Abstract
Background
While substantial placebos have been used in herbal medicine (HM) clinical trials for rare diseases, the use and quality of reporting of HM-placebo remain unclear. We aim to describe the use of HM-placebo in clinical trials for rare diseases and determine the quality of reporting in these trials.
Methods
This is a cross-sectional study. We searched PubMed, Embase, Web of Science, SinoMed, China National Knowledge Infrastructure, WanFang database, China Science and Technology Journal Database, National Institute of Informatics Support Academic Information Services, ClinicalTrials.gov and Chinese Clinical Trials Registry from their inception date to 14 February 2023 to identify registered and published trials that use placebos as a comparator in rare diseases. We collected data on placebo use reporting and the efficacy and safety of placebo. Descriptive statistics, the Chi-square test, and Binary multivariable logistic regression analysis were used to determine the placebo characteristics of the HM trial and its effect on reporting.
Results
Among the 55 studies, we included that with a median administration time of placebo of 84 days (IQR 42–180) and a median placebo sample size of 30 (IQR 24–54). About half of the trials (27, 49.1%) did not provide their ethical approvals, and one trial had details of informed consent. None of the studies were fully reported and more than half of the items reported less than 50%. A total of 10 trials (18.2%) of placebo has active ingredients even though none of them performed pharmacological inert tests. Of the 29 studies with available data on adverse events, 5 (17.2%) trials did not show a better safety profile in the placebo group. Under the context that a relatively high-quality report is defined as a report with more than 9 items, there was a statistically significant difference between the two groups in the rate of relatively high-quality reports of the administration time (p = 0.047, OR 0.10, 95% CI 0.01 to 0.90), but the results are not representative.
Conclusion
The overall situation of HM-placebo in the field of rare diseases was poor. In particular, the placebo is tied to the quality of trials, and poor placebo hinders the generation of high-quality evidence for herbal clinical trials in the field of rare diseases. We summarize the current methods of assessment involved in the use of placebos and propose various considerations for placebos in different contexts. Our study can greatly promote rare disease researchers to review the quality of their placebo and clinical trials. It is imperative to guarantee that meticulously conducted research generates clinical evidence of the highest caliber. We also expect that in the future, more rigorous relevant standards about the reporting and design of HM-placebo will be developed. High-quality clinical trials are the prerequisite for the wide clinical application of herbal medicines for rare diseases.
Similar content being viewed by others
Introduction
Rare diseases are a group of diseases that are uncommon and have a very low prevalence compared to other diseases [1]. Currently, there are approximately 7000 different rare diseases affecting 3.5–5.9% of individuals worldwide, which amounts to 263–446 million individuals [2]. There are many kinds of rare diseases with complex etiology. Currently, the rare disease lists of different countries do not contain exactly the same diseases. The terms “rare disease” and “orphan drug” are used most widely and the average prevalence threshold is between 40 and 50 cases/100,000 people. As a result, the terminology and prevalence thresholds used to define rare diseases vary across jurisdictions and organizations [3]. At the same time, only 10% of rare diseases in the world are treated accordingly, and ~ 7000 rare diseases still lack specific treatments [4, 5]. The cure of rare diseases and the research of new drugs for rare diseases are common expectations of researchers worldwide.
Herbal medicine (HM), one of the main treatment modalities in the world, has a history of thousands of years and is still actively used in Asia and elsewhere worldwide. In modern times, HM is widely used in rare diseases, and experimental evidence has been obtained. Through our preliminary search in Web of Science, CNKI, and other databases on February 14, 2023. A total of 528 clinical trials of HM were found to have been conducted in the rare disease field. Among these clinical trials, there were also well-designed trials with effective for therapeutics such as ImmunoGuard®, which showed safety and efficacy for the management of patients with Familial Mediterranean Fever [6]. However, some published systematic reviews of HM trials in rare diseases suggest that the quality of clinical studies with poor trial designs still needs to be improved. Placebo-controlled trials were included [7,8,9].
For clinical trials of drugs, it is essential to follow the basic principles of randomization, repetition, blindness, and control [10]. High-quality randomized, double-blind, and placebo-controlled clinical trials can provide evidence to support HM treatment approaches [11]. Criticism of the quality of HM-placebos used is unfortunately common. The preparation and use of HM-placebos have been continuously explored by researchers [10, 12]. However, due to the characteristics of rare disease clinical trials, the use of HM-placebos in rare diseases has not been analyzed.
Given the critical need to generate robust clinical evidence, it is essential that clinical trials are completed with high quality. Our objective was to systematically review clinical trials that had been conducted in the field of rare diseases and to collect relevant trial information, with a focus on the use of placebo in the trials and on placebo reporting. This study accurately captures the problems in the field of herbal medicine in the treatment of rare diseases and provides references for future researchers to conduct safer and more effective clinical trials.
Methods
Data source
We conducted a cross-sectional analysis of HM clinical trials focusing on rare diseases. We searched 8 electronic databases, including PubMed, Embase, Web of Science, SinoMed, China National Knowledge Infrastructure (CNKI), WanFang database, China Science and Technology Journal Database (VIP), and National Institute of Informatics Support Academic Information Services (CiNii). The literature retrieval time ranged from the inception of each database to 14 February 2023. Ongoing trials and unpublished studies were searched via ClinicalTrials.gov and the Chinese Clinical Trials Registry (ChiCTR). The retrieval strategies are listed in Additional file 1.
Selection criteria
To be included, articles and trials had to meet the following criteria: (1) original clinical research; (2) due to the different definitions of rare diseases in different countries and regions, such as rare diseases defined as no more than one in 2000 individuals in the European Union and no more than approximately one in 1250 in the USA [13]. We also referred to the List of Rare Diseases (https://rarediseases.org/rare-diseases). Finally, combining population bases and different definitions of rare diseases, we chose China’s First List of Rare Diseases as a reference [14]; (3) placebo conducted as the control group in the trial.
