Abstract
Background
Plasma biomarkers reflecting the pathology of frontotemporal dementia would add significant value to clinical practice, to the design and implementation of treatment trials as well as our understanding of disease mechanisms. The aim of this study was to explore the levels of multiple plasma proteins in individuals from families with genetic frontotemporal dementia.
Methods
Blood samples from 693 participants in the GENetic Frontotemporal Dementia Initiative study were analysed using a multiplexed antibody array targeting 158 proteins.
Results
We found 13 elevated proteins in symptomatic mutation carriers, when comparing plasma levels from people diagnosed with genetic FTD to healthy non-mutation controls and 10 proteins that were elevated compared to presymptomatic mutation carriers.
Conclusion
We identified plasma proteins with altered levels in symptomatic mutation carriers compared to non-carrier controls as well as to presymptomatic mutation carriers. Further investigations are needed to elucidate their potential as fluid biomarkers of the disease process.
Similar content being viewed by others
Background
Frontotemporal dementia (FTD) is a group of neurodegenerative diseases where the most common phenotypes are behavioural variant FTD (bvFTD) and primary progressive aphasias (PPA). There is a great heterogeneity in FTD, both in terms of clinical symptoms, underlying genetic causes, and neuropathological findings. Over the past years, effort has been put into explaining the diversity by searching for fluid biomarkers that reflect different aspects of FTD [1]. Most efforts have focused on finding biomarkers in cerebrospinal fluid (CSF) and a few promising candidates have been found, such as neurofilament light chain (NEFL) and neuronal pentraxin 2 (NPTX2) [2, 3]. However, the use of CSF biomarkers is limited by the invasive nature of the sampling procedure and restricted availability. Therefore, a reliable blood-based biomarker would be extremely valuable. A well-known blood-based biomarker in genetic FTD is progranulin (GRN), which is reduced in individuals with loss-of-function mutations in the gene with the same name [4]. While serum or plasma GRN levels can be used to confirm mutations in GRN, they do not correlate with clinically important metrics such as age at onset [4]. Previous studies have also identified glial fibrillary acidic protein (GFAP), tau and NEFL as possible plasma-based biomarkers, where GFAP is elevated in symptomatic GRN mutation carriers, tau is elevated in sporadic FTD and in symptomatic MAPT mutation carriers, and NEFL is elevated in both genetic and sporadic FTD [5,6,7]. However, none of the proteins are specific for FTD since increased levels have been observed in other neurological diseases [8, 9]. A large screen of plasma proteins in FTD and Alzheimer disease (AD) found a panel of 12 proteins that discriminated between the two diseases. However, these proteins were associated with AD pathology and no differences were found between FTD cases and controls [10]. Further studies are therefore needed to find biomarkers that are FTD specific.
Here, we present an exploratory plasma profiling study of 158 proteins in 693 participants in the well-described genetic FTD cohort. To our knowledge, a plasma proteomic analysis of this magnitude has not been done in genetic FTD before. We aimed to investigate differences in plasma protein levels between both symptomatic and presymptomatic mutation carriers compared to non-carrier family members who serve as controls. Our findings indicate alterations in plasma protein levels between symptomatic mutation carriers and non-carrier controls, as well as gene specific differences in GRN mutation carriers.
Materials and methods
Cohort
All clinical data and samples included in the study were collected within the Genetic frontotemporal dementia initiative (GENFI) between 2012 and 2019 [11]. Variables included were age at sampling, sex, mutation group (symptomatic mutation carriers, SMC; presymptomatic mutation carriers, PMC; or non-carrier controls, NC), genetic group (chromosome 9 open reading frame 72, C9orf72; progranulin, GRN; or microtubule associated protein tau, MAPT), clinical phenotype, and age at onset. In total, baseline plasma samples from 701 participants were collected including 141 SMC (63 C9orf72, 50 GRN, and 28 MAPT), 283 PMC (97 C9orf72, 135 GRN and 51 MAPT) and 277 NC. Carriers of FTD-causing variants in other genes were not included. Clinically, the SMC most frequently presented with bvFTD (n = 102), followed by PPA (n = 25), FTD with concomitant amyotrophic lateral sclerosis (ALS) (n = 5) and other FTD-related phenotypes (n = 5).
Sample collection according to GENFI protocol
Blood samples (n = 701) were collected at 20 different sites in Europe and Canada in ethylenediaminetetraacetic acid (EDTA) tubes. Samples were centrifuged at 2200 × g for 5 min at 22 °C and the supernatant plasma was transferred to 0.5 ml polypropylene cryotubes and stored at -80 °C until analysis.
Suspension bead array assay
The plasma samples were diluted and labelled with a tenfold molar excess of biotin (NHS-PEG4-biotin. 21329, Thermo Scientific), heat treated, and subsequently mixed with an antibody suspension bead array as described in detail previously [12, 13]. A streptavidin conjugated fluorophore (Streptavidin R-Phycoerythrin Conjugate, Invitrogen) enabled the detection of the proteins, and the readout was performed on a Flexmap 3D instrument (Luminex corporation). Binding events were displayed as signal intensity. Published as well as internal unpublished work were used to guide the selection of target proteins (n = 163) which was based on previously identified promising targets, proteins involved in suggested pathological processes of neurodegeneration and proteins with enriched expression in brain compared to other tissue [14,15,16,17]. The majority of the antibodies (n = 156) were selected from the Human Protein Atlas project (www.proteinatlas.org) and the remaining seven were obtained from other providers (M067-3 from MBL International; MA1-70053, PA5-34943, 34–1000 from Invitrogen Antibodies; MAB2037-SP, AF2420, AF3154 from R&D Systems). The mean coefficient of variance per 384-well plate (n = 3) was less than 10%, and 97% of the antibodies had an individual coefficient of variance below 20%. The inter-assay correlations were high (rho > 0.8 for 154 antibodies). After quality control analysis, five antibodies were excluded due to high correlation to a negative control (rho > 0.6) resulting in 158 protein targets for further analysis (Supplementary Table 1).
