Abstract
Background
Cervical cancer is one of the most common cancers in women. Evidences show that, routine immunization of girls at age 14 year and immunization of girls at age 9 year through a 5 years extended interval between doses are the most efficient to control the disease. Despite this, there is very little information on parents’ willingness to accept the human papilloma virus vaccine. Therefore, assessing willingness to accept human papilloma virus vaccination and its associated factors among parents with eligible daughter will help to designing, implementing and monitoring effectiveness of HPV vaccine immunization program.
Methods
A community-based cross-sectional study was conducted among 386 parents with eligible daughters from 8July–6August, 2022. The multistage sampling technique was used. Data was collected using an interviewer-administered questionnaire. Responses were coded and entered into the computer using EPI data version 4.606 statistical packages, and SPSS version 23 was used for data analysis. Frequencies, percentages and means were as to describe the study variables in relation to the participants. Bivariable and multivariable logistic regression were employed. The statistical significance was set at a p-value of < 0.05 with its respected odds ratio.
Results
A total of 386 study participants were included in the study. Among participants, 80.3% (95% CI: 76.3, 84) were willing to vaccinate their daughters for HPV vaccination. The parents’ willingness was affected by the male parents ([AOR = 3.5; 95% CI (1.673–7.371)], fear of side effects [AOR = 0.385; 95% CI (0.206–0.718)], and with poor awareness on the HPV vaccine [AOR = 0.483; 95% CI (0.259- 0.900)].
Conclusion
The study has shown that willingness to accept the HPV vaccine is about 80% and significantly affected with parental sex, information on the HPV vaccine, and fear of side effects. As such, it may be helpful for the health care providers and the health care policy makers to emphasize on providing easily understandable information using mass media and social campaign. In addition giving trainings more targeted to female parents might be important.
Similar content being viewed by others
Introduction
The projected incidence of cervical cancer(CC) is 13.1 per 100,000 women worldwide but varied extensively in different regions of the globe, with less than 2 per 100,000 women in economically advanced nations to 75/100,000 in low income developing nations [1]. It is the main cause of cancer related mortalities among women in Africa [1].
In the absence of vaccination against human papilloma virus (HPV), 11.6 million cases of CC are expected by 2094 in the globe [2]. About 75% of the disease burden is concentrated in 25 countries mostly found in Africa and Asia [2]. Global immunization with HPV vaccine targeted to HPV types 16 and 18, with cross-protection against HPV types 31, 33, and 45, might prevent about 8.7 million cases [2, 3].
There are more than 100 kinds of HPV types of which at least 14 are cancer-causing.
HPV is mainly transmitted through sexual contact and most people are infected with shortly after the onset of sexual activity. Two HPV types (16 and 18) cause about 70% of cervical cancers and pre-cancerous cervical lesions causing squamous intraepithelial lesions [4,5,6].
The two effective vaccines composed of HPV strains 16 and 18 are primary prevention strategies of HPV which is the main cause of CC [7]. Strategies involving vaccinating girls aged 9–14 with two doses are predicted to be the most cost-effective in low- and middle-income countries [8]. Evidences showed that, routine immunization of girls at age 14 year and immunization of girls at age 9 year through a 5 years extended interval between doses and a catch up programme at age 14 years are the most efficient to control this cancer [9, 10].
Despite this fact, there is no information regarding the HPV vaccine acceptance and associated factors among parents with eligible daughters in the study setting. Therefore, the aim of this study was to assess willingness to accept human papilloma virus vaccine and its associated factors among parents with eligible daughter in Addis Zemen town, Northwest Ethiopia.
Methods and materials
Study design, period and area
A community-based cross-sectional study was conducted from July 8–August 6, 2022. This study was conducted in Addis Zemen town which is located in the Northwestern part of Ethiopia. It is around 637 km away from Addis Ababa, the capital city of Ethiopia and 82 km from Bahir Dar city. According to the current statistics, the town has 4 kebeles and a total of 198,374 population [11].
Populations
The source population for this study was all parents who had eligible daughter living in Addis Zemen town and the study population was all parents who had eligible daughter in selected kebele at Addis Zemen during the study period. Parents with psychiatric disorder and severely ill during the study period were excluded in the study.
