Abstract
Background
The pathogenic variants responsible for Birt-Hogg-Dubé syndrome (BHDS) in folliculin (FLCN) gene mostly consist of point mutations. Although large intragenic deletions/duplications have been reported in several case reports, the relationship between large intragenic deletions/duplications and phenotype in BHDS remains unclear.
Methods
We retrospectively identified and reviewed patients with a large intragenic deletion spanning exons 1–3 and analyzed their phenotypic features to compare with those of point mutation carriers in our hospital from January 1, 2017 to August 31, 2022.
Results
Twenty unique point mutations (including 4 novel mutations) were detected in 62 patients from 45 families (90%). Exons 1–3 deletion were identified in 8 patients from 5 families (10%) that resided in the same region, Feidong County of Anhui Province, China. Breakpoint analysis indicated that all the deletion breakpoints were flanked by Alu repeats. The prevalence of exons 1–3 deletion carriers in Feidong County was 8.1-times higher than that for BHDS in Anhui Province, suggesting a clustered phenomenon of exons 1–3 deletion. Significantly increased risk of pneumothorax was observed in those with exons 1–3 deletion compared with point mutations (91% vs. 58%, p value 0.047). The risk of renal cancer may be higher in those with exons 1–3 deletion than for those with point mutations (18% vs. 4%, p > 0.05).
Conclusions
Large intragenic deletion of exons 1–3 in FLCN was identified as a local aggregation phenomenon in Feidong County, China, and was associated with a significantly higher risk of pneumothorax compared to those with point mutations.
Similar content being viewed by others
Introduction
Birt-Hogg-Dubé syndrome (BHDS) is a rare autosomal dominant inherited disease caused by germline mutations in the FLCN gene [1]. It is characterized by varying expressivity of pulmonary, renal and cutaneous involvement. Multiple bilateral pulmonary cysts have been reported in over 80% of BHDS patients and predispose affected individuals to the occurrence of spontaneous pneumothorax [2, 3]. BHDS-associated renal tumors develop in 12–34% of cases and skin benign tumors occur in 68–84% of patients [4,5,6,7].
Mutations in the gene FLCN, located on chromosome 17p11.2, is associated with BHDS and consists of 14 exons [1]. To date, over 200 pathogenic variants have been reported worldwide, most of which are point mutations resulting in premature protein truncation [8, 9]. Toro et al. identified FLCN mutations in 88% of 58 clinically-diagnosed BHDS families by bidirectional DNA sequencing; large intragenic rearrangements may have been missed in the remaining 12% [4].
Kunogi et al. were the first to confirm the association of large intragenic deletions associated with BHDS in two affected individuals in 2010 [10]. Ding et al. identified three heterozygous large deletions in unrelated BHDS families, but genotype–phenotype correlations between large intragenic deletions versus point mutations were not comprehensively evaluated [11]. Further studies of large intragenic deletions in patients with BHDS seemed warranted.
We previously described the largest cohort of BHDS patients diagnosed in China, of which five patients from three unrelated families were identified to have a deletion encompassing exons 1–3 in FLCN [6]. In the current study, we aimed to report all the families with exons 1–3 deletion in FLCN evaluated at our hospital in an attempt to analyze their genotype–phenotype correlations compared with those carrying point mutations.
Methods
Study population
This single-centered, retrospective study was approved by the ethics committee of the First Affiliated Hospital of University of Science and Technology of China in Anhui Province (Number 2022-RE-436). We recruited patients diagnosed with BHDS in our Rare Lung Disease Clinic, supported by a multidisciplinary team, from January 1, 2017 to August 31, 2022 in this study. Informed consent was obtained from all patients but one died, which was waived. The study inclusion was a diagnosis of BHDS, which was based on the criteria proposed by the European BHDS consortium and required a patient to fulfill one major or two minor criteria [12]. The major criteria included: (1) At least five adult-onset fibrofolliculomas or trichodiscomas with at least one histologically confirmed; (2) Pathogenic FLCN germline mutation. The minor criteria: (1) Multiple bilateral, basally located lung cysts with no other apparent cause, with or without spontaneous pneumothorax; (2) Early onset (< 50 years), multifocal or bilateral renal cancer, or renal cancer of mixed chromophobe and oncocytic histology; (3) A first-degree relative with BHDS. Patients with the following conditions were excluded: age below 18 years, those with unclear diagnosis of BHDS or insufficient clinical data.
