Abstract
It is commonly accepted that host genes show high methylation in cervical intraepithelial neoplasia 3 (CIN3) or worse (CIN3+). However, study quality varies, as does the clinical performance of markers in different populations. We aimed to validate candidate gene DNA methylation with standardized testing methods in the same batch of samples. We first compared the performance of 16 DNA methylation markers for detecting CIN3+ in the 82-sample training set, including 24 subjects with ≤ CIN1, 10 subjects with CIN2, 23 subjects with CIN3, and 25 subjects with cervical cancer (CC). Then five methylation markers were selected and subsequently validated among an independent set of 74 subjects, including 47 subjects with ≤ CIN1, 13 subjects with CIN2, 6 subjects with CIN3, and 8 subjects with CC. The results in the validation set revealed that methylation analysis of the SOX1 (SOX1m) showed a superior level of clinical performance (AUC = 0.879; sensitivity = 85.7%; specificity = 90.0%). SOX1m had better accuracy than cytology, with a reduced referral rate (23.0% vs. 31.4%) and a lower number of overtreatment (5 vs. 13) cases among high-risk human papillomavirus (hrHPV)-positive women. Importantly, among hrHPV-positive and SOX1m-negative women, only 1 CIN3 patient was at risk for follow-up after 1 year, whereas 1 CIN3 patient and 1 CC patient were at risk among hrHPV-positive and cytology-negative women. In this investigation, we screened 16 reported methylation markers to provide a basis for future studies related to potential precancerous lesion/cancer methylation markers in the Chinese population. The study also revealed that SOX1m has optimal CIN3+ detection performance, suggesting that it may be a promising biomarker for detecting CIN3+ in the Chinese population.
Similar content being viewed by others
Introduction
Cervical cancer (CC) had the fourth highest incidence and mortality among women worldwide in 2020 [1, 2], and its incidence had markedly increased in China since 2000 [3]. Most cervical cancers are in poor- and middle-income countries. Nevertheless, its incidence and mortality in the United States have dropped notably since the 1950s [4], as a result of prevention programs [5], which include human papillomavirus (HPV) vaccination (primary prevention) and screening (secondary prevention). Although prevention programs have grown greatly over the past [6], the measures have not been equitably implemented across and within countries [7]. As long as HPV vaccination is restricted, screening still serves as a cornerstone for detecting and preventing cervical cancer.
Over the past 30 years, research has shown a cause-and-effect relationship between high-risk HPV (hrHPV) infection of the cervix and cervical cancer, of which persistent hrHPV drives the slow progression of precancerous lesions and eventually cervical cancer [8]. Large longitudinal studies have found that hrHPV testing is effective as a primary screening tool [9, 10]. The current guidelines recommend hrHPV testing as the primary test or a co-test with cytology [11]. The hrHPV test as primary screening has a better sensitivity than cytology for detecting cervical intraepithelial neoplasia 3 (CIN3) or worse (CIN3+). However, hrHPV testing cannot distinguish whether the infection is transient or persistent, which results in less specificity, leading to unnecessary referrals to the gynecologist and anxiety in false-positive women. Cytology detecting cervical (pre)malignancies focuses on abnormal cells and has relatively limited sensitivity due to the subjectivity of analysis [12]. Cytology mitigates the above concerns through co-testing or triage of hrHPV infection patients, but the disadvantages of cytology testing still limit its use. Therefore, a high-accuracy and feasible triage strategy is urgently needed.