Statistical analysis
Data pre-processing
All data pre-processing, analysis and illustrations were performed in R Studio version 2022.2.3.492 using R version 4.2.1 [18]. The data was normalised in two steps to diminish the effects of time delay during readout and potential differences between plates [19]. Prior to statistical analysis, the data was log2- and z-transformed via mean centring and unit variance scaling. Outlier samples with a median protein level three standard deviations higher or lower than the median for the whole cohort were excluded from the analysis (n = 8 samples removed). A residual adjustment approach was used to deal with the potential confounding effect of healthy ageing on protein levels [20]. The effect of healthy ageing on protein levels was estimated in the NC via linear mixed effect models using protein levels as the response variable, age as a fixed effect and collection site as a random intercept (lmer, lme4, [21]). For each subject in the overall cohort (including each of the NC, PMC, and SMC groups), the adjusted protein levels were then obtained through the following:
where Proteinadj. is the age adjusted protein level, Protein is the original protein level, β is the age-associated beta coefficient, Age is the subject’s age and \(\overline{Age}\) is the mean age in the entire cohort.
Demographic statistics
The participants’ ages followed a normal distribution, evaluated by visual assessment of normal probability plot and histogram. Differences in age between SMC, PMC and NC were assessed by one-way ANOVA and Tukey’s HSD post hoc test. Pearson’s Chi-squared test was used to investigate differences in sex between SMC, PMC and NC. P-values below 0.05 were considered significant.
Protein profile analysis
Differences in protein levels between SMC and NC were examined via binomial generalised linear mixed effects models using clinical status (i.e. SMC or NC) as the response variable, protein levels and sex as fixed effects with a random intercept based on collection site (glmer, lme4, [21]). One model per protein was built. The same method was used to assess differences in protein levels between SMC and presymptomatic mutation carriers (PMC), PMC versus NC, as well as to analyse gene specific differences e.g., SMC carrying a GRN mutation (SMC-GRN) vs NC. Log2 fold changes were calculated by subtracting the median log2 transformed protein levels in NC or PMC from the median log2 transformed protein levels in SMC. In contrast, the effects of age and sex on the protein levels in mutation carriers as well as in non-carriers were estimated via generalised linear mixed-effects models using protein levels as the response; age and sex as fixed effects with a random intercept based on collection site (lmer, lme4, [21]). P-values were calculated using the Satterthwaite’s degrees of freedom method (lmerTest, [22]). Multiple testing corrections were made via the Benjamini–Hochberg method for controlling false-discovery rates and an adjusted p-value of 0.05 was considered significant. Only adjusted p-values are reported unless clearly stated otherwise. Protein – protein correlations were calculated using Spearman's rank correlation coefficient. Protein clusters are based on hierarchical clustering using Ward’s clustering criterion.
Results
Cohort
In total, plasma results from 693 participants were included in the statistical analysis, and demographic data of the cohort is presented in Table 1. The age was not significantly different between NC and PMC (p-value = 0.06), but SMC were older than both NC and PMC (p-value = 7.13 × 10–41). There were more females in NC (55%) and PMC (62%) compared to SMC (42%) (NC vs SMC: p-value = 1.3 × 10–2; PMC vs SMC: p-value = 1.1 × 10–4).
Altered plasma protein levels in symptomatic mutation carriers
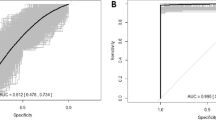
When comparing plasma protein levels in SMC to NC, we found that 13 proteins were elevated in SMC (Fig. 1A, Table 2 and Supplementary Fig. 1). In the comparison between SMC versus PMC, we found that 10 proteins were elevated in SMC (Fig. 1B, Table 2). There were six overlapping proteins i.e., six proteins had elevated levels in SMC both in the comparison to NC as well as in the comparison to the protein levels in PMC. An overview of how these proteins correlate with each other can be found in Fig. 2. When stratifying by genetic group, rabphilin 3a (RPH3A) was increased in SMC-GRN compared to NC (p-value = 1.3 × 10–3, odds ratio = 1.915) whereas progranulin, as expected, was decreased (p-value = 9.3 × 10–6, odds ratio = 0.152). No proteins had significantly different levels in the comparison between SMC-C9 and NC nor in the comparison between SMC-MAPT and NC (data not shown).
Volcano plots of plasma protein levels showing -log10 (p-values) of the log2(fold change) for comparisons between different groups. Plasma protein level differences between A) all SMC and NC, B) all SMC and all PMC. Each protein is represented by a gray dot and are coloured red if the protein levels are increased in the SMC compared to the comparison group (NC, or PMC). Dotted horizontal line = adjusted p-value 0.05, dotted vertical line = log2 fold change 0
Plots of protein – protein correlations. Protein order is based on hierarchical clustering. Correlation plot of the 17 proteins with elevated levels in symptomatic mutation carriers (SMC) compared to non-carriers (NC) or presymptomatic mutation carriers (PMC). The colour scale indicates Spearman's rank correlation coefficient from dark blue (-1) to bright red (1)
Next, we investigated the correlation between age and protein levels of the altered proteins in mutation carriers. Among the 17 unique proteins with elevated levels in SMC (SMC vs NC or SMC vs PMC), 13 had a significant correlation with age (Table 3).
