summary. World Health Organization; 2019,12 p.
The World Bank. Maternal mortality ratio (modeled estimate, per 100,000 live births). Published online 2017. https://data.worldbank.org/indicator/SH.STA.MMRT.
Atuoye KN, Amoyaw JA, Kuuire VZ, et al. Utilisation of skilled birth attendants over time in Nigeria and Malawi. Glob Public Health. 2017;12(6):728–43. https://doi.org/10.1080/17441692.2017.1315441.
Say L, Chou D, Gemmill A, et al. Global causes of maternal death: A WHO systematic analysis. Lancet Glob Health. 2014;2(6):323–33. https://doi.org/10.1016/S2214-109X(14)70227-X.
The World Health Organization. Maternal mortality. Published online 2019. https://www.who.int/news-room/fact-sheets/detail/maternal-mortality.
The World Health Organization. WHO Antenatal care randomized trial: manual for the implementation of the new model. 2002.
The World Health Organization. WHO Recommendations on antenatal care for a positive pregnancy experience. 2016. https://apps.who.int/iris/bitstream/handle/10665/250796/9789241549912-eng.pdf?sequence=1.
Omer K, Afi NJ, Baba MC, et al. Seeking evidence to support efforts to increase use of antenatal care: a cross-sectional study in two states of Nigeria. BMC Pregnancy Childb. 2014. https://doi.org/10.1186/s12884-014-0380-4.
Andersen RM. Andersen and Newman framework of health services utilization. J Health Soc Behav. 1995;36:1–10. https://doi.org/10.1111/pme.12756.
National Heart Blood and Lung Institute. Study quality assessment tools. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
Neuman WL, Robson K. Basics of social researh. 3rd ed. Toronto: Pearson Canada; 2014.
Warri D, George A. Perceptions of pregnant women of reasons for late initiation of antenatal care: a qualitative interview study. BMC Pregnancy Childb. 2020. https://doi.org/10.1186/s12884-020-2746-0.
Ndidi E, Oseremen I. Reasons given by pregnant women for late initiation of antenatal care in the Niger Delta, Nigeria. Ghana Med J. 2010. https://doi.org/10.4314/gmj.v44i2.68883.
Kluckow H, Panisi L, Larui J, et al. Socio-demographic predictors of unintended pregnancy and late antenatal booking in Honiara, Solomon Islands. Aust N Z J Obstet Gynaecol. 2018;58(3):349–57. https://doi.org/10.1111/ajo.12782.
Ebeigbe PN, Igberase GO. Antenatal care: a comparison of demographic and obstetric characteristics of early and late attenders in the Niger Delta, Nigeria. Med Sci Monit. 2005;11(11):529–32.
Edie GEHE, Obinchemti TE, Tamufor EN, Njie MM, Njamen TN, Achidi EA. Perceptions of antenatal care services by pregnant women attending government health centres in the Buea health district, Cameroon: a cross sectional study. Pan Afr Med J. 2015;21:1–9. https://doi.org/10.11604/pamj.2015.21.45.4858.
Khanal V, da Cruz JLNB, Mishra SR, Karkee R, Lee AH. Under-utilization of antenatal care services in Timor-Leste: results from demographic and health survey 2009–2010. BMC Pregnancy Childb. 2015. https://doi.org/10.1186/s12884-015-0646-5.
Benage M, Gregg Greenough P, Vinck P, Omeira N, Pham P. An assessment of antenatal care among Syrian refugees in Lebanon. Confl Health. 2015. https://doi.org/10.1186/s13031-015-0035-8.
Anderson RM. Revisiting the behavioral model and access to medical care: Does it matter? J Health Soc Behav. 1995;36(1):1–10.
Babitsch B, Gohl D, von Lengerke T. Re-revisiting Andersen’s behavioral model of health services use: a systematic review of studies from 1998–2011. Psycho-Soc Med. 2012. https://doi.org/10.3205/psm000089.
Abimbola JM, Makanjuola AT, Ganiyu SA, Babatunde UMM, Adekunle DK, Olatayo AA. Pattern of utilization of ante-natal and delivery services in a semi-urban community of north-central Nigeria. Afr Health Sci. 2016;16(4):962–71. https://doi.org/10.4314/ahs.v16i4.12.
Adam IF, Nakamura K, Kizuki M, Al Rifai R, Vanching U. Relationship between implementing interpersonal communication and mass education campaigns in emergency settings and use of reproductive healthcare services: Evidence from Darfur, Sudan. BMJ Open. 2015. https://doi.org/10.1136/bmjopen-2015-008285.
Edu BC, Agan TU, Monjok E, Makowiecka K. Effect of free maternal health care program on health-seeking behavior of women during pregnancy, intra-partum and postpartum periods in Cross River State of Nigeria: a mixed method study. Maced J Med Sci. 2017;5(3):370–82. https://doi.org/10.3889/oamjms.2017.075.