Data extraction
YXL, CYR, and XYS authors reviewed the titles and abstracts of the retrieved articles after removing duplicates according to prespecified screening criteria. Articles that did not meet the inclusion criteria were removed. The full text of the remaining articles was independently screened by two authors (YXL and XBZ). Any discrepancies between the primary screening and full-text screening were discussed to resolve. The third (CZ) author was consulted when necessary.
Predefined data extraction tables were used to collect information for this study, two authors (YXL and XBZ) extracted the data from each trial record independently. The form of data extraction was composed of four parts: (1) General characteristics (title, author, country, year of publication, trial design, type of comparison, allocation ratio, type of disease, HM-intervention, ethics approval, informed consent, outcomes, calculation of sample size, randomization procedure, implementation of the intervention, measurement of outcome measures, and reporting of results and funding); (2) Placebo use characteristics (dosage form, administration route, the sample size of the placebo group, administration time of placebos, and controlled treatment method); (3) Reporting (TIDieR-placebo checklist [15], physically identical, quality control of placebo, assessment of safety, pharmacological inert test) and compositional characteristics of HM-placebo; (4) Efficacy and safety indicators (outcome measures and the occurrence of adverse events).
Data analysis
Trials characteristics are presented as mean ± standard deviation (SD) for continuous variables as all were confirmed to be normally distributed, or median and interquartile range for data that were not normally distributed. The Shapiro–Wilk test was used to inspect the normality of the quantitative data. Categorical variables were reported as counts (n) and percentages (%). All data were collected and recorded in Microsoft Office Excel (Version 365). Analyses were conducted using IBM SPSS version 26 (IBM, Armonk, NY, USA).
For the assessment of safety and efficacy, we calculated the frequency of any significant difference in results between the experimental and control groups and the frequency of adverse events in each group. Among the outcome measures of the trial, the proportions of outcome measures that had a positive effect with a statistically significant difference in the intervention group compared with the control group were calculated. The primary and secondary outcomes have equal status. For the comparison of safety, we used a similar method. An intervention was considered to be safer than placebos if adverse events occurred more frequently in the placebo group.
For the reported placebo analysis, a total of 17 reporting items were counted. The first is TIDieR-Placebo which is a user-friendly guide for reporting placebo and sham control interventions that include 13 items. In addition, considering the characteristics of HM-placebo, we added 4 additional items (physically identical, quality control of placebo, assessment of safety, and pharmacological inert test) for analysis. As the five trials had no published trial protocol or publication of results, data were missing at the time of TIDieR-placebo statistics, therefore, these five studies were excluded.
To analyze associations between the number of reporting items and the above factors, Chi-squared tests, and Binary multivariable logistic regression were used. The strength of the association with each categorical characteristic was described using an odds ratio and 95% Wald confidence intervals. Funding was dichotomized as non-business versus business involvement or not reporting. HM intervention was dichotomized as single herbal versus HM formula. Ethics approval was dichotomized as reported versus not reported. Inform consent was dichotomized as reported versus not reported. The sample size was dichotomized as 1–84 versus 84–150 according to the median value. Administration time of placebos was dichotomized as ≤ 1 month versus > 1 month according to the median value. The controlled treatment method was dichotomized as placebo added to other treatments versus only placebo. Whether the control group was treated with a placebo alone, we relied on the statements in their publications. For the sensitivity analysis, we define reporting items > 7, > 8, and > 9 as relatively high-quality reporting. The seven factors we selected were based on the number of each factor after classification.
We also rated the risk of bias of the RCTs using the revised Cochrane risk of bias, version 2 (RoB 2) tool according to journal articles, study protocols, clinical trials registries information and so on.
Results
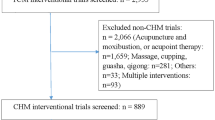
A total of 3101 records were retrieved. 837 records remained after duplicates were removed. After titles and abstracts were screened, 1645 records were excluded due to irrelevant study questions, non-herbal treatment and nonclinical trials. After the examination of 619 studies, a total of 55 studies accounting for 2233 enrolled patients were included (Fig. 1). The top four diseases were multiple sclerosis (32.7%), generalized myasthenia gravis (25.5%), idiopathic pulmonary fibrosis (23.6%), and amyotrophic lateral sclerosis (12.7%). In addition, 37 rare disease studies were conducted in China, and 18 were conducted in other countries, including Iran, Chile, the United Kingdom, Italy, and the United States (Fig. 2).
Distribution of included studies by countries’ disease and year. Data from 55 studies are included in this figure. Because of the relatively large number of trials in China and Iran, bubble plots were used for presentation. For trials in the ‘recruiting’ status, we included the time that the trial started. For trials in the ‘complete’ status, we included the time that the trial was completed. In China, the size of a scatter plot is the trial’s numbers. In Iran, the size of a scatter plot is the subject number because the disease was exclusively multiple sclerosis
General characteristics of included trials and HM-placebo use in trials.
For the characteristics of the included trials, 2 trials [16, 17] with the largest sample size included 123 subjects, and the intervention in one trial [18] was used for up to 2 years. Four [19,20,21,22] of the included trials had crossover designs and one trial [23] had an N-of-1 design. One [24] trial used a noninferiority trial and a 1:1:1 allocation ratio. One [25] trial had a 2:1 allocation ratio for the intervention versus the control group. The HM interventions were classified as either HM formulas (42; 76.4%) or single herbs (13; 23.6%). Of 55 included trials, 27 (59.1%) did not provide their ethical approvals; 11 (20%) also did not report informed consent, and only one trial had details of informed consent. Most (53; 96.4%) of the trials chose the oral route, and the common dosage forms were granules (24; 43.6%) and tablets (8; 14.5%). In these 55 trials, the median of placebo administration time is 84 days (IQR 42–180), and the median of placebo sample size is 30 (IQR 24–54). The sample size and duration of the placebo control group were mainly distributed from 1 to 30 (29; 52.7%, 31/56) and ≤ 3 months (28; 50.9%), respectively (Table 1). Additional details about the trial design are provided in Additional file 2: Table S1.