When analysing sex differences for the 17 proteins elevated in SMC, two proteins were found to be increased in men compared to women in the mutation carriers: apolipoprotein E (APOE, p-value = 1.73 × 10–2, β = 0.267) and apolipoprotein C1 (APOC1, p-value = 1.73 × 10–2, β = 0.235). No sex differences were found among the NC for either protein (p-value = 1.49 × 10–1 and p-value = 7.4 × 10–1, respectively).
Finally, we explored if any of the 158 proteins included in this study were found at different levels in SMC with bvFTD compared to SMC with PPA but found no significant differences (data not shown).
Plasma protein levels in the presymptomatic stage
We also investigated the possibility to detect differences in protein levels already at the presymptomatic stage of FTD by first comparing PMC to NC and then stratifying by gene. The only difference found in these comparisons was decreased levels of GRN in PMC-GRN compared to NC (p-value = 4.44 × 10–3). However, the proteins neurofilament medium chain (NEFM), neuronal pentraxin 2 (NPTX2) and chitinase 3 like 1 (CHI3L1) showed trends of being elevated in PMC-GRN compared to NC (unadjusted p-value = 3.1 × 10–3, unadjusted p-value = 4.8 × 10–3 and unadjusted p-value = 4.6 × 10–3, respectively), though these differences were not significant after adjustment for multiple testing. None of the three proteins showed any correlation with age when analysed in PMC-GRN alone or in PMC-GRN together with SMC-GRN (Supplementary Table 2). NPTX2 was, however, elevated in SMC compared to NC and CHI3L1 was just above the significance threshold in the same comparison (p-value = 5.1 × 10–2). Neither were significant in the comparison between SMC and PMC (both p-values > 0.3).
Discussion
We performed extensive protein profiling of plasma from a genetic FTD cohort, collected within the GENFI study. We found 13 significantly increased plasma proteins in patients with genetic FTD compared to non-carrier controls and 10 proteins that were significantly increased compared to presymptomatic mutation carriers. Six of these proteins were significantly different in both comparisons, indicating that they likely are associated with symptom onset rather than the presence of one of the pathogenic mutations. These six proteins were also significantly correlated with increased age in mutation carriers, after correcting for healthy ageing, which further strengthens their association with symptom onset.
In contrast, four proteins, increased in SMC vs NC, were not correlated with age, nor elevated in the SMC vs PMC comparison, suggesting that they may be elevated already before symptom onset. One of these proteins NPTX2, is of particular interest. NPTX2, a synaptic protein, which has previously been shown to be reduced in CSF from patients with FTD and is potentially one of the first protein biomarkers to become abnormal in genetic FTD [3, 23, 24]. We have, as of yet, no explanation to why NPTX2 is reduced in CSF and elevated in plasma, or if the NPTX2 detected in plasma is brain derived. However, finding elevated levels of NPTX2 in plasma from SMC suggests that NPTX2 could work as a plasma-based biomarker.
We found two proteins, GRN and RPH3A, that differed in SMC-GRN compared to NC, while no proteins were observed at different levels in neither SMC-MAPT nor SMC-C9, compared to NC. A reduction of GRN in progranulin mutation carriers is of course expected since all known pathogenic FTD-related GRN mutations lead to haploinsufficiency. On the other hand, RPH3A was elevated in SMC-GRN. RPH3A is involved in presynaptic vesicle trafficking and has been implicated to play a role in synaptic dysfunction in other neurodegenerative diseases [25, 26]. In addition to the findings in SMC-GRN, we observed some indications of differences already in the presymptomatic stages in GRN mutation carriers. While not statistically significant after adjustment for multiple testing, the differences are still noteworthy since the proteins, NEFM, NPTX2 and CHI3L1, all have been reported as biomarker candidates in CSF [16, 27]. NPTX2 was also elevated in all SMC compared to NC and CHI3L1 was just above the threshold for significance while neither of these two proteins were elevated in SMC when compared to PMC. Taken together this indicates that these two proteins might be upregulated already at the presymptomatic stage. However, further studies are needed to establish if these proteins indeed are related to presymptomatic changes in GRN mutation carriers or if it is a spurious finding.
Biological sex is a known risk factor for several types of dementia, with female sex being a risk factor for AD and male sex being more common in FTD [28, 29]. In light of this, we analysed if any of the proteins identified in the current study exhibited any sex specific patterns. While we could not determine any significant interactions between sex and mutation status for these proteins (data not shown), two proteins were significantly correlated with sex in the mutation carrier group, but not in controls, suggesting a potential biological effect.
We acknowledge several limitations in this study. The focus was on genetic FTD and samples from patients with other neurodegenerative diseases were not included in the analysis. Follow-up studies with comparisons to for example AD and ALS will elucidate the importance of altered plasma proteins in FTD in relation to other diseases as well as sporadic FTD. The suspension bead array technique is a method for analysing multiple proteins simultaneously, which is useful in an exploratory study like this. However, a high-throughput antibody-based single-binder assay can have reduced sensitivity, which may limit the detection of low abundant proteins and require further validation of antibody specificity. In addition, we used a targeted approach, and the protein analysis was thus limited by the protein selection as well as the availability of antibodies.