Sample size determination
The sample size was calculated by using single population proportion formula considering 81.3% vaccine acceptance [12], 95% confidence interval (CI), 5% margin of error (d) and 1.5 design effect:
n = (Zα/2)2p (1-P)
d2
Where, n = initial sample size
Z = 1.96 the corresponding Z-score for the 95% CI
P = Proportion = 81.3%
W = Margin of error = 5%= 0.05
n= \(\frac{\left(1.96\right)2 \text{x} 0.813(1-0.813)}{\left(0.05\right)2}\)= 233.6≈234
This sample size multiplied by design effect of 1.5 and adding 10% non-response rate gives 386.
Sampling technique and procedure
The multistage sampling method was used. There are four kebeles, and two kebeles were selected by a simple random method and from the selected kebeles, 386 participants were selected by an identification number that was given after a house-to-house visit. Then, a proportional-to-size allocation technique was employed to determine the study participants from each kebele. Finally, the study participants were selected by a simple random sampling method.
Operational definitions
Eligible daughter- young daughters aged 9-14years.
Knowledge- There were 16 knowledge questions and every questions have yes, no and I don’t know answer and if the study participant answered 0–4 ‘yes’ out of 16 items was considered as “poor knowledge”, 5–12 “moderate Knowledge”, and 13 − 16 “good knowledge” [12].
Attitude-There were 10 questions. Every questions have yes/no answer and if the study participant answered 0–5 ‘yes’ out of 10 items was considered as having negative and 6–10 positive attitude [13].
Willingness to accept the vaccine – using the question, “Are you willing to vaccinate your daughter for HPV vaccination that can protect against HPV infection?“(options: Yes/No). Those who answered “yes” were considered are willing to accept HPV vaccine and those who answered “no” were considered as they aren’t willing to accept HPV vaccine [12].
Data collection tools and procedures
Data were collected using structured interviewer administrated questionnaire adapted from the literature [12]. The face-to-face interview method was used to collect all relevant information from respondents. Three nurses with BSc degree were involved in data collection process. For the case if more than one parents were available in the household, data collectors has selected one parent using a lottery method to make interview.
Data quality control
The questionnaire was prepared in English and translated to the local language (Amharic) by language experts, and back-translated to English to check for consistency of the questionnaire. Before the actual data collection, pre-test was conducted among 5% of the sample size in kebeles other than selected kebeles to evaluate the clarity of questions and validity of the instrument and reaction of respondents to the questions. Every day, all questionnaires were reviewed and checked at the end of the data collection period, and any errors were corrected accordingly with the supervisor and data collectors. Two nurses with MSc educational level supervised the data collection process.
Data processing and analyzing
After data collection, each questionnaire was checked for completeness and consistency. Responses were coded and entered into the computer using EPI data version 4.606 statistical packages, and SPSS version 23 was used for data analysis. Descriptive statistics like frequencies, percentages and mean were used to describe the study participants in relation to the study variables. Binary logistic regression model was used to identify factors associated with the outcome variable. Variables at a p value < 0.2 in the bivariable analysis were included in the multivariable analysis. Explanatory Variables with p-value < 0.05 and with their respected odds ratio in multivariable analysis were declared as statistically significant.
Results
Socio-demographic characteristics
A total of 386 participants were included in this study with a response rate of 100%. The mean age of the respondents was 44.55 years and 140 (36.3%) of the participants were found in the age group between 30 and 39 years and 251 (65%) of respondents were female (Table 1).
Knowledge towards cervical cancer
One hundred eight six (48.2%) study participants had poor knowledge, 160(41.5%) had moderate knowledge, and 40 (10.1%) had good knowledge towards cervical cancer (Table 2).
Attitude towards HPV vaccine
From the study participants, 289 (74.9%) had a positive attitude, and the rest, 97 (25.1%), had a negative attitude (Table 3).
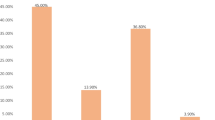
Information about HPV vaccine and related characteristics
Among study participants, 302 (78.2%) heard about the HPV vaccine, 202 (52.3%) feared the vaccine’s side effects for their daughters, and almost all participants think the vaccine price is zero (94.8%)(Fig. 1).