Aberrant DNA methylation patterns are a hallmark of cancer, and cytosine methylation (5mC) can lead to the activation of oncogenes and the inactivation of tumor suppressor genes, driving tumorigenesis. The methylation of CpG islands within gene promoter region is a frequently observed epigenetic phenomenon in many types of cancer, including cervical cancer [13]. The epigenetic alteration accumulated in epithelial cells is one of the processes underlying the driver of cervical carcinogenesis and progression. The literature [13,14,15,16] reported that promoter methylation levels of host genes, such as EPB41L3, FAM19A4, JAM3, miR124-2, PAX1, ZNF671, and SOX1, were related to the severity of cervical histological lesions. Methylation analysis could be a promising biomarker for the early detection of cervical lesions. However, the clinical representation of gene methylation varies in studies of various populations. Leeuwen et al. [17] evaluated the clinical performance of EPB41L3 and JAM3 methylation (EPB41L3m and JAM3m), showing that the sensitivities of EPB41L3m and JAM3m were 84% and 68%, respectively, for detecting CIN3+ in Slovenian patients. An exploratory study [18] was performed on Chinese patients, which also involved analyzing the performance of EPB41L3m and JAM3m. The results indicated that the sensitivity (74.8%) of EPB41L3m in detecting CIN3+ was poorer than that in the Slovenian population, but the sensitivity (80.4%) of JAM3m was superior. Therefore, it is necessary to evaluate the clinical performance of potential candidate genes in the same cohort.
Although various methylation biomarker-based kits [19,20,21,22] were dedicated to detecting CIN3+ in HPV-positive women, we could still keep optimizing the methylation marker for clinical implementation [23] in the Chinese population. We surveyed a variety of publications and found that most DNA methylation biomarker-based studies had been performed by distinct research groups using different analysis methods in different populations. Therefore, in the current study, we sought to evaluate the clinical performance of candidate gene DNA methylation in the same batch of clinical samples. The performance of the selected methylation marker was subsequently compared to that of cytology in hrHPV-positive women.
Methods
Clinical specimens
The clinical study was approved by the local medical ethics review committee. Subjects enrolled in methylation testing at Xiangya Hospital and Second Xiangya Hospital from January 2021 to June 2022. Study inclusion criteria included cervical screening populations, or who were suspected of cervical lesions on gynecological examination. Patients with any history of CIN or cervical cancer treatment, a current pregnancy, or menstruation were excluded. All subjects had the colposcopic examination results. Cervical biopsies were collected from each visible lesion for histological evaluation and categorized in accordance with international criteria including ≤ CIN1, CIN2, CIN3 (including carcinoma in situ), or CC. To ensure the quality of the diagnosis, two experienced pathologists independently reviewed the histology slides. Cytology was categorized as negative for intraepithelial lesion or malignancy (NILM), atypical squamous cells of undetermined significance (ASC-US), low-grade squamous intraepithelial lesion (LSIL), atypical squamous cells: cannot exclude high-grade squamous intraepithelial lesion (ASC-H) and high-grade squamous intraepithelial lesion (HSIL). The study enrolled 156 women, 82 of whom were trained for screening candidate genes, and 74 of whom were collected for validation of selected genes with the complete information (with cytology and hrHPV).
Candidate gene selection
Candidate methylation genes were selected according to the following criteria: (1) the genes were reported in previous studies as DNA markers to identify cervical lesions; (2) primer sequences were shown in the literature or were designed to stabilize detection in our experiment. Finally, GFRA1, MIR124-2, ASCL1, CCDC181, EPB41L3, JAM3, PAX1, SORCS1, PCDHA13, LOC100289333, BOLL, FAM19A4, MIR129-2, ZIC1, SOX1 and SST were selected as candidate genes [13,14,15, 24,25,26].
Sample preparation and hrHPV testing
The clinician took cervical scrapes using a cervix brush and directly placed the brush in the preservation solution (ThinPrep, MA). The hrHPV test was conducted by a fluorescence quantitative PCR (ABI 7500) system (Life Tech, USA) with an hrHPV kit (Sansure-Biotech, China). The kit uses type-specific probes to detect pooled results for hrHPV types, including HPV 16, 18 and other types (31, 33, 35, 39, 45, 51–53, 56, 58–59, 66 and 68).