Conclusions
To our knowledge, this is the first large scale plasma protein profiling specifically in genetic FTD. A reliable fluid biomarker could aid for example in diagnosing FTD at an early stage or in selecting individuals for upcoming clinical trials. Blood-based biomarkers would have the advantage of being easy to access and widely available compared to CSF-biomarkers. Here, we have presented an exploratory study providing proteins, including a previous CSF-biomarker, that are of interest for future investigations as potential biomarkers.
Availability of data and materials
Anonymized data may be shared upon request from a qualified academic investigator for the purpose of replication of the results and procedures detailed in this article. All requests must be in agreement with EU legislation on general data protection and must be in line with the decisions from the Ethical Review Board of Sweden. Data sharing should be regulated in a material transfer agreement and/or data processing agreement as appropriate.
References
van der Ende EL, van Swieten JC. Fluid biomarkers of frontotemporal lobar degeneration. Adv Exp Med Biol. 2021;1281:123–39.
Bridel C, van Wieringen WN, Zetterberg H, Tijms BM, Teunissen CE, Alvarez-Cermeño JC, et al. Diagnostic value of cerebrospinal fluid neurofilament light protein in neurology: a systematic review and meta-analysis. JAMA Neurol. 2019;76(9):1035–48.
van der Ende EL, Xiao M, Xu D, Poos JM, Panman JL, Jiskoot LC, et al. Neuronal pentraxin 2: a synapse-derived CSF biomarker in genetic frontotemporal dementia. J Neurol Neurosurg Psychiatry. 2020;91(6):612–21.
Sleegers K, Brouwers N, Van Damme P, Engelborghs S, Gijselinck I, van der Zee J, et al. Serum biomarker for progranulin-associated frontotemporal lobar degeneration. Ann Neurol. 2009;65(5):603–9.
Heller C, Foiani MS, Moore K, Convery R, Bocchetta M, Neason M, et al. Plasma glial fibrillary acidic protein is raised in progranulin-associated frontotemporal dementia. J Neurol Neurosurg Psychiatry. 2020;91(3):263–70.
Foiani MS, Woollacott IO, Heller C, Bocchetta M, Heslegrave A, Dick KM, et al. Plasma tau is increased in frontotemporal dementia. J Neurol Neurosurg Psychiatry. 2018;89(8):804–7.
Rojas JC, Wang P, Staffaroni AM, Heller C, Cobigo Y, Wolf A, et al. Plasma Neurofilament Light for Prediction of Disease Progression in Familial Frontotemporal Lobar Degeneration. Neurology. 2021May 4;96(18):e2296–312.
Johansson C, Thordardottir S, Laffita-Mesa J, Rodriguez-Vieitez E, Zetterberg H, Blennow K, Graff C. Plasma biomarker profiles in autosomal dominant Alzheimer’s disease. Brain. 2023;146(3):1132–40.
Leuzy A, Cullen NC, Mattsson-Carlgren N, Hansson O. Current advances in plasma and cerebrospinal fluid biomarkers in Alzheimer’s disease. Curr Opin Neurol. 2021;34(2):266–74.
Mofrad RB, Del Campo M, Peeters CFW, Meeter LHH, Seelaar H, Koel-Simmelink M, et al. Plasma proteome profiling identifies changes associated to AD but not to FTD. Acta Neuropathol Commun. 2022;10(1):148.
Rohrer JD, Nicholas JM, Cash DM, van Swieten J, Dopper E, Jiskoot L, et al. Presymptomatic cognitive and neuroanatomical changes in genetic frontotemporal dementia in the Genetic Frontotemporal dementia Initiative (GENFI) study: a cross-sectional analysis. Lancet Neurol. 2015;14(3):253–62.
Schwenk JM, Igel U, Neiman M, Langen H, Becker C, Bjartell A, et al. Toward next generation plasma profiling via heat-induced epitope retrieval and array-based assays. Mol Cell Proteomics. 2010;9(11):2497–507.
Schwenk JM, Gry M, Rimini R, Uhlén M, Nilsson P. Antibody suspension bead arrays within serum proteomics. J Proteome Res. 2008;7(8):3168–79.
Remnestål J, Just D, Mitsios N, Fredolini C, Mulder J, Schwenk JM, et al. CSF profiling of the human brain enriched proteome reveals associations of neuromodulin and neurogranin to Alzheimer’s disease. Proteomics Clin Appl. 2016;10(12):1242–53.
Remnestål J, Öijerstedt L, Ullgren A, Olofsson J, Bergström S, Kultima K, et al. Altered levels of CSF proteins in patients with FTD, presymptomatic mutation carriers and non-carriers. Transl Neurodegener. 2020;9(1):27.
Bergström S, Öijerstedt L, Remnestål J, Olofsson J, Ullgren A, Seelaar H, et al. A panel of CSF proteins separates genetic frontotemporal dementia from presymptomatic mutation carriers: a GENFI study. Mol Neurodegener. 2021;16(1):79.
Sjöstedt E, Zhong W, Fagerberg L, Karlsson M, Mitsios N, Adori C, et al. An atlas of the protein-coding genes in the human, pig, and mouse brain. Science. 2020;367(6482):eaay5947.
R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2022. https://www.R-project.org/.
Hong MG, Lee W, Nilsson P, Pawitan Y, Schwenk JM. Multidimensional normalization to minimize plate effects of suspension bead array data. J Proteome Res. 2016;15(10):3473–80.
