Abstract
Background
Despite successful combined antiretroviral therapy (cART), the risk of non-AIDS defining cancers (NADCs) remains higher for HIV-infected individuals than the general population. The reason for this increase is highly disputed. Here, we hypothesized that T-cell receptor (TCR) γδ cells and/or mucosal-associated invariant T (MAIT) cells might be associated with the increased risk of NADCs. γδ T cells and MAIT cells both serve as a link between the adaptive and the innate immune system, and also to exert direct anti-viral and anti-tumor activity.
Methods
We performed a longitudinal phenotypic characterization of TCR γδ cells and MAIT cells in HIV-infected individuals developing Hodgkin’s lymphoma (HL), the most common type of NADCs. Cryopreserved PBMCs of HIV-infected individuals developing HL, matched HIV-infected controls without (w/o) HL and healthy controls were used for immunophenotyping by polychromatic flow cytometry, including markers for activation, exhaustion and chemokine receptors.
Results
We identified significant differences in the CD4+ T cell count between HIV-infected individuals developing HL and HIV-infected matched controls within 1 year before cancer diagnosis. We observed substantial differences in the cellular phenotype mainly between healthy controls and HIV infection irrespective of HL. A number of markers tended to be different in Vδ1 and MAIT cells in HIV+HL+ patients vs. HIV+ w/o HL patients; notably, we observed significant differences for the expression of CCR5, CCR6 and CD16 between these two groups of HIV+ patients.
Conclusion
TCR Vδ1 and MAIT cells in HIV-infected individuals developing HL show subtle phenotypical differences as compared to the ones in HIV-infected controls, which may go along with functional impairment and thereby may be less efficient in detecting and eliminating malignant cells. Further, our results support the potential of longitudinal CD4+ T cell count analysis for the identification of patients at higher risk to develop HL.
Similar content being viewed by others
Introduction
Combined antiretroviral therapy (cART) is highly efficient in suppressing HIV replication with life expectancies of HIV-infected individuals nowadays being almost similar to the general population [1,2,3,4]. In particular, a significant decline of AIDS-defining cancers (ADCs), such as Kaposi Sarcoma and non-Hodgkin’s lymphoma, has been observed upon cART [5,6,7]. Strikingly, the percentage of cancer-induced death increased from approximately 10% in the pre-cART era to 28% in the era of cART [8, 9]. The increased cancer burden observed is associated with a higher risk of HIV-infected individuals to develop non-AIDS defining cancers (NADCs) including lung cancer, colorectal cancer, hepatocellular carcinoma, anal cancer, and Hodgkin’s lymphoma (HL) [10,11,12,13,14]. The overall risk of those cancers is three-fold higher for HIV-infected individuals than for the general population and even 5 to 30-fold higher for HL, the most common type of NADCs [10, 15,16,17].
NADCs are associated with many factors including antiretroviral drug toxicity, aging, and known risk factors such as alcohol and tobacco smoking, but they do not fully explain the higher risk of HIV-infected people to suffer from NADCs [18,19,20]. Moreover, chronic immune activation, persistent immunodeficiency, as well as co-infections seem to contribute to this increased risk [10, 21,22,23]. In HIV-infected individuals, for example, almost all cases of HL are associated with EBV infection versus 40% in the general population [24]. In addition, they are also more likely to develop mixed cellular and lymphocyte-depleted subtypes of HL, which are associated with a less favorable outcome than the nodular sclerosis subtype, which is predominant in the general population [25, 26]. The higher incidence rate and development of subtypes with less favorable outcome might be linked to HIV-associated immune dysfunction such as the depletion and/or functional impairment of cells involved in immune surveillance against cancer [24, 27]. Even though the age-specific rates are projected to decrease through 2030 for a number of tumor types, most likely due to the timely treatment of HIV, we are currently challenged with a still increased incidence rate of HL [28]. In fact, in a recent study by Cornejo-Juarez et al., HL figured as the most frequent NADCs in an oncology unit [29].
Strong associations of low CD4+ T cell counts and ADCs are well proven, while associations of CD4+ T cell counts and NADCs are weaker or not observed for all NADCs [17, 19, 23, 30,31,32]. Further, the immediate initiation of cART reduces serious AIDS-related and non-AIDS related events [33, 34]. The START study, for example, showed a reduced risk for cancers (ADCs and NADCs) when cART was initiated immediately and irrespective of CD4+ T cell count but there was no evidence that this beneficial effect was associated with CD4+ T cell count or viral load [34, 35]. Thus, the higher risk for NADCs is not simply an equation of CD4+ T cell counts but likely involves more complex mechanisms of immune activation and immune surveillance.
TCR γδ cells and mucosal-associated invariant T (MAIT) cells are innate-like T lymphocytes with important functions in both innate and adaptive immune response [36,37,38,39]. TCR γδ cells express an invariant T cell receptor (TCR), composed of a gamma (γ) and a delta (δ) chain. They usually comprise 0.5–16% of all CD3+ T cells in the peripheral blood (PB) but can expand to up to 60% during bacterial and viral infections [40,41,42]. Based on their TCR Vδ chain usage, they can be divided into two major sub-populations; namely, Vδ1- and Vδ2-expressing cells. A minority of TCR γδ cells instead express Vδ chains other than these two. Tissue-associated TCR γδ T cells mostly express the TCR Vδ1 chain, whereas cells expressing the Vδ2 chain (usually paired with the Vγ9 chain, and therefore also called Vγ9Vδ2 cells) are the predominant population in the PB [43]. Upon HIV infection, an expansion of Vδ1 cells accompanied by a depletion of Vδ2 cells in the PB is observed, resulting in an inversion of the Vδ1/ Vδ2 ratio [44,45,46,47]. TCR γδ cells perform diverse functions and are also involved in anti-viral and anti-tumor activity [48]. They can rapidly secrete large amounts of IFN-γ, TNF-α, IL-4 and IL-17, and can act as potent cytotoxic effector cells against virus-infected and malignant cells through the release of perforin and granzyme-B [49,50,51,52]. These cells may also have a regulatory function via secretion of IL-10 and TGF-β with potential suppressive effects on anti-tumor function [53]. The role of TCR γδ cells in tumor immunity is not fully understood, and further analysis of individual populations based on the TCR-repertoire and functional heterogeneity is needed [54].
MAIT cells, which are abundant in the PB, mesenteric lymph nodes, liver and intestinal mucosa, are also involved in tumor immunity [55,56,57,58]. They express the semi-invariant TCR Vα7.2, paired with a limited Vβ repertoire and the C-type lectin CD161 [59, 60]. Similar to TCR γδ cells, MAIT cells can rapidly secrete cytokines, including IFN-γ, TNF-α, IL-17, and IL-22, and may also kill target cells [55, 59, 61, 62]. Early during HIV infection, MAIT cells are depleted and functionally impaired and like TCR γδ cells, do not fully recover upon long-term cART [63,64,65].
As MAIT and TCR γδ cells are involved in antitumor immunity, we hypothesized that the extent of their depletion and/or their phenotype differ between HIV-infected patients developing HL (prior to the diagnosis of HL) and HIV-infected matched controls. Notably, extensive characterization of immune cells in the PB of HIV-infected individuals over time may provide detailed insight on their immune reconstitution and on the phenotype of cellular populations with distinct functions, and could also provide useful predictors of disease progression. To address this possibility, we performed a detailed phenotypic characterization of TCR γδ and MAIT cells in the PB of HIV-infected individuals enrolled in the Swiss HIV Cohort Study (SHCS).
Material and methods
Swiss HIV cohort study (SHCS)
The SHCS (www.shcs.ch) is a prospective cohort study with ongoing enrollment of HIV-infected adults in Switzerland since 1988 [66]. It includes 73% of all diagnosed HIV-infections in Switzerland [67]. Representation has remained stable throughout the study duration. Detailed information on demographics, mode of HIV acquisition, risk behavior, clinical events, co-infections, and treatment is collected using a standard protocol at registration and at intervals of 6 months. Plasma samples are collected every 6–12 months in all study participants. Local ethical committees of all participating study sites approved the study and written consent was obtained from all participants.
Samples
Blood was obtained from healthy controls and HIV-infected patients with and without HL, which were enrolled in the Swiss HIV Cohort Study (SHCS). Peripheral blood mononuclear cells (PBMCs) were isolated using Lymphoprep gradients and cryopreserved. Within the SHCS demographic, clinical, laboratory and behavioral data are recorded at enrolment and at follow-up visits every 6 months. Samples were selected based on the following inclusion criteria: i) male, ii) ≥ 18 years, iii) Caucasian, iv) HIV RNA copies > 400 copies/ml, v) sample availability before cART, 1–2 years after suppression, and 0–1 years prior to HL diagnosis, i.e., for the HIV-patients w/o HL we chose the samples closest to the times of the corresponding matching HIV+ HL+ patients. Matching of cancer-free HIV-infected individual was done according to: i) gender, ii) ethnicity, iii) age, iv) sample availability, v) CD4+ T cell count (before cART), vi) HIV RNA copy number (before cART).