Ntambue AM, Malonga FK, Dramaix-Wilmet M, Ngatu RN, Donnen P. Better than nothing? Maternal, newborn, and child health services and perinatal mortality, Lubumbashi, democratic republic of the Congo: a cohort study. BMC Pregnancy Childb. 2016. https://doi.org/10.1186/s12884-016-0879-y.
De Allegri M, Ridde V, Louis VR, et al. Determinants of utilisation of maternal care services after the reduction of user fees: a case study from rural Burkina Faso. Health Policy. 2011;99(3):210–8. https://doi.org/10.1016/j.healthpol.2010.10.010.
Bashour H, Abdulsalam A, Al-Faisal W, Cheikha S. Patterns and determinants of maternity care in Damascus. East Mediterr Health J. 2008;14(3):595–604.
Ebeigbe PN, Gharoro EP. Obstetric complications, intervention rates and maternofetal outcome in teenage nullipara in Benin City, Nigeria. Trop Doct. 2007;37(2):79–83. https://doi.org/10.1258/004947507780609356.
Nwakamma IJ, Erinmwinhe A, Ajogwu A, Udoh A, Ada-Ogoh A. Mitigating gender and maternal and child health injustices through faith community-led initiatives. Int J MCH AIDS. 2019;8(2):146–55. https://doi.org/10.21106/ijma.326.
Failing F, Ripa P, Tefuarani N, Vince J. A comparison of booked and unbooked mothers delivering at the Port Moresby General Hospital: a case-control study. P N G Med J. 2004;47(3–4):174–80.
El-Kak F, Chaaya M, Campbell O, Kaddour A. Patterns of antenatal care in low-versus high-risk pregnancies in Lebanon. East Mediterr Health J. 2004;10(3):268–76.
Oyetundeo and Elery. Factors influecing use of antenatal care and delivery services in Gwagwalada Area Council, Nigeria. Afr J Midwifery Women’s Health. 2014;8(4):195–202.
Alosaimi AN, Nwaru B, Luoto R, Al Serouri AW, Mouniri H. Using household socioeconomic indicators to predict the utilization of maternal and child health services among reproductive-aged women in rural Yemen. Glob Pediatr Health. 2019. https://doi.org/10.1177/2333794X19868926.
Arnaert A, Ponzoni N, Debe Z, Meda MM, Nana NG, Arnaert S. Experiences of women receiving mhealth-supported antenatal care in the village from community health workers in rural Burkina Faso. Africa Digit Health. 2019. https://doi.org/10.1177/2055207619892756.
Al-Mujtaba M, Cornelius LJ, Galadanci H, et al. Evaluating religious influences on the utilization of maternal health services among Muslim and Christian Women in North-Central Nigeria. BIOMED Res Int. 2016. https://doi.org/10.1155/2016/3645415.
Telfer ML, Rowley JT, Walraven GEL. Experiences of mothers with antenatal, delivery and postpartum care in rural Gambia. Afr J Reprod Health. 2002;6(1):74–83. https://doi.org/10.2307/3583148.
Sibanda EL, Bernays S, Weller IVD, Hakim JG, Cowan FM. “Well, not me, but other women do not register because”—Barriers to seeking antenatal care in the context of prevention of mother-to-child transmission of HIV among Zimbabwean women: a mixed-methods study. BMC Pregnancy Childb. 2018. https://doi.org/10.1186/s12884-018-1898-7.
Somé DT, Sombié I, Meda N. How decision for seeking maternal care is made——a qualitative study in two rural medical districts of Burkina Faso. Reprod Health. 2013;10(1):1–6. https://doi.org/10.1186/1742-4755-10-8.
Laing SP, Sinmyee SV, Rafique K, Smith HE, Cooper MJ. Barriers to antenatal care in an urban community in the Gambia: an in-depth qualitative interview study. Afr J Reprod Health. 2017;21(3):62–9.
Wilunda C, Scanagatta C, Putoto G, et al. Barriers to utilisation of antenatal care services in South Sudan: a qualitative study in Rumbek North County. Reprod Health. 2017. https://doi.org/10.1186/s12978-017-0327-0.
Haggaz A, Ahmed S, Adam I. Use of prenatal care services in Darfur, Sudan. Int J Gynecol Obstet. 2008;103(3):252–3. https://doi.org/10.1016/j.ijgo.2008.06.010.
Andrew EVW, Pell C, Angwin A, et al. Factors affecting attendance at and timing of formal antenatal care: results from a qualitative study in Madang, Papua New Guinea. PLoS ONE. 2014. https://doi.org/10.1371/journal.pone.0093025.
Talhouk R, Mesmar S, Thieme A, et al. Syrian refugees and digital health in Lebanon: Opportunities for improving antenatal health. In: Conference on human factors in computing systems—proceedings. 2016;331–342. https://doi.org/10.1145/2858036.2858331.
Tolefac PN, Halle-Ekane GE, Agbor VN, Sama CB, Ngwasiri C, Tebeu PM. Why do pregnant women present late for their first antenatal care consultation in Cameroon? Matern Health Neonatol Perinatol. 2017;3(1):1–6. https://doi.org/10.1186/s40748-017-0067-8.