Voevodskaya O, Simmons A, Nordenskjöld R, Kullberg J, Ahlström H, Lind L, et al. The effects of intracranial volume adjustment approaches on multiple regional MRI volumes in healthy aging and Alzheimer’s disease. Front Aging Neurosci. 2014;7(6):264.
Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67(1):1–48. https://doi.org/10.18637/jss.v067.i01.
Kuznetsova A, Brockhoff PB, Christensen RHB. lmerTest Package: Tests in Linear Mixed Effects Models. J Stat Softw. 2017;82(13):1–26.
Sogorb-Esteve A, Nilsson J, Swift IJ, Heller C, Bocchetta M, Russell LL, et al. Differential impairment of cerebrospinal fluid synaptic biomarkers in the genetic forms of frontotemporal dementia. Alzheimers Res Ther. 2022;14(1):118.
van der Ende EL, Bron EE, Poos JM, Jiskoot LC, Panman JL, Papma JM, et al. A data-driven disease progression model of fluid biomarkers in genetic frontotemporal dementia. Brain. 2022;145(5):1805–17.
Ferrari E, Scheggia D, Zianni E, Italia M, Brumana M, Palazzolo L, et al. Rabphilin-3A as a novel target to reverse α-synuclein-induced synaptic loss in Parkinson’s disease. Pharmacol Res. 2022;183:106375.
Tan MG, Lee C, Lee JH, Francis PT, Williams RJ, Ramírez MJ, et al. Decreased rabphilin 3A immunoreactivity in Alzheimer’s disease is associated with Aβ burden. Neurochem Int. 2014;64:29–36.
Woollacott IOC, Nicholas JM, Heller C, Foiani MS, Moore KM, Russell LL, et al. Cerebrospinal Fluid YKL-40 and Chitotriosidase Levels in Frontotemporal Dementia Vary by Clinical, Genetic and Pathological Subtype. Dement Geriatr Cogn Disord. 2020;49(1):56–76.
Ferretti MT, Iulita MF, Cavedo E, Chiesa PA, Schumacher Dimech A, Santuccione Chadha A, et al. Sex differences in Alzheimer disease - the gateway to precision medicine. Nat Rev Neurol. 2018;14(8):457–69.
Logroscino G, Piccininni M, Graff C, Hardiman O, Ludolph AC, Moreno F, et al. Incidence of syndromes associated with frontotemporal lobar degeneration in 9 European countries. JAMA Neurol. 2023;30:e225128.
Acknowledgements
First, we would like to thank all the participants and their families for contributing to the study. We would also like to thank the GENFI research coordinators who helped with arranging the visits and the entire staff of the Human Protein Atlas for their efforts.
Genetic Frontotemporal Dementia Initiative (GENFI) collaboration group
Author | Affiliation |
Sónia Afonso | Instituto Ciencias Nucleares Aplicadas a Saude. Universidade de Coimbra. Coimbra. Portugal |
Maria Rosario Almeida | Faculty of Medicine. University of Coimbra. Coimbra. Portugal |
Sarah Anderl-Straub | Department of Neurology. University of Ulm. Ulm. Germany |
Christin Andersson | Department of Clinical Neuroscience. Karolinska Institutet. Stockholm. Sweden |
Anna Antonell | Alzheimer’s disease and Other Cognitive Disorders Unit. Neurology Service. Hospital Clínic. Barcelona. Spain |
Andrea Arighi | Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico. Neurodegenerative Diseases Unit. Milan. Italy; University of Milan. Centro Dino Ferrari. Milan. Italy |
Mircea Balasa | Alzheimer’s disease and Other Cognitive Disorders Unit. Neurology Service. Hospital Clínic. Barcelona. Spain |
Myriam Barandiaran | Cognitive Disorders Unit. Department of Neurology. Donostia University Hospital. San Sebastian. Gipuzkoa. Spain; Neuroscience Area. Biodonostia Health Research Insitute. San Sebastian. Gipuzkoa. Spain |
Nuria Bargalló | Imaging Diagnostic Center. Hospital Clínic. Barcelona. Spain |
Robart Bartha | Department of Medical Biophysics. The University of Western Ontario. London. Ontario. Canada; Centre for Functional and Metabolic Mapping. Robarts Research Institute. The University of Western Ontario. London. Ontario. Canada |
Benjamin Bender | Department of Diagnostic and Interventional Neuroradiology. University of Tübingen. Tübingen. Germany |
Emanuele Buratti | ICGEB Trieste, Italy |
Luisa Benussi | Istituto di Ricovero e Cura a Carattere Scientifico Istituto Centro San Giovanni di Dio Fatebenefratelli. Brescia. Italy |
Maxime Bertoux | Inserm 1172. Lille. France |
Giuliano Binetti | Istituto di Ricovero e Cura a Carattere Scientifico Istituto Centro San Giovanni di Dio Fatebenefratelli. Brescia. Italy |
Sandra Black | Sunnybrook Health Sciences Centre. Sunnybrook Research Institute. University of Toronto. Toronto. Canada |
Martina Bocchetta | Department of Neurodegenerative Disease. Dementia Research Centre. UCL Institute of Neurology. Queen Square. London. UK |
Sergi Borrego-Ecija | Alzheimer’s disease and Other Cognitive Disorders Unit. Neurology Service. Hospital Clínic. Barcelona. Spain |
Jose Bras | Center for Neurodegenerative Science. Van Andel Institute. Grand Rapids. Michigan. MI 49503. USA |
Rose Bruffaerts | Laboratory for Cognitive Neurology. Department of Neurosciences. KU Leuven. Leuven. Belgium |
Marta Cañada | CITA Alzheimer. San Sebastian. Gipuzkoa. Spain |
