Abstract
Background
As the most common subtype of adult muscular dystrophy worldwide, large cohort reports on myotonic dystrophy type I (DM1) in China are still lacking. This study aims to analyze the genetic and clinical characteristics of Chinese Han DM1 patients.
Methods
Based on the multicenter collaborating effort of the Pan-Yangtze River Delta Alliance for Neuromuscular Disorders, patients with suspected clinical diagnoses of DM1 were genetically confirmed from January 2020 to April 2023. Peak CTG repeats in the DMPK gene were analyzed using triplet repeat-primed PCR (TP-PCR) and flanking PCR. Time-to-event analysis of onset age in females and males was performed. Additionally, detailed clinical features and longitudinal changes from the disease onset in 64 DM1 patients were retrospectively collected and analyzed. The Epworth Sleepiness Scale and Fatigue Severity Scale were used to quantify the severity of daytime sleepiness and fatigue.
Results
Among the 211 genetically confirmed DM1 patients, the mean age at diagnosis was 40.9 ± 12.2 (range: 12–74) with a male-to-female ratio of 124:87. The average size of CTG repeats was 511.3 (range: 92–1945). Among the DM1 patients with comprehensive clinical data (n = 64, mean age 41.0 ± 12.0), the age at onset was significantly earlier in males than in females (4.8 years earlier, p = 0.026). Muscle weakness (92.2%), myotonia (85.9%), and fatigue (73.4%) were the most prevalent clinical features. The predominant involved muscles at onset are hands (weakness or myotonia) (52.6%) and legs (walking disability) (42.1%). Of them, 70.3% of patients had daytime sleepiness, 14.1% had cataract surgery, 7.8% used wheelchairs, 4.7% required ventilatory support, and 1.6% required gastric tubes. Regarding the comorbidities, 4.7% of patients had tumors, 17.2% had diabetes, 23.4% had dyspnea, 28.1% had intermittent insomnia, 43.8% experienced dysphagia, and 25% exhibited cognitive impairment. Chinese patients exhibited smaller size of CTG repeats (468 ± 139) than those reported in Italy (613 ± 623), the US (629 ± 386), and Japan (625 [302, 1047]), and milder phenotypes with less multisystem involvement.
Conclusion
The Chinese Han DM1 patients presented milder phenotypes compared to their Caucasian and Japanese counterparts. A male predominance and an early age of onset were identified in male Chinese Han DM1 patients.
Similar content being viewed by others
Background
Myotonic dystrophy (DM) is the most prevalent type of muscular dystrophy in adults worldwide (0.37–36.29 cases per 100,000) [1]. It is more than just a progressive degenerative disease confined in skeletal muscles. Multiorgan involvement is highly common in DM patients, encompassing conditions such as cataracts, cardiac conduction abnormalities, infertility, insulin resistance, and so on [2]. DM can be further categorized into DM1 and DM2 according to the different responding genes. DM1 is caused by an expansion of cytosine-thymine-guanine (CTG) trinucleotide repeats in the 3′-untranslated region of the DMPK gene and typically presents with more severe symptoms and a higher prevalence than DM2, which is caused by tetranucleotide repeat expansion located in the CNBP gene. Normal DMPK gene alleles contain 5–34 CTG repeats, while repeats ranging from 51 to 100 are defined as protomutations. Typically, longer CTG expansions in DMPK are responsible for an earlier onset phenotype and severe forms of DM1. These range from late-onset DM1 (100–600 repeats) to adult DM1 (250–750 repeats), childhood DM1 (400–1000 repeats), and congenital DM1 (> 750 repeats) [3]. Most DM1 patients become symptomatic during the second, third, or fourth decade of life, which is termed adult DM1 (classical DM1).
DM1 is much less prevalent in Asia. Compared to the reported global prevalence (9.27 per 100,000), the prevalence of DM1 is 0.77, 0.45, and 0.37 per 100,000 in South Korea, Taiwan, and Hong Kong, respectively [4,5,6]. Apart from the disease prevalence, clinical features in non-Caucasian DM1 were considerably different from their Caucasian counterparts. For instance, cardiac defects, cataracts, and sleep disturbances were less common in a retrospective study of 37 Chinese DM1 patients [7]. Similarly, a lower prevalence of conduction abnormalities and arrhythmia was reported in a South Korean nationwide study [4]. Hence, the clinical and genetic features of non-Caucasian DM1 patients could expand the global spectrum of DM1. To evaluate the genetic and clinical features of Chinese DM1 patients, we performed this alliance-based multicenter cohort study in genetically confirmed DM1 patients (n = 211). Among them, clinical features of 64 DM1 patients including multi-organ symptoms, age of onset, comorbidities, fatigue and sleepiness scales, and current medications were analyzed.