Flow Cytometry
Frequencies and cell count of conventional CD4+ and CD8+ T cells were determined throughout the study and provided by the SHCS, frequencies of unconventional γδ T cells and MAIT cells were determined retrospectively. Samples were analyzed on two consecutive days. To ensure comparability of the samples, all time points and matched control samples were stained and acquired on the same day. We checked for technical performance by analyzing one healthy control sample on both days. Cryopreserved PBMCs were thawed, washed, and resuspended in phosphate buffered saline (PBS). Cell number after thawing was determined with the COULTER® Ac · T diff™ Analyzer (Beckman Coulter). Three different polychromatic flow cytometry panels were used for the identification and characterization of γδ T cells and MAIT cells. Each staining step included incubation for 20 min at 4 °C. One million PBMCs were used per panel and stained with purified anti-TCRγδ (BD Bioscience) and the Zombie NIR Fixable Viability dye (BioLegend) in PBS with 2 mM. PBMCs were washed 2x and then stained with anti-mouse IgG (H + L) – Pacific Orange (Thermo Fisher Scientific) in FACS buffer (PBS containing 2% FBS and 0.05% sodium azide). PBMCs were washed 2x, followed by a 20 min blocking step with mouse serum (Thermo Fisher Scientific) at 4 °C. After blocking, cells were washed and surface staining with three different panels was performed. Each panel included anti-TCRVδ1 - PE-Vio770 (Miltenyi Biotec), anti-TCRVδ2 - PerCP (BioLegend), anti-CD161 - BV711 (BD Bioscience) and anti-TCRVα7.2 – BV785 (BioLegend), plus, Panel 1: anti-CCR5 – APC, anti-CCR6 – PE, anti-CXCR3 – PE-Dazzle, anti-CXCR4 – BV421, anti-CD38 – BV605, and anti-CD69 – FITC (all BioLegend); Panel 2: anti-NKG2D –BV605 (BD Bioscience), anti-CD94 – FITC, anti-Tim3 – PE-Dazzle, anti-PD-1 – BV421, anti-ILT2 – PE, anti-CD158b – APC (all BioLegend); and Panel 3: anti-CD16 – FITC (BD Bioscience), anti-KLRG1 – PE, anti-CTLA4 – BV421, anti-CD57 – PE-Dazzle, anti-CD56 – APC (all BioLegend). Before acquisition, cells were fixed with 1% paraformaldehyde. Samples were acquired on a BD LSR II Fortessa (BD Bioscience). Ultra Comp eBeads (Thermo Fisher Scientific) were used for compensation, except for anti-CD57 – PE-Dazzle and the Zombie NIR Fixable Viability dye, for which compensation was done with PBMCs. Anti- TCRVδ1 - PE-Vio770 was compensated using the MACS Comp bead Kit, anti REA (Miltenyi Biotec). Data were analyzed using FlowJo software (TreeStar). All results shown included gating on lymphocytes, single cells, and live cells. Detailed subset analysis of γδ T cells was performed by gating on TCRγδ+/TCRVδ1+ or on TCRγδ+/TCRVδ2+ cells. MAIT cells gated based on TCRVα7.2+/CD161+. Subset analysis was only performed when a threshold of 100 detected events for the parental population was reached.
Quantification and statistical analysis
Results on frequencies of δγ T cells, Vδ1, Vδ2 cells, and MAIT cells were extracted from all three panels. The mean frequency was calculated and used for further analysis. Data was only plotted when results were available for four or more patients per group. Statistical data analyses were performed using GraphPad Prism 8 software (GraphPad). The ROUT method was used for the identification of outliers. Data were subjected to a Wilcoxon signed-rank test or Kruskal-Wallis with Dunn’s multiple comparison test. P values were considered as significant at p < 0.05.
All analysis was performed within the R statistical computing environment, version 3.6.3 [68]. FACS data from the three panels (CCR, Exhaustion and NK) and population (MAIT, Gamma-delta VdX, Vd1 and Vd2) were analyzed independently, using a common analytical framework described here. Data was first zero-centered on gate-values for each marker and arcsin transformed before dimensional reduction and clustering using Rphenograph [69]. The proportions of HC, HIV+ w/o HL and HIV+ HL+ cells and median marker expression within each cluster were calculated and heatmapped to visualize phenotypic signatures. To train the SVM classifier, a training set containing equal numbers of cells from each of the three conditions was obtained by sampling using the caret package [70]. Training data for each population (MAIT, Gamma-delta VdX, Vd1 and Vd2) were used to build separate SVM model using the e1071 package [71] under default parameters. These models were then used to predict condition (HC, HIV+ w/o HL or HIV+ HL+) for each cell in the dataset with probabilities for each condition. The median predicted condition probability was calculated for each phenograph cluster. Similarly, down-sampled datasets were presented to the DDRTree and Slingshot [72, 73] algorithms for pseudotemporal ordering based on phenotypic markers (i.e., non-lineage) alone.
Results
Patient characteristics
We screened the entire SHCS cohort for cryopreserved PBMC samples of HIV-infected individuals developing NADCs and identified a group of 10 patients developing HL (HIV+ HL+) (Table 1). Even though the SHCS enrolls more than 70% of all HIV-infected individuals in Switzerland [67], the number of patients with other NADCs and sufficient sample availability was 2 to 3 and thus did not justify their inclusion in our study. In addition, we included matched HIV-negative healthy controls (HC) in this study (n = 10) (Table 1). The identification of the specimens at the various time points was only feasible thanks to the biannually biobanking of specimens from all patients in the SHCS cohort.
Dynamics of T cell populations in HIV-infected patients with and without HL
We analyzed CD4+ and CD8+ T cell counts and frequencies of TCR γδ and MAIT cells in the PB of HIV-infected individuals prior to cART, 1–2 years after the suppression of plasma viremia, 0–1 year before HL diagnosis.
The CD4+ T-cell counts were similar between HIV-infected individuals developing HL and their matched HIV-infected controls prior to cART or 1–2 years after successful cART. However, we observed a significantly lower CD4+ T cell count in HIV+ HL+ patients just prior to its diagnosis than in HIV+ w/o HL patients (Fig. 1a). The CD8+ T-cell counts were similar between the groups at all times assessed (data not shown).
Longitudinal analysis of T cell populations in the PB of HIV-infected individuals with and without HL. a CD4+ T cell count per μl in the PB of HIV-infected individuals developing HL (HIV+ HL+) and matched controls (HIV+ w/o HL). b-e Distribution of γδ T cells and MAIT cell in the PB of HIV-infected individuals developing HL (HIV+ HL+), matched controls (HIV+ w/o HL), and healthy controls. b Frequencies of MAIT cells of total lymphocytes. c Frequencies of Vδ1 cells of γδ T cells. d Frequencies of Vδ2 cells of γδ T cells. e Ratio of Vδ1 cells and Vδ2 cells. f Frequencies of VδX cells of total lymphocytes. Whiskers represent minimum and maximum. Analysis of HIV+ HL+ group versus HIV+ control group w/o HL by Wilcoxon signed-rank test, comparison of HIV-infected groups versus HC by Kruskal Wallis with Dunnett’s multiple comparison test. * without indicating line represent significance compared to healthy control. **** p ≤ 0.0001; *** p ≤ 0.001; ** p ≤ 0.01; *p ≤ 0.05. (PB) peripheral blood, (HL) Hodgkin’s lymphoma, (MAIT) Mucosal associated invariant T cells
Further, we observed a significant decrease of MAIT cells in HIV-infected patients irrespective of HL, which did not recover following cART (Fig. 1b). TCR γδ T subset analyses revealed a significant expansion of the Vδ1 cell subset in HIV-infected patients w/o HL under cART as compared to HCs (Fig. 1c). At the same time, Vδ2 cells in PB were significantly reduced irrespective of HL (Fig. 1d). This led to an inversion of the Vδ1/ Vδ2 ratio in all HIV-infected patients, which differed significantly from the ratio detected in HCs (Fig. 1e). We did not observe any differences for TCR VδX cells between HIV+ HL+, HIV+ w/o HL and HC at any time point (Fig. 1f). In conclusion, the overall frequencies of γδ T or MAIT cells were similar in HIV-infected patients irrespective of HL diagnosis whereas the CD4+ T cell counts were significantly lower in HIV+ HL+ patients just prior to HL diagnosis as compared to HIV+ w/o HL patients.