Valentina Cantoni | Centre for Neurodegenerative Disorders. Neurology Unit. Department of Clinical and Experimental Sciences. University of Brescia. Brescia. Italy |
Paola Caroppo | Fondazione IRCCS Istituto Neurologico Carlo Besta. Milano. Italy |
David Cash | Department of Neurodegenerative Disease. Dementia Research Centre. UCL Institute of Neurology. Queen Square. London. UK |
Miguel Castelo-Branco | Faculty of Medicine. University of Coimbra. Coimbra. Portugal |
Rhian Convery | Department of Neurodegenerative Disease. Dementia Research Centre. UCL Institute of Neurology. Queen Square. London. UK |
Thomas Cope | Department of Clinical Neuroscience. University of Cambridge. Cambridge. UK |
Vincent Deramecourt | Univ Lille. France |
Giuseppe Di Fede | Fondazione IRCCS Istituto Neurologico Carlo Besta. Milano. Italy |
Alina Díez | Neuroscience Area. Biodonostia Health Research Insitute. San Sebastian. Gipuzkoa. Spain |
Chiara Fenoglio | Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico. Neurodegenerative Diseases Unit. Milan. Italy; University of Milan. Centro Dino Ferrari. Milan. Italy |
Catarina B. Ferreira | Laboratory of Neurosciences. Institute of Molecular Medicine. Faculty of Medicine. University of Lisbon. Lisbon. Portugal |
Nick Fox | Department of Neurodegenerative Disease. Dementia Research Centre. UCL Institute of Neurology. Queen Square. London. UK |
Morris Freedman | Baycrest Health Sciences. Rotman Research Institute. University of Toronto. Toronto. Canada |
Giorgio Fumagalli | Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico. Neurodegenerative Diseases Unit. Milan. Italy; University of Milan. Centro Dino Ferrari. Milan. Italy |
Aurélie Funkiewiez | Centre de référence des démences rares ou précoces. IM2A. Département de Neurologie. AP-HP—Hôpital Pitié-Salpêtrière. Paris. France |
Alazne Gabilondo | Neuroscience Area. Biodonostia Health Research Insitute. San Sebastian. Gipuzkoa. Spain |
Roberto Gasparotti | Neuroradiology Unit. University of Brescia. Brescia. Italy |
Serge Gauthier | Alzheimer Disease Research Unit. McGill Centre for Studies in Aging. Department of Neurology & Neurosurgery. McGill University. Montreal. Québec. Canada |
Antonella Alberici | Centre for Neurodegenerative Disorders, Department of Clinical and Experimental Sciences, University of Brescia, Brescia, Italy |
Giorgio Giaccone | Fondazione IRCCS Istituto Neurologico Carlo Besta. Milano. Italy |
Ana Gorostidi | Neuroscience Area. Biodonostia Health Research Insitute. San Sebastian. Gipuzkoa. Spain |
Caroline Greaves | Department of Neurodegenerative Disease. Dementia Research Centre. UCL Institute of Neurology. Queen Square. London. UK |
Rita Guerreiro | Center for Neurodegenerative Science. Van Andel Institute. Grand Rapids. Michigan. MI 49503. USA |
Carolin Heller | Department of Neurodegenerative Disease. Dementia Research Centre. UCL Institute of Neurology. Queen Square. London. UK |
Begoña Indakoetxea | Cognitive Disorders Unit. Department of Neurology. Donostia University Hospital. San Sebastian. Gipuzkoa. Spain; Neuroscience Area. Biodonostia Health Research Insitute. San Sebastian. Gipuzkoa. Spain |
Vesna Jelic | Division of Clinical Geriatrics. Karolinska Institutet. Stockholm. Sweden |
Hans-Otto Karnath | Division of Neuropsychology. Hertie-Institute for Clinical Brain Research and Center of Neurology. University of Tübingen. Tübingen. Germany |
Ron Keren | The University Health Network. Toronto Rehabilitation Institute. Toronto. Canada |
Gregory Kuchcinski | Univ Lille. France |
Tobias Langheinrich | Division of Neuroscience and Experimental Psychology. Wolfson Molecular Imaging Centre. University of Manchester. Manchester. UK |
Thibaud Lebouvier | Univ Lille. France |
Maria João Leitão | Centre of Neurosciences and Cell Biology. Universidade de Coimbra. Coimbra. Portugal |
Albert Lladó | Alzheimer’s disease and Other Cognitive Disorders Unit. Neurology Service. Hospital Clínic. Barcelona. Spain |
Carolina Maruta | Laboratory of Language Research. Centro de Estudos Egas Moniz. Faculty of Medicine. University of Lisbon. Lisbon. Portugal |
Simon Mead | MRC Prion Unit. Department of Neurodegenerative Disease. UCL Institute of Neurology. Queen Square. London. UK |
Lieke Meeter | Department of Neurology. Erasmus Medical Center. Rotterdam. Netherlands |
Gabriel Miltenberger | Faculty of Medicine. University of Lisbon. Lisbon. Portugal |
Rick van Minkelen | Department of Clinical Genetics. Erasmus Medical Center. Rotterdam. Netherlands |
Sara Mitchell | Sunnybrook Health Sciences Centre. Sunnybrook Research Institute. University of Toronto. Toronto. Canada |
Katrina Moore | Department of Neurodegenerative Disease. Dementia Research Centre. UCL Institute of Neurology. Queen Square. London. UK |
Jennifer Nicholas | Department of Medical Statistics. London School of Hygiene and Tropical Medicine. London. UK |
Jaume Olives | Alzheimer’s disease and Other Cognitive Disorders Unit. Neurology Service. Hospital Clínic. Barcelona. Spain |