Clinical data of all patients including gender, age at diagnosis, smoking history, prior medical history (skin lesion, pneumothorax, and renal cancer), family history, imaging studies, genetic testing, and treatment were reviewed. Chest computed tomography (CT) results were assessed for the presence of pulmonary cysts and pneumothorax by a radiologist (Dr. WW) and two pulmonary physicians (Drs. YW, XH) independently. The total number (< 10, 10–20, > 20) and maximum diameter (< 2, 2–5, > 5 cm) of pulmonary cysts were recorded. The renal involvement was evaluated by ultrasound, abdominal CT, magnetic resonance imaging (MRI) or positron emission tomography-computed tomography (PET-CT). Skin manifestations were examined by an experienced dermatologist (Dr. JL) and skin biopsies were performed if the patient consented.
Mutation analysis of the FLCN gene
Genomic DNA was extracted from peripheral blood leukocytes following standard protocols and performed by Sanger sequencing or next generation sequencing (NGS) strategy. The sequencing reactions were conducted as previously described [6, 13]. MLPA (Multiplex Ligation-Dependent Probe Amplification) assay was performed to detect for large intragenic deletions/duplications in FLCN and its up/downstream regions using the commercial kit P256-B1 FLCN (MRC-Holland, Amsterdam, Netherlands). The probes of the kit can target all 14 exons. MLPA reactions were performed by following the manufacturer’s instructions. The polymerase chain reaction (PCR) products were analyzed on an ABI 3130 Genetic Analyzer (Applied Biosystems). Data were analyzed using the Coffalyser software (MRC-Holland). The junction fragments adjacent to the deleted regions were amplified using the PCR Amplification Kit (Takara, China) with specially designed primers (F: CTGAGGGACACCAAGCACTC R: TGGGAAAGATGTTAATGGCCTA). PCR products were separated by 2% agarose gel electrophoresis. Bidirectional Sanger sequencing was performed. FLCN mutations were numbered based on Genbank accession numbers NM_144997.7 according to the HGVS nomenclature guideline (http://www.hgvs.org/mutnomen).
Statistical analysis
Statistical analyses were conducted using SPSS version 25.0. Continuous variables were expressed as means and standard deviations and compared by independent sample t-test. Categorical variables were described as frequencies and percentages, and compared by the chi-square test and Fisher’s exact test. Binary logistic regression analysis was performed to identify risk factors for pneumothorax in BHDS. A value of p < 0.05 was considered statistically significant.
Results
A total of 76 patients from 50 unrelated families were diagnosed as BHDS in our Rare Lung Disease Clinic from January 1, 2017 to August 31, 2022. All patients with BHDS were of Han ethnic group. Seventy patients were confirmed by genetic testing and the remaining six by clinical diagnosis. Among them, forty-seven were female and the ratio of male to female was 1:1.6. The average age of diagnosis was 44 ± 14 years (range, 18–76 years). Eight (11%) patients had a smoking history.