Method
Patients with DM1 were enrolled from January 2020 to April 2023 through the collaborative efforts of the Pan-Yangtze River Delta Alliance for Neuromuscular Disorders (PYDAN) network in China [8,9,10]. Written informed consent to be included in the study was obtained from all patients. The study was approved by the ethics committee of Huashan Hospital (2020–008) and other participating hospitals and was registered on clinicaltrials.gov (NCT06101940). The clinical diagnosis of DM1 was based on classical clinical presentations, electromyography, and family history.
The genetic diagnosis of DM1 was set at an abnormal CTG expansion in the DMPK gene (≥ 50 repeats). The peak CTG repeats were measured using flanking PCR and triplet repeat-primed PCR (TP-PCR) [11]. All blood samples were collected and analyzed by the Shanghai Amplicon-gene medical test laboratory using a self-developed DMPK sizing kit. The TP-PCR cycle comprised of an initial denaturation step at 94 °C for 30 s followed by 38 cycles of 94 °C for 30 s, 66 °C for 90 s, with a final extension step at 4 °C for 10 min. TP-PCR amplification products were analyzed by capillary electrophoresis, and the final peak of each sample was identified based on signal height and/or peak morphology [12].
Detailed clinical information of 64 DM1 patients was analyzed, which included: (1) demographics; (2) clinical features (first symptom, myotonia, cognitive impairment, tumor, glucose metabolism, daily sleep, histories of cataract surgery, wheelchair use, cardiac pacemaker implantation, and the use of gastric tubes and respirators); (3) clinical scales including the Epworth Sleepiness Scale (ESS) and Fatigue Severity Scale (FSS) which were used to quantitatively measure daytime sleepiness and fatigue respectively. Daytime sleepiness was defined as an ESS score ≥ 36, and fatigue was defined as an FSS score ≥ 10 based on the suggested threshold scores [13, 14]. Additionally, current medication and main diet were also analyzed. The onset age of DM1 was defined as the onset of noticeable clinical symptoms.
All data and figures were analyzed and generated using R (version 4.3.1). The time-to-event analysis of onset age with respect to sex was conducted using the Log-rank test, utilizing the ‘survminer’ R package. Comparisons of clinical features between true and absent groups, in terms of onset age, were calculated using the Wilcoxon test and the ‘ggpubr’ R package. Additionally, mean values were reported as mean ± SD, and median values were reported as median [0.25 quantile, 0.75 quantile].
Results
Among 230 Chinese Han individuals with clinically suspected DM1, 211 cases were finally genetically confirmed (91.7%). These patients were from 11 provinces across China (except the Northwest region), most of whom (75%) were from East China (Fig. 1). This gave a minimal disease prevalence of 0.13/100,000. The mean age in 211 DM1 patients was 40.9 ± 12.2 and the male-to-female ratio was 124:87. Among them, 92.2% (195/211) had myotonic discharges and myogenic changes in electromyography studies and 20.4% (42/211) had a positive family history. The mean peak CTG repeat length in the DMPK gene was 511.3, ranging from a minimum of 92 to a maximum of 1945 repeats. The distribution of peak CTG repeats was similar between male and female patients, with an average length of approximately 500 repeats (Fig. 2a). More specifically, the average peak CTG repeats were 454.6 ± 248.4 in 124 male patients (mean age 40.9 ± 12.9) and 511.3 ± 358.8 in 87 female patients (mean age 42.0 ± 11.2). However, a time-to-event analysis of onset age by sex revealed an earlier onset in males by 4.8 years (average onset age) (p = 0.026) in those 64 patients with detailed clinical information (Fig. 2b).