Reporting and compositional characteristics of HM-placebo
More than half of the items (11/17) were reported as relatively poor (Fig. 3). Performance was particularly poor in five areas: procedures, tailoring, modification, pharmacological inert test and measuring the success of blinding. None of the trials (0%) described procedures, activities, or processes for placebo use. 4 (8%) trials [21, 26,27,28] reported the placebo was personalized adapted. No one trial (0%) reported placebo was modified during the course of the study. No trials conducted pharmacological inert test. Successful blinding of the placebo design was assessed in only 1 (2%) trial [18].
Reporting rate of each item.17 reporting items were used for statistical analysis. The 13 items from the bottom up are the TIDieR-placebo checklist. a (Brief name) We counted all trials that provided the name of the placebo used by the control group, including the name “placebo”. b (Why) We accounted for all statements of reasons for the use of placebos, which reached 100% as stated in the purpose of the trial. c (What) We refer to the official example of TIDieR, and the studies we included did not have eligible procedures. d (Where) We analyzed the data by country or hospital. e (When and how much) For this item, we counted drug doses for each trial. f (Modification) If the placebo was modified during the course of the study, describe the changes. g (How well, actual) If adherence or fidelity was assessed, describe the true situation. 8 (16%) trials [6, 18, 29,30,31,32,33,34] did complete reporting for the composition of the placebo. 10 (20%) trials reported that who provided placebos. 7 (14%) trials [16, 28, 31, 35,36,37,38] described the modes of delivery. 7 (14%) trials [18, 28, 30, 33, 39,40,41] described strategies to maintain or improve adherence. 23 (46%) trials showed that the placebo was physically identical to experimental HM, but one trial [42] the placebo was checked by a pharmacist to make sure the placebo was physically identical to experimental HM. Moreover, a trial [6] that used the same coating for the drugs, which can effectively avoid the failure of trials caused by dissimilarity. The safety assessment includes safety testing of raw materials and health testing of subjects. Only 3 (5.5%) trials [27, 30, 31] have controlled placebo raw materials, and they include microbial limits and certificates of quality. The commonly used safety tests of subjects include routine blood, urine, stool, liver function, renal function, blood test, ECG, and adverse reactions. None of the trials performed a pharmacological inert test of the placebo, even though some of the placebos used the experimental HM. More detailed information is shown in Additional file 2: Table S1. We have also translated the abstracts of the studies published in Chinese and can be found in Additional file 3
For 32 trials that reported placebo compositions, 10 (18.2%; 10/55) trials included HM ingredients, and 22 (40%; 22/55) trials excluded HM ingredients in their placebos. The lower doses of the experimental HM were used primarily as placebo-containing herbal ingredients. 5% (n = 3) [35, 42, 43] and 10% (n = 4) [27, 36, 44, 45] were the most commonly used dosage percentages of HM ingredients. The placebos were mainly composed of excipients, such as soybean powder, starch, dextrin, maltodextrin, b-cyclodextrin, lactose powder, bitter taste agent, food color, etc. (Table 2). One trial [29] did not use the tested HM but also did not use additives. They used divine comedy, malt, Poria, Atractylodes, and coix seed, which are theoretically ineffective in MS.
Efficacy and safety profiles of herbal medicine compared to placebo
Based on the results showed that among the 50 trials with the outcome indicators 23 (46%) trials did not reflect the advantage of the intervention compared with the control group. Of the 29 studies with available data on adverse events, 14 (48.3%) had 'no adverse events were observed', and 5 (17.2%) [24, 27, 30, 46, 47] studies did not show a better safety profile in the placebo group. Trials that not fitted into the extraction format were narratively summarized in Additional file 2: Table S1.
Factors that might affect the quality of placebo reporting
The analytic factors included funding, HM-intervention, ethical approval, informed consent, sample size, administration time, and controlled treatment methods. Through the results of the Chi-squared analysis, we found that under the context that the number of report entries is delimited by 9, there was a statistically significant difference between the two groups in the rate of relatively high-quality reports of the administration time (p = 0.047, OR 0.1 95% CI 0.01 to 0.9) (Table 3). The results of the remaining Chi-square tests are shown in Additional file 4: Tables S2 and S3. Through the Binary multivariable logistic regression analysis of the results found, we found that the seven factors included had no statistically significant impact on the quality of the report. The results are attached in Additional file 5: Tables S4, S5 and S6. These phenomena suggest that the relatively poor design and reporting of placebos is a common problem in the rare disease field.
RoB2 assessment
The results of the risk of bias assessment were as follows. Regarding performance bias, 7 studies were evaluated high risk and 32 studies were evaluated some concerns. The missing outcome data domain is low risk. Randomization process and interventions implementation more than half existing some concerns. In terms of random sequence generation, only 14 RCTs described the specific randomization process. 9 studies without appropriate measurements of the outcome (Additional file 6: Fig. S1).
Discussion
A total of 55 herbal clinical trials were conducted for 6 rare diseases. The overall quality of HM-placebo in the field of rare diseases was poor. In the placebo preparation phase, almost all trials whether by technical or manual methods, did not assess placebo for safety, inertia, or blinding. None of the studies reported the overall details of the placebo. Nearly half of the trials provided their ethical approvals. In terms of safety, 17.2% of the clinical trials showed that placebos did not perform better than the intervention. Meanwhile, the quality of the included RCTS also deserves our attention.