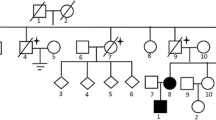
Germline mutations of the FLCN gene
DNA samples from these 50 unrelated families were analyzed, of which unique pathogenic FLCN variants were identified in 62 patients from 45 families (90%) by Sanger sequencing (38 families) and NGS strategy (7 families), and three patients (12.2, 21.2 and 44.2) did not undergo genetic testing since their first-degree relatives carried germline FLCN mutations (Additional file 1: Table S1). The mutation spectrum revealed 20 different mutations, including seven nonsense, seven frameshift, three splice site, two missense, and one in-frame mutations (Fig. 1). A known mutational “hot spot”, c.1285dupC in exon 11, was detected in 9 patients from 7 families (14%) (Additional file 2: Fig. S1B). In addition, four heterozygous novel mutations were identified: c.761 T > C detected in three families, c.599 T > C in one family, c.1381_1382insA in one and c.1283_1284insA in one, respectively. The remaining 5 FLCN sequence-mutation negative families (10%) were detected to have a large intragenic deletion encompassing exons 1–3, of which 8 patients from 5 families were diagnosed by MLPA analysis (F13、F14、F15、F34、F40) (Fig. 2A). In addition, 3 patients (34.2, 34.3 and 34.4) in F34 were clinically diagnosed since they exhibited at least one of BHDS-related manifestations and the proband (34.1) was an exons 1–3 deletion carrier. The 1.8 kb PCR products of the junction fragment was separated by agarose gel electrophoresis, whereas the 9.3 kb wildtype sequence was too long to be amplified (Fig. 2A). Analysis of the sequencing results demonstrated one breakpoint to be located near chr 17: 17,134,286 and another breakpoint near chr 17: 17,141,828 with the estimated deletion size of 7,543 bp in length. Further analysis illustrated the involvement of AluSz and AluSc located on the up and downstream breakpoint junctions, respectively (Fig. 2B and C). A 23 bp stretch of microhomology in both Alu repeats suggested microhomology-mediated genomic recombination as a possible mechanism underlying in the deletion.
Point mutations at FLCN found in our cohort are listed. White boxes represent exons and yellow boxes represent exons with pathogenic point mutations in FLCN. The number of patients for each mutation is given in parentheses. *One patient in each of the three mutations did not undergo genetic testing, but the mutations were identified in their first-degree relatives
The results of identification of FLCN intragenic deletion in BHDS patients. A The electrophoretogram by MLPA on the left shows that the patient (F14-3) has a loss of heterozygosity in exon 1, 2 and 3 (in red); PCR products of junction fragments were separated by 2% agarose gel electrophoresis on the right. The characters and numbers above the lanes corresponded to the subjects (P1-P4) and controls (C1-C2). B and C The electrophoretogram and DNA sequence analysis of breakpoint junction show the 7,543 bp deletion mediated by the microhomology (blue bold bases in C) in Alu repeats (Alu SZ and Alu SC indicated by blue rectangular box in Fig. 2B and blue bases in C) span the exon 1 to 3 (E1-E3) of FLCN gene. The black arrows indicate the position of the primer for amplification of breakpoint junction in B
The local aggregation phenomenon of exons 1–3 deletion
Interestingly, all 5 families harboring exons 1–3 deletion came from the same region, Feidong County, located near the center of Anhui Province; no kinship was identified among these families. Since nearly all BHDS patients in Anhui Province (including Feidong County) are evaluated and managed at our hospital, based on the most recent demographic data for Anhui Province at the end of 2021, the prevalence of BHDS in Anhui Province (population 61.13 million [14]) was estimated to be 1.24 cases per million. In Feidong County (population 1.09 million [15]), the carrier frequency of exons 1–3 deletion was 10.09 cases per million, which is 8.1 times higher prevalence of BHDS compared with that in Anhui population overall. The markedly increased frequency of exons 1–3 deletion carriers in a local region shows a clustered phenomenon of this variant in the FLCN gene.
Genotype–phenotype correlations
Of 76 affected individuals, 11 cases were carriers of exons 1–3 deletion, while the other 65 harbored point mutations. The demographic characteristics of these subjects are summarized in Table 1. The average age at diagnosis for BHDS in intragenic deletion carriers was 47 ± 12 years (range, 19–73 years); 8 patients (73%) were females and only 1 had a history of smoking. There was no significant difference between the patients with exons 1–3 deletion and those with point mutations in age at diagnosis, gender distribution, and smoking history.
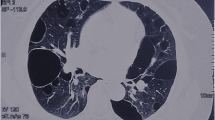
All 11 patients with large deletion had multiple bilateral pulmonary cysts, predominantly distributed in the lower lung fields (Fig. 3A). The cyst morphology varied greatly, mainly of round, oval or irregular shapes. All patients had pulmonary cysts > 20 mm, while the largest cysts in four (36%) were > 50 mm with the maximum size at 74 mm. For total number of cysts, 9 patients (82%) had more than 20 pulmonary cysts, 1 (9%) had 10–20 cysts; the remaining patient (9%) with fewer than 10 cysts were a 19-year-old female who was treated by bullectomy after suffering an episode of pneumothorax.