HIV infection leads to an increase in activation and exhaustion marker expression
Next, we investigated whether TCR γδ and MAIT cells differ between HIV+ HL+ patients, their HIV+ w/o HL matched controls and HCs in their activation and exhaustion status.
We observed main differences between HIV-infected patients irrespective of HL vs. HC. Namely, the frequency of Vδ1 cells expressing the activation marker CD38 increased significantly upon HIV-infection and decreased upon long-term cART (Fig. 2a). This increased frequency of CD38+ Vδ1 cells was not observed for MAIT cells (Fig. 2e). Cells expressing the activation marker CD69 showed a similar trend of higher frequencies in HIV infection but was highly variable with solely a significant increased frequency of CD69+ MAIT cells in HIV+ w/o HL patients 0–1 years prior to HL diagnosis (Fig. 2b and f).
Activation and exhaustion marker analysis on Vδ1 and MAIT cells of HIV-infected individuals with and without HL. a-d Frequency of Vδ1 cells positive for activation marker (CD38 and CD69) and exhaustion maker (PD-1 and Tim3) expression. e-h Frequency of MAIT cells positive for activation marker (CD38 and CD69) and exhaustion maker (PD-1 and Tim3) expression. Whiskers represent minimum and maximum. Analysis of HIV+ HL+ group versus HIV+ control group w/o HL by Wilcoxon signed-rank test, comparison of HIV-infected groups versus HC by Kruskal Wallis with Dunnett’s multiple comparison test. * without indicating line represent significance compared to healthy control. **** p ≤ 0.0001; *** p ≤ 0.001; ** p ≤ 0.01; *p ≤ 0.05. (PB) peripheral blood, (HL) Hodgkin’s lymphoma, (MAIT) Mucosal associated invariant T cells
The frequencies of cells expressing the exhaustion marker PD-1 was highly variable across and within the groups at all times assessed with only significant increases of Vδ1 cells in viremic HIV+ HL+ patients, and of MAIT cells in HIV+ HL+ patients just prior to HL diagnosis (Fig. 2c and g). The frequencies of Vδ1 cells expressing Tim-3 were overall significantly higher throughout HIV infection when compared to those detected in HCs (Fig. 2d). In MAIT cells, no significant differences in the frequencies of Tim-3+ cells were observed (Fig. 2h).
Overall, Vδ1 cells and MAIT cells with an activated and exhausted phenotype were more frequent upon HIV infection, which was only partially reverted upon long-term cART.
Expression of tissue homing receptors on γδ T cells and MAIT cells is altered upon HIV infection
We also determined the expression of different tissue homing receptors in our cohort, including CXCR3, CCR6, as well as CXCR4 and CCR5, with the latter two serving as viral co-receptors during entry of HIV. Notably, homing is a very critical function for immunosurveillance and its dysfunction a potential indication for insufficient control of infections or tumors.
The frequency of CCR5+ Vδ1 cells was significantly higher in HIV+ w/o HL vs. HIV+ HL+ 0–1 years prior to HL diagnosis (Fig. 3a). Instead, a slight but significant decrease in the frequency of CCR5+ MAIT cells was observed upon infection with HIV irrespective of HL (Fig. 3d).
Tissue homing receptor expression on Vδ1 and MAIT cells of HIV-infected individuals with and without HL. a-c Frequencies of Vδ1 cells expression CCR5, CXCR3, and CXCR4. d-f Frequencies of MAIT cells expression CCR5, CXCR4, and CCR6. Whiskers represent minimum and maximum. Comparison of HIV-infected groups versus HC by Kruskal Wallis with Dunnett’s multiple comparison test. * without indicating line represent significance compared to healthy control. **** p ≤ 0.0001; *** p ≤ 0.001; ** p ≤ 0.01; *p ≤ 0.05. (PB) peripheral blood, (HL) Hodgkin’s lymphoma, (MAIT) Mucosal associated invariant T cells
Overall, the frequencies of CXCR4+ Vδ1 and CXCR4+ MAIT cells were very heterogeneous in HCs and HIV-infected individuals (Fig. 3b and e). Notably, the frequencies of CXCR4+ MAIT cells tended to be higher in HIV infection with a significant increase during the viremic phase and 1–2 years after HIV suppression (Fig. 3e). Further, we found a trend towards a decrease of CXCR3+ Vδ1 and MAIT cells in HIV infection (Fig. 3c and data not shown). CCR6+ Th17-like Vδ1 cells were barely detectable in all groups (data not shown). In MAIT cells, the majority displayed a CCR6+ Th17-like phenotype, and the frequency of these cells was significantly reduced upon HIV-infection (Fig. 3f).
Characterization of natural killer cell markers expression
The phenotype of TCR γδ and MAIT cells was further assessed by investigation of different natural killer (NK) cell-associated receptors. We detected a significantly higher frequency of CD16+ Vδ1 and Vδ2 cells in the PB of HIV+ w/o HL as compared to HC and to HIV+ HL+ at various time points (Fig. 4a and Supp. 1E). MAIT cells did not express CD16 (data not shown).
Characterization of natural killer cell marker and receptor expression on Vδ1 and MAIT cells of HIV-infected individuals with and without HL. a-d Frequencies of Vδ1 cells being CD16+, CD94+, CD158b+, and ILT2+. e-h Frequencies of MAIT cells expressing CD57, KLRG1, NKG2D, and ILT2. Whiskers represent minimum and maximum. Analysis of HIV+ HL+ group versus HIV+ control group w/o HL by Wilcoxon signed-rank test, comparison of HIV-infected groups versus HC by Kruskal Wallis with Dunnett’s multiple comparison test. * without indicating line represent significance compared to healthy control. **** p ≤ 0.0001; *** p ≤ 0.001; ** p ≤ 0.01; *p ≤ 0.05. (PB) peripheral blood, (HL) Hodgkin’s lymphoma, (MAIT) Mucosal associated invariant T cells
The NK cell-associated receptors CD94 and ILT-2 were expressed by a substantial fraction of Vδ1 cells upon HIV infection (Fig. 4b and c). The percentages of CD94+ Vδ1 cells tended to remain elevated despite long-term cART (Fig. 4b). The inhibitory ILT2 receptor was expressed by the majority of TCR Vδ1 cells in HCs and the frequency of these cells tended to increase further upon HIV infection (Fig. 4c). In contrast, only a small fraction of MAIT cells were ILT-2+ (Fig. 4g).
The frequencies of Vδ1 cells expressing inhibitory killer cell immunoglobulin-like receptor (KIR) CD158b were significantly increased upon HIV infection. Frequencies of CD158b+ Vδ1 cells tended to be higher in HIV+ w/o HL individuals than in HIV+ HL+ patients (Fig. 4d). CD94 and CD158b expression was barely detectable on MAIT cells (data not shown). KLRG1 and NKG2D were expressed by the majority of MAIT cells in HC and HIV+ individuals (Fig. 4f and h), but barely detectable on Vδ1 cells.
Taken together, these findings showed a long-term impact of HIV-infection on the frequencies of TCR Vδ1 cells expressing particular NK cell markers, and their frequencies remained even under successful cART.
Analyses of Vδ2 and the VδX cells
Notably, we also extracted the data for the TCR Vδ2 and TCR VδX cells from our flow cytometric analyses (Suppl. Figures 1 and 2). The overall number of TCR Vδ2 cells were rather limited, and the expression pattern of TCR VδX did reveal only for a few significant differences, thus we only present a subset of the data. Similar to the data in TCR Vδ1 cells, we observed a higher frequency of TCR Vδ2 cells with an activated phenotype and with a decrease in the homing molecule CXCR3 in HIV infection (Suppl. Figure 1A and B). Notably, the TCR Vδ2 cells in patients w/o HL presented a higher frequency of CD16+ and KLRG1+ cells as compared to HIV+ HL+ patients. In synopsis, HIV+ w/o HL have more terminally differentiated cells (Suppl. Figure 1F and G) and cells expressing CD16 (Suppl. Figure 1E) than HIV+ HL+ patients. We also observed similarities between TCR Vδ1 and VδX cells. Namely, the higher frequency of CCR5+ cells in HIV+ w/o HL patients 1–2 years suppression and prior to diagnosis and the increased frequencies of CD158b+ cells in viremic HIV+ w/o HL patients (Suppl. Figure 2A and D). Further, HIV-infected patients irrespective of HL presented lower frequencies of CCR6+ VδX at all times assessed (Suppl. Figure 2B) and CXCR4+ VδX cells during the viremic state compared to healthy controls (Suppl. Figure 2C). Apart from those findings, the cell frequencies did not differ significantly between the three groups analyzed.