Among the 64 DM1 patients with detailed clinical data (mean age 41.0 ± 12.0, male: female ratio = 36: 28, CTG repeats 468 ± 139), the most common clinical features observed were muscle weakness (92.2%), myotonia (85.9%), fatigue (73.4%) (Table 1). The onset symptoms mostly presented in hand muscles (weakness or myotonia) (52.6%) and legs (walking disability) (42.1%), and others included vision impairment, persistent fatigue, or cognitive decline. Additionally, 70.3% of patients had daytime sleepiness, 14.1% had undergone cataract surgery, 7.8% used wheelchairs, 4.7% required respirators, and 1.6% needed gastric tubes. Furthermore, 31.3% of patients had frequent heart palpitations (no cardiac device implantation or ablation procedures), 4.7% of patients had tumors (thyroid cancer), 17.2% had diabetes, 23.4% experienced dyspnea, 28.1% occasionally suffered from insomnia, 43.8% reported dysphagia, and 25% exhibited cognitive impairment, primarily in the form of memory decline. In summary, 7.8% of patients were highly disabled as defined by being wheelchair-bound, requiring ventilatory support, or using a gastric tube.
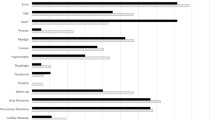
In terms of medication, 51.6% of patients took mexiletine, and 26.6% took coenzyme Q10. There were no food restrictions for most patients (84.4%). However, 3.1% of patients were meat-oriented, 6.3% of patients were vegetable-oriented, and 6.3% of patients had swallowing difficulty with food restricted in soft fluid. There were no apparent correlations between peak CTG repeats in the DMPK gene and the severity of symptoms. However, patients with an earlier age of onset were prone to present symptoms including myotonia, memory impairment, insomnia, and dysphagia (Fig. 3).
Onset age difference in various clinical features in Chinese Han DM1 patients. Daytime sleepiness was defined as an Epworth Sleepiness Scale (ESS) score ≥ 36, and fatigue was defined as a Fatigue Severity Scale (FSS) score ≥ 10, in accordance with the suggested threshold scores provided by the scales
Compared to adult DM1 patients with the same age at diagnosis and onset reported in other ethnicities (Table 2), Chinese DM1 exhibited fewer CTG repeats (468 ± 139) than those reported in Italy (613 ± 623) [15], the US (629 ± 386) [16], and Japan (625 [302, 1047]) [17]. More importantly, the Chinese patients also presented less multisystem impairments, with lower proportions of cataracts (14–30%) and cardiac defects (35%) reported compared to their Caucasian and Japanese counterparts.
Discussion
This retrospective cross-sectional study primarily analyzed the genetic and clinical features of Chinese DM1 patients, revealing two key characteristics among our patients. First, there is a relatively less severe form of DM1 in Chinese patients compared to their Caucasian counterparts. Second, there is a male dominance in sex composition and disease severity among our DM1 cohort.
The overall milder form of DM1 in Chinese patients may be attributed to the lower CTG repeats in the DMPK gene. Previous studies have reported significantly lower CTG repeat numbers (less than 19 times) in the Chinese Han normal population (1.0%) when compared to Caucasians (10.0%) and Japanese (8.5%) [18, 19]. This difference in CTG repeat length may also explain the lower estimated prevalence and fewer previous reports of Chinese Han DM1 patients. The lower CTG repeat numbers also influence the most common symptom composition in Chinese Han patients. Lu et al. reported lower rates of cataracts (32.4%), cardiac defects (16.2%), and daytime sleepiness (32.4%) in a cohort of 37 Chinese Han DM1 patients [7]. These three key features are typically common in Caucasians and Japanese DM1, often with a proportion that exceeds 50% [17, 20]. The results of our study are generally consistent with those of Lu et al., although we identified a much higher prevalence of daytime sleepiness (70.3%). This difference might be attributed to our use of a more objective method, the ESS score, to measure daytime sleepiness. Additionally, an increased proportion of muscle weakness and higher FSS scores, along with the increasing CTG repeats were identified in our cohort, which supports the correlation between CTG repeats and severity.
The predominance of males in both sex composition and severity is evident in our DM1 cohort. While gender differences may not be apparent in some populations, a nationwide French study of 1409 adult DM1 patients identified gender as a modifying factor influencing DM1 phenotype severity and mortality. They found that male patients were more likely to exhibit more severe muscular disability with marked myotonia, muscle weakness, cardiac issues, and respiratory involvement compared to female patients [21]. A similar myotonia situation was also reported in a UK Myotonic Dystrophy Patient Registry study (n = 556) [22]. Our study also revealed a higher severity of DM1 in male patients. It’s possible that sex hormones may play a role in modifying the myotonic phenotype by affecting ion channels [23]. However, further clinical, and basic research is needed to fully explain this phenomenon.