Okonofua F, Ogu R, Agholor K, et al. Qualitative assessment of women’s satisfaction with maternal health care in referral hospitals in Nigeria. Reprod Health. 2017;14(1):1–8. https://doi.org/10.1186/s12978-017-0305-6.
Ifenne DI, Utoo BT. Gestational age at booking for antenatal care in a tertiary health facility in north-central, Nigeria. J Niger Med Assoc. 2012;53(4):236–9. https://doi.org/10.4103/0300-1652.107602.
Rahmani Z, Brekke M. Antenatal and obstetric care in Afghanistan—a qualitative study among health care receivers and health care providers. BMC Health Serv Res. 2013. https://doi.org/10.1186/1472-6963-13-166.
Alam N, Chowdhury ME, Kouanda S, et al. The role of transportation to access maternal care services for women in rural Bangladesh and Burkina Faso: a mixed methods study. Int J Gynecol Obstet. 2016;135:S45–50. https://doi.org/10.1016/j.ijgo.2016.09.003.
Donmozoun TS, Sombie I, Meda N. What prevent women for a sustainable use of maternal care in two medical districts of Burkina Faso? a qualitative study. Pan Afr Med J. 2014;18:1–6. https://doi.org/10.11604/pamj.2014.18.43.2210.
Wallace HJ, McDonald S, Belton S, et al. The decision to seek care antenatally and during labour and birth—Who and what influences this in Timor-Leste? A qualitative project exploring the perceptions of Timorese women and men. Midwifery. 2018;65:35–42. https://doi.org/10.1016/j.midw.2018.05.013.
Shabila NP, Ahmed HM, Yasin MY. Women’s views and experiences of antenatal care in Iraq: a Q methodology study. BMC Pregnancy Childb. 2014. https://doi.org/10.1186/1471-2393-14-43.
Chol C, Hunter C, Debru B, Haile B, Negin J, Cumming RG. Stakeholders’ perspectives on facilitators of and barriers to the utilisation of and access to maternal health services in Eritrea: a qualitative study. BMC Pregnancy Childb. 2018. https://doi.org/10.1186/s12884-018-1665-9.
Alex M, Whitty-Rogers J. Experiences of pregnancy complications: Voices from central Haiti. Health Care Women Int. 2017;38(10):1034–57. https://doi.org/10.1080/07399332.2017.1350179.
Lawry L, Canteli C, Rabenzanahary T, Pramana W. A mixed methods assessment of barriers to maternal, newborn and child health in gogrial west, south Sudan. Reprod Health. 2017;14(1):1–13. https://doi.org/10.1186/s12978-016-0269-y.
Mourtada R, Bottomley C, Houben F, Bashour H, Campbell OMR. A mixed methods analysis of factors affecting antenatal care content: a Syrian case study. PLoS ONE. 2019;14(3):1–24. https://doi.org/10.1371/journal.pone.0214375.
Jallow IK, Chou YJ, Liu TL, Huang N. Womens perception of antenatal care services in public and private clinics in the Gambia. Int J Qual Health Care. 2012;24(6):595–600. https://doi.org/10.1093/intqhc/mzs033.
Badal NF, Yusuf UA, Egal J, et al. With knowledge and support, women can attend antenatal care: the views of women in IDP camps in Somaliland. 2015.
Gure F, Yusuf M, Foster AM. Exploring Somali women’s reproductive health knowledge and experiences: results from focus group discussions in Mogadishu. Reprod Health Matters. 2015;23(46):136–44. https://doi.org/10.1016/j.rhm.2015.11.018.
Ekabua J, Ekabua K, Njoku C. Proposed framework for making focused antenatal care services accessible: a review of the Nigerian setting. ISRN Obstet Gynecol. 2011;2011:1–5. https://doi.org/10.5402/2011/253964.
Stojanovski K, Holla A, Hoxha I, Howell E, Janevic T. The influence of ethnicity and displacement on quality of antenatal care: the case of Roma, Ashkali, and Balkan Egyptian communities in Kosovo. Health Hum Rights. 2017;19(2):35–48.
Mullany LC, Beyrer C, Lee TJ, et al. Access to essential maternal health interventions and human rights violations among vulnerable communities in eastern burma. PLoS Med. 2008;5(12):1689–98. https://doi.org/10.1371/journal.pmed.0050242.
Leone T, Alburez-Gutierrez D, Ghandour R, Coast E, Giacaman R. Maternal and child access to care and intensity of conflict in the occupied Palestinian territory: a pseudo longitudinal analysis (2000–2014). Confl Health. 2019. https://doi.org/10.1186/s13031-019-0220-2.
Solanke BL. Factors associated with use of maternal healthcare services during the Boko Haram insurgency in North-East Nigeria. Med Confl Surviv. 2018;34(3):158–84. https://doi.org/10.1080/13623699.2018.1511358.