Clustering and phenotypic signature analysis of FACS panels
To identify discrete phenotypes within MAIT, TCR Vδx, Vδ1 or Vδ2 populations that distinguish or predict HL within HIV+ patients, we used PhenoGraph [74] for visualization and clustering of high-dimensional FACS data. We sought to identify clusters containing a high majority of cells from HIV+ HL+ patients, indicating a population of cells specific to HIV+ HL+ vs. HIV+ w/o HL patients or HC. In general, the clustering analysis indicated that MAIT and TCR Vδx, Vδ1 or Vδ2 populations in both HIV+ HL+ and HIV+ w/o HL patients shared phenotypes and clustering is most likely driven by differences caused by HIV infection and not HL (Suppl. Figures 3, 4, 5).
Given the complexity of the clustering and difficulty in identifying populations with phenotypic signatures unique to HIV+ HL+ patients, we trained support vector machine (SVM) classifier models to predict whether a cell comes from HC, HIV+ HL+ or HIV+ w/o HL. Ideally, the probability distributions for the SVM’s prediction should show discrete peaks of high-probability for each of the three groups (HIV+ HL+, HIV+ w/o HL and HC). Instead, we observed that in each population the probability curves for both HIV+ HL+ and HIV+ w/o HL predictions overlapped and the models yielded relatively poor predictions overall, suggesting that phenotypes in both groups were too similar to be distinguished (Suppl. Figures 6, 7, 8) and no phenotypic signatures could be attributed to HIV infection with or without HL.
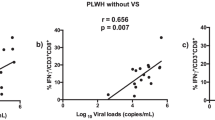
Since the data contained two time-variables (duration of infection and duration of treatment), we next attempted to establish whether there was any time-dependent effect on phenotypes. Therefore, we performed pseudotime analysis using DDRTree trained on the expression data [73, 75](Suppl. Figures 9, 10, 11). If any time-dependent effects on the phenotype were present, a gradient in infection-duration or treatment-duration in relation to the predicted trajectories would have been clearly observed. However, in agreement with the clustering and SVM classifier, cells from HIV+ HL+ and HIV+ w/o HL patients and HC were generally evenly distributed across the tree, indicating that the phenotype of these cell populations in these panels was independent of disease condition. Nevertheless, three populations in separate FACS panels appear to have pseudotemporal-dependent distributions in the DDR Trees, namely MAIT cells in the CCR panel (Fig. 5A), TCR Vδ1 cells in the exhaustion panel, and TCR Vδ2 cells in the NK panel (Fig. 5B and C). However, there was no correlation between pseudotime and duration of viral suppression or disease, indicating that phenotype and therefore, pseudotemporal ordering is driven by HIV infection and not Hodgkin’s lymphoma as indicated by the violin plots.
Pseudotemporal ordering of MAIT, Vδ1 and Vδ2 populations. Data for each population, down-sampled evenly over patients, conditions and time-points to 1e4 cells, was used to predict phenotype trajectories using DDRTree and Slingshot. Predicted trajectories, labelled within each tree, show imbalanced distributions of cells from HC, HIV and HIV HL patients in response to CCR expression in MAIT cells (A), exhaustion marker expression in Vδ1 (B) and NK marker expression in Vδ2 cells (C). Asterisks indicate significance of permutation tests (*** p < 0.001)
Discussion
In the present study, we investigated whether TCR γδ and MAIT cells differ in HIV-infected individuals developing HL from HIV-infected individuals, which otherwise are healthy. The main findings were: i) an association of a lower CD4+ T cell count and HL risk 0–1 year before HL diagnosis, and ii) prominent phenotypic changes between HIV infected patients irrespective of HL vs. HC. We observed subtle phenotypic changes in TCR Vδ1 and MAIT cells potentially going along with a greater functional impairment in HIV-infected individuals developing HL. However, clustering and SVM analyses of the data did not identify the presence/loss of unique cell populations associated with HL development. In fact the DDRtree algorithm also supported that the phenotypes observed was driven by HIV infection and not by HL.
Even though we screened the entire SHCS cohort, we only identified a limited number of HIV-infected patients developing HL. For each HIV+ HL+ patient, we had a matched control.
The CD4+ T-cell count, prior to cART, and its initial increase in response to cART were similar in both HIV-infected patient groups. In contrast, the CD4+ T cell counts 0–1 year prior to HL diagnosis were lower in patients with HL. This is in line with studies by the French Hospital Database on HIV and Collaboration of Observational HIV Epidemiological Research in Europe (COHERE), strengthening the potential of the CD4+ T cell count as a surrogate marker to identify HIV+ patients with a high risk to develop HL [17, 76,77,78]. The decline in the CD4+ T cell count might be explained by the sequestration of lymphocytes to the growing tumor, or by a lack of continuing T-cell recovery, which might result in a lack of EBV-specific CD4+ T cells, which are important for the immune surveillance of EBV-infection [79,80,81,82,83].
In addition to the CD4+ T cell count, Powls et al. identified an association between the treatment with the non-nucleoside reverse transcriptase inhibitor efavirenz and HL risk, whereas more recent investigations did not identify an association between EFV and HL risk [84,85,86]. In our study, 6 out of 10 HIV+ HL+ patients received EFV versus 3 out of 10 of HIV-infected matched controls. However, our sample size did not permit any reasonable statistical analysis.
We did not observe any difference of the overall frequency of TCR γδ T or MAIT cells between HIV-infected patients ± HL. The overall effect of HIV infection on γδ T cells in the PB is in agreement with previous studies, reporting an expansion of TCR Vδ1 cells and a decline of TCR Vδ2 cells, resulting in an inverted Vδ1/Vδ2 ratio [42, 44, 46], and lack of recovery of the altered Vδ1 and Vδ2 distribution upon cART [45]. Similarly, we found a non-reversible reduction of MAIT cells in the PB as previously reported [64].
As cell frequencies and total cell counts alone are not sufficient to determine the involvement of each T cell population in the disease progression, we performed a detailed phenotypic analysis of TCR γδ and MAIT cells in our cohort. The phenotypic analysis comprised immune activation, exhaustion, homing, NK receptor as well as inhibitory markers.
The longitudinal analysis of TCR Vδ1 cells expressing the activation marker CD38 showed an HIV-associated increase similar to what is described for its expression on TCR αβ cells, and in some studies on total TCR γδ cells or on the TCR Vγ9Vδ2 population [87,88,89,90,91,92,93]. The increase in the frequency of CD69+ MAIT cells was very subtle and in line with earlier observations [63,64,65, 94]. The frequencies of TCR Vδ1 cells expressing the inhibitory receptors PD-1 and TIM-3 and of MAIT cells expressing PD-1 were overall increased in HIV-infected individuals. Thus, we observed an activated and an exhausted phenotypic profile of these innate immune cells in HIV-infected patients. In fact, HIV-associated T cell activation persists in all kinds of investigated T cell subsets, even in successfully treated HIV-infected patients without detectable viremia, and whether it hampers T cell functions and contributes to T cell immunosenescence remains to be further investigated [95,96,97].
We also investigated the homing capacities of TCR γδ and MAIT cells in the same patient cohort by studying the expression pattern of CXCR3, CXCR4, CCR5 and CXCR6. The chemokine receptors CXCR3 and CCR5 guide T cells to sites of infection, inflammation and tumors in response to chemokines released by inflammatory tissue and tumor cells [98,99,100]. CXCR4 is important for homing to the bone marrow [101], and CCR6 is also involved in regulating mucosal immunity, as well as homing of lymphatic cells to the gut mucosal lymphoid tissue [102] and correlates with a Th17-like functional phenotype [55]. TCR γδ cells showed only minor differences between HIV+ patients and HC. Instead, MAIT cells expressing CCR5 and CCR6 showed lower frequencies in HIV infection as compared to HCs and their frequencies remained significantly lower even during cART. These results suggest that MAIT cells in HIV-infected individuals might be compromised in their ability to produce IL-17 as well as their homing capacity to specific tissues and sites of inflammation as compared to HCs [55, 103]. We noted a higher frequency of TCR Vδ1 cell and MAIT cells expressing CCR5 and CXCR4, respectively, in HIV+ patients w/o HL as compared to HIV+ HL+ patients just prior to the diagnosis of HL. These findings might point to a particular dysfunction of those cells in the latter group.