Application of assessment methods
Superior placebo preparation is fundamental not only to trials but also to good placebo reporting. Placebo preparation of HM is limited due to its special sense of smell and taste, which is much more complicated compared to compound drugs. The materials used in the preparation of the placebo should be selected in strict accordance with the quality standards of pharmaceutical excipients and the hygienic standards for the use of food additives. Under the premise of ensuring safety and no active substances, the characteristics of various excipients and additives were compared to obtain the optimal formulation of each placebo [10]. For the raw materials of the placebo, we should ensure their safety and test items such as pesticide residue limit, microbial limit, aflatoxin, and nitrosamine. The safety of the drug during the trial is the focus of the subjects, especially the HM-placebo, which is often complex in composition, and its combination of substances may cause adverse reactions in the subjects. Therefore, safety monitoring during the trial is particularly important. The most used tests include routine blood tests, routine urine tests, electrocardiograms, liver function tests, and kidney function tests. Due to the vulnerability of patients with rare diseases, we should pay more attention to safety monitoring.
There are some difficulties in the preparation of placebos, some HM placebos are designed to contain 5% to 10% of the standard dose and to better simulate the specific odor and taste of HM extract, the remaining formulation consists of suitable excipient and additive. Therefore, the pharmacological inert test was recommended. The phenomenon can be seen from our statistical results that some trials did not show the superiority of intervention that used low doses of tested drugs over placebo, which may be related to the characteristics of rare diseases, but also cannot prove that this is not related to low doses of HM. Therefore, the detection of drug inertia may help us to support our trial results reasonably. The content of active ingredients was determined by pharmacodynamic tests, thin-layer chromatography, high-performance liquid chromatography, infrared spectroscopy, and ultraviolet spectroscopy.
One of the most important properties of placebos is similarity. The evaluation of similarity can be divided into manual evaluation and intelligent evaluation. In terms of manual evaluation, a study proposed three comparative evaluation methods, tested three dosage forms (oral liquid, capsule, granule), and compared the better evaluation method for other researchers to reference [48]. Intelligent evaluation methods include electronic noses, electronic tongues, and visual sensors [49,50,51]. Intelligent sensory technology can realize the objective evaluation of traditional HM-placebo. Machine vision technology, electronic nose and electronic tongue technology are used to collect relevant data for each sample, and the characteristics of placebo data are analyzed by different statistical methods. It can avoid the subjective factors caused by artificial scoring to some extent and is a powerful auxiliary for the evaluation of placebo. The similarity is fundamental to the success of blinding. According to Consolidated Standards of Reporting Trials (CONSORT), investigators are required to report not only whether blinding was performed but also the details and procedures of blinding and whether blinding was successfully performed. In 1996, James et al. systematically introduced the theory and application of James’ index through an application example of a clinical randomized controlled trial [52]. Later, Bang et al. further proposed Bang's index to evaluate blinding success [53]. The findings from RoB 2.0 indicate that a significant proportion of trials encountered challenges related to randomization and intervention delivery. Among the pivotal considerations in this evaluation is the aspect of blinding. The successful implementation of blinding crucially hinges upon the quality and similarity of placebos employed. Consequently, the role of placebo similarity is a factor of paramount importance that cannot be underestimated. The quality of placebos stands in close correlation with the conduct of clinical trials and, indeed, can be the determinant in ensuring the smooth implementation of a clinical trial. To improve the quality of HM clinical trials in the field of rare diseases and to produce higher quality clinical evidence under the premise of fully protecting the interests of subjects.
Ethical considerations
From the results of our trial, we can also see that the ethical review required by international authoritative organizations has not been perfect, and ethical review in the field of rare diseases should be fully considered. Given the genetic characteristics of rare diseases, children account for about 50% of patients with rare diseases. Thus, researchers and clinicians should always keep in mind that additional ethical considerations exist [54]. First, the researcher must provide adequate informed consent. How to get them to fully understand placebos is something researchers must carefully consider. Full informed consent should not simply be stated as ‘signed’. In the cases of pediatric patients, vulnerable patients are unable to provide consent, and trial details also need to be provided to their legal guardians. The summary of both the laboratory and clinical data accumulated to date was explained to subjects and their legal guardians in simple nontechnical language.
Placebos are a key link to trial design and ethics, and we also briefly analyze the ethical considerations for patients with rare diseases in different contexts. First, alternative trial designs, such as crossover studies, are needed. Crossover studies that include a placebo treatment period face the same ethical challenges as placebo-controlled studies using monotherapy [55]. Second, in noninferiority studies, the null hypothesis of inferiority must be rejected, demonstrating that experimental treatment is not inferior to the active comparator arm. If an established effective therapy (EET) is superior to placebos in prior clinical trials, performance on that EET should be able to be used as a control [56]. However, patient populations recruited for studies at different times may not be the same, and EET effects over time and in different study populations may differ [57]. Thus, comparability between the results of past placebo-controlled trials and the performance of the active control in the new trial cannot be demonstrated. The non-inferiority study design is inherently marked by its safety features. However, its application in the context of rare diseases poses a significant challenge, primarily because many rare diseases lack established, standard, and effective treatment modalities. Third, clinical trials in which an experimental agent or its placebo control is added to an EET are feasible and ethically acceptable [58]. However, this situation may affect the accurate assessment of the efficacy and safety of the tested drug. For rare diseases and smaller populations, researchers have always carried out studies on trial design to conduct clinical trials reasonably and effectively in the future [59,60,61,62]. We believe these considerations are consistent with both the need to develop improved therapies and the legitimate concerns for individual patient protection.