Mugo NS, Dibley MJ, Damundu EY, Alam A. “The system here isn’t on patients’ side”—perspectives of women and men on the barriers to accessing and utilizing maternal healthcare services in South Sudan. BMC Health Serv Res. 2018. https://doi.org/10.1186/s12913-017-2788-9.
Othman S, Almahbashi T, Alabed AAA, Abdulwahed A. Factors affecting utilization of antenatal care services in Sana’a city, Yeman. Malays J Public Health Med. 2017;17(3):1–14.
Oyewale TO, Mavundla TR. Socioeconomic factors contributing to exclusion of women from maternal health benefit in Abuja, Nigeria. Curationis. 2015;38(1):1–11. https://doi.org/10.4102/curationis.v38i1.1272.
Teguete I, Maiga AW, Leppert PC. Maternal and neonatal outcomes of grand multiparas over two decades in Mali. Acta Obstet Gynecol Scand. 2012;91(5):580–6. https://doi.org/10.1111/j.1600-0412.2012.01372.x.
Ntambue AM, Dramaix-Wilmet M, Donnen P. Determinants of maternal health services utilization in urban settings of the Democratic Republic of Congo—a case study of Lubumbashi City. BMC Pregnancy Childb. 2012;12(1):66.
Doctor HV, Findley SE, Ager A, et al. Using community-based research to shape the design and delivery of maternal health services in Northern Nigeria. Reprod Health Matters. 2012;20(39):104–12. https://doi.org/10.1016/S0968-8080(12)39615-8.
Truppa C, Leresche E, Fuller AF, et al. Utilization of primary health care services among Syrian refugee and Lebanese women targeted by the ICRC program in Lebanon: a cross-sectional study. Confl Health. 2019. https://doi.org/10.1186/s13031-019-0190-4.
Kiruja J, Osman F, Egal JA, Essén B, Klingberg-Allvin M, Erlandsson K. Maternal near-miss and death incidences—frequencies, causes and the referral chain in Somaliland: a pilot study using the WHO near-miss approach. Sex Reprod Healthc. 2017;12:30–6. https://doi.org/10.1016/j.srhc.2017.02.003.
Steenland M, Robyn PJ, Compaore P, et al. Performance-based financing to increase utilization of maternal health services: evidence from Burkina Faso. SSM Popul Health. 2016;2017(3):179–84. https://doi.org/10.1016/j.ssmph.2017.01.001.
Ashir GM, Doctor HV, Afenyadu GY. Performance based financing and uptake of maternal and child health services in yobe sate, northern Nigeria. Glob J Health Sci. 2013;5(3):34–41. https://doi.org/10.5539/gjhs.v5n3p34.
Ziegler BR, Kansanga M, Sano Y, Kangmennaang J, Kpienbaareh D, Luginaah I. Antenatal care utilization in the fragile and conflict-affected context of the Democratic Republic of the Congo. Soc Sci Med. 2020;262(July):113253. https://doi.org/10.1016/j.socscimed.2020.113253.
Ramos Jaraba SM, Quiceno Toro N, Ochoa Sierra M, et al. Health in conflict and post-conflict settings: reproductive, maternal and child health in Colombia. Confl Health. 2020;14(1):33. https://doi.org/10.1186/s13031-020-00273-1.
Filippi V, Ronsmans C, Campbell OM, et al. Maternal health in poor countries: the broader context and a call for action. Lancet. 2006;368(9546):1535–41. https://doi.org/10.1016/S0140-6736(06)69384-7.
Kpienbaareh D, Atuoye KN, Ngabonzima A, et al. Spatio-temporal disparities in maternal health service utilization in Rwanda: What next for SDGs? Soc Sci Med. 2019;226(March):164–75. https://doi.org/10.1016/j.socscimed.2019.02.040.
Sami S, Mayai A, Sheehy G, et al. Maternal and child health service delivery in conflict-affected settings: a case study example from Upper Nile and Unity states, South Sudan. Confl Health. 2020;14(1):34. https://doi.org/10.1186/s13031-020-00272-2.
Kelly JT, Betancourt TS, Mukwege D, Lipton R, VanRooyen MJ. Experiences of female survivors of sexual violence in eastern Democratic Republic of the Congo: a mixed-methods study. Confl Health. 2011;5(1):25. https://doi.org/10.1186/1752-1505-5-25.
Daley P. Gender and genocide in burundi: the search for spaces of peace in the great Lakes region. 2008.
Baaz ME, Stern M. Why do soldiers rape? Masculinity, violence, and sexuality in the armed forces in the Congo (DRC). Int Stud Q. 2009;53(2):495–518. https://doi.org/10.1111/j.1468-2478.2009.00543.x.
Ezeh OK, Ogbo FA, Stevens GJ, et al. Factors Associated with the Early Initiation of Breastfeeding in Economic Community of West African States (ECOWAS). Nutrients. 2019. https://doi.org/10.3390/nu11112765.