Sebastien Ourselin | School of Biomedical Engineering & Imaging Sciences. King's College London. London. UK |
Alessandro Padovani | Centre for Neurodegenerative Disorders. Department of Clinical and Experimental Sciences. University of Brescia. Italy |
Jessica Panman | Department of Neurology. Erasmus Medical Center. Rotterdam. Netherlands |
Janne M. Papma | Department of Neurology. Erasmus Medical Center. Rotterdam. Netherlands |
Georgia Peakman | Department of Neurodegenerative Disease. Dementia Research Centre. UCL Institute of Neurology. Queen Square. London. UK |
Michela Pievani | Istituto di Ricovero e Cura a Carattere Scientifico Istituto Centro San Giovanni di Dio Fatebenefratelli. Brescia. Italy |
Yolande Pijnenburg | Amsterdam University Medical Centre. Amsterdam VUmc. Amsterdam. Netherlands |
Enrico Premi | Stroke Unit. ASST Brescia Hospital. Brescia. Italy |
Sara Prioni | Fondazione IRCCS Istituto Neurologico Carlo Besta. Milano. Italy |
Rosa Rademakers | Department of Neurosciences. Mayo Clinic. Jacksonville. Florida. USA |
Veronica Redaelli | Fondazione IRCCS Istituto Neurologico Carlo Besta. Milano. Italy |
Daisy Rinaldi | Centre de référence des démences rares ou précoces. IM2A. Département de Neurologie. AP-HP—Hôpital Pitié-Salpêtrière. Paris. France |
Tim Rittman | Department of Clinical Neurosciences. University of Cambridge. Cambridge. UK |
Ekaterina Rogaeva | Tanz Centre for Research in Neurodegenerative Diseases. University of Toronto. Toronto. Canada |
Adeline Rollin | CHU. CNR-MAJ. Labex Distalz. LiCEND Lille. France |
Pedro Rosa-Neto | Translational Neuroimaging Laboratory. McGill Centre for Studies in Aging. McGill University. Montreal. Québec. Canada |
Giacomina Rossi | Fondazione IRCCS Istituto Neurologico Carlo Besta. Milano. Italy |
Martin Rosser | Department of Neurodegenerative Disease. Dementia Research Centre. UCL Institute of Neurology. Queen Square. London. UK |
Elio Scarpini | Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico. Neurodegenerative Diseases Unit. Milan. Italy; University of Milan. Centro Dino Ferrari. Milan. Italy |
Elisa Semler | Department of Neurology. University of Ulm. Ulm |
Rachelle Shafei | Department of Neurodegenerative Disease. Dementia Research Centre. UCL Institute of Neurology. Queen Square. London. UK |
Christen Shoesmith | Department of Clinical Neurological Sciences. University of Western Ontario. London. Ontario. Canada |
Miguel Tábuas-Pereira | Neurology Department. Centro Hospitalar e Universitario de Coimbra. Coimbra. Portugal; Faculty of Medicine, University of Coimbra, Coimbra, Portugal |
Mikel Tainta | Neuroscience Area. Biodonostia Health Research Insitute. San Sebastian. Gipuzkoa. Spain |
Ricardo Taipa | Neuropathology Unit and Department of Neurology. Centro Hospitalar do Porto—Hospital de Santo António. Oporto. Portugal |
David Tang-Wai | The University Health Network. Krembil Research Institute. Toronto. Canada |
David L Thomas | Neuroimaging Analysis Centre. Department of Brain Repair and Rehabilitation. UCL Institute of Neurology. Queen Square. London. UK |
Paul Thompson | Division of Neuroscience and Experimental Psychology. Wolfson Molecular Imaging Centre. University of Manchester. Manchester. UK |
Håkan Thonberg | Center for Alzheimer Research. Division of Neurogeriatrics. Karolinska Institutet. Stockholm. Sweden |
Carolyn Timberlake | Department of Clinical Neurosciences. University of Cambridge. Cambridge. UK |
Pietro Tiraboschi | Fondazione IRCCS Istituto Neurologico Carlo Besta. Milano. Italy |
Emily Todd | Department of Neurodegenerative Disease. Dementia Research Centre. UCL Institute of Neurology. Queen Square. London. UK |
Philip Van Damme | Neurology Service. University Hospitals Leuven. Belgium; Laboratory for Neurobiology. VIB-KU Leuven Centre for Brain Research. Leuven. Belgium |
Mathieu Vandenbulcke | Geriatric Psychiatry Service. University Hospitals Leuven. Belgium; Neuropsychiatry. Department of Neurosciences. KU Leuven. Leuven. Belgium |
Michele Veldsman | Nuffield Department of Clinical Neurosciences. Medical Sciences Division. University of Oxford. Oxford. UK |
Ana Verdelho | Department of Neurosciences and Mental Health. Centro Hospitalar Lisboa Norte—Hospital de Santa Maria & Faculty of Medicine. University of Lisbon. Lisbon. Portugal |
Jorge Villanua | OSATEK. University of Donostia. San Sebastian. Gipuzkoa. Spain |
Jason Warren | Department of Neurodegenerative Disease. Dementia Research Centre. UCL Institute of Neurology. Queen Square. London. UK |
Carlo Wilke | Department of Neurodegenerative Diseases. Hertie-Institute for Clinical Brain Research and Center of Neurology. University of Tübingen. Tübingen. Germany; Center for Neurodegenerative Diseases (DZNE). Tübingen. Germany |
Ione Woollacott | Department of Neurodegenerative Disease. Dementia Research Centre. UCL Institute of Neurology. Queen Square. London. UK |