Sodium bisulfite treatment and methylation testing
DNA from residual cervical scrapes was extracted with a HiPure Universal DNA Kit (Magen Biotech, China) after analysis of cytology and hrHPV, and the concentrations and 260/280 ratios were determined using a Nanodrop microspectrophotometer (Thermo Fisher Scientific, USA). Bisulfite conversion was performed on the isolated DNA with an EZ DNA Methylation Kit (Zymo Research, USA). DNA was purified and then eluted with 20 μL solution. All procedures were performed in accordance with the manufacturer’s instructions. Methylation analysis of the candidate genes and internal reference gene (ACTB) were evaluated using SYBR Green I (Solarbio, China) and the ABI 7500 system. PCRs were conducted with 5 μL of real-time PCR mix, 1 μL of bisulfite-treated DNA, primers for the respective genes and nuclease-free water to a final volume of 10 μL (Additional file 1: Table S1). The PCR conditions were as follows: 95 °C for 5 min, 45 cycles at 95 °C for 15 s and 60 °C for 30 s, and a standard melting curve. To ensure the quality of the samples, the ACTB cycle threshold (Ct) of all samples should be below 30. The delta cycle threshold value (ΔCt) of each sample was calculated by the candidate methylated gene Ct minus the methylated ATCB gene Ct. Nonbisulfite-converted gDNA was used as a negative control, and bisulfite-converted DNA from women with cervical cancer was used as a positive control for each MSP plate.
Statistical analysis
The cutoff values of each gene DNA methylation were generated from methylated gene ΔCt of all samples with a receiver operating characteristic curve (ROC). The methylated genes with maximal values of the Youden index were determined as the optimal cutoff values. The optimal cutoff values in the training set were generated from 82 subjects, while the optimal cutoff values in the validation set were generated from 156 subjects. The area under the ROC curve (AUC) differentiating between CIN2- (≤ CIN1 and CIN2) and CIN3+ (CIN3 and CC) was greater than or equal to 0.8 (AUC ≥ 0.8). The positivity of cytology, hrHPV or methylation testing was calculated according to the cervical disease status confirmed by histology. Clinical sensitivity and specificity were estimated along with the exact 95% confidence interval (CI), which was the proportion calculated assuming a binomial distribution. Women with positive results in both hrHPV and DNA methylation testing were classified as triage positive and others were classified as triage negative. All analyses were conducted by using Statistical Product and Service Solutions (SPSS) Statistics 21.0 software (IBM Corporation, USA).
Results
Candidate DNA methylation markers in the training set
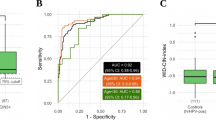
A flow scheme of the study is shown in Fig. 1. Pathology results for 82 samples were as follows: ≤ CIN1, n = 24 (29.3%); CIN2, n = 10 (12.2%); CIN3, n = 23 (28.0%); and CC, n = 25 (30.5%). DNA isolated from 82 cervical scrapes was bisulfite-treated and tested in MSP experiments for the 16 candidate DNA methylation markers GFRA1, MIR124-2, ASCL1, CCDC181, EPB41L3, JAM3, PAX1, SORCS1, PCDHA13, LOC100289333, BOLL, FAM19A4, MIR129-2, ZIC1, SOX1 and SST. There were 5 genes with AUCs greater than or equal to 0.8 (AUC ≥ 0.8) showing a distinction between CIN2- and CIN3+ in cervical scrapings (Fig. 2), which were validated next. The AUCs of MIR124-2, JAM3, LOC100289333, ZIC1, and SOX1 were 0.856 (95% CI 0.770–0.942), 0.800 (95% CI 0.701–0.898), 0.822 (95% CI 0.726–0.919), 0.839 (95% CI 0.751–0.928) and 0.814 (95% CI 0.720–0.909), respectively. The cutoff values corresponding to the above five genes were 9.89, 9.22, 6.2, 3.29 and 5.25, respectively (Additional file 1: Table S2). The positive rates of 16 candidate genes in the training set are shown in Additional file 1: Fig. S1. Eleven genes were excluded from further analysis.