Reporting of placebo
There is no standard checklist for the quality evaluation of HM-placebo. Therefore, we refer to the TIDieR-placebo report for statistics and analysis in this study. However, we found that there was a need to develop a reporting checklist for HM-placebos. Based on our results, we recommend the following additional reporting information. First, the source of the raw materials should be reported. Regardless of the dosage form used, different sources of materials and different production personnel may affect the quality of the final placebo. Therefore, the entire control method for placebos should be reported. Second, the method of similarity assessment should be reported. Most of the included studies briefly describe the similarity in words. We recommend reporting on how to ensure their placebo is similar to HM. Researchers could choose one or more reasonable similarity evaluation indices mentioned above. As a special preparation, the dosage of each component of the HM placebo should be clearly defined. More attention should be paid to materials with pharmacological effects. For the addition of HM, regardless of whether it is a trial drug, we recommend a pharmacological inert test or a pharmacodynamic test to ensure that it has no pharmacological effect. At the same time, there is no optimal imitation method to explain why tested HM is added to placebos.
Strengths and limitations
This study has some limitations that must be considered. First, the localization study used only 10 databases, potentially limiting the number of studies included. Second, search terms are extensive, simple, and free. At present, there is no unified definition of rare diseases. Searches were limited to titles and abstracts, so it is possible that some articles were excluded from the study if the search term was not mentioned in the title or abstract. Third, this study focused on describing the use and reporting quality of HM-placebo, the logistic regression analysis was helpful to describe the reporting of HM-placebo in more depth. However, the limited trials included in this study may pose a challenge to the modeling process. To the best of our knowledge, this is the first study that summarized the use of HM-placebos in rare diseases. As our predefined selection criteria were wide, there are differences in the reporting content of each trial, but this can better reflect the problems with the current trial reporting. We did not have a priori restrictions regarding language, but our search only identified full-length articles in English and Chinese. We have done our best to retrieve all available data and to include factors that might have influenced the quality of placebo reporting, we believe that the general trends indicated by the analyses we have made are valid even if the information we have included in the analyses is incomplete .
Conclusion
Herbal medicines encompass the combination of practices of indigenous systems of medicine and several therapeutic experiences of many previous generations. Which delivers valuable references to the selection, preparation, and application of herbal formulation for the treatment, control, and management of rare diseases. Currently, certain countries have established well-defined herbal diagnostic and treatment protocols within the domains of hepatolenticular degeneration, multiple sclerosis, retinitis pigmentosa and so on. These endeavors have been instrumental in the ongoing exploration of the therapeutic potential of herbal medicine, offering promising pharmaceutical alternatives for orphan diseases. The ongoing progression of clinical trials in this sphere simultaneously serves as a cornerstone for future drug development. The use of HM-placebo in the field of rare diseases has increased in recent years. Despite its advantages in the evaluation of herbal products, its use in rare diseases is still relatively poor. As guidelines developed specifically from the point of view of placebos have increased over the years, they have matured and are used in controlled trials. However, in the future, more emphasis should be placed on a systematic reporting checklist of the compositions of HM-placebo to obtain quality publications. Regardless of the missing information in earlier reporting, while HM-placebo has been implemented in research, the use of HM-placebo in rare disease trials is highly recommended, and researchers are encouraged to apply it.
Availability of data and materials
Not applicable. Placebo-related data were collected from clinical trials of HM in the field of rare diseases and were not derived from a single data set.
Abbreviations
- ChiCTR:
-
Chinese Clinical Trials Registry
- CiNii:
-
National Institute of Informatics Support Academic Information Services
- CNKI:
-
China National Knowledge Infrastructure
- CONSORT:
-
Consolidated Standards of Reporting Trials
- ECG:
-
Electrocardiogram
- EET:
-
Established effective therapy
- HM:
-
Herbal medicine
- IQR:
-
Inter quartile range
- MS:
-
Multiple sclerosis
- N-of-1:
-
Randomized controlled trial in individual patient
- OR:
-
Odds ratio
- RCT:
-
Randomized controlled trial
- SD:
-
Standard deviation
- TIDieR:
-
Template for intervention description and replication
- 95% CI:
-
95% confidence interval
References
Haendel M, Vasilevsky N, Unni D, Bologa C, Harris N, Rehm H, et al. How many rare diseases are there? Nat Rev Drug Discov. 2020;19(2):77–8. https://doi.org/10.1038/d41573-019-00180-y.
Shourick J, Wack M, Jannot AS. Assessing rare diseases prevalence using literature quantification. Orphanet J Rare Dis. 2021;16(1):139. https://doi.org/10.1186/s13023-020-01639-7.
Richter T, Nestler-Parr S, Babela R, Khan ZM, Tesoro T, Molsen E, et al. Rare disease terminology and definitions—a systematic global review: report of the ISPOR rare disease special interest group. Value Health. 2015;18(6):906–14. https://doi.org/10.1016/j.jval.2015.05.008.
Tambuyzer E. Rare diseases, orphan drugs and their regulation: questions and misconceptions. Nat Rev Drug Discov. 2010;9(12):921–9. https://doi.org/10.1038/nrd3275.
Sharma A, Jacob A, Tandon M, Kumar D. Orphan drug: development trends and strategies. J Pharm Bioallied Sci. 2010;2(4):290–9. https://doi.org/10.4103/0975-7406.72128.
Amaryan G, Astvatsatryan V, Gabrielyan E, Panossian A, Panosyan V, Wikman G. Double-blind, placebo-controlled, randomized, pilot clinical trial of ImmunoGuard—a standardized fixed combination of Andrographis paniculata Nees, with Eleutherococcus senticosus Maxim, Schizandra chinensis Bail. and Glycyrrhiza glabra L. extracts in patients with Familial Mediterranean Fever. Phytomedicine. 2003;10(4):271–85. https://doi.org/10.1078/094471103322004767.
Song Y, Jia Q, Guan X, Kazuo S, Liu J, Duan W, et al. Herbal medicine for amyotrophic lateral sclerosis: a systematic review and meta-analysis. Front Pharmacol. 2022;13:946548. https://doi.org/10.3389/fphar.2022.946548.