We next determined the frequency of cells expressing NK markers and co-stimulatory or inhibitory receptors. A large number of TCR Vδ1 cells expressed CD16 in HIV+ w/o HL patients and their frequency was higher in cART treated HIV+ w/o HL patients than in HIV+ HL+ patients. As CD16a is the Fcγ IIIa receptor involved in antibody dependent cytotoxicity and phagocytosis, the observed discrepancy could point to a causal role in the pathogenesis of HL.
TCR Vδ1 cells expressing the inhibitory KIR molecule CD158b also showed a higher frequency in HIV+ w/o HL patients compared to HC. Previous studies showed a potent inhibitory effect of KIR molecules on antigen stimulation of TCR γδ cells [104]. Furthermore, in HIV-infected patients an upregulation of KIR expression on CD8+ T cells was found, which inhibited their TCR-dependent stimulation [105].
When we performed clustering of high-dimensional FACS data, we found a similar distribution in HIV+ w/o HL and HIV+ HL+ individuals of all TCR γδ populations and MAIT cells. Notably, different clustering was instead observed in healthy controls, thus indicating that the observed differences are driven by differences caused by HIV infection and not HL. The analysis performed with a support vector machine classifier also showed overlapping probability curves for both HIV+ w/o HL and HIV+ HL+ patients. Clear differences were instead observed between HIV-infected and HC and only for the TCR Vδ1 population. Finally, when we analyzed a possible time-dependent effect on phenotypes, we did not see differences between the two groups of HIV+-patients, confirming the SVM analysis.
In conclusion, our study provides additional evidence for the ambiguous lower CD4+ cell counts just prior to HL as compared to their matched controls even though patients were treated successfully with cART. Our results showed subtle differences between populations of TCR γδ and MAIT cells in HIV+-patients with vs. without HL. To what extent these subtle differences contribute to the pathogenesis of HL remains unknown. Future studies need to address their potential role in the development of NADCs in HIV-infected individuals, and whether they might be exploited in novel types of cell therapy.
Availability of data and materials
The SHCS (www.shcs.ch) is a prospective cohort study with ongoing enrollment of HIV-infected adults in Switzerland since 1988 [66]. It includes 73% of all diagnosed HIV-infections in Switzerland [67]. Representation has remained stable throughout the study duration. Detailed information on demographics, mode of HIV acquisition, risk behavior, clinical events, co-infections, and treatment is collected using a standard protocol at registration and at intervals of 6 months. Plasma samples are collected every 6–12 months in all study participants.
Abbreviations
- ADCs:
-
AIDS defining cancers
- cART:
-
Combined anti-retroviral treatment
- HC:
-
Healthy controls
- HL:
-
Hodgkin’s lymphoma
- MAIT cells:
-
Mucosal-associated invariant T-cells
- NADCs:
-
Non-AIDS defining cancers
- NK cells:
-
Natural killer cells
- PB:
-
Peripheral blood
- PBMC:
-
Peripheral blood mononuclear cell
- PBS:
-
Phosphate buffered saline
- SHCS:
-
Swiss HIV Cohort Study
- SVM:
-
Support vector machine
- TCR:
-
T-cell receptor
References
Palella FJ Jr, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338(13):853–60.
Ledergerber B, Egger M, Erard V, Weber R, Hirschel B, Furrer H, et al. AIDS-related opportunistic illnesses occurring after initiation of potent antiretroviral therapy: the Swiss HIV cohort study. JAMA. 1999;282(23):2220–6. https://doi.org/10.1001/jama.282.23.2220.
Gueler A, Moser A, Calmy A, Günthard HF, Bernasconi E, Furrer H, et al. Life expectancy in HIV-positive persons in Switzerland: matched comparison with general population. AIDS. 2017;31(3):427–36. https://doi.org/10.1097/QAD.0000000000001335.
Egger M, et al. Impact of new antiretroviral combination therapies in HIV infected patients in Switzerland: prospective multicentre study. Swiss HIV Cohort Study. BMJ. 1997;315(7117):1194–9.
Ledergerber B, Telenti A, Egger M. Risk of HIV related Kaposi's sarcoma and non-Hodgkin's lymphoma with potent antiretroviral therapy: prospective cohort study. Swiss HIV Cohort Study. BMJ. 1999;319(7201):23–4.
International Collaboration on, H.I.V. and Cancer. Highly active antiretroviral therapy and incidence of cancer in human immunodeficiency virus-infected adults. J Natl Cancer Inst. 2000;92(22):1823–30.
Jacobson LP, et al. Impact of potent antiretroviral therapy on the incidence of Kaposi's sarcoma and non-Hodgkin's lymphomas among HIV-1-infected individuals. Multicenter AIDS Cohort Study. J Acquir Immune Defic Syndr. 1999;21(Suppl 1):S34–41.
Bonnet F, Lewden C, May T, Heripret L, Jougla E, Bevilacqua S, et al. Malignancy-related causes of death in human immunodeficiency virus-infected patients in the era of highly active antiretroviral therapy. Cancer. 2004;101(2):317–24. https://doi.org/10.1002/cncr.20354.
Bower M, Palmieri C, Dhillon T. AIDS-related malignancies: changing epidemiology and the impact of highly active antiretroviral therapy. Curr Opin Infect Dis. 2006;19(1):14–9. https://doi.org/10.1097/01.qco.0000200295.30285.13.
Grulich AE, van Leeuwen MT, Falster MO, Vajdic CM. Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: a meta-analysis. Lancet. 2007;370(9581):59–67. https://doi.org/10.1016/S0140-6736(07)61050-2.
Deeken JF, Tjen-A-Looi A, Rudek MA, Okuliar C, Young M, Little RF, et al. The rising challenge of non-AIDS-defining cancers in HIV-infected patients. Clin Infect Dis. 2012;55(9):1228–35. https://doi.org/10.1093/cid/cis613.
Palella FJ Jr, et al. Mortality in the highly active antiretroviral therapy era: changing causes of death and disease in the HIV outpatient study. J Acquir Immune Defic Syndr. 2006;43(1):27–34. https://doi.org/10.1097/01.qai.0000233310.90484.16.
Brugnaro P, Morelli E, Cattelan F, Petrucci A, Panese S, Eseme F, et al. Non-AIDS definings malignancies among human immunodeficiency virus-positive subjects: epidemiology and outcome after two decades of HAART era. World J Virol. 2015;4(3):209–18. https://doi.org/10.5501/wjv.v4.i3.209.
Cobucci RN, et al. Assessing the impact of HAART on the incidence of defining and non-defining AIDS cancers among patients with HIV/AIDS: a systematic review. J Infect Public Health. 2015;8(1):1–10. https://doi.org/10.1016/j.jiph.2014.08.003.
Newnham A, Harris J, Evans HS, Evans BG, Møller H. The risk of cancer in HIV-infected people in Southeast England: a cohort study. Br J Cancer. 2005;92(1):194–200. https://doi.org/10.1038/sj.bjc.6602273.
Grulich AE, Li Y, McDonald A, Correll PKL, Law MG, Kaldor JM. Rates of non-AIDS-defining cancers in people with HIV infection before and after AIDS diagnosis. AIDS. 2002;16(8):1155–61. https://doi.org/10.1097/00002030-200205240-00009.
Clifford GM, Rickenbach M, Lise M, Dal Maso L, Battegay M, Bohlius J, et al. Hodgkin lymphoma in the Swiss HIV cohort study. Blood. 2009;113(23):5737–42. https://doi.org/10.1182/blood-2009-02-204172.
Boffetta P, Hashibe M. Alcohol and cancer. Lancet Oncol. 2006;7(2):149–56. https://doi.org/10.1016/S1470-2045(06)70577-0.
Clifford GM, Polesel J, Rickenbach M, on behalf of the Swiss HIV Cohort Study, Dal Maso L, Keiser O, et al. Cancer risk in the Swiss HIV cohort study: associations with immunodeficiency, smoking, and highly active antiretroviral therapy. J Natl Cancer Inst. 2005;97(6):425–32. https://doi.org/10.1093/jnci/dji072.
Deeks SG, Phillips AN. HIV infection, antiretroviral treatment, ageing, and non-AIDS related morbidity. BMJ. 2009;338(jan26 2):a3172. https://doi.org/10.1136/bmj.a3172.
Bedimo RJ, McGinnis KA, Dunlap M, Rodriguez-Barradas MC, Justice AC. Incidence of non-AIDS-defining malignancies in HIV-infected versus noninfected patients in the HAART era: impact of immunosuppression. J Acquir Immune Defic Syndr. 2009;52(2):203–8. https://doi.org/10.1097/QAI.0b013e3181b033ab.