Patients and histological outcomes
The clinicopathological data and cytology results of the validation cervical scrapes are summarized in Table 1. Pathology results for 74 samples were as follows: ≤ CIN1, n = 47 (63.5%); CIN2, n = 13 (17.6%); CIN3, n = 6 (8.1%); and CC, n = 8 (10.8%). CIN3+ subjects (average age 54.3 years) were older than CIN2- subjects (average age 43.0 years) (p < 0.05). The cytology results included 51 (68.9%) cases of NILM, 8 (10.8%) cases of ASC-US, 1 (1.4%) case of LSIL, 3 (4.1%) cases of ASC-H, and 11 (14.9%) cases of HSIL. Cytological results showed that NILM constituted 86.3% of ≤ CIN1 and ASC-US constituted 62.5% of CIN2, while HISL constituted 45.4% of cancer.
Clinical performance of five DNA methylation markers in the validation set
Five genes selected from the training set were validated with 74 cervical scrapings (Fig. 3). The positivity rate of HPV16/18 and methylation raised with increased pathological grade. Compared to the results of cytology (sensitivity: 71.4%, 95% CI 42.0–90.4%; specificity: 78.3%, 95% CI 65.4–87.5%), the sensitivity of hrHPV (92.9%, 95% CI 64.2–99.6%) was significantly higher with a slightly lower specificity (76.7%, 95% CI 63.7–86.2%), and the sensitivity of HPV16/18 genotyping (50.0%, 95% CI 24.0–76.0%) was lower with a higher specificity (95.0%, 95% CI 85.2–98.7%). Overall, methylation rates ranged from 16.7% to 66.7% for CIN3 and from 75.0% to 100.0% for cervical cancer. Single methylation of LOC100289333 (LOC100289333m), ZIC1 (ZIC1m) and SOX1 (SOX1m) tested positive in all cervical cancer scrapings. The new cutoff values in the validation set were recalculated from 156 subjects. The AUCs of LOC100289333m, ZIC1m, and SOX1m that distinguished CIN2- and CIN3+ in the validation set were still greater than 0.8, with 0.862 (95% CI 0.744–0.980), 0.835 (95% CI 0.700–0.969) and 0.879 (95% CI 0.763–0.994) by the new cutoff values of 6.27, 3.29 and 5.25, respectively. The AUCs of MIR124-2m and JAM3m were less than 0.8, with 0.763 (95% CI 0.605–0.922) and 0.750 (95% CI 0.576–0.924), respectively, resulting in exclusion from further analysis (Table 2). LOC100289333m and SOX1m, compared with ZIC1m (78.6%, 95% CI 48.8–94.3%), had better clinical performance, and which sensitivity was greater than 85% (85.7%, 95% CI 56.2–97.5%). However, SOX1m had higher specificity (90.0%, 95% CI 78.8–95.9%) than LOC100289333m (86.7%, 95% CI 74.9–93.7%).
DNA methylation markers for the triage of hrHPV-positive women
Forty-four of 74 (59.5%) subjects were hrHPV positive, with HPV16/18 positivity constituting 36.5% and non-16/18 hrHPV positivity constituting 23.0% of all subjects (Fig. 4). HPV16/18 genotyping was used to triage hrHPV-positive scrapings, and subjects with HPV16/18 positivity were referred directly to colposcopy. Among HPV16/18-positive women, 8 cases of CIN3+ (3 cases CIN3 and 5 cases CC) were detected, and 3 cases of CIN2- (1 case CIN1 and 2 cases CIN2) were overtreated. The rate of referral for colposcopy was 18.9% in non-16/18 hrHPV (+) plus cytology (≥ ASC-US) subjects. Thus, when cytology was applied as a screening strategy for hrHPV (+), the overall rate of referral for colposcopy was 31.4%, at which point the number of overtreatments was 13, and the number of missed diagnoses was 1 CIN3 and 1 CC (Fig. 4A). LOC100289333m, ZIC1m, or SOX1m in hrHPV-positive women was evaluated, with colposcopy referral rates of 20.3%, 20.3% or 23.0% and missed diagnoses in subjects with two, two or one CIN3 cases (Fig. 4B, D).
Discussion
In the cross-sectional study, we assessed the performance of 16 possible methylation markers by standardized testing methods in the same batch of samples. We found SOX1m to be a significant biomarker for detecting CIN3+ subjects. The data showed that SOX1m was superior to cytology in hrHPV-positive women. The current results imply that SOX1m analysis identifying cervical lesions is promising in the Chinese population.