Bell S. The quantitative impact of conflict on education. 2011.
Uvin P. Life after violence: a people’s story of Burundi. 2008.
Manjoo R, McRaith C. Gender-based violence and justice in conflict and post-conflict areas. Cornell Int Law J. 2011;44:11–31.
Wirtz AL, Pham K, Glass N, et al. Gender-based violence in conflict and displacement: qualitative findings from displaced women in Colombia. Confl Health. 2014;8(1):10. https://doi.org/10.1186/1752-1505-8-10.
Alhusen JL, Ray E, Sharps P, Bullock L. Intimate partner violence during pregnancy: maternal and neonatal outcomes. J Womens Health. 2015;24(1):100–6. https://doi.org/10.1089/jwh.2014.4872.
Gill MM, Ditekemena J, Loando A, et al. Addressing early retention in antenatal care among HIV-positive women through a simple intervention in Kinshasa, DRC: The Elombe “Champion” standard operating procedure. AIDS Behav. 2018;22(3):860–6. https://doi.org/10.1007/s10461-017-1770-1.
Sano Y, Antabe R, Atuoye KN, Braimah JA, Galaa SZ, Luginaah I. Married women’s autonomy and post-delivery modern contraceptive use in the Democratic Republic of Congo. BMC Womens Health. 2018;18(1):4–10. https://doi.org/10.1186/s12905-018-0540-1.
Tlapek SM. Women’s status and intimate partner violence in the Democratic Republic of Congo. J Interpers Violence. 2015;30(14):2526–40. https://doi.org/10.1177/0886260514553118.
Mkandawire P, Atari O, Kangmennaang J, Arku G, Luginaah I, Etowa J. Pregnancy intention and gestational age at first antenatal care (ANC) visit in Rwanda. Midwifery. 2018;2019(68):30–8. https://doi.org/10.1016/j.midw.2018.08.017.
White D, Dynes M, Rubardt M, Sissoko K, Stephenson R. The influence of intra familial power on maternal health care in Mali: perspectives of women, men and mothers-in-law. Int Perspect Sex Reprod Health. 2013;39(2):58–68. https://doi.org/10.1363/3905813.
Ali R, Barra AF, Berg CN, Damania R, Nash JD, Russ J. Infrastructure in Conflict-Prone and Fragile Environments: Evidence from the Democratic Republic of Congo. Geneva: The World Bank; 2015. https://doi.org/10.1596/1813-9450-7273.
Mullany LC, Lee TJ, Yone L, et al. Impact of community-based maternal health workers on coverage of essential maternal health interventions among internally displaced communities in eastern Burma: The MOM project. PLoS Med. 2010. https://doi.org/10.1371/journal.pmed.1000317.
Ebener S, Guerra-Arias M, Campbell J, et al. The geography of maternal and newborn health: the state of the art. Int J Health Geogr. 2015. https://doi.org/10.1186/s12942-015-0012-x.
Simkhada B, Van Teijlingen ER, Porter M, Simkhada P. Factors affecting the utilization of antenatal care in developing countries: systematic review of the literature. J Adv Nurs. 2008;61(3):244–60. https://doi.org/10.1111/j.1365-2648.2007.04532.x.
Fakunle B, Okunlola MA, Fajola A, Ottih U, Ilesanmi AO. Community health insurance as a catalyst for uptake of family planning and reproductive health services: The Obio Cottage Hospital experience. J Obstet Gynaecol. 2014;34(6):501–3. https://doi.org/10.3109/01443615.2014.902044.
Ibnouf AH, van den Borne HW, Maarse JA. Utilization of antenatal care services by Sudanese women in their reproductive age. Saudi Med J. 2007;28(5):737–43.
Alenoghena IO, Isah EC, Isara AR. Maternal health services uptake and its determinants in public primary health care facilities in edo state, Nigeria. Niger Postgrad Med J. 2015;22(1):25–31.
Alhaidari T, Amso N, Jawad TM. Feasibility and acceptability of text messaging to support antenatal healthcare in Iraqi pregnant women: a pilot study. J Perinat Med. 2017;46(1):67–74. https://doi.org/10.1515/jpm-2016-0127.
Balinska MA, Nesbitt R, Ghantous Z, Ciglenecki I, Staderini N. Reproductive health in humanitarian settings in Lebanon and Iraq: Results from four cross-sectional studies, 2014–2015. Confl Health. 2019. https://doi.org/10.1186/s13031-019-0210-4.
Chi PC, Bulage P, Urdal H, Sundby J. A qualitative study exploring the determinants of maternal health service uptake in post-conflict Burundi and Northern Uganda. BMC Pregnancy Childb. 2015. https://doi.org/10.1186/s12884-015-0449-8.
Findley SE, Doctor HV, Ashir GM. Reinvigorating health systems and community-based services to improve maternal health outcomes: case study from northern Nigeria. J Prim Care Community Health. 2015;6(2):88–99. https://doi.org/10.1177/2150131914549383.