Chen S, Xu MB, Zhou XL, Rong PQ, Jin TY, Zheng GQ. Chinese herbal medicine for myasthenia gravis: a systematic review and meta-analysis. Front Pharmacol. 2018;9:969. https://doi.org/10.3389/fphar.2018.00969.
Zhu SJ, Wang RT, Yu ZY, Zheng RX, Liang CH, Zheng YY, et al. Chinese herbal medicine for myasthenia gravis: a systematic review and meta-analysis of randomized clinical trials. Integr Med Res. 2022;11(2): 100806. https://doi.org/10.1016/j.imr.2021.100806.
Guo N, Wu F, Wu M, Wang Y, Lang Q, Lin X, et al. Progress in the design and quality control of placeboe’s for clinical trials of traditional Chinese medicine. J Integr Med. 2022;20(3):204–12. https://doi.org/10.1016/j.joim.2022.02.005.
Bian ZX, Moher D, Dagenais S, Li YP, Liu L, Wu TX, et al. Improving the quality of randomized controlled trials in Chinese herbal medicine, part II: control group design. Zhong Xi Yi Jie He Xue Bao. 2006;4(2):130–6. https://doi.org/10.3736/jcim20060205.
Zhang X, Tian R, Zhao C, Tang X, Lu A, Bian Z. Placebo design in WHO-registered trials of Chinese herbal medicine need improvements. BMC Complement Altern Med. 2019;19(1):299. https://doi.org/10.1186/s12906-019-2722-2.
Schieppati A, Henter JI, Daina E, Aperia A. Why rare diseases are an important medical and social issue. Lancet. 2008;371(9629):2039–41. https://doi.org/10.1016/s0140-6736(08)60872-7.
He J, Kang Q, Hu J, Song P, Jin C. China has officially released its first national list of rare diseases. Intractable Rare Dis Res. 2018;7(2):145–7. https://doi.org/10.5582/irdr.2018.01056.
Howick J, Webster RK, Rees JL, Turner R, Macdonald H, Price A, et al. TIDieR-Placebo: a guide and checklist for reporting placebo and sham controls. PLoS Med. 2020;17(9):e1003294. https://doi.org/10.1371/journal.pmed.1003294.
Zhang J, Zhang H, Yuan D, et al. Clinical efficacy of compound Huang Qi combined with bromopyzia in the treatment of myasthenia gravis. Chin Arch Tradit Chin Med. 2018;36(04):779–82. https://doi.org/10.13193/j.issn.1673-7717.2018.04.002.
Qiao W, Cui Y, Kong J, Jin D, Wang H, Xie W, et al. To evaluate the efficacy of compound Huangqi granules in the treatment of myasthenia gravis of spleen-kidney deficiency type I and II. Liaoning J Tradit Chin Med. 2018;45(07):1360–3. https://doi.org/10.13192/j.issn.1000-1719.2018.07.005.
Bertoglio JC, Baumgartner M, Palma R, Ciampi E, Carcamo C, Caceres DD, et al. Andrographis paniculata decreases fatigue in patients with relapsing-remitting multiple sclerosis: a 12-month double-blind placebo-controlled pilot study. BMC Neurol. 2016. https://doi.org/10.1186/s12883-016-0595-2.
Kim E, Cameron M, Lovera J, Schaben L, Bourdette D, Whitham R. American ginseng does not improve fatigue in multiple sclerosis: a single center randomized double-blind placebo-controlled crossover pilot study. Mult Scler. 2011;17(12):1523–6. https://doi.org/10.1177/1352458511412062.
Naseri M, Ahmadi A, Gharegozli K, Nabavi M, Faghihzadeh S, Ashtarian N, et al. A double blind, placebo-controlled, crossover study on the effect of MS14, an herbal-marine drug, on quality of life in patients with multiple sclerosis. J Med Plants Res. 2009;3(4):271–5.
Vaney C, Heinzel-Gutenbrunner M, Jobin P, Tschopp F, Gattlen B, Hagen U, et al. Efficacy, safety and tolerability of an orally administered cannabis extract in the treatment of spasticity in patients with multiple sclerosis: a randomized, double-blind, placebo-controlled, crossover study. Mult Scler. 2004;10(4):417–24. https://doi.org/10.1191/1352458504ms1048oa.
Deng T, Li R, Li S, Zhang S, Liu X, Yang W, et al. Curative effect of Qiang Ji Jian Li capsule in a randomized, double-blind, self-cross-controled test for myasthenia gravis. J Guangzhou Univ Tradit Chin Med. 1992;9(01):7–10.
Qiu G. A single case randomized controlled trial of Qiangji Jianli capsule in the treatment of myasthenia gravis with spleen-stomach qi deficiency. [Master]: GangZhou University of Chinese Medicine; 2022.
Fan M, Zhang Y, Miao Q, Zhang Q, Tao K, et al. Clinical trial of Feitong oral liquid in treating idiopathic pulmonary fibrosis. Tradit Chin Drug Res Clin Pharmacol. 2013;24(03):317–22.
Collin C, Davies P, Mutiboko IK, Ratcliffe S, Sativex Spasticity MSSG. Randomized controlled trial of cannabis-based medicine in spasticity caused by multiple sclerosis. Eur J Neurol. 2007;14(3):290–6. https://doi.org/10.1111/j.1468-1331.2006.01639.x.
Riva N, Mora G, Sorarù G, Lunetta C, Ferraro OE, Falzone Y, et al. Safety and efficacy of nabiximols on spasticity symptoms in patients with motor neuron disease (CANALS): a multicentre, double-blind, randomised, placebo-controlled, phase 2 trial. Lancet Neurol. 2019;18(2):155–64. https://doi.org/10.1016/s1474-4422(18)30406-x.
Zhe Z, Liu J, Zhao Z, et al. Clinical study on Modified Xiayuxue Granule combined with prednisone acetate tablets in the treatment of idiopathic pulmonary fibrosis with syndromes of deficiency of qi and yin and obstruction of lung collaterals. Acad J Shanghai Univ Tradit Chin Med. 2020;34(06):9–13. https://doi.org/10.16306/j.1008-861x.2020.06.002.