To solve the low specificities of hrHPV testing, cytology is used for effective triage and management of hrHPV-positive samples. However, for hrHPV screening, only districts with high-quality cytology can relatively balance detection and over-referrals. It is challenging to recruit and relent skilled cytologists in rural areas. Methylation analysis with high reproducibility and objectivity is a feasible alternative biomarker [27]. As previously described, host gene DNA methylation might be useful for the triage and management of hrHPV-positive women. Compared to cytology, LOC100289333m, ZIC1m, or SOX1m had better accuracy for triage and management of hrHPV-positive women (Fig. 4), with lower colposcopy referral rates along with improved CIN3+ case detection. Moreover, all cancer patients were identified as hrHPV-positive women.
LOC100289333 is a pseudogene, whose methylation analysis is first reported in our study. Our data revealed that LOC100289333m has a middle level of performance among the three validated genes in the detection of CIN3+ with a sensitivity of 85.7% (56.2–97.5%) and specificity of 86.7% (74.9–93.7%). However, the performance in hrHPV-positive women was less favorable with a sensitivity of 66.7% (24.2–94.0%) and specificity of 90.9% (57.1–99.5%), which may be due to quantity bias from the small population size. The ZIC1 protein was first studied in cerebellum tissues and serves as a transcription factor in the central nervous system, muscle, and bone growth and development. Recent studies [28] found that the levels of ZIC1 mRNA and protein in cervical cancer and increased CIN grade were significantly decreased compared with normal and CIN samples, which is presumably a promising biomarker for prognosis. In addition, ZIC1m was elevated when the lesions of the cervix worsened [25, 29], which correlated with the downregulation of ZIC1 in increased lesion grades. ZIC1m in cervical scrapes was associated with the presence and progression of lesions among hrHPV-positive women, with a clinical performance of sensitivity of 86.3%, specificity of 80.4%, and a highest AUC of 0.89 [30]. In a Dutch cohort, Verhoef et al. [25] reported that ASCL1m, with the highest AUC (0.844), showed better performance than ZIC1m (AUC = 0.725) and SSTm (AUC = 0.720) for CIN3+ detection among candidate methylation markers. In our data (Fig. 2 and Additional file 1: Table S3), the performance of ZIC1m in discerning CIN3+ in hrHPV-positive women was better than that of ASCL1m. Use of ZIC1m in hrHPV-positive women could decrease colposcopy referral rates (31.4% vs. 20.3%) compared with cytology and avoid missed diagnoses of cancer subjects.
The SOX1 protein is important in developmental processes as a transcription factor. The study showed that SOX1 might be a tumor suppressor in cervical cancer partly through the Wnt/β-catenin signaling pathway [31]. Furthermore, the expression level of SOX1 was higher in the normal groups than in the CC and CIN groups [32]. Hypermethylation of SOX1, resulting in decreased expression, was recognized as a potential biomarker for high-grade lesions. In the present study, SOX1m had a specificity of 81.8% in hrHPV‐positive scrapings, detecting CIN3+ (Additional file 1: Table S3) with a similar sensitivity (83%), which was better than the specificities previously published (74%) [26]. Compared to the results reported previously, the performance of SOX1m in detecting CIN3+ (sensitivity: 83.3% and specificity: 81.8%) in our data was better than that of the two commercial methylation-specific PCR assays [21] (GynTect®: sensitivity: 66.7% and specificity: 84.1%; QIAsure methylation test: sensitivity: 78.6% and specificity: 68.2%) in hrHPV‐positive scrapings and poorer than that of GynTect® (sensitivity: 94.1% and specificity: 68.4%) performed at three rural sites in China [22]. In comparison to the Slovenian population, high sensitivity of SOX1m was observed among methylation markers for CIN3+ instead of EPB41L3m in our study. Although our goal was to evaluate the biomarker potential of candidate gene methylation to triage hrHPV-positive women, we also observed elevated SOX1m in a hrHPV-negative woman (Additional file 1: Fig. S2). We used 14 cases of CIN3+ and 60 cases of CIN2- for the calculation. Notably, all 8 cancer cases were detected by SOX1m. This suggests that analysis of methylation may help identify women at risk of developing cervical cancer regardless of hrHPV status.