Franco LM, Diop FP, Burgert CR, Kelley AG, Makinen M, Simparae CHT. Effects of mutual health organizations on use of priority health-care services in urban and rural Mali: a case-control study. Bull World Health Organ. 2008;86(11):830–8. https://doi.org/10.2471/BLT.08.051045.
Gao X, Kelley DW. Understanding how distance to facility and quality of care affect maternal health service utilization in Kenya and Haiti: a comparative geographic information system study. Geospat Health. 2019;14(1):92–102. https://doi.org/10.4081/gh.2019.690.
Ibrahim HK, El Borgy MD, Mohammed HO. Knowledge, attitude, and practices of pregnant women towards antenatal care in primary healthcare centers in Benghazi, Libya. J Egypt Public Health Assoc. 2014;89(3):119–26. https://doi.org/10.1097/01.EPX.0000455673.91730.50.
Jibril UN, Saleh GN, Badaki O, Anyebe EE, Umar A, Kamal A. Health education intervention on knowledge and accessibility of pregnant women to antenatal care services in Edu, Kwara State, Nigeria. Int J Womens Health Reprod Sci. 2018;6(2):154–60. https://doi.org/10.15296/ijwhr.2018.26.
Larsen GL, Lupiwa S, Kave HP, Gillieatt S, Alpers MP. Antenatal care in Goroka: issues and perceptions. P N G Med J. 2004;47(3–4):202–14.
Maraga S, Namosha E, Gouda H, Vallely L, Rare L, Phuanukoonnon S. Sociodemographic factors associated with maternal health care utilization in Wosera. East Sepik Province. 2011;54(3–4):154–63.
Okonofua F, Ntoimo L, Ogungbangbe J, Anjorin S, Imongan W, Yaya S. Predictors of women’s utilization of primary health care for skilled pregnancy care in rural Nigeria. BMC Pregnancy Childb. 2018. https://doi.org/10.1186/s12884-018-1730-4.
Rossier C, Muindi K, Soura A. Maternal health care utilization in Nairobi and Ouagadougou: evidence from HDSS. Glob Health Action. 2014;7:1–10. https://doi.org/10.3402/gha.v7.24351.
Turan JM, Tesfagiorghis M, Polan ML. Evaluation of a community intervention for promotion of safe motherhood in Eritrea. J Midwifery Womens Health. 2011;56(1):8–17. https://doi.org/10.1111/j.1542-2011.2010.00001.x.
Vail J. Antenatal utilization, family planning and fertility preferences in Tari. P N G Med J. 2002;45(1–2):134–41.
Viswanathan K, Hansen PM, Hafizur RM. Can community health workers increase coverage of reproductive health services? J Epidemiol Community Health. 2012;66(10):894–900. https://doi.org/10.1136/jech-2011-200275.
Adebangbe FT, Mturi AJ. Factors associated with the number of antenatal care visits among internally displaced women in northern Nigeria. Afr J Reprod Health. 2021;25(2):120–30.
Feng Y, Ahuru RR, Anser MK, Osabohien R, Ahmad M, Efegbere AH. Household economic wealth management and antenatal care utilization among business women in the reproductive-age. Afr J Reprod Health. 2021;25(6):143.
Laing SP, Guzek JM, Rassam DM, Ceesay IS, N’Dow JMO. Determinants of compliance with the World Health Organisation recommendations for pregnant women in an urban health centre in The Gambia. Afr J Reprod Health. 2020;24(3):24–32. https://doi.org/10.29063/ajrh2020/v24i3.3.
Onalu C, Agwu P, Gobo B, Okoye U. Mortality experiences for women in riverine areas of the Niger delta and utilization of maternal health services. Health Soc Work. 2021;46(1):59–67. https://doi.org/10.1093/hsw/hlaa032.
Oyovwe P, Woolhead G. Exploring health care professionals’ and women’s perspectives on the barriers to maternal health services: a qualitative study in Eku Town of Delta State, Nigeria. AIMS Public Health. 2021;8(1):154–71. https://doi.org/10.3934/publichealth.2021012.
Somé A, Baguiya A, Coulibaly A, Bagnoa V, Kouanda S. Prevalence and factors associated with late first antenatal care visit in kaya health district, Burkina Fao. Afr J Reprod Health. 2020;24(2):19–26. https://doi.org/10.29063/ajrh2020/v24i2.2.
Stanikzai MH, Wafa MH, Wasiq AW, Sayam H. Magnitude and determinants of antenatal care utilization in Kandahar City, Afghanistan. Obstet Gynecol Int. 2021;2021:e5201682. https://doi.org/10.1155/2021/5201682.
Sui Y, Ahuru RR, Huang K, Anser MK, Osabohien R. Household socioeconomic status and antenatal care utilization among women in the reproductive-age. Front Public Health. 2021. https://doi.org/10.3389/fpubh.2021.724337.