Pulmonary, kidney and skin involvements in BHDS patients with exons 1–3 deletion. A Chest CT showing multiple cysts distributed in the lower lungs (red arrows) and pneumothorax on the right. B Abdominal CT showing multiple bilateral kidney tumors with irregular edges (white arrows). C Hematoxylin and eosin staining of skin biopsy showing histologic features consistent with fibrofolliculoma (× 200)
Excluding 3 individuals without detailed CT data, multiple cysts were observed in 60 patients (97%) carrying point mutations including a 30-year-old male with only left-sided cysts. The largest cysts measured 20 to 50 mm in 31 patients (52%), and measured > 50 mm in 17 patients (28%). Sixty-three percent (38/60) of patients had more than 20 lung cysts and 25% (15/60) had 10–20 cysts. Although no significant difference in the sizes pulmonary cysts when comparing the two groups (exons 1–3 deletion versus point mutations), there was a tendency for the number of cysts in carriers of exons 1–3 deletion to be higher compared to those with point mutations (82% vs. 63%, p value 0.312).
Among 11 patients with intragenic deletion, 91% (10/11) experienced at least one episode of pneumothorax, with the mean age at the first episode of 36 ± 11 years (range, 19–58 years). The average number of pneumothorax was 2 ± 3 (range, 1–11). A female patient suffered the initial left pneumothorax at age 24 years and six episodes of ipsilateral recurrences, four episodes of contralateral pneumothoraces respectively in the following years despite three bullectomies and three chest tube drainage. A 43-year-old female has not developed pneumothorax yet, but her chest CT demonstrated more than 20 cysts with the largest cyst measuring 47 mm and located adjacent to the pleura.
58% (38/65) of sequence mutation-positive patients had experienced pneumothorax with an average number of 2 ± 2 episodes (range, 1–7). The mean age at onset of pneumothorax was 37 ± 12 years (range, 18–62 years). Mutation c.1285dupC was associated with a 33% risk (3/9) of pneumothorax. Significant difference was noted in pneumothorax risk between individuals with exons 1–3 deletion and those with point mutations (91% vs. 58%, p value 0.047). The risk of pneumothorax for subjects with exons 1–3 deletion was 2.8-times higher compared to those with c.1285dupC mutation (91% vs. 33%, p value 0.017). In addition, the relationship between history of pneumothorax and related factors mentioned above (smoking history, parameters related to pulmonary cysts, exons 1–3 deletion) was further examined by logistic regression analysis, which showed that only exons 1–3 deletion was associated with the presence of pneumothorax in BHDS (p value 0.028, odds ratio 10.000, 95% CI 1.280–78.117). However, there was no significant difference in the age at onset (p value 0.753) and the number of pneumothorax episodes between exons 1–3 deletion carriers and those with point mutation (p value 0.752).
Renal tumors were detected in 2 of 11 patients with exons 1–3 deletion (18%) (Fig. 3B). One patient underwent a partial nephrectomy for clear cell renal cell carcinoma at the age of 38 years. Due to poor performance status, another 73-year-old female was clinically diagnosed as having bilateral multifocal renal tumors by PET-CT. This patient underwent three renal artery embolization and died of advanced renal cancer 17 months later. Two patients with point mutations (4%) were found to have renal tumors as we previously described [6]. Large intragenic deletion carriers tended to be more likely to develop renal tumors compared to those with point mutations (18% vs. 4%, p value 0.126).
Eighty-nine percent (8/9) of carriers with exons 1–3 deletion manifested multiple pale or normal skin-colored papules on the face, neck, or upper trunk, of whom one underwent a biopsy and was confirmed to have fibrofolliculoma (Fig. 3C). Cutaneous involvement was seen in 78% (47/60) of point mutations carriers. Fibrofolliculomas were confirmed in 3 patients and trichodiscoma in 1. The prevalence of skin involvement in patients with large deletion and point mutations appeared to be similar (p value 0.674).