In addition to cervical scrapes, DNA methylation analysis in urine is also feasible. Many women felt unpleasant after experiencing the collection of cervical scrapes. Urine as a kind of noninvasive sample including cervicovaginal secretions, is easily accepted by patients, offering an effective solution to attract non-responders. The clinical performance of ZICm discerning CIN3+ from CIN2- in scrapes was higher than that in urine (AUC = 0.558, 95% CI 0.400–0.742) [33], whereas methylation analysis of SOX1 was not yet reported, which could be considered in future trials.
The strength of our study is the analysis of the DNA methylation of sixteen candidate genes with MSP in the same batch of clinical samples. Despite the expense of whole genome methylation sequencing, different ethnic groups should be taken into account before translating the available results to the clinic. Our findings underscore the essentiality of verifying methylation biomarkers in different nationalities or populations. The study is cross-sectional without follow-up, which is a major limitation. It is necessary to ascertain the optimal reassessment interval for hrHPV-positive women who test negative for SOX1m by longitudinal evaluation. Another limitation of this study is quantity bias due to the small sample size. Although subjects were collected randomly from women who met the criteria, the population in the methylation test may not represent all women. Our study focuses on CIN3+ rather than CIN2+ to evaluate clinical performance. It is moderately reproducible when women are diagnosed with CIN2. In addition, young CIN2 patients have a relatively high regression rate [34]. The CONCERVE study [19] suggested that women with untreated CIN2/3 and negative methylation results showed clinical regression. This might reveal that excessive improvement of methylation test performance in detecting CIN2+ without other combination test strategies could result in excessive attention and considerable overtreatment.
Conclusion
The performance of the candidate methylation markers was evaluated in the same batch of samples, which could provide a basis for future studies related to potential precancerous lesion/cancer methylation markers in the Chinese population. The data of our study show that the performance of SOX1m has a high sensitivity among candidate methylation markers for CIN3+ in the Chinese cohort. Meanwhile, it is a promising biomarker of triage in hrHPV-positive women for colposcopy referral. Further studies are still warranted in screening populations.
Availability of data and materials
The datasets used and analyzed in the current study are available where appropriate from the corresponding author on reasonable request.
Abbreviations
- ASCL1:
-
Achaete-scute family bHLH transcription factor 1
- ASCUS:
-
Atypical squamous cells of undetermined significance
- AUC:
-
The area under the curve
- BOLL:
-
Boule homolog, RNA binding protein
- CC:
-
Cervical cancer
- CCDC181:
-
Coiled-coil domain containing 181
- CI:
-
Confidence interval
- CIN2:
-
Cervical intraepithelial neoplasia grade 2
- CIN3:
-
Cervical intraepithelial neoplasia grade 3
- Ct:
-
Cycle threshold
- FAM19A4:
-
Family with sequence similarity 19 (chemokine (C–C motif)-like) member A4
- gDNA:
-
Genomic DNA
- GFRA1:
-
GDNF family receptor alpha 1
- HPV:
-
Human papillomaviruses
- hrHPV:
-
High-risk human papillomavirus
- JAM3:
-
Junctional adhesion molecule 3
- LSIL:
-
Low-grade squamous intraepithelial lesion
- MIR124-2:
-
MicroRNA 124-2
- miR129-2:
-
MicroRNA 129-2
- MSP:
-
Methylation-specific PCR
- PAX1:
-
Paired box gene 1
- PCDHA13:
-
Protocadherin alpha 13
- ROC:
-
Receiver operating characteristic
- SORCS1:
-
Sortilin related VPS10 domain containing receptor 1
- SOX1:
-
SRY-box transcription factor 1
- TCT:
-
Thinprep cytologic test
- ZIC1:
-
Zinc finger protein of the cerebellum 1
References
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Wang KH, Lin CJ, Liu CJ, et al. Global methylation silencing of clustered proto-cadherin genes in cervical cancer: serving as diagnostic markers comparable to HPV. Cancer Med. 2015;4(1):43–55.