Kane S, Rial M, Kok M, Matere A, Dieleman M, Broerse JEW. Too afraid to go: fears of dignity violations as reasons for non-use of maternal health services in South Sudan. Reprod Health. 2018. https://doi.org/10.1186/s12978-018-0487-6.
Lowe M, Chen DR, Huang SL. Social and cultural factors affecting maternal health in rural Gambia: an exploratory qualitative study. PLoS ONE. 2016. https://doi.org/10.1371/journal.pone.0163653.
Meiksin R, Meekers D, Thompson S, Hagopian A, Mercer MA. Domestic violence, marital control, and family planning, maternal, and birth outcomes in Timor-Leste. Matern Child Health J. 2015;19(6):1338–47. https://doi.org/10.1007/s10995-014-1638-1.
Ntoimo LFC, Okonofua FE, Igboin B, Ekwo C, Imongan W, Yaya S. Why rural women do not use primary health centres for pregnancy care: evidence from a qualitative study in Nigeria. BMC Pregnancy Childb. 2019. https://doi.org/10.1186/s12884-019-2433-1.
Igboanugo GM, Martin CH. What are pregnant women in a rural Niger Delta community’s perceptions of conventional maternity service provision? An exploratory qualitative study. Afr J Reprod Health. 2011;15(3):59–72.
Mohamed-Ahmed R, Aziz MA, Walker R. Antenatal care in Sudan: a qualitative study into accessibility and quality of maternal health services in Khartoum. Int J Childb. 2018;8(2):77–86. https://doi.org/10.1891/2156-5287.8.2.77.
Bayo P, Belaid L, Ochola E, et al. Maternal and neonatal health care service utilisation in the wake of active conflict and socio-economic downturn in Torit County, Republic of South Sudan: a multimethod locally driven study. Afr J Reprod Health. 2021;25(3s):30–42.
Akseer N, Bhatti Z, Rizvi A, Salehi AS, Mashal T, Bhutta ZA. Coverage and inequalities in maternal and child health interventions in Afghanistan. BMC Public Health. 2016. https://doi.org/10.1186/s12889-016-3406-1.
Galadanci HS, Ejembi CL, Iliyasu Z, Alagh B, Umar US. Maternal health in Northern Nigeria—a far cry from ideal. BJOG Int J Obstet Gynaecol. 2007;114(4):448–52. https://doi.org/10.1111/j.1471-0528.2007.01229.x.
Merrell LK, Blackstone SR. Women’s empowerment as a mitigating factor for improved antenatal care quality despite impact of 2014 Ebola Outbreak in Guinea. Int J Environ Res Public Health. 2020;17(21):8172. https://doi.org/10.3390/ijerph17218172.
Mutowo J, Yazbek M, van der Wath A, Maree C. Barriers to using antenatal care services in a rural district in Zimbabwe. Int J Afr Nurs Sci. 2021;15:100. https://doi.org/10.1016/j.ijans.2021.100319.
Chittambo BR, Smith JE, Ehlers VJ. Community participation in providing antenatal services in Zimbabwe. Afr J Nurs Midwifery. 2003;5(1):9.
Edmond KM, Yousufi K, Anwari Z. Can community health worker home visiting improve care-seeking and maternal and newborn care practices in fragile states such as Afghanistan? A population-based intervention study. BMC Med. 2018. https://doi.org/10.1186/s12916-018-1092-9.
Edmond KM, Foshanji AI, Naziri M. Conditional cash transfers to improve use of health facilities by mothers and newborns in conflict affected countries, a prospective population based intervention study from Afghanistan. BMC Pregnancy Childb. 2019. https://doi.org/10.1186/s12884-019-2327-2.
Rudasingwa M, Soeters R, Basenya O. The effect of performance-based financing on maternal healthcare use in Burundi: a two-wave pooled cross-sectional analysis. Glob Health Action. 2017. https://doi.org/10.1080/16549716.2017.1327241.
Christou A, Alam A, Sadat Hofiani SM, et al. Understanding pathways leading to stillbirth: the role of care-seeking and care received during pregnancy and childbirth in Kabul province, Afghanistan. Women Birth J Aust Coll Midwives. 2020;33(6):544–55. https://doi.org/10.1016/j.wombi.2020.02.012.
Kim C, Tappis H, Natiq L, et al. Travel time, availability of emergency obstetric care, and perceived quality of care associated with maternal healthcare utilisation in Afghanistan: a multilevel analysis. Glob Public Health. 2021. https://doi.org/10.1080/17441692.2021.1873400.
Jeremiah I, Kasso T, Oriji VK. Patients’ perception of antenatal care at the University of Port Harcourt Teaching Hospital. Niger J Med J Natl Assoc Resid Dr Niger. 2012;21(1):66–9.
King S, Passey M, Dickson R. Perceptions and use of maternal health services by women in rural coastal Madang Province. P N G Med J. 2013;56(1–2):5–13.
Hyzam D, Zou M, Boah M, et al. Health information and health-seeking behaviour in Yemen: perspectives of health leaders, midwives and mothers in two rural areas of Yemen. BMC Pregnancy Childb. 2020;20(1):404. https://doi.org/10.1186/s12884-020-03101-9.