Discussion
In current study, we identified by MLPA and breakpoint assay a unique large intragenic deletion encompassing exons 1–3 in 11 individuals with BHDS from 5 unrelated families; clinical features were also analyzed comprehensively by comparing to those with point mutations. Deletion of the promoter region (contained in exon 1) would significantly reduce FLCN expression from the mutant allele, which was consequently proved to be a pathogenic variant. Benhammou et al. defined the promoter region as a “hot spot” for FLCN deletions [16]. FLCN intragenic deletions/duplications reported around the world were summarized and compared with point mutations, but no genotype–phenotype correlation was found [17]. To our knowledge, our study is the first to evaluate the relationship between a large intragenic deletion and a particular phenotype in the Chinese population.
Although the prevalence of BHDS in the general population was recently calculated to be 1.86 cases per million, the exons 1–3 deletion carrier frequency in Feidong County was 10.1 per million, 5.4-fold higher, and 8.1-times higher than the prevalence of pathogenic FLCN variant carriers in Anhui Province [18]. Thus far, only 2 BHDS families with deletion spanning exons 1–3 have been reported, in Anhui Province and an adjacent province, Jiangsu, respectively; the two families shared a 3.0 Mb common haplotype [11].
Lagerstedt-Robinson et al. identified a splice site variant c.779 + 1G > T in 57% of BHDS families in the Swedish population, which showed a strikingly high carrier frequency in Swedish origin and was verified to be a founder mutation [19]. A previous study also revealed a similar phenomenon of mutation c.1062 + 2 T > G in the Danish population and defined it as a founder mutation [20]. In combination with previous studies, our data raise the suspicion that a founder effect might have contributed to the dramatically high prevalence of exons 1–3 deletion in localized region, i.e., Feidong County. Although further research is required to prove this hypothesis, we speculate that the five families and previously reported two families with exons 1–3 deletion are distant relatives. The local aggregation phenomenon of exons 1–3 deletion is predicted to emphasize that BHDS is more common than we have previously thought and that a founder effect might exist in populations with less genetic diversity.
BHDS is characterized by a wide phenotypic variability, leading to difficulty in timely recognition and diagnosis. There have been several studies in recent years examining the genotype–phenotype correlation in BHDS [21, 22]. In the current study, we analyzed the cases carrying exons 1–3 deletion and point mutations diagnosed in our hospital and discovered a novel genotype–phenotype correlation. The deletion spanning exons 1–3 was associated with a 91% risk for pneumothorax, 1.6-times higher than for those with point mutations (58%) and 2.8-times higher than for c.1285dupC (33%). Moreover, there seemed a higher risk of developing renal tumors in exons 1–3 deletion (18%) compared with those with point mutations (4%).
Multiple pulmonary cysts are usually the earliest and the most common manifestation in BHDS. Imaging features of varying sizes, irregular shape, and basal predominant distribution of pulmonary cysts are considered important clues to distinguish BHDS from other diffuse cystic lung diseases [23]. The mechanisms leading to the development pulmonary cysts are still incompletely understood. Several hypotheses have been proposed, including alterations in matrix metalloproteinases resulting from disturbed extracellular matrix homeostasis, and stretch theory based on defects in cell–cell adhesion [24, 25]. Previous studies illustrated that the removal of the putative FLCN promoter region resulted in reduced mRNA and protein expression levels of FLCN, which was confirmed to be pathogenic in pulmonary cyst formation [16, 26]. In this study, significant difference was not found for the size of pulmonary cysts, but the intragenic deletion tended to have more pulmonary cysts compared to those with point mutations.
Pulmonary cysts in BHDS are associated with a 50-times higher risk of spontaneous pneumothorax compared to the general population [27, 28]. An American survey from patients with BHDS showed that more than 70% of affected individuals experienced at least one episode of pneumothorax, consistent with the reports on the Japanese population [29, 30]. Pneumothorax was the main reason leading to the BHDS diagnosis in 42% of patients at our medical center [6]. A German study illustrated that the risk of pneumothorax was 1.6-fold higher in those with c.1300G > C variant and 2.1-fold higher in those with c.250-2A > G variant compared with 37% risk with c.1285dupC [31]. The present study revealed that more than 90% of patients with exons 1–3 deletion experienced pneumothorax with the youngest affected patient being just 19-years-old at the initial onset. This risk was significantly higher than 58% risk for pneumothorax in those with the point mutations and 33% risk in the subgroup with c.1285dupC variant.