Xia C, Dong X, Li H, et al. Cancer statistics in China and United States, 2022: profiles, trends, and determinants. Chin Med J (Engl). 2022;135(5):584–90.
Rimel BJ, Kunos CA, Macioce N, Temkin SM. Current gaps and opportunities in screening, prevention, and treatment of cervical cancer. Cancer. 2022.
Allanson ER, Schmeler KM. Preventing cervical cancer globally: are we making progress? Cancer Prev Res (Phila). 2021;14(12):1055–60.
Maver PJ, Poljak M. Primary HPV-based cervical cancer screening in Europe: implementation status, challenges, and future plans. Clin Microbiol Infect. 2020;26(5):579–83.
PATH. Global HPV Vaccine Introduction Overview. 2022; https://www.path.org/resources/global-hpv-vaccine-introduction-overview/.
Crosbie EJ, Einstein MH, Franceschi S, Kitchener HC. Human papillomavirus and cervical cancer. Lancet. 2013;382(9895):889–99.
Arbyn M, Simon M, Peeters E, et al. 2020 list of human papillomavirus assays suitable for primary cervical cancer screening. Clin Microbiol Infect. 2021;27(8):1083–95.
Zhang J, Zhao Y, Dai Y, et al. Effectiveness of high-risk human papillomavirus testing for cervical cancer screening in china: a multicenter, open-label, randomized clinical trial. JAMA Oncol. 2021;7(2):263–70.
Fontham ETH, Wolf AMD, Church TR, et al. Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA Cancer J Clin. 2020;70(5):321–46.
Gottschlich A, Gondara L, Smith LW, et al. Human papillomavirus-based screening at extended intervals missed fewer cervical precancers than cytology in the HPV For Cervical Cancer (HPV FOCAL) trial. Int J Cancer. 2022;151(6):897–905.
El Aliani A, El-Abid H, El Mallali Y, Attaleb M, Ennaji MM, El Mzibri M. Association between gene promoter methylation and cervical cancer development: global distribution and a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2021;30(3):450–9.
Molina MA, CarosiDiatricch L, Castany Quintana M, Melchers WJ, Andralojc KM. Cervical cancer risk profiling: molecular biomarkers predicting the outcome of hrHPV infection. Expert Rev Mol Diagn. 2020;20(11):1099–120.
Kremer WW, Steenbergen R, Heideman D, Kenter GG, Meijer C. The use of host cell DNA methylation analysis in the detection and management of women with advanced cervical intraepithelial neoplasia: a review. BJOG. 2021;128(3):504–14.
Zhu P, Xiong J, Yuan D, et al. ZNF671 methylation test in cervical scrapings for cervical intraepithelial neoplasia grade 3 and cervical cancer detection. Cell Rep Med. 2023;4(8):101143.
van Leeuwen RW, Oštrbenk A, Poljak M, van der Zee AGJ, Schuuring E, Wisman GBA. DNA methylation markers as a triage test for identification of cervical lesions in a high risk human papillomavirus positive screening cohort. Int J Cancer. 2019;144(4):746–54.
Kong L, Wang L, Wang Z, et al. DNA methylation for cervical cancer screening: a training set in China. Clin Epigenetics. 2020;12(1):91.
Kremer WW, Dick S, Heideman DAM, et al. Clinical regression of high-grade cervical intraepithelial neoplasia is associated with absence of FAM19A4/miR124-2 DNA methylation (CONCERVE study). J Clin Oncol. 2022;40(26):3037–46.
Louvanto K, Aro K, Nedjai B, et al. Methylation in predicting progression of untreated high-grade cervical intraepithelial neoplasia. Clin Infect Dis. 2020;70(12):2582–90.
Dippmann C, Schmitz M, Wunsch K, et al. Triage of hrHPV-positive women: comparison of two commercial methylation-specific PCR assays. Clin Epigenetics. 2020;12(1):171.
Zhang L, Zhao X, Hu S, et al. Triage performance and predictive value of the human gene methylation panel among women positive on self-collected HPV test: results from a prospective cohort study. Int J Cancer. 2022;151(6):878–87.