Willingness to accept HPV vaccine
From the total study participants, 80.3%(95%CI:76.3–84) were willing to accept the HPV vaccine for their daughters that can protect HPV infection, and 64.8% of the participants’ daughters got the vaccine before and of which the majority got it in school (Fig. 2).
Factor associated with willingness to accept HPV vaccine
Binary logistic regression analysis model was employed to identify factors that affect the willingness to accept HPV vaccine. In bivariable analysis, sex, income, educational status, occupation, fear of side effects, and information on the HPV vaccine were associated to the outcome variable at p-value < 0.2. Then, sex, fear of side effects and information on the HPV vaccine were significantly associated to vaccine acceptance at p-value < 0.05 in multivariable analysis.
The study revealed that male parents were about 3.5 times more likely to accept HPV vaccine than female parents [AOR = 3.51; 95% CI (1.673–7.371)].
The study also showed that parents who had a fear of side effects of the HPV vaccine were about 61.5% less likely to accept the vaccine as compared to those who had no fear of side effects [AOR = 0.385; 95% CI (0.206–0.718)].
Parents who had no information on the HPV vaccine were 51.7% less likely to accept the HPV vaccine for their daughters than those who had information [AOR = 0.48; 95% CI (0.25–0.90)] (Table 4).
Discussion
The study was conducted to assess the willingness to accept HPV vaccine and associated factors among parents with eligible daughters in Addis Zemen town.
The study showed that more than 80% of the study participants were willing to accept the HPV vaccine to be given for their eligible daughters. This finding is aligned with studies done in Gondar (81.3%) [14] and Nigeria (81.8%) [15], south Africa (80%) [16] and Denmark (80%) [17]. However, several studies conducted in different study settings such as Addis Ababa (94.3%) [18], Kenya (89%) [19], Tanzania (93%) [20], Honduras (91%) [21] and Malaysia (87.1%) [22] Shows higher acceptance level than the current finding. This discrepancy may be due to socio cultural, literacy level, study setting and health policy differences of the respected countries.
This finding also revealed that the sex of the parents was statistically associated with willingness to accept the vaccine. The current finding shows that males are more likely to show willingness to accept the HPV vaccine, unlike other studies reveal as females show greater willingness than males, like studies conducted in Spain [23] and European countries [24]. This may be due to males are more exposed to the information related to the vaccine in different public meeting and social media than females in the current study area. This is as males are more expected to engage in the outdoor activities but on the contrary females according to the community’s socio cultural context in the study setting and the region at all.
The current research finding revealed that fear of side effects made study participant less likely to accept the HPV vaccine. This finding is aligned with studies done in Hong Kong [25], and China [26]. People prefer not to get vaccines for a variety of reasons, but the main ones are a lack of trust in vaccine safety and fears about side effects [27].
Additionally, this study revealed that information on HPV vaccination was significantly associated with willingness to accept the vaccine. This finding was consistent with a study done in Gondar [12] and Addis Ababa [18]. This might be due to confusion or a lack of information, which are common factors for vaccine hesitancy [28]. Parents who received information about the HPV vaccine may know more about the vaccine property, where it is given, and who gets vaccinated. This might helped informed parents to be willing to accept the HPV vaccine for their daughters.
Conclusion
The study has shown that willingness to accept the HPV vaccine is about 80% and it was significantly affected with parental sex, information on the HPV vaccine, and fear of side effects. It may be helpful for the health care providers and the health care policy makers to emphasize on providing easily understandable information related to the vaccine using mass media and social campaign. Furthermore, the HPV acceptance rate will be increased if information is disseminated for female parents as well.
Limitations of the study
This study is cross sectional in nature, so it shares the limitations of cross sectional study design. In addition, there may be social desirability bias which may inflate the proportion of HPV acceptance rate.
Data Availability
Data will be available upon request from the corresponding author.