Renal cancer is the most severe complication of BHDS, with a seven-fold increased risk compared to the general population [28]. Sattler et al. examined the relationship between the risk of renal cancer and the intragenic position of the mutation, but did not find a significant correlation [22]. The prevalence of renal cancer in our cohort was relatively low (5%). Exons 1–3 deletion was associated with 4.5-fold higher risk compared to those with point mutations, but the difference was not significant; limited sample size and lack of long-term follow-up might be partly responsible. There may also have been a referral bias since most BHDS patients were identified in the respiratory department. Future studies with larger cohorts recruited from multidisciplinary approach are needed to explore the relationship between renal cancer and specific FLCN mutations.
Skin involvement is regarded as a common feature of BHDS in both Asian and Caucasian populations, presenting as multiple, dome-shaped, and asymptomatic papules during the third to fourth decades [6, 32, 33]. A skin biopsy can assist physicians to establish a diagnosis together with pulmonary or renal manifestations [12]. We observed no correlation between skin lesions and the variant of exons 1–3 deletion in this study but skin biopsies were performed in only a minority of cases (lack of patient consent).
There are several limitations to this study. Firstly, as a single-centered study, the sample size is relatively small, which may lead to potential bias in statistical results; multi-centered studies with larger cohorts are required to clarify the genotype–phenotype relationship in the future. Due to the retrospective nature of this study, thorough family screening was lacking for some patients which prevented us from verifying the founder effect of exons 1–3 deletion further. In addition, since the study is based on cases identified mainly through a lung disease clinic although with a multidisciplinary team, a selection bias may have led to an underestimation of renal cancers.
Conclusion
In conclusion, we identified a local aggregation phenomenon of large intragenic deletion spanning exons 1–3 in a region in the center of Anhui Province, China, which may represent a founder effect of FLCN mutation. Patients with exons 1–3 deletion were more likely to experience pneumothorax than point mutations carriers. Multi-centered prospective studies are needed to explore the relationship between renal cancer and large intragenic deletions.
Availability of data and materials
The datasets generated and analyzed for this study are not publicly available due to participant privacy but are available from the corresponding author upon reasonable request.
Abbreviations
- BHDS:
-
Birt-Hogg-Dubé syndrome
- FLCN :
-
Folliculin
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- PET-CT:
-
Positron emission tomography-computed tomography
- PCR:
-
Polymerase chain reaction
- NGS:
-
Next generation sequencing
- MLPA:
-
Multiplex ligation-dependent probe amplification
References
Schmidt LS, Warren MB, Nickerson ML, Weirich G, Matrosova V, Toro JR, et al. Birt-Hogg-Dubé syndrome, a genodermatosis associated with spontaneous pneumothorax and kidney neoplasia, maps to chromosome 17P11.2. Am J Hum Genet. 2001;69(4):876–82.
Gupta N, Sunwoo BY, Kotloff RM. Birt-Hogg-Dubé syndrome. Clin Chest Med. 2016;37(3):475–86.
Hu X, Zhang G, Chen X, Xu K. Birt-Hogg-Dubé syndrome in Chinese patients: a literature review of 120 families. Orphanet J Rare Dis. 2021;16(1):223.
Toro JR, Wei MH, Glenn GM, Weinreich M, Toure O, Vocke C, et al. BHD mutations, clinical and molecular genetic investigations of Birt-Hogg-Dubé syndrome: a new series of 50 families and a review of published reports. J Med Genet. 2008;45(6):321–31.
Schmidt LS, Linehan WM. Molecular genetics and clinical features of Birt-Hogg-Dubé syndrome. Nat Rev Urol. 2015;12(10):558–69.
Zhang G, Liu J, Wang Y, Wang Y, Jiang X, Peng Y, et al. Birt-Hogg-Dubé syndrome encountered at rare lung disease clinic in Anhui province, China. Orphanet J Rare Dis. 2022;17(1):203.
Schmidt LS, Nickerson ML, Warren MB, Glenn GM, Toro JR, Merino MJ, et al. Germline BHD-mutation spectrum and phenotype analysis of a large cohort of families with Birt-Hogg-Dubé syndrome. Am J Hum Genet. 2005;76(6):1023–33.