Harper DM. Cervical cancer elimination is dependent on women’s self-tests for primary human papillomavirus testing triaged by methylation status. J Clin Oncol. 2022;40(26):3003–5.
Vrba L, Futscher BW. A suite of DNA methylation markers that can detect most common human cancers. Epigenetics. 2018;13(1):61–72.
Verhoef L, Bleeker MCG, Polman N, et al. Performance of DNA methylation analysis of ASCL1, LHX8, ST6GALNAC5, GHSR, ZIC1 and SST for the triage of HPV-positive women: results from a Dutch primary HPV-based screening cohort. Int J Cancer. 2022;150(3):440–9.
Li N, Hu Y, Zhang X, et al. DNA methylation markers as triage test for the early identification of cervical lesions in a Chinese population. Int J Cancer. 2021;148(7):1768–77.
Adcock R, Nedjai B, Lorincz AT, et al. DNA methylation testing with S5 for triage of high-risk HPV positive women. Int J Cancer. 2022;151(7):993–1004.
Gu X, Guo XK, Chen BH, Gao XJ, Chen F, Liu Q. Prognostic and clinicopathological value of ZIC1 in patients with cervical squamous cell carcinoma. Oncol Lett. 2019;18(6):6621–7.
Dick S, Verhoef L, De Strooper LM, et al. Evaluation of six methylation markers derived from genome-wide screens for detection of cervical precancer and cancer. Epigenomics. 2020;12(18):1569–78.
Verlaat W, Snijders PJF, Novianti PW, et al. Genome-wide DNA methylation profiling reveals methylation markers associated with 3q gain for detection of cervical precancer and cancer. Clin Cancer Res. 2017;23(14):3813–22.
Lin YW, Tsao CM, Yu PN, Shih YL, Lin CH, Yan MD. SOX1 suppresses cell growth and invasion in cervical cancer. Gynecol Oncol. 2013;131(1):174–81.
Dudea-Simon M, Mihu D, Pop LA, et al. Alteration of gene and miRNA expression in cervical intraepithelial neoplasia and cervical cancer. Int J Mol Sci. 2022;23(11).
Van Keer S, van Splunter AP, Pattyn J, et al. Triage of human papillomavirus infected women by methylation analysis in first-void urine. Sci Rep. 2021;11(1):7862.
Ehret A, Bark VN, Mondal A, Fehm TN, Hampl M. Regression rate of high-grade cervical intraepithelial lesions in women younger than 25 years. Arch Gynecol Obstet. 2022.
Acknowledgements
We sincerely thank all participants in the study.
Funding
This research was supported by the National Natural Science Foundation (NNSF) of China (81973401) and Natural Science Foundation of Hunan Province (2023JJ60077).
Author information
Authors and Affiliations
Contributions
PC and QL conceived and designed the study. YL and JX acquired patient samples and clinical information. YC, PZ, YA and SL acquired data and performed the data analysis. YC wrote the first draft of the manuscript. QL supervised the study. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The protocol was approved by the local ethical committees where applicable (No. 202101007). All patients gave written informed consent before participation in this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1. Primer sequence of 16 candidate methylation genes. Table S2. Sensitivity, specificity, and cut-off of candidate gene DNA methylation markers differentiated between CIN2- and CIN3+ detection. Fig. S1. Sixteen genes methylation positivity in cervical scrapings (n = 82). The distribution of the methylation positivity of the 16 candidate markers in ≤CIN1, CIN2, CIN3, and CC group. Table S3. Sensitivity and specificity of cytology and DNA methylation for detecting CIN3+ in hrHPV-positive women. Fig. S2. SOX1m analysis in the Chinese cohort.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, Y., Chen, Y., Xiong, J. et al. Performance of DNA methylation analysis in the detection of high-grade cervical intraepithelial neoplasia or worse (CIN3+): a cross-sectional study. Infect Agents Cancer 18, 77 (2023). https://doi.org/10.1186/s13027-023-00555-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13027-023-00555-2