Abbreviations
- AOR:
-
Adjusted Odd Ratio
- CDC:
-
Centers for Disease Control and Prevention
- CI:
-
Confidence Interval
- COR:
-
Crude Odd Ratio
- HPV:
-
Human Papilloma virus
- SPSS:
-
Statistical Package for the Social Sciences
References
Arbyn M, Weiderpass E, Bruni L, de Sanjosé S, Saraiya M, Ferlay J, et al. Estimates of incidence and mortality of Cervical cancer in 2018: a worldwide analysis. The Lancet Global Health. 2020;8(2):e191–e203.
Bonjour M, Charvat H, Franco EL, Piñeros M, Clifford GM, Bray F, et al. Global estimates of expected and preventable cervical cancers among girls born between 2005 and 2014: a birth cohort analysis. The Lancet Public Health. 2021;6(7):e510–e21.
Abbas K, Zandvoort Kv, Brisson M, Jit M. Effects of Demography, Disability weights and Cervical Cancer Burden on HPV Vaccination Impact estimates in 177 countries: PRIME modelling study. Disability weights and Cervical Cancer Burden on HPV Vaccination Impact estimates in. 2019;177.
Organization WH. Human papillomavirus vaccines: WHO position paper. May 2017–Recommendations Vaccine. 2017;35(43):5753–5.
Burd EM. Human papillomavirus and Cervical cancer. Clin Microbiol Rev. 2003;16(1):1–17.
Ma L, Lei J, Ma L, Cong X, Wang N, Yang H, et al. Characteristics of women infected with human papillomavirus in a tertiary hospital in Beijing China, 2014–2018. BMC Infect Dis. 2019;19(1):1–8.
Crosbie EJ, Einstein MH, Franceschi S, Kitchener HC. Human papillomavirus and Cervical cancer. The Lancet. 2013;382(9895):889–99.
Shet A, Bar-Zeev N. Human papillomavirus vaccination strategies for accelerating action towards Cervical cancer elimination. The Lancet Global Health. 2023;11(1):e4–e5.
Drolet M, Laprise J-F, Martin D, Jit M, Bénard É, Gingras G, et al. Optimal human papillomavirus vaccination strategies to prevent Cervical cancer in low-income and middle-income countries in the context of limited resources: a mathematical modelling analysis. Lancet Infect Dis. 2021;21(11):1598–610.
Farmer E, Cheng MA, Hung CF, Wu TC. Vaccination strategies for the control and treatment of HPV Infection and HPV-Associated Cancer. Recent Results in cancer Research Fortschritte Der Krebsforschung Progres dans les recherches sur le cancer. 2021;217:157–95.
Wondimeneh Y, Takele Y, Atnafu A, Ferede G, Muluye D. Trend analysis of visceral Leishmaniasis at Addis Zemen health center, Northwest Ethiopia. Biomed Res Int. 2014;2014.
Alene T, Atnafu A, Mekonnen ZA, Minyihun A. Acceptance of human papillomavirus vaccination and associated factors among parents of daughters in Gondar town, Northwest Ethiopia. Cancer Manage Res. 2020;12:8519.
Sinshaw MT, Berhe S, Ayele SG. Knowledge and attitude towards Human Papillomavirus Vaccine and Associated factors among mothers who have eligible daughters in Debre Markos Town, Northwest Ethiopia. Infect Drug Resist. 2022;15:781.
Alene T, Atnafu A. Acceptance of Human Papillomavirus Vaccination and Associated factors among parents of daughters in Gondar Town. Northwest Ethiopia. 2020;12:8519–26.
Okunade KS, Sunmonu O, Osanyin GE, Oluwole AA. Knowledge and acceptability of human papillomavirus vaccination among women attending the gynaecological outpatient clinics of a university teaching hospital in Lagos, Nigeria. Journal of Tropical Medicine. 2017;2017.
Hoque ME. Acceptability of human papillomavirus vaccination among academics at the University of KwaZulu-Natal, South Africa. South Afr Family Pract. 2015;57(5):318–21.
Mortensen GL. Parental attitudes towards vaccinating sons with human papillomavirus vaccine. Dan Med Bull. 2010;57(12):A4230.
Dereje N, Ashenafi A, Abera A, Melaku E, Yirgashewa K, Yitna M, et al. Knowledge and acceptance of HPV vaccination and its associated factors among parents of daughters in Addis Ababa, Ethiopia: a community-based cross-sectional study. Infect Agents Cancer. 2021;16(1):1–7.