Kennedy JC, Khabibullin D, Boku Y, Shi W, Henske EP. New Developments in the pathogenesis of pulmonary cysts in Birt-Hogg-Dubé syndrome. Semin Respir Crit Care Med. 2020;41(2):247–55.
Lim DH, Rehal PK, Nahorski MS, Macdonald F, Claessens T, Van Geel M, et al. A new locus-specific database (LSDB) for mutations in the folliculin (FLCN) gene. Hum Mutat. 2010;31(1):E1043–51.
Kunogi M, Kurihara M, Ikegami TS, Kobayashi T, Shindo N, Kumasaka T, et al. Clinical and genetic spectrum of Birt-Hogg-Dube syndrome patients in whom pneumothorax and/or multiple lung cysts are the presenting feature. J Med Genet. 2010;47(4):281–7.
Ding Y, Zhu C, Zou W, Ma D, Min H, Chen B, et al. FLCN intragenic deletions in Chinese familial primary spontaneous pneumothorax. Am J Med Genet A. 2015;5:1125–33.
Menko F, van Steensel M, Giraud S, Friis-Hansen L, Richard S, Ungari S, et al. Birt-Hogg-Dubé syndrome: diagnosis and management. Lancet Oncol. 2009;10(12):1199–206.
Zhang X, Ma D, Zou W, Ding Y, Zhu C, Min H, et al. A rapid NGS strategy for comprehensive molecular diagnosis of Birt-Hogg-Dubé syndrome in patients with primary spontaneous pneumothorax. Respir Res. 2016;17(1):64.
Bureau of Statistics of Anhui Province, Anhui survey team of National Bureau of Statistics. Statistical Communiqué of Anhui Province on the 2021 National Economic and Social Development (in Chinese). Stat Theory Pract. 2022; (3): 31–79.
Bureau of Statistics of Feidong County. Statistical Communiqué of Feidong County on the 2021 National Economic and Social Development (in Chinese) https://tjgb.hongheiku.com/xjtjgb/xj2020/29816.html. Accessed 9 October 2022.
Benhammou J, Vocke C, Santani A, Schmidt L, Baba M, Seyama K, et al. Identification of intragenic deletions and duplication in the FLCN gene in Birt-Hogg-Dubé syndrome. Genes Chromosomes Cancer. 2011;50(6):466–77.
Cai M, Zhang X, Fan L, Cheng S, Kiram A, Cen S, et al. A Novel FLCN Intragenic Deletion Identified by NGS in a BHDS Family and Literature Review. Front Genet. 2021;12:636900.
Muller M, Daccord C, Taffé P, Lazor R. Prevalence of Birt-Hogg-Dubé syndrome determined through epidemiological data on spontaneous pneumothorax and Bayes theorem. Front Med (Lausanne). 2021;8:631168.
Lagerstedt-Robinson K, Baranowska Körberg I, Tsiaprazis S, Björck E, Tham E, Poluha A, et al. A retrospective two centre study of Birt-Hogg-Dubé syndrome reveals a pathogenic founder mutation in FLCN in the Swedish population. PLoS ONE. 2022;17(2):e0264056.
Rossing M, Albrechtsen A, Skytte AB, Jensen UB, Ousager LB, Gerdes AM, et al. Genetic screening of the FLCN gene identify six novel variants and a Danish founder mutation. J Hum Genet. 2017;62(2):151–7.
Sattler EC, Syunyaeva Z, Reithmair M, Dempke W, Steinlein OK. Colorectal cancer risk in families with Birt-Hogg-Dubé syndrome increased. Eur J Cancer. 2021;151:168–74.
Sattler E, Reithmair M, Steinlein O. Kidney cancer characteristics and genotype-phenotype-correlations in Birt-Hogg-Dubé syndrome. PLoS ONE. 2018;13(12):e0209504.
Xu W, Xu Z, Liu Y, Zhan Y, Sui X, Feng R, et al. Characterization of CT scans of patients with Birt-Hogg-Dubé syndrome compared with those of Chinese patients with non-BHD diffuse cyst lung diseases. Orphanet J Rare Dis. 2020;15(1):176.