This study has several limitations. First, flanking PCR and TP-PCR are not suitable for the accurate analysis of somatic mosaicism in CTG repeats. The estimated progenitor allele length could not be determined in this study. Second, the absence of detailed survey responses in some patients may cause information and selection biases in this study. Since the patients with severe cognitive impairment may not respond to our survey in time, the overall DM1 phenotypes of the Chinese population may be more severe. Fourth, clinical data was retrospectively collected, thus we can not collect enough baseline variables to explore the factors affecting the onset age and other clinical outcomes.
Conclusions
In summary, this retrospective cohort study summarized the genetic and clinical features of Han Chinese DM1 patients. Chinese DM1 patients exhibited a milder form of the condition compared to their Caucasian and Japanese counterparts and displayed a different clinical phenotype. This complements the global clinical spectrum of DM1.
Data availability
For privacy reasons, the data is available from the corresponding author upon request.
References
Liao Q, Zhang Y, He J, Huang K. Global prevalence of myotonic dystrophy: an updated systematic review and meta-analysis. Neuroepidemiology. 2022;56:163–73.
Udd B, Krahe R. The myotonic dystrophies: molecular, clinical, and therapeutic challenges. Lancet Neurol. 2012;11:891–905.
Yum K, Wang ET, Kalsotra A. Myotonic dystrophy: disease repeat range, penetrance, age of onset, and relationship between repeat size and phenotypes. Curr Opin Genet Dev. 2017;44:30–7.
Lee J-Y, Jeong H-N. Nationwide incidence of myotonic dystrophy type 1 and the status of multi-organ involvement. J Neurol. 2022;269:2666–72.
Hsiao KM, Chen SS, Li SY, Chiang SY, Lin HM, Pan H, et al. Epidemiological and genetic studies of myotonic dystrophy type 1 in Taiwan. Neuroepidemiology. 2003;22:283–9.
Chung B, Wong V, Ip P. Prevalence of neuromuscular diseases in Chinese children: a study in Southern China. J Child Neurol. 2003;18:217–9.
Lu H, Li Y, Sadowsky M, Da Y. Clinical characteristics of 37 Chinese patients with myotonic dystrophy type 1. Brain Circ. 2016;2:95–8.
Zhong H, Ruan Z, Yan C, Lv Z, Zheng X, Goh L-Y, et al. Short-term outcome prediction for myasthenia gravis: an explainable machine learning model. Ther Adv Neurol Disord. 2023;16:17562864231154976.
Jiao K, Dong J, Luo S, Yu L, Ke Q, Wang Z, et al. High-risk screening of late-onset Pompe disease: a different early portrait in China. Front Neurol. 2022. https://doi.org/10.3389/fneur.2022.965207.
Wang Y, Huan X, Jiao K, Jiang Q, Goh L-Y, Shi J, et al. Plasma exchange versus intravenous immunoglobulin in AChR subtype myasthenic crisis: a prospective cohort study. Clin Immunol. 2022;241:109058.
Pešović J, Perić S, Brkušanin M, Brajušković G, Rakočević-Stojanović V, Savić-Pavićević D. Molecular genetic and clinical characterization of myotonic dystrophy type 1 patients carrying variant repeats within DMPK expansions. Neurogenetics. 2017;18:207–18.
Leferink M, Wong DPW, Cai S, Yeo M, Ho J, Lian M, et al. Robust and accurate detection and sizing of repeats within the DMPK gene using a novel TP-PCR test. Sci Rep. 2019;9:8280.
Lapin BR, Bena JF, Walia HK, Moul DE. The epworth sleepiness scale: validation of one-dimensional factor structure in a large clinical sample. J Clin Sleep Med. 2018;14:1293–301.
Valko PO, Bassetti CL, Bloch KE, Held U, Baumann CR. Validation of the fatigue severity scale in a swiss cohort. Sleep. 2008;31:1601–7.
Rossi S, Della Marca G, Ricci M, Perna A, Nicoletti TF, Brunetti V, et al. Prevalence and predictor factors of respiratory impairment in a large cohort of patients with myotonic dystrophy type 1 (DM1): a retrospective, cross sectional study. J Neurol Sci. 2019;399:118–24.