Wade DT, Makela P, Robson P, House H, Bateman C. Do cannabis-based medicinal extracts have general or specific effects on symptoms in multiple sclerosis? A double-blind, randomized, placebo-controlled study on 160 patients. Mult Scler. 2004;10(4):434–41. https://doi.org/10.1191/1352458504ms1082oa.
Zhuang Y. Therapeutic effect of integrated traditional Chinese and western medicine on multiple sclerosis. J Pract Tradit Chin Med. 2013;29(06):443–4.
Motaghi N, Tajadini H, Shafiei K, Sharififar F, Ansari M, Sharifi H, et al. Lavender improves fatigue symptoms in multiple sclerosis patients: a double-blind, randomized controlled trial. Mult Scler Relat Disord. 2022. https://doi.org/10.1016/j.msard.2022.104000.
Schröder S, Wang M, Sima D, Schröder J, Zhu X, Zheng X, et al. Slower progression of amyotrophic lateral sclerosis with external application of a Chinese herbal plaster—the randomized, placebo-controlled triple-blinded ALS-CHEPLA trial. Front Neurol. 2022;13:990802. https://doi.org/10.3389/fneur.2022.990802.
Rezaeizadeh H, Gharegozli K, Nabavi SM, Shayegannejad V, Ghaffarpoor M, Daneshfard B, et al. Effect of MS14 (R) on physical activity of multiple sclerosis patients: a randomized triple-blind placebo-controlled clinical trial. Mult Scler Relat Disord. 2023. https://doi.org/10.1016/j.msard.2022.104467.
Adalat M, Khalili M, Ayromlou H, Haririan S, Fazljou SMB, Rezaeizadeh H, et al. Antidepressant effects of a Persian medicine remedy on multiple sclerosis patients: a double-blinded randomized clinical trial. Galen Med J. 2019. https://doi.org/10.31661/gmj.v8i0.1212.
Adalat M, Khalili M, Ayromlou H, Haririan S, Rezaeizadeh H, Safari AA, et al. Anti-fatigue and hypnotic effects of a traditional herbal extract on multiple sclerosis patients: a double blind randomized clinical trial. World Fam Med. 2018;16(8):22–31. https://doi.org/10.5742/MEWFM.2018.93484.
Guo S, Feng J, Song Y, et al. Effects of Qizhu Kangxian Granules on the pulmonary function and life quality in patients with idiopathic pulmonary fibrosi. China J Tradit Chin Med Pharm. 2019;34(06):2810–4.
Liu Q. Clinical study of Fuzheng Tongluo decoction in the treatment of idiopathic pulmonary interstitial fibrosis syndrome of lung and kidney qi deficiency [Master]: ShangHai University of Chinese Medicine; 2019.
Deng T, Li R, Li S, Zhang S, et al. Curative effect of Qiang Ji Jian Li capsule in a randomized, double-blind, self-cross-controled test for myasthenia gravis. J Guangzhou Univ Tradit Chin Med. 1992;9(01):7–10.
Guo G, editor Effect of Shenzhe Zhurun mixture on esophageal lesions of systemic sclerosis. In: The 11th national symposium on rheumatology of traditional Chinese medicine, Guiyang, Guizhou, China; 2006.
Li JS, Yu XQ, Xie Y, Yang SG, Zhao LM, Zhou M, et al. Efficacy and safety of traditional Chinese medicine treatment for idiopathic pulmonary fibrosis: an exploratory, randomized, double-blinded and placebo controlled trial. Front Pharmacol. 2022. https://doi.org/10.3389/fphar.2022.1053356.
Delaviz E, Salehi M, Ahmadi A, Fararooei M, Vakili M, Ashjazadeh N. Effect of cinnamon on inflammatory factors, pain and anthropometric indices in progressive-relapsing multiple sclerosis patients: a randomized controlled trial. Jundishapur J Nat Pharm Prod. 2021. https://doi.org/10.5812/jjnpp.14505.
Etemadifar M, Sayahi F, Abtahi SH, Shemshaki H, Dorooshi GA, Goodarzi M, et al. Ginseng in the treatment of fatigue in multiple sclerosis: a randomized, placebo-controlled, double-blind pilot study. Int J Neurosci. 2013;123(7):480–6. https://doi.org/10.3109/00207454.2013.764499.
Cui F, Su H, Liu R, et al. Clinical observation of Fuzheng Tixie Souluo Formulain the treatment of idiopathic pulmonary fibrosi. Mod Chin Clin Med. 2017;24(04):27–30+5.
Yang SG, Yu XQ, Li JS, Xie Y, Zhang W, Ban C, et al. Efficacy and safety of Jin-shui Huan-xian granule for idiopathic pulmonary fibrosis: study protocol for a multicenter, randomized, double-blind, placebo-controlled trial. Trials. 2022;23(1):725. https://doi.org/10.1186/s13063-022-06684-0.
Zhu X, Zhang H, et al. Clinical efficacy and safety evaluation of supplementary Sijunzi decoction in treatment of ALS patients with splenasthenic syndrom. Clin Misdiagn Misther. 2017;30(01):81–7.
Gao Y, Liu Q, Zhang W. Clinical study of Fuzheng Tongluo decoction in the treatment of pulmonary and kidney Qi deficiency syndrome of idiopathic pulmonary fibrosis. J Liaoning Univ Tradit Chin Med. 2020;22(07):172–6. https://doi.org/10.13194/j.issn.1673-842x.2020.07.042.
Xu F, Chen J, Ping Y, et al. Clinical study on treatment of myasthenia gravis with Zhongjiling tablets. Mod Chin Clin Med. 2004;04:4–8.