Kumasaka T, Hayashi T, Mitani K, Kataoka H, Kikkawa M, Tobino K, et al. Characterization of pulmonary cysts in Birt-Hogg-Dubé syndrome: histopathological and morphometric analysis of 229 pulmonary cysts from 50 unrelated patients. Histopathology. 2014;65(1):100–10.
Kennedy JC, Khabibullin D, Henske EP. Mechanisms of pulmonary cyst pathogenesis in Birt-Hogg-Dube syndrome: The stretch hypothesis. Semin Cell Dev Biol. 2016;52:47–52.
Ding Y, Zou W, Zhu C, Min H, Ma D, Chen B, et al. Promoter methylation is not associated with FLCN irregulation in lung cyst lesions of primary spontaneous pneumothorax. Mol Med Rep. 2015;12(5):7770–6.
Yang J, Hu X, Li J, Zhang G, Ge Y, Wei W. Correlative analysis of lung CT findings in patients with Birt-Hogg-Dubé Syndrome and the occurrence of spontaneous pneumothorax: a preliminary study. BMC Med Imaging. 2022;22(1):22.
Zbar B, Alvord WG, Glenn G, Turner M, Pavlovich CP, Schmidt L, et al. Risk of renal and colonic neoplasms and spontaneous pneumothorax in the Birt-Hogg-Dubé syndrome. Cancer Epidemiol Biomarkers Prev. 2002;11(4):393–400.
Gupta N, Kopras EJ, Henske EP, James LE, El-Chemaly S, Veeraraghavan S, et al. Spontaneous pneumothoraces in patients with Birt-Hogg-Dubé syndrome. Ann Am Thorac Soc. 2017;14(5):706–13.
Furuya M, Yao M, Tanaka R, Nagashima Y, Kuroda N, Hasumi H, et al. Genetic, epidemiologic and clinicopathologic studies of Japanese Asian patients with Birt-Hogg-Dubé syndrome. Clin Genet. 2016;90(5):403–12.
Sattler EC, Syunyaeva Z, Mansmann U, Steinlein OK. Genetic risk factors for spontaneous pneumothorax in Birt-Hogg-Dubé syndrome. Chest. 2020;157(5):1199–206.
Dal Sasso A, Belém L, Zanetti G, Souza C, Escuissato D, Irion K, et al. Birt-Hogg-Dubé syndrome. State-of-the-art review with emphasis on pulmonary involvement. Respir Med. 2015;109(3):289–96.
Hasal E, Baskan EB, Gul S, Dilektasli AG, Sag SO, Adim SB, et al. Birt-Hogg-Dubé syndrome: diagnostic journey of three cases from skin to gene. Ann Dermatol. 2022;34(1):66–71.
Acknowledgements
We thank all the patients and families for their contribution to this work.
Funding
Funding was provided by Key medical and health specialty construction project of Anhui Province (Grant No. 2021szdzk05).
Author information
Authors and Affiliations
Contributions
XH and YW designed the study and drafted the manuscript. BS performed the molecular genetic testing, mutation analysis and manuscript editing. XH, YW, MC, GL, DH and GZ collected patients’ samples and clinical information, contributed to data analysis. XJ performed pneumothorax survey and manuscript editing. JL was consulted with patients’ skin lesions and performed the histological analysis of biopsied specimens. WW read all the CT scans of BHDS and assess all the CT features of BHDS patients. JX performed renal survey and manuscript editing. JHR supervised this study, checked, and revised this manuscript. All the authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of the First Affiliated Hospital of University of Science and Technology of China in Anhui Province (Number 2022-RE-436), and informed consent was obtained from all patients but one died, which was waived.
Consent for publication
Not applicable.
Competing interests
No competing interests were declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
FLCN germline mutations detected in 50 BHDS families.
Additional file 2: Fig. S1.
Genetic test revealed different FLCN mutations in 3 unrelated families.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, Y., Cai, M., Jiang, X. et al. Exons 1–3 deletion in FLCN is associated with increased risk of pneumothorax in Chinese patients with Birt-Hogg-Dubé syndrome. Orphanet J Rare Dis 18, 115 (2023). https://doi.org/10.1186/s13023-023-02710-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13023-023-02710-9