Franzetti M, Adorni F, Parravicini C, Vergani B, Antinori S, Milazzo L, et al. Trends and predictors of non-AIDS-defining cancers in men and women with HIV infection: a single-institution retrospective study before and after the introduction of HAART. J Acquir Immune Defic Syndr. 2013;62(4):414–20. https://doi.org/10.1097/QAI.0b013e318282a189.
Silverberg MJ, Chao C, Leyden WA, Xu L, Horberg MA, Klein D, et al. HIV infection, immunodeficiency, viral replication, and the risk of cancer. Cancer Epidemiol Biomark Prev. 2011;20(12):2551–9. https://doi.org/10.1158/1055-9965.EPI-11-0777.
Dolcetti R, Boiocchi M, Gloghini A, Carbone A. Pathogenetic and histogenetic features of HIV-associated Hodgkin's disease. Eur J Cancer. 2001;37(10):1276–87. https://doi.org/10.1016/S0959-8049(01)00105-8.
Biggar RJ, Jaffe ES, Goedert JJ, Chaturvedi A, Pfeiffer R, Engels EA, et al. Hodgkin lymphoma and immunodeficiency in persons with HIV/AIDS. Blood. 2006;108(12):3786–91. https://doi.org/10.1182/blood-2006-05-024109.
Hasenclever D, Diehl V. A prognostic score for advanced Hodgkin's disease. International prognostic factors project on advanced Hodgkin's disease. N Engl J Med. 1998;339(21):1506–14. https://doi.org/10.1056/NEJM199811193392104.
Franzetti M, Ricci E, Bonfanti P. The pattern of non-AIDS-defining cancers in the HIV population: epidemiology, risk factors and prognosis. A review. Curr HIV Res. 2019;17(1):1–12. https://doi.org/10.2174/1570162X17666190327153038.
Shiels MS, Islam JY, Rosenberg PS, Hall HI, Jacobson E, Engels EA. Projected Cancer incidence rates and burden of incident Cancer cases in HIV-infected adults in the United States through 2030. Ann Intern Med. 2018;168(12):866–73. https://doi.org/10.7326/M17-2499.
Cornejo-Juarez P, Cavildo-Jeronimo D, Volkow-Fernandez P. Non-AIDS defining cancer (NADC) among HIV-infected patients at an oncology tertiary-care center in Mexico. AIDS Res Ther. 2018;15(1):16. https://doi.org/10.1186/s12981-018-0202-2.
Prosperi MC, Cozzi-Lepri A, Castagna A, Mussini C, Murri R, Giacometti A, et al. Incidence of malignancies in HIV-infected patients and prognostic role of current CD4 cell count: evidence from a large Italian cohort study. Clin Infect Dis. 2010;50(9):1316–21. https://doi.org/10.1086/651688.
Franceschi S, et al. Kaposi sarcoma incidence in the Swiss HIV cohort study before and after highly active antiretroviral therapy. Br J Cancer. 2008;99(5):800–4. https://doi.org/10.1038/sj.bjc.6604520.
Polesel J, Clifford GM, Rickenbach M, Dal Maso L, Battegay M, Bouchardy C, et al. Non-Hodgkin lymphoma incidence in the Swiss HIV cohort study before and after highly active antiretroviral therapy. AIDS. 2008;22(2):301–6. https://doi.org/10.1097/QAD.0b013e3282f2705d.
Group, T.A.S, et al. A trial of early Antiretrovirals and isoniazid preventive therapy in Africa. N Engl J Med. 2015;373(9):808–22.
Group, I.S.S, et al. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med. 2015;373(9):795–807.
Borges AH, Neuhaus J, Babiker AG, Henry K, Jain MK, Palfreeman A, et al. Immediate antiretroviral therapy reduces risk of infection-related Cancer during early HIV infection. Clin Infect Dis. 2016;63(12):1668–76. https://doi.org/10.1093/cid/ciw621.
Bonneville M, O'Brien RL, Born WK. Gammadelta T cell effector functions: a blend of innate programming and acquired plasticity. Nat Rev Immunol. 2010;10(7):467–78. https://doi.org/10.1038/nri2781.
Napier RJ, et al. The role of mucosal associated invariant T cells in antimicrobial immunity. Front Immunol. 2015;6:344.
Zheng J, Liu Y, Lau YL, Tu W. Gammadelta-T cells: an unpolished sword in human anti-infection immunity. Cell Mol Immunol. 2013;10(1):50–7. https://doi.org/10.1038/cmi.2012.43.
Mori L, Lepore M, De Libero G. The immunology of CD1- and MR1-restricted T cells. Annu Rev Immunol. 2016;34(1):479–510. https://doi.org/10.1146/annurev-immunol-032414-112008.
Balbi B, Valle MT, Oddera S, Giunti O, Manca F, Rossi GA, et al. T-lymphocytes with gamma delta+ V delta 2+ antigen receptors are present in increased proportions in a fraction of patients with tuberculosis or with sarcoidosis. Am Rev Respir Dis. 1993;148(6 Pt 1):1685–90. https://doi.org/10.1164/ajrccm/148.6_Pt_1.1685.
Chien YH, Meyer C, Bonneville M. gammadelta T cells: first line of defense and beyond. Annu Rev Immunol. 2014;32(1):121–55. https://doi.org/10.1146/annurev-immunol-032713-120216.
De Maria A, et al. Selective increase of a subset of T cell receptor gamma delta T lymphocytes in the peripheral blood of patients with human immunodeficiency virus type 1 infection. J Infect Dis. 1992;165(5):917–9. https://doi.org/10.1093/infdis/165.5.917.
Kalyan S, Kabelitz D. Defining the nature of human gammadelta T cells: a biographical sketch of the highly empathetic. Cell Mol Immunol. 2013;10(1):21–9. https://doi.org/10.1038/cmi.2012.44.
Autran B, Triebel F, Katlama C, Rozenbaum W, Hercend T, Debre P. T cell receptor gamma/delta+ lymphocyte subsets during HIV infection. Clin Exp Immunol. 1989;75(2):206–10.
Poles MA, Barsoum S, Yu W, Yu J, Sun P, Daly J, et al. Human immunodeficiency virus type 1 induces persistent changes in mucosal and blood gammadelta T cells despite suppressive therapy. J Virol. 2003;77(19):10456–67. https://doi.org/10.1128/JVI.77.19.10456-10467.2003.
De Paoli P, et al. A subset of gamma delta lymphocytes is increased during HIV-1 infection. Clin Exp Immunol. 1991;83(2):187–91. https://doi.org/10.1111/j.1365-2249.1991.tb05612.x.
Hermier F, Comby E, Delaunay A, Petitjean J, Favennec L, Bazin C, et al. Decreased blood TcR gamma delta+ lymphocytes in AIDS and p24-antigenemic HIV-1-infected patients. Clin Immunol Immunopathol. 1993;69(2):248–50. https://doi.org/10.1006/clin.1993.1176.
Vantourout P, Hayday A. Six-of-the-best: unique contributions of gammadelta T cells to immunology. Nat Rev Immunol. 2013;13(2):88–100. https://doi.org/10.1038/nri3384.
Morita CT, Verma S, Aparicio P, Martinez-A. C, Spits H, Brenner MB. Functionally distinct subsets of human gamma/delta T cells. Eur J Immunol. 1991;21(12):2999–3007. https://doi.org/10.1002/eji.1830211215.
Fenoglio D, Poggi A, Catellani S, Battaglia F, Ferrera A, Setti M, et al. Vdelta1 T lymphocytes producing IFN-gamma and IL-17 are expanded in HIV-1-infected patients and respond to Candida albicans. Blood. 2009;113(26):6611–8. https://doi.org/10.1182/blood-2009-01-198028.
Wallace M, et al. Gamma delta T lymphocyte responses to HIV. Clin Exp Immunol. 1996;103(2):177–84. https://doi.org/10.1046/j.1365-2249.1996.d01-625.x.
Silva-Santos B, Serre K, Norell H. gammadelta T cells in cancer. Nat Rev Immunol. 2015;15(11):683–91. https://doi.org/10.1038/nri3904.
Zhao Y, Niu C, Cui J. Gamma-delta (gammadelta) T cells: friend or foe in cancer development? J Transl Med. 2018;16(1):3. https://doi.org/10.1186/s12967-017-1378-2.
Wu D, Wu P, Qiu F, Wei Q, Huang J. Human gammadeltaT-cell subsets and their involvement in tumor immunity. Cell Mol Immunol. 2017;14(3):245–53. https://doi.org/10.1038/cmi.2016.55.