Ciampi E, Uribe-San-Martin R, Cárcamo C, Cruz JP, Reyes A, Reyes D, et al. Efficacy of andrographolide in not active progressive multiple sclerosis: a prospective exploratory double-blind, parallel-group, randomized, placebo-controlled trial. BMC Neurol. 2020;20(1):173. https://doi.org/10.1186/s12883-020-01745-w.
Xiao M, Ying J, Zhao Y, Li Q, Zhao Y, Gao R, et al. Developing Placebos for clinical research in traditional Chinese medicine: assessing organoleptic properties of three dosage forms (oral liquid, capsule and granule). Front Pharmacol. 2021;12: 673729. https://doi.org/10.3389/fphar.2021.673729.
Huang Q, Xiao J, Sun Y, Hu X. Preparation method and quality evaluation of traditional Chinese medicine compound placebo. J Tradit Chin Med. 2015;56(15):1294–7. https://doi.org/10.13288/j.11-2166/r.2015.15.010.
Wang R, Luo D, He Z, Wu C. Objective evaluation of Huoxiang Zhengqi granule placebo. Chin J Exp Tradit Med Formulae. 2014;20(12):91–5. https://doi.org/10.13422/j.cnki.syfjx.2014120091.
Xiao S, Zhu X, Wang Y, Cheng J. Research overview of placebo quality evaluation in clinical trials of new traditional Chinese medicine. Tradit Chin Drug Res Clin Pharmacol. 2020;31(09):1128–32. https://doi.org/10.19378/j.issn.1003-9783.2020.09.019.
James KE, Bloch DA, Lee KK, Kraemer HC, Fuller RK. An index for assessing blindness in a multi-centre clinical trial: disulfiram for alcohol cessation—a VA cooperative study. Stat Med. 1996;15(13):1421–34. https://doi.org/10.1002/(sici)1097-0258(19960715)15:13%3c1421::Aid-sim266%3e3.0.Co;2-h.
Bang H, Ni L, Davis CE. Assessment of blinding in clinical trials. Control Clin Trials. 2004;25(2):143–56. https://doi.org/10.1016/j.cct.2003.10.016.
Giannuzzi V, Devlieger H, Margari L, Odlind VL, Ragab L, Bellettato CM, et al. The ethical framework for performing research with rare inherited neurometabolic disease patients. Eur J Pediatr. 2017;176(3):395–405. https://doi.org/10.1007/s00431-017-2852-9.
Lublin FD, Reingold SC. Placebo-controlled clinical trials in multiple sclerosis: ethical considerations. National Multiple Sclerosis Society (USA) Task Force on Placebo-Controlled Clinical Trials in MS. Ann Neurol. 2001;49(5):677–81.
Polman CH, Reingold SC, Barkhof F, Calabresi PA, Clanet M, Cohen JA, et al. Ethics of placebo-controlled clinical trials in multiple sclerosis: a reassessment. Neurology. 2008;70(13 Pt 2):1134–40. https://doi.org/10.1212/01.wnl.0000306410.84794.4d.
Temple R, Ellenberg SS. Placebo-controlled trials and active-control trials in the evaluation of new treatments. Part 1: ethical and scientific issues. Ann Intern Med. 2000;133(6):455–63. https://doi.org/10.7326/0003-4819-133-6-200009190-00014.
Rudick RA, Stuart WH, Calabresi PA, Confavreux C, Galetta SL, Radue E-W, et al. Natalizumab plus interferon beta-1a for relapsing multiple sclerosis. N Engl J Med. 2006;354(9):911–23. https://doi.org/10.1056/NEJMoa044396.
Gagne JJ, Thompson L, O’Keefe K, Kesselheim AS. Innovative research methods for studying treatments for rare diseases: methodological review. BMJ. 2014;349:g6802. https://doi.org/10.1136/bmj.g6802.
Roes KC. A framework: make it useful to guide and improve practice of clinical trial design in smaller populations. BMC Med. 2016;14(1):195. https://doi.org/10.1186/s12916-016-0752-xv.
Day S, Jonker AH, Lau LPL, Hilgers RD, Irony I, Larsson K, et al. Recommendations for the design of small population clinical trials. Orphanet J Rare Dis. 2018;13(1):195. https://doi.org/10.1186/s13023-018-0931-2.
Halley MC, Smith HS, Ashley EA, Goldenberg AJ, Tabor HK. A call for an integrated approach to improve efficiency, equity and sustainability in rare disease research in the United States. Nat Genet. 2022;54(3):219–22. https://doi.org/10.1038/s41588-022-01027-w.
Acknowledgements
The authors wish to acknowledge Dandan Zhang who volunteered her time and suggestions in this study.
Funding
This study was funded by the China Association of Chinese Medicine Project (Grant No.2021XS-001-01) and the Beijing University of Chinese Medicine Project (Grant No.2020TSRC-002).
Author information
Authors and Affiliations
Contributions
CZ designed the study and organized the team. CZ and XD provided methodological direction. YL, XZ and XS conducted study selection and data extraction. YL and PD conducted data analysis. YL wrote the main draft of the manuscript. YL prepared Figs. 1–2. CR prepared Fig. 3. XZ made all tables. CZ revised the language and draft. All authors reviewed the final manuscript and accepted responsibility for the decision to submit it for publication.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable. No clinical trials were conducted in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Retrieval strategies.
Additional file 2.
Summary of trials information.
Additional file 3.
Summary of abstracts of studies published in Chinese.
Additional file 4.
Chi-squared analysis.
Additional file 5.
Logistic regression.
Additional file 6.
Risk of bias of included studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, Y., Du, P., Zhang, X. et al. Qualified placebo for trials of herbal medicine treatment in rare diseases? A cross-sectional analysis. Orphanet J Rare Dis 18, 373 (2023). https://doi.org/10.1186/s13023-023-02987-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13023-023-02987-w