Henrik Zetterberg | Dementia Research Institute. Department of Neurodegenerative Disease. UCL Institute of Neurology. Queen Square. London. UK |
Miren Zulaica | Neuroscience Area. Biodonostia Health Research Insitute. San Sebastian. Gipuzkoa. Spain |
João Durães | Neurology Department, Centro Hospitalar e Universitario de Coimbra, Coimbra, Portugal |
Marisa Lima | Neurology Department, Centro Hospitalar e Universitario de Coimbra, Coimbra, Portugal |
João Lemos | Faculty of Medicine, University of Coimbra, Coimbra, Portugal |
Funding
Open access funding provided by Karolinska Institute. C.G. received funding from EU Joint Programme—Neurodegenerative Disease Research -Prefrontals Vetenskapsrådet Dnr 529–2014-7504, Vetenskapsrådet 2015–02926, Vetenskapsrådet 2018–02754, the Swedish FTD Inititative-Schörling Foundation, Alzheimer Foundation, Brain Foundation, Dementia Foundation and Region Stockholm ALF-project. PN received funding from KTH Center for Applied Precision Medicine (KCAP) funded by the Erling-Persson Family Foundation, the Swedish FTD Inititative-Schörling Foundation and Åhlén foundation. D.G. received support from the EU Joint Programme—Neurodegenerative Disease Research and the Italian Ministry of Health (PreFrontALS) grant 733051042. E.F. has received funding from a Canadian Institute of Health Research grant #327387. F.M. received funding from the Tau Consortium and the Center for Networked Biomedical Research on Neurodegenerative Disease. J.B.R. has received funding from the Welcome Trust (103838) and is supported by the Cambridge University Centre for Frontotemporal Dementia, the Medical Research Council (SUAG/051 G101400) and the National Institute for Health Research Cambridge Biomedical Research Centre (BRC-1215–20014). J.C.V.S. was supported by the Dioraphte Foundation grant 09–02-03–00, Association for Frontotemporal Dementias Research Grant 2009, Netherlands Organization for Scientific Research grant HCMI 056–13-018, ZonMw Memorabel (Deltaplan Dementie, project number 733 051 042), Alzheimer Nederland and the Bluefield Project. J.D.R. is supported by the Bluefield Project and the National Institute for Health and Care Research University College London Hospitals Biomedical Research Centre, and has received funding from an MRC Clinician Scientist Fellowship (MR/M008525/1) and a Miriam Marks Brain Research UK Senior Fellowship. M.M. has received funding from a Canadian Institute of Health Research operating grant and the Weston Brain Institute and Ontario Brain Institute. M.O. has received funding from Germany’s Federal Ministry of Education and Research (BMBF). R.S-V. is supported by Alzheimer’s Research UK Clinical Research Training Fellowship (ARUK-CRF2017B-2) and has received funding from Fundació Marató de TV3, Spain (grant no. 20143810). R.V. has received funding from the Mady Browaeys Fund for Research into Frontotemporal Dementia. This work was also supported by the EU Joint Programme—Neurodegenerative Disease Research GENFI-PROX grant [2019–02248; to J.D.R., M.O., B.B., C.G., J.C.V.S. and M.S.
Author information
Authors and Affiliations
Consortia
Contributions
AU, LÖ, JO, PN and CG developed the experimental design. LÖ and CG contributed to study coordination and sample collection. JO performed the experimental work with support from SB and JR. AU and LÖ analysed and interpreted the data with support from JO, SB, JR, AM, PN and CG. CG, PN and AM supervised the project. AU, CG and LÖ drafted and revised the manuscript with input from JO, SB, JR, AM, and PN. All other authors contributed to the sample collection, acquisition of data and they critically reviewed and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The GENFI-study was performed in accordance with the Declaration of Helsinki, reviewed and approved by all countries’ respective Ethics committees and all participants signed an informed consent to take part in the research. This research study was performed in Sweden an approved by the Ethical Review Board (EPN) Dnr 2012/1611–31/1 and 2017/2097–32.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interest relevant to the work conducted in the presented study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
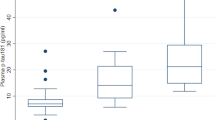
Supplementary Table 1. Antibodies used in the suspension bead array plasma analysis. Supplementary Table 2. Proteins with different levels in PMC compared to NC. Supplementary Figure 1. Boxplots for the 13 proteins that differed between SMC and NC. Supplementary Figure 2. Boxplots for the 10 proteins that differed between SMC and PMC.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ullgren, A., Öijerstedt, L., Olofsson, J. et al. Altered plasma protein profiles in genetic FTD – a GENFI study. Mol Neurodegeneration 18, 85 (2023). https://doi.org/10.1186/s13024-023-00677-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13024-023-00677-6