Masika MM, Ogembo JG, Chabeda SV, Wamai RG, Mugo N. Knowledge on HPV vaccine and Cervical cancer facilitates vaccine acceptability among school teachers in Kitui County, Kenya. PLoS ONE. 2015;10(8):e0135563.
Cunningham MS, Skrastins E, Fitzpatrick R, Jindal P, Oneko O, Yeates K, et al. Cervical cancer screening and HPV vaccine acceptability among rural and urban women in Kilimanjaro Region, Tanzania. BMJ open. 2015;5(3):e005828.
Perkins RB, Langrish SM, Cotton DJ, Simon CJ. Maternal support for human papillomavirus vaccination in Honduras. J Women’s Health. 2011;20(1):85–90.
Ezat SWP, Hod R, Mustafa J, Mohd Dali AZH, Sulaiman AS, Azman A. National HPV immunisation programme: knowledge and acceptance of mothers attending an obstetrics clinic at a teaching hospital, Kuala Lumpur. Asian Pac J Cancer Prev. 2013;14(5):2991–9.
López N, Salamanca de la Cueva I, Vergés E, Suarez Vicent E, Sánchez A, López AB, et al. Factors influencing HPV knowledge and vaccine acceptability in parents of adolescent children: results from a survey-based study (KAPPAS study). Hum Vaccines Immunotherapeutics. 2022;18(1):2024065.
Lee Mortensen G, Adam M, Idtaleb L. Parental attitudes towards male human papillomavirus vaccination: a pan-european cross-sectional survey. BMC Public Health. 2015;15(1):1–10.
Wong CK, Man KK, Ip P, Kwan M, McGhee SM. Mothers’ preferences and willingness to pay for human papillomavirus vaccination for their daughters: a discrete choice experiment in Hong Kong. Value in Health. 2018;21(5):622–9.
Lin Y, Su Z, Chen F, Zhao Q, Zimet GD, Alias H, et al. Chinese mothers’ intention to vaccinate daughters against human papillomavirus (HPV), and their vaccine preferences: a study in Fujian Province. Hum Vaccines Immunotherapeutics. 2021;17(1):304–15.
Geoghegan S, O’Callaghan KP, Offit PA. Vaccine safety: myths and misinformation. Front Microbiol. 2020;11:372.
sciences nml. What are the Main Causes of Vaccine Hesitancy? What are the Main Causes of Vaccine Hesitancy? 2022. Available from: https://www.news-medical.net/health/What-are-the-Main-Causes-of-Vaccine-Hesitancy.aspx.
Acknowledgements
The authors would like to acknowledge University of Gondar, Addis Zemen City administration office and data collectors.
Funding
The authors didn’t receive any funding.
Author information
Authors and Affiliations
Contributions
MW: Involved in conceptualization, design, analysis, interpretation, report and manuscript writing. AFZ: involved in design, analysis, and interpretation. WW: involved in interpretation, report, and manuscript writing. TS: involved in analysis, report, and manuscript writing. TE: conceptualization, involved in interpretation, report, and design. DAG: involved in interpretation, report, design and manuscript writing.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Ethical clearance and support letters were obtained from the Ethical Review Committee (ERC) of the University of Gondar College of Medicine and health Sciences, School of nursing and it was submitted and approved by the Ethical Review Committee (S/N/163/7/2014). The support letter was submitted to Addis Zemen town administration. Then, permission was obtained from the City administration.
Informed consent was obtained from all study participants before the data collection. In addition, participants who were unwilling to take part in the study and those who needed to quit their participation at any stage were informed to do so without any restriction. Study participants’ privacy, secrecy, and wellbeing were protected. The names of the participants were anonymous and all the collected data was protected with strong password. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declared that there is no competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wassie, M., Zegeye, A.F., Worku, W. et al. Willingness to accept human papilloma virus vaccination and its associated factors among parents with eligible daughters in Addis Zemen town, Northwest Ethiopia. Infect Agents Cancer 18, 84 (2023). https://doi.org/10.1186/s13027-023-00551-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13027-023-00551-6