Dusseaux M, Martin E, Serriari N, Péguillet I, Premel V, Louis D, et al. Human MAIT cells are xenobiotic-resistant, tissue-targeted, CD161hi IL-17-secreting T cells. Blood. 2011;117(4):1250–9. https://doi.org/10.1182/blood-2010-08-303339.
Martin E, Treiner E, Duban L, Guerri L, Laude H, Toly C, et al. Stepwise development of MAIT cells in mouse and human. PLoS Biol. 2009;7(3):e54. https://doi.org/10.1371/journal.pbio.1000054.
Treiner E, Duban L, Bahram S, Radosavljevic M, Wanner V, Tilloy F, et al. Selection of evolutionarily conserved mucosal-associated invariant T cells by MR1. Nature. 2003;422(6928):164–9. https://doi.org/10.1038/nature01433.
Vacchini A, Chancellor A, Spagnuolo J, Mori L, de Libero G. MR1-restricted T cells are unprecedented Cancer fighters. Front Immunol. 2020;11:751. https://doi.org/10.3389/fimmu.2020.00751.
Lepore M, Kalinichenko A, Colone A, Paleja B, Singhal A, Tschumi A, et al. Parallel T-cell cloning and deep sequencing of human MAIT cells reveal stable oligoclonal TCRbeta repertoire. Nat Commun. 2014;5(1):3866. https://doi.org/10.1038/ncomms4866.
Reantragoon R, Kjer-Nielsen L, Patel O, Chen Z, Illing PT, Bhati M, et al. Structural insight into MR1-mediated recognition of the mucosal associated invariant T cell receptor. J Exp Med. 2012;209(4):761–74. https://doi.org/10.1084/jem.20112095.
Kurioka A, Ussher JE, Cosgrove C, Clough C, Fergusson JR, Smith K, et al. MAIT cells are licensed through granzyme exchange to kill bacterially sensitized targets. Mucosal Immunol. 2015;8(2):429–40. https://doi.org/10.1038/mi.2014.81.
Sundstrom P, et al. Tumor-infiltrating mucosal-associated invariant T (MAIT) cells retain expression of cytotoxic effector molecules. Oncotarget. 2019;10(29):2810–23. https://doi.org/10.18632/oncotarget.26866.
Cosgrove C, Ussher JE, Rauch A, Gärtner K, Kurioka A, Hühn MH, et al. Early and nonreversible decrease of CD161++ /MAIT cells in HIV infection. Blood. 2013;121(6):951–61. https://doi.org/10.1182/blood-2012-06-436436.
Eberhard JM, Hartjen P, Kummer S, Schmidt RE, Bockhorn M, Lehmann C, et al. CD161+ MAIT cells are severely reduced in peripheral blood and lymph nodes of HIV-infected individuals independently of disease progression. PLoS One. 2014;9(11):e111323. https://doi.org/10.1371/journal.pone.0111323.
Leeansyah E, Ganesh A, Quigley MF, Sönnerborg A, Andersson J, Hunt PW, et al. Activation, exhaustion, and persistent decline of the antimicrobial MR1-restricted MAIT-cell population in chronic HIV-1 infection. Blood. 2013;121(7):1124–35. https://doi.org/10.1182/blood-2012-07-445429.
Swiss HIVCS, et al. Cohort profile: the Swiss HIV cohort study. Int J Epidemiol. 2010;39(5):1179–89.
Kohler P, Schmidt AJ, Cavassini M, Furrer H, Calmy A, Battegay M, et al. The HIV care cascade in Switzerland: reaching the UNAIDS/WHO targets for patients diagnosed with HIV. AIDS. 2015;29(18):2509–15. https://doi.org/10.1097/QAD.0000000000000878.
R Development Core Team. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2010.
Chen H. Rphenograph: R implementation of the phenograph algorithm; 2015.
Kuhn M. caret: Classification and Regression Training; 2020.
Meyer DD, Evgenia, Hornik K, Weingessel A, Leisch F. e1071: Misc Functions of the Department of Statistics, Probability Theory Group (Formerly: E1071): TU Wien; 2019. https://www.scienceopen.com/document?vid=fc1a25fa-4c7b-4b91-a707-1ce7ce33659e.
Qiu XT, Cole, Mao Q, Wang L. DDRTree: Learning Principal Graphs with DDRTree; 2017.
Street K, Risso D, Fletcher RB, Das D, Ngai J, Yosef N, et al. Slingshot: cell lineage and pseudotime inference for single-cell transcriptomics. BMC Genomics. 2018;19(1):477. https://doi.org/10.1186/s12864-018-4772-0.
Levine JH, Simonds EF, Bendall SC, Davis KL, Amir EAD, Tadmor MD, et al. Data-driven phenotypic dissection of AML reveals progenitor-like cells that correlate with prognosis. Cell. 2015;162(1):184–97. https://doi.org/10.1016/j.cell.2015.05.047.
Mao Q, et al. Dimensionality Reduction Via Graph Structure Learning. In: Proceedings of the 21th ACM SIGKDD International Conference on Knowledge Discovery and Data Mining; 2015. p. 765–74.
Bohlius J, Schmidlin K, Boué F, Fätkenheuer G, May M, Caro-Murillo AM, et al. HIV-1-related Hodgkin lymphoma in the era of combination antiretroviral therapy: incidence and evolution of CD4(+) T-cell lymphocytes. Blood. 2011;117(23):6100–8. https://doi.org/10.1182/blood-2010-08-301531.
Guiguet M, Boué F, Cadranel J, Lang JM, Rosenthal E, Costagliola D, et al. Effect of immunodeficiency, HIV viral load, and antiretroviral therapy on the risk of individual malignancies (FHDH-ANRS CO4): a prospective cohort study. Lancet Oncol. 2009;10(12):1152–9. https://doi.org/10.1016/S1470-2045(09)70282-7.
Shepherd L, Ryom L, Law M, Hatleberg CI, de Wit S, Monforte A'A, et al. Differences in Virological and immunological risk factors for non-Hodgkin and Hodgkin lymphoma. J Natl Cancer Inst. 2018;110(6):598–607. https://doi.org/10.1093/jnci/djx249.
Bickham K, Münz C, Tsang ML, Larsson M, Fonteneau JF, Bhardwaj N, et al. EBNA1-specific CD4+ T cells in healthy carriers of Epstein-Barr virus are primarily Th1 in function. J Clin Invest. 2001;107(1):121–30. https://doi.org/10.1172/JCI10209.
Murray RJ, Kurilla MG, Brooks JM, Thomas WA, Rowe M, Kieff E, et al. Identification of target antigens for the human cytotoxic T cell response to Epstein-Barr virus (EBV): implications for the immune control of EBV-positive malignancies. J Exp Med. 1992;176(1):157–68. https://doi.org/10.1084/jem.176.1.157.
Rickinson AB, Moss DJ. Human cytotoxic T lymphocyte responses to Epstein-Barr virus infection. Annu Rev Immunol. 1997;15(1):405–31. https://doi.org/10.1146/annurev.immunol.15.1.405.
Romagnani S, del Prete G, Maggi E, Bosi A, Bernardi F, Ponticelli P, et al. Displacement of T lymphocytes with the 'Helper/Inducer' phenotype from peripheral blood to lymphoid organs in untreated patients with Hodgkin's disease. Scand J Haematol. 1983;31(4):305–14. https://doi.org/10.1111/j.1600-0609.1983.tb00658.x.
van den Berg A, Visser L, Poppema S. High expression of the CC chemokine TARC in reed-Sternberg cells. A possible explanation for the characteristic T-cell infiltratein Hodgkin's lymphoma. Am J Pathol. 1999;154(6):1685–91. https://doi.org/10.1016/S0002-9440(10)65424-7.
Powles T, Robinson D, Stebbing J, Shamash J, Nelson M, Gazzard B, et al. Highly active antiretroviral therapy and the incidence of non-AIDS-defining cancers in people with HIV infection. J Clin Oncol. 2009;27(6):884–90. https://doi.org/10.1200/JCO.2008.19.6626.
Chao C, Leyden WA, Xu L, Horberg MA, Klein D, Towner WJ, et al. Exposure to antiretroviral therapy and risk of cancer in HIV-infected persons. AIDS. 2012;26(17):2223–31. https://doi.org/10.1097/QAD.0b013e32835935b3.
Krishnan S, Schouten JT, Jacobson DL, Benson CA, Collier AC, Koletar SL, et al. Incidence of non-AIDS-defining cancer in antiretroviral treatment-naive subjects after antiretroviral treatment initiation: an ACTG longitudinal linked randomized trials analysis. Oncology. 2011;80(1–2):42–9. https://doi.org/10.1159/000328032.