Grenier L, Suhowatsky S, Kabue MM. Impact of group antenatal care (G-ANC) versus individual antenatal care (ANC) on quality of care, ANC attendance and facility-based delivery: a pragmatic cluster-randomized controlled trial in Kenya and Nigeria. PLoS ONE. 2019;14(10):1–18. https://doi.org/10.1371/journal.pone.0222177.
Currie S, Natiq L, Anwari Z, Tappis H. Assessing respectful maternity care in a fragile, conflict-affected context: observations from a 2016 national assessment in Afghanistan. Health Care Women Int. 2021. https://doi.org/10.1080/07399332.2021.1932890.
Mourtada R, Bashour H, Houben F. A qualitative study exploring barriers to adequate uptake of antenatal care in pre-conflict Syria: low cost interventions are needed to address disparities in antenatal care. Contracept Reprod Med. 2021;6(1):17. https://doi.org/10.1186/s40834-021-00156-7.
Udenigwe O, Okonofua FE, Ntoimo LFC, Imongan W, Igboin B, Yaya S. “We have either obsolete knowledge, obsolete equipment or obsolete skills”: policy-makers and clinical managers’ views on maternal health delivery in rural Nigeria. Fam Med Community Health. 2021;9(3):e000994. https://doi.org/10.1136/fmch-2021-000994.
Perry HB, King-Schultz LW, Aftab AS, Bryant JH. Health equity issues at the local level: socio-geography, access, and health outcomes in the service area of the Hôpital Albert Schweitzer-Haiti. Int J Equity Health. 2007;6:1–10. https://doi.org/10.1186/1475-9276-6-7.
Erismann S, Gami JP, Ouedraogo B, Revault D, Prytherch H, Lechthaler F. Effects of a four-year health systems intervention on the use of maternal and infant health services: results from a programme evaluation in two districts of rural Chad. BMC Public Health. 2021;21(1):2304. https://doi.org/10.1186/s12889-021-12330-2.
Ekzayez A, Alhaj Ahmad Y, Alhaleb H, Checchi F. The impact of armed conflict on utilisation of health services in north-west Syria: an observational study. Confl Health. 2021;15(1):91. https://doi.org/10.1186/s13031-021-00429-7.
Edmond K, Yousufi K, Naziri M. Mobile outreach health services for mothers and children in conflict-affected and remote areas: a population-based study from Afghanistan. Arch Child. 2020;105(1):18–25. https://doi.org/10.1136/archdischild-2019-316802.
Nie J, Unger JA, Thompson S, Hofstee M, Gu J, Mercer MA. Does mobile phone ownership predict better utilization of maternal and newborn health services? A cross-sectional study in Timor-Leste. BMC Pregnancy Childbirth. 2016. https://doi.org/10.1186/s12884-016-0981-1.
O’Keefe D, Davis J, Yakuna G, Van Gemert C, Morgan C. Formal and informal maternal health care: comparing the service provision of health facilities and village health volunteers in East Sepik Province. P N G Med J. 2011;54(3–4):147–53.
Ye M, Bagagan C, Millogo O. Use of mobile phone to promote governance and equity within the health system: experience of rural health district in Burkina Faso. J Heal Commun. 2016;1(3):1–11. https://doi.org/10.4172/2472-1654.100017.
Ouedraogo C, Vosti S, Wessells K, Arnold C, Faye M, Hess S. Out-of-pocket costs and time spent attending antenatal care services: a case study of pregnant women in selected rural communities in Zinder, Niger. BMC Health Serv Res. 2021. https://doi.org/10.1186/s12913-020-06027-2.
Samiah S, Stanikzai MH, Wasiq AW, Sayam H. Factors associated with late antenatal care initiation among pregnant women attending a comprehensive healthcare facility in Kandahar Province, Afghanistan. Indian J Public Health. 2021;65(3):298–301. https://doi.org/10.4103/ijph.IJPH_62_21.
Acknowledgements
Not applicable.
Funding
This research was supported by a Canadian Graduate Scholarship-Masters from the Social Science and Humanities Research Council and an Ontario Graduate Scholarship.
Author information
Authors and Affiliations
Contributions
B.Z. developed the search string and developed the data extraction form. B.Z. and K.A. performed title, abstract, and full-text screening and independently extracted and coded the data. B.Z., L.M., and E.B. analyzed and interpreted the data. B.Z., K.A., L.M., and E.B. wrote the manuscript in consultation with I.L. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This systematic review did not require ethics approval as data was collected from publicly available documents.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Detailed description of included studies in this systematic review (n = 121).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Alibhai, K.M., Ziegler, B.R., Meddings, L. et al. Factors impacting antenatal care utilization: a systematic review of 37 fragile and conflict-affected situations. Confl Health 16, 33 (2022). https://doi.org/10.1186/s13031-022-00459-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13031-022-00459-9