Groh WJ, Groh MR, Shen C, Monckton DG, Bodkin CL, Pascuzzi RM. Survival and CTG repeat expansion in adults with myotonic dystrophy type 1. Muscle Nerve. 2011;43:648–51.
Yamauchi K, Matsumura T, Takada H, Kuru S, Kobayashi M, Kubota T, et al. The current status of medical care for myotonic dystrophy type 1 in the national registry of Japan. Muscle Nerve. 2023;67:387–93.
Sizhong Z, Hui W, Agen P, Cuiying X, Ge Z, Yiping H, et al. Low incidence of myotonic dystrophy in Chinese Hans is associated with a lower number of CTG trinucleotide repeats. Am J Med Genet. 2000;96:425–8.
Pan H, Lin HM, Ku WY, Li TC, Li SY, Lin CC, et al. Haplotype analysis of the myotonic dystrophy type 1 (DM1) locus in Taiwan: implications for low prevalence and founder mutations of Taiwanese myotonic dystrophy type 1. Eur J Hum Genet. 2001;9:638–41.
Petri H, Witting N, Ersbøll MK, Sajadieh A, Dunø M, Helweg-Larsen S, et al. High prevalence of cardiac involvement in patients with myotonic dystrophy type 1: a cross-sectional study. Int J Cardiol. 2014;174:31–6.
Dogan C, De Antonio M, Hamroun D, Varet H, Fabbro M, Rougier F, et al. Gender as a modifying factor influencing myotonic dystrophy type 1 phenotype severity and mortality: a nationwide multiple databases cross-sectional observational study. PLoS ONE. 2016;11:e0148264.
Wood L, Cordts I, Atalaia A, Marini-Bettolo C, Maddison P, Phillips M, et al. The UK myotonic dystrophy patient registry: facilitating and accelerating clinical research. J Neurol. 2017;264:979–88.
Fialho D, Kullmann DM, Hanna MG, Schorge S. Non-genomic effects of sex hormones on CLC-1 may contribute to gender differences in myotonia congenita. Neuromuscul Disord NMD. 2008;18:869–72.
Peric S, Stojanovic VR, Basta I, et al. Influence of multisystemic affection on health-related quality of life in patients with myotonic dystrophy type 1. Clin Neurol Neurosurg. 2013;115(3):270–5. https://doi.org/10.1016/j.clineuro.2012.05.015.
Hagerman KA, Howe SJ, Heatwole CR. Christopher Project Reference Group. The myotonic dystrophy experience: a North American cross-sectional study. Muscle Nerve. 2019;59(4):457–64. https://doi.org/10.1002/mus.26420.
Papadimas GK, Papadopoulos C, Kekou K, et al. A Greek National Cross-Sectional Study on Myotonic Dystrophies. Int J Mol Sci. 2022;23(24):15507. https://doi.org/10.3390/ijms232415507.
Acknowledgements
We would like to extend our special thanks to the DM1 patients and their families for participating in the survey of their disease condition. Additionally, we want to express our gratitude to the members of the PYDAN network for their assistance with data collection and cooperation. We also thank Shanghai Amplicongene Corp. for their assistance in this study.
Funding
This study was funded by China’s National Key R&D Program (No. 2022YFC3501303, 2022YFC3501305), National Natural Science Foundation of China (No. 82071410, 82001335), Shanghai Municipal Science and Technology Major Project (No.2018SHZDZX01), and ZJLab.
Author information
Authors and Affiliations
Contributions
HHZ, LZ, JHL, CBZ, and SSL contributed to the conceptual design of the study. HHZ and LZ contributed to the data analysis and the first draft. XFY, QK, JHD, YC, LJL, XLC, JHG, YQW, HX, RRL, CXL, JBW, JL, JYX, WHZ, ST, and FCL contributed to the data collection and participated in the drafting and critical revision of the article.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethic committee of Huashan Hospital and other participating hospitals (2020–008) and registered on clinicaltrials.gov (NCT06101940). Written informed consent was acquired from every participant according to the Declaration of Helsinki.
Consent for publication
All authors have consented to the publication of this manuscript.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhong, H., Zeng, L., Yu, X. et al. Clinical features and genetic spectrum of a multicenter Chinese cohort with myotonic dystrophy type 1. Orphanet J Rare Dis 19, 103 (2024). https://doi.org/10.1186/s13023-024-03114-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13023-024-03114-z