Day CL, Kaufmann DE, Kiepiela P, Brown JA, Moodley ES, Reddy S, et al. PD-1 expression on HIV-specific T cells is associated with T-cell exhaustion and disease progression. Nature. 2006;443(7109):350–4. https://doi.org/10.1038/nature05115.
Paiardini M, Muller-Trutwin M. HIV-associated chronic immune activation. Immunol Rev. 2013;254(1):78–101. https://doi.org/10.1111/imr.12079.
Jones RB, Ndhlovu LC, Barbour JD, Sheth PM, Jha AR, Long BR, et al. Tim-3 expression defines a novel population of dysfunctional T cells with highly elevated frequencies in progressive HIV-1 infection. J Exp Med. 2008;205(12):2763–79. https://doi.org/10.1084/jem.20081398.
Belkina AC, Starchenko A, Drake KA, Proctor EA, Pihl RMF, Olson A, et al. Multivariate computational analysis of Gamma Delta T cell inhibitory receptor signatures reveals the divergence of healthy and ART-suppressed HIV+ aging. Front Immunol. 2018;9:2783. https://doi.org/10.3389/fimmu.2018.02783.
Iwasaki M, Tanaka Y, Kobayashi H, Murata-Hirai K, Miyabe H, Sugie T, et al. Expression and function of PD-1 in human gammadelta T cells that recognize phosphoantigens. Eur J Immunol. 2011;41(2):345–55. https://doi.org/10.1002/eji.201040959.
Jouen-Beades F, Gilbert D, Ramzaoui S, Borsa-Lebas F, Humbert G, Tron F. Similarity of expression of activation markers and CD28 on gamma delta and alpha beta-receptor T cells in HIV infection. Clin Immunol Immunopathol. 1996;79(2):189–93. https://doi.org/10.1006/clin.1996.0066.
Bhatnagar N, Girard PM, Lopez-Gonzalez M, Didier C, Collias L, Jung C, et al. Potential role of Vdelta2(+) gammadelta T cells in regulation of immune activation in primary HIV infection. Front Immunol. 2017;8:1189. https://doi.org/10.3389/fimmu.2017.01189.
Saeidi A, et al. Attrition of TCR Valpha7.2+ CD161++ MAIT cells in HIV-tuberculosis co-infection is associated with elevated levels of PD-1 expression. PLoS One. 2015;10(4):e0124659.
Jain V, Hartogensis W, Bacchetti P, Hunt PW, Hatano H, Sinclair E, et al. Antiretroviral therapy initiated within 6 months of HIV infection is associated with lower T-cell activation and smaller HIV reservoir size. J Infect Dis. 2013;208(8):1202–11. https://doi.org/10.1093/infdis/jit311.
Vinikoor MJ, Cope A, Gay CL, Ferrari G, McGee KS, Kuruc JD, et al. Antiretroviral therapy initiated during acute HIV infection fails to prevent persistent T-cell activation. J Acquir Immune Defic Syndr. 2013;62(5):505–8. https://doi.org/10.1097/QAI.0b013e318285cd33.
Sokoya T, et al. HIV as a cause of immune activation and Immunosenescence. Mediat Inflamm. 2017;2017:6825493.
Moser B, Loetscher P. Lymphocyte traffic control by chemokines. Nat Immunol. 2001;2(2):123–8. https://doi.org/10.1038/84219.
Proost P, Wuyts A, van Damme J. The role of chemokines in inflammation. Int J Clin Lab Res. 1996;26(4):211–23. https://doi.org/10.1007/BF02602952.
Spagnolo P, Renzoni EA, Wells AU, Copley SJ, Desai SR, Sato H, et al. C-C chemokine receptor 5 gene variants in relation to lung disease in sarcoidosis. Am J Respir Crit Care Med. 2005;172(6):721–8. https://doi.org/10.1164/rccm.200412-1707OC.
Burger JA, Burkle A. The CXCR4 chemokine receptor in acute and chronic leukaemia: a marrow homing receptor and potential therapeutic target. Br J Haematol. 2007;137(4):288–96. https://doi.org/10.1111/j.1365-2141.2007.06590.x.
Ito T, Carson WF IV, Cavassani KA, Connett JM, Kunkel SL. CCR6 as a mediator of immunity in the lung and gut. Exp Cell Res. 2011;317(5):613–9. https://doi.org/10.1016/j.yexcr.2010.12.018.
Billerbeck E, Kang YH, Walker L, Lockstone H, Grafmueller S, Fleming V, et al. Analysis of CD161 expression on human CD8+ T cells defines a distinct functional subset with tissue-homing properties. Proc Natl Acad Sci U S A. 2010;107(7):3006–11. https://doi.org/10.1073/pnas.0914839107.
Carena I, Shamshiev A, Donda A, Colonna M, Libero GD. Major histocompatibility complex class I molecules modulate activation threshold and early signaling of T cell antigen receptor-gamma/delta stimulated by nonpeptidic ligands. J Exp Med. 1997;186(10):1769–74. https://doi.org/10.1084/jem.186.10.1769.
Alter G, Rihn S, Streeck H, Teigen N, Piechocka-Trocha A, Moss K, et al. Ligand-independent exhaustion of killer immunoglobulin-like receptor-positive CD8+ T cells in human immunodeficiency virus type 1 infection. J Virol. 2008;82(19):9668–77. https://doi.org/10.1128/JVI.00341-08.
Acknowledgments
We thank Sandra Chaudron for extracting and providing patient data from the SHCS databank. We thank Stephan Benke for support in panel design and data analysis and Stefan Kuster for support in statistical analysis.
Members of the Swiss HIV Cohort Study:
Aebi-Popp K, Anagnostopoulos A, Battegay M, Bernasconi E, Böni J, Braun DL, Bucher HC, Calmy A, Cavassini M, Ciuffi A, Dollenmaier G, Egger M, Elzi L, Fehr J, Fellay J, Furrer H, Fux CA, Günthard HF (President of the SHCS), Haerry D (deputy of “Positive Council”), Hasse B, Hirsch HH, Hoffmann M, Hösli I, Huber M, Kahlert CR (Chairman of the Mother & Child Substudy), Kaiser L, Keiser O, Klimkait T, Kouyos RD, Kovari H, Ledergerber B, Martinetti G, Martinez de Tejada B, Marzolini C, Metzner KJ, Müller N, Nicca D, Paioni P, Pantaleo G, Perreau M, Rauch A (Chairman of the Scientific Board), Rudin C, Scherrer AU (Head of Data Centre), Schmid P, Speck R, Stöckle M (Chairman of the Clinical and Laboratory Committee), Tarr P, Trkola A, Vernazza P, Wandeler G, Weber R, Yerly S.
Disclaimer
The founders had no role in the study design, data collection, analysis and interpretation of the data, writing of the manuscript and the decision to submit for publication.
Funding
This study has been financed within the framework of the Swiss HIV Cohort Study, supported by the Swiss National Science Foundation (grant #177499), by SHCS project #804 and by the SHCS research foundation. The data are gathered by the Five Swiss University Hospitals, two Cantonal Hospitals, 15 affiliated hospitals and 36 private physicians (listed in Http://www.shcs.ch/180-health-care-providers). We thank the healthy volunteers for donating blood.
Author information
Authors and Affiliations
Consortia
Contributions
The study was conceptualized, designed by R.F.S. A.A, GL and MB. R.F.S. supervised the study. A.A. and C.K.S.M. designed polychromatic panels. A.A., A.U.S., and C.K.S.M., identified patient samples within the SHCS database. Data acquisition was done by D.R. and C.K.S.M. MH and RK provided critical input into the overall concept. Data analysis and first draft of manuscript by C.K.S.M., J.S., RK, and A.C. G.L. and R.F.S. reviewed manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Local ethical committees of all participating study sites approved the study, i.e., the ethical committee of both Basel, Berne (21/88), Geneva (01–142), Canton de Vaud (131/01), Ticino (CE 813); St. Gallen (EKSG 12/003) and Zurich (KEK-ZH-NR: EK-793) (http://www.shcs.ch/206-ethic-committee-approval-and-informed-consent) and written consent was obtained from all participants.
Consent for publication
All authors consented for the publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Muller, C.K.S., Spagnuolo, J., Audigé, A. et al. Immunophenotypic characterization of TCR γδ T cells and MAIT cells in HIV-infected individuals developing Hodgkin’s lymphoma. Infect Agents Cancer 16, 24 (2021). https://doi.org/10.1186/s13027-021-00365-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13027